Abstract
Historically, surgical repair of pectus excavatum type of deformities was performed on patients who exhibited several sternal depressions, as the surgical procedure was associated with a high risk to justify it in patients with mild or moderate forms. Unnecessary radical procedures to repair pectus excavatum were not recommended and even partial or non-esthetic repairs were proposed to be considered as acceptable outcomes. Also, the primary intention of these surgical procedures was to address the symptoms of the patients with the aim of relieving cardiac compression, with cosmesis not being considered as the main aim of such repairs. With the changes in contemporary fashion trends and increased participation in sport activities, both of which are associated with larger exposure of the body, pectus excavatum repairs regained limelight in the past two decades. This chapter reviews the surgical procedures as they evolved in open repairs as well as minimal access repairs of pectus excavatum. Outcomes of these procedures have also been presented.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
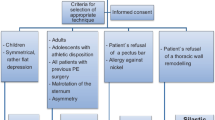
Historically, surgical repair of pectus excavatum type of deformities was performed on patients who exhibited several sternal depressions, as the surgical procedure was associated with a high risk to justify it in patients with mild or moderate forms [1]. Unnecessary radical procedures to repair pectus excavatum were not recommended and even partial or non-esthetic repairs were proposed to be considered as acceptable outcomes [2]. Also, the primary intention of these surgical procedures was to address the symptoms of the patients with the aim of relieving cardiac compression, with cosmesis not being considered as the main aim of such repairs. With the changes in contemporary fashion trends and increased participation in sport activities, both of which are associated with larger exposure of the body, pectus excavatum repairs regained limelight in the past two decades. Patients with pectus excavatum type of deformities perceived their bodies as a possible source of embarrassment which further manifested as socio-psychological problem of varying degrees in these patients. With the increase in self-referrals in the absence of symptoms to general practitioners during puberty and early adulthood, the trend of further referring these patients to Centers who could evaluate these patients as well as offer surgical corrections was established.
The timing of the surgical intervention is an area where the surgical community is divided and the opinions are divergent. Surgical procedures are best performed in early adolescence when the thoracic skeleton is more pliable and accommodating [3]. This view has also been shared by other groups that have large experiences with correction of pectus deformities [4]. The concerns of developing acquired thoracic dystrophy that has been reported after repairs in early years needs to be addressed [5]. In large series reported with open pectus repairs on young adolescents, the acquired thoracic dystrophy complication has not been observed [4, 6, 7]. The main reasons for the absence of this complication in these series was that surgical procedures were performed in Centers of expertise and in the hands of experienced surgeons and the common denominator in these techniques being the preservation of part of the perichondrium and the growth centers at the ends of the cartilages. Another important aspect that also favors correction in early adolescence is the observation of the fact that in half of the patients with pectus excavatum and mitral valve prolapse, the mitral dysfunction disappeared after pectus excavatum repairs [8].
Overview of Procedures
Prior to the advent of thoracic surgery, correction of pectus excavatum deformity was performed using by external traction, a method that was reintroduced in the 1920s by Zahradnicek [9]. The technique involved using traction on two wires introduced through operative perforations of the sternum.
The first surgical repair of pectus excavatum was performed by Wilhelm Meyer in 1911 who resected short segments of the right 2nd and 3rd costal cartilages with the intention of relieving cardiac compression [10] (Fig. 27.1). Meyer reported that the patient, who was significantly dyspneic before this intervention, improved significantly afterwards. Sauerbruch found this procedure to be of limited use and hypothesized that this limited resection could not be expected to relieve cardiac compression. In 1913, he performed a more radical procedure by resecting segments from the 5th down to the 9th costal cartilage, as well as the corresponding left hemisternum [11] (Fig. 27.2). Sauerbruch also advocated a more radical approach with bilateral resection of the 5th to 9th costal cartilage along with transverse resection of the sternum (Fig. 27.3).
Lexer in 1927 reported the treatment of a patient with severe pectus excavatum by resecting the sternum and replacing it in a turned-over position. Due to the resulting gap that occurred between the flipped sternum and the cartilages which caused difficulty in reattachment, the depressed sternal segment was removed [12] (Fig. 27.4).
Alexander in 1929 presented two different techniques on the two patients that were operated with trauma-induced pectus excavatum [13]. In the first patient, the sternum was divided transversely at the level of the third rib, then axially down to the xiphoid process (Fig. 27.5). In the second patient, the entire sternum was removed except the manubrium and the associated costal cartilages, leaving the heart exposed under the skin cover (Fig. 27.6). Alexander further used external traction after open repair and maintained it for various time intervals with the intention of achieving sufficient tissue fixation.
The next procedures advocated for repair involved the dissection as well as reattachment of the sternum. Nissen in 1943 resected the deformed portion of the sternum, after which it was flipped over and reattached horizontally to the costal cartilages [14] (Fig. 27.7). Judet and Judet in 1954 performed a complete sternal turn-over procedure by dissecting the sternum and reattaching the resected sternochondral margin into the consequent gap in the anterior chest wall [15] (Fig. 27.8). In these turn-over procedures the depressed portion of the sternum was explanted together with the deformed cartilages, turned over and reinserted into the resulting gap in the anterior chest wall. Any unwanted protuberance of the sternum was flattened using a hammer. This method was used extensively only in Japan by Wada, the shortcoming of this method being sternal necrosis and fistula formation [16, 17]. These complications prompted Taguchi to preserve the internal thoracic vessels. Ninkovic in 2003 revived the procedure by performing vascular anastomosis of the internal thoracic vessels (i.e. anastomosis of the the right internal thoracic vessels to the inverted left thoracic vessels) [18].
Lincoln Brown who proposed that pectus excavatum was caused by undue traction exerted upon the sternum by the diaphragmatico-sternal ligament, appropriately in 1940 designed two operative procedures in which all the tissue connection between the diaphragm and the lower sternum were divided [19]. The 1st procedure was indicated for infants or children. The basis of this procedure was to dissect the substernal ligament and/or the attachment to diaphragm under a small, vertical incision at level of the xiphoid in order to prevent the progression of pectus excavatum deformity in adulthood. The 2nd was indicated for older children, adolescents and adults (Fig. 27.9). The basis of this procedure was (a) resection of 2 cm costal cartilage segments of the 4th to 7th ribs near the junction with the sternum, and (b) wedge resection of the sternum at level of junction of the manubrium and sternal body. The elevated sternum was secured by wire sutures at the site of wedge resection. An external traction was added by fixation of a wire that penetrated the caudal part of the sternum and the 5th costal cartilage with a bridge placed on the anterior chest wall. The results of the operation were satisfactory only in young patients and this technique was unsuccessful in older individuals.
Sweet in 1943 and Brodkin in 1948 performed surgical repairs which was similar to the later but more popular Ravitch procedure [20, 21]. The Ravitch procedure consisted of (a) resection of deformed costal cartilages (b) dissection of the xiphoid-sternal junction, (c) cranial transverse sternal wedge osteostomy, and (d) refixation of the correctly positioned sternum [22] (Fig. 27.10). The wedge osteotomy was closed by interrupted silk sutures or wire sutures. However, the extensive defect resulting from excision of all of the deformed cartilages was left without sutures of any tissues. In 1965, Ravitch revised his original procedure in which he preffere an (a) oblique chondrotomy at 2nd or 3rd costal cartilages and overlap suture, sternal osteotomy on the posterior side of the sternum, instead of the anterior side as in the original procedure, and insertion of a small bone graft in the sternal opening. These modifications were done to offer better fixation to the mobilized sternum. A numerous modifications of the Ravitch procedure have been described by other surgeons and these modifications mainly differ from each other on the techniques to fix the mobilized sternum.
Due to less favorable outcomes of the Ravitch procedure, several surgeons such as Alexander, Adams, Lester, and Dailey propagated the idea of using posterior rib struts for fixation of the newly positioned sternum [2, 13, 23, 24]. Adkins in 1958 was the first to use a methyl methacrylate substernal support for fixation of the sternum [25].
The following surgical techniques which were developed to fix the sternum without the use of support:
-
(a)
Sicard in 1959 achieved the elevation and stabilization of the sternum by leaving the deformed cartilages in place and dividing them slanted towards the sternum [26]. These were then sutured together such that the divided ends overlap.
-
(b)
Ravitch in 1961 propagated the placement of 2–3 nonabsorbable periostal sutures onto the edges of the sternal transverse osteotomy is applied to maintain sternal stability [27].
-
(c)
Masson in 1970 utilized autogenous bone for concealment of the sternal depression [28].
-
(d)
Ravitch in 1977 also proposed to keep the sternum elevated is by shortening the perichondrial strips after chondral resection using “ruffling” sutures [29].
-
(e)
The Leonard procedure reported in 2003 which involves external traction applied for several months following open resection of the deformed cartilages and transverse wedge osteotomy using wires inserted through separate stab incisions has also been used to stabilize the sternum [30].
The following surgical techniques were developed to fix the sternum with the use of support using autogenous tissues:
-
(a)
Robicsek in 1960 used the xiphoid process which is frequently dissected from the sternum during pectus repairs. He mobilized the xiphoid process and flipped it under the sternum to support the corrected position of the sternum [31] (Fig. 27.11). For this the xiphoid was partially freed of its attachment to the rectus fascia, pulled under the sternum and suspended with heavy wire sutures on the superior ribs or perichondrial strips. The long, vertical incisions essential for appropriate exposure left unsightly scars, hence were replaced by Baronofsky with the currently used vertical submammary incisions [32].
-
(b)
Autogenous tibial grafts and ribs have also been used for retrosternal support [2, 13, 23, 24]. The only drawback with this technique is that it may create a second scar at the place of procurement if the tibial graft is opted and prolong the operating time; however, it offers advantages to metal bars as it does not require a second intervention for removal of the bars.
-
(c)
Suturing the perichondrial strips together behind the sternum in order to support the sternum should be avoided. This maneuver has not only been responsible for the decreases the thoracic diameter, but may retard chest growth and could lead to acquired thoracic dystrophy syndrome [33].
Welch in 1958 proposed a rather less radical procedure than Ravitch for the correction of pectus excavatum [34] (Fig. 27.12). Surgical correction was performed using bilateral subperichondrial resection of the deformed costal cartilages and sternal osteotomy resecting a wedge of the anterior cortex along with the fracturing of the posterior cortex. In the early cases using this technique, the sternum was secured by intramedullary fixation with a Steinman pin. Later on, the procedure was modified and the anteriorly displaced sternum was maintained with silk sutures closing the osteotomy defect [35].
Metals in the form of Kirschner wires or metal struts or plates were utilized for the correction of pectus deformities and an assortment of these materials is available for repairs [25]. Plates have been used for anterior, trans-sternal and posterior sternal supports [1, 36, 37].
Haller adopted the Ravitch procedure but presented it with two modifications in 1989 [38] (Fig. 27.13). Haller realized that the sternum was not properly supported in the Ravitch procedure for which he advocated the placement of a temporary stainless steel strut beneath the sternum, and anchored the strut bilaterally to the 5th or 6th ribs. The strut was removed on an outpatient basis, 6–9 months after the primary repair. Haller also noticed that too extensive and surgical repair in the early years could induce constriction of the chest wall and the total resections of the deformed costal cartilages in Ravitch procedure resulted in the removal of growth centers of costal cartilages which he termed as “acquired Jeune’s syndrome” [5]. His second modification was to shorten the length of the costal cartilages to 2.5 am and to exclude children below 4 years of age from surgery.
Fonkalsrud observed that in patients after the removal of deformed costal cartilages in the Ravitch’s procedure, the regenerated cartilages are thin, irregular, and commonly rigid with calcification, even if the perichondrial sheaths are preserved. His approach was to resect short segments of costal cartilages (3–8 mm) on the medial and the lateral ends of the deformed cartilages [39] (Fig. 27.14). After this resection, the remaining costal cartilages were reattached to the sternum and the ribs. A transverse sternal wedge osteotomy was also performed and the sternum was fixed using a thin stainless steel Adkins strut which was placed posterior to both the sternum and the costal cartilages to elevate the sternum.
Rehbein in 1957 presented a procedure to correct pectus excavatum with rib splints [40] (Fig. 27.15). After completing the mobilization of the costal cartilages with minimal resection, narrow metal splints were pushed into the rib. The sternum and the cartilages were elevated, the blades crossed and depressed. The sternum was fixed with a wire sling at the point of intersection. Costal cartilages which have been resected before to the necessary extent were secured by means of sutures. A stable fixation was achieved as the metal blades cross each other. In mild forms of pectus deformities one pair of rib splints were sufficient, however in moderate cases two pairs and in severe cases three pairs of ribs splints were necessary.
The Willital-Hegemann procedure has been used for the correction of pectus excavatum, pectus carinatum and other combined forms of protrusion-depression combined deformities since 1981 [37] (Fig. 27.16). In this procedure, repair is performed using a standard method of double bilateral chondrotomy parasternally and at points of transition to normal ribs. This is followed by a transverse sternal wedge osteostomy and detorsion of the sternum. The sternum edges after osteotomy are readapted by heavy absorbable sutures. Correction of the inverted ribs is performed using wedge osteotomy of ribs and readaptation using figure-of-8 sutures. Stabilization of the displaced sternum is performed using one trans-sternal strut. The two bilateral flail chest segments created are stabilized by and two parasternal metal struts. The metal struts are secured with each other by metal wires at the culmination points. Heavy absorbable sutures are used to secure the ribs to the struts at multiple points. Chest tubes are placed before completion of the procedure.
The PLIER procedure was reported in 2009 by the author and has been used for the correction of a variety of chest wall deformities [41] (Fig. 27.17). In this procedure, the repair is commenced with the dissection of the rectus muscle from the xiphoid and the lowere rib attachments. After this a retro-sternal extra-pleural space is created. The repair is performed using a standard method of double bilateral chondrotomy parasternally of 1 cm in a caudal to cranial direction. A minimum length of 1 cm of cartilage is left on the sternum ends with the aim of maintaining an intact growth centre. A transverse sternal wedge osteostomy and the sternum is brought to the desired position. The sternum edges after osteotomy are readapted by heavy non-absorbable sutures. Correction of the inverted ribs is performed using wedge osteotomy of ribs. Stabilization of the displaced sternum is performed using one trans-sternal strut. The costal cartilages are readapted with absorbable suture. Heavy absorbable sutures are used to secure the ribs to the struts at multiple points, and two non-absorbable heavy sutures are that circumvent the ribs are used to secure the metal strut at the both ends. Only, in case of severe pectus deformities or the presence of a platythorax the bilateral flail chest segments created are stabilized by and additional parasternal metal struts. The strut(s) are removed after 15 months.
Robicsek in 2000 reported a large series extending over a period of three decades using a synthetic mesh which was applied as a hammock to maintain the position of the sternum [4] (Fig. 27.18). In this procedure, segments of the involved costal cartilages are resected subperichondrially, beginning at the level of the height of the sternal depression. A minimum length of 1 cm of cartilage at both ends with the aim of preserving the growth centres. The xiphoid process is detached from the sternum. The lower end of the sternum is raised and is freed of mediastinal attachments. Staying close to the sternal edges, the perichondrial and intercostal strips are disconnected. Effective drainage of the entire operative field is achieved by widely connecting the retrosternal space with the right pleural cavity and draining the right chest through an intercostal drain. A transverse wedge osteotomy is then done at the upper level of the sternal depression and the posterior lamina is broken by bending the sternum forward. A sheath of large-pore Marlex mesh (CR Bard Inc., Covington, GA, USA) is cut roughly to the size of the previously existing chest wall depression and placed under the sternum like a hammock. The edges of the mesh are spread tight and sutured to the remnants of the costal cartilages or bony ribs with heavy, non-absorbable filaments. The detached xiphoid process is mobilized and sutured to the lower edge of the mesh. The edges of the pectoralis major muscles are adapted and the incision is closed without additional drainage.
Hu in 2008 presented a procedure with subperichondrial resections and trans-sternal strut placement [42] (Fig. 27.19). A transverse incision is made at the level of the xiphoid and the pectoralis major muscle is elevated from the sternum with ribs. Subperichondral resection of all deformed rib cartilages and a transverse wedge osteotomy were made across the anterior table of the sternum at the level where the sternum angles to depress posteriorly. Nonabsorbable sutures were placed across the osteotomy. In this procedure when subperichondral resection of deformed costal cartilages is performed, it is recommended to preserve the costochondral junction. The incisions made through perichondrium should be clean, so that after removal of the deformed cartilage, the perichondral sheaths can be sutured to form a tube to enable regeneration of new cartilage tissue. The intercostal muscle bundles attached to the side of the sternum are left intact and attached to the sternum. The metal strut for sternal elevation is passed through the sternum and is bent to an “arch” shape, after which the perichondrial sheath is wired to the strut to provide better remolding for the chest wall.
Masaoka in 2012 presented a correction procedure without the use of metal struts with five different series modifications [43] (Fig. 27.20).
-
In Series I the patients underwent the original Ravitch procedure (Fig. 27.20a), which was characterized by (a) resection of total deformed cartilages, (b) detachment of the sternum from the xiphoid, perichondria, and intercostal muscles, and (c) transverse sternal osteotomy and tripod fixation which involved fixation of the osteotomized sternum with a wedge of bone chip and overlap sutures of the obliquely transected bilateral 2nd or 3rd rib cartilages.
-
In Series II the modifications involved (a) suturing of the sternum and rectus abdominal muscle and (b) plication of the perichondria of the removed costal cartilages and attachment to the sternum (Fig. 27.20b).
-
In Series III two important modifications were adopted to strengthen the remodelled anterior chest wall. They were (a) shortening of the sternum by a 1–2 cm resection at the 5th intercostal level and (b) reduction of the length of the resected cartilages and suturing both stumps of the cartilages (Fig. 27.20c).
-
In Series IV, the modifications involved an oblique osteotomy on the posterior surface of the sternum to correct the rotation of the sternum, and a bone chip was wedged in this slit. Tripod fixation remained unchanged (Fig. 27.20d). This procedure was planned for adults and a different procedure was developed for children. The tripod fixation was omitted because the sternum could be elevated effortlessly by resection of deformed cartilages (Fig. 27.20e). The adult-type procedure was abandoned because of difficulties in correction of platythorax and asymmetry pectus without the use of a metal strut.
-
In Series V, sternal resection was performed at the 5th costal level, moving slightly to the cranial side, which was supported by a bridge constructed with bilateral 4th or 5th rib cartilages (Fig. 27.20f). This procedure was developed to strengthen the sternal support by autogenous tissue.
Nuss in 1998 reported on a minimal access procedure for the repair of pectus excavtum [44] (Fig. 27.21). The procedure involves bilateral chest wall incisions in the mid-axillary line and depending on the severity of the deformity, insertion of 1–3, arched metal bars through small lateral incisions, pushing them forward through both pleural cavities and the retrosternal space, then turning them with their convex side up, pushing forward the depressed anterior chest wall. The ends of the metal par are secured with stabilizer plates, with the trend to use a single stabilizer plate on the right side by most of the Centres. The bars are left in place for a period of 3 years. Nuss modified the original procedure, with the aim of avoiding injuries to vascular structures and to address the problem of bar dislocations. The modifications included (a) use of endoscopic visualization to observe the progression of the introducer tip in the thorax, (b) use of introducer to establish a tunnel for bar placement and (c) securing the bar with stabilizer with a polydioxanone (PDS) sutures around the bar and underlying ribs on the right side, and (d) use of two or more bars in the patients with asymmetry or platythorax. A variety of this technique was reported by Schaarschmidt in 2002, where the bars are positioned under the sub-muscular space rather than through the pleural spaces [45]. Park in 2010 added three further modifications: (a) use of a ‘crane’ to elevate the depressed sternum before introducer is inserted and (b) use of morphology-tailored bar shaping system named “terrain contour matching” and (c) multipoint fixation of the bar (the bar is fixed at the hinge point which is done by passing a needle directly through the overlying skin, passing it around the rib, and back through the skin and tied) [46]. Pilegaard in 2008 proposed to use absorbable stabilizer in order to avoid chronic pain and necessity of removal. However, since these stabilizers break easily, further research is needed if they are to be used as part of the standard procedure [47].
Harrison in 2010 proposed the Magnetic Mini-Mover Procedure (3MP) for the correction of pectus excavutum [48] (Fig. 27.22). The 3MP uses a magnetic implant coupled with an external magnet to generate force sufficient to gradually remodel the deformities. The magnimplant is set at surface of the sternum, and the magnatract is set on the rear side of the external brace, which is worn by the patient. The principle of this procedure is that the magnetic attraction between the magnimplant and the magnatract is used to lift up the sternal depression.
There are various procedures that have been suggested for the repair of pectus excvatum by plastic surgeons. In 1970, Masson and colleagues implanted a preformed silastic implant, with Dacron mesh patches on it, through a transverse incision just below the xiphoid [28]. Snel in 2009 presented a review of 75 patients with silastic implants in which complications occurred in seven patients (43 %) (Prolonged seroma in five, in which the implant was removed in one patient while repositioning was necessary in 2) [49]. Further, in two patients implants were removed due to pain and discomfort. Michlits in 2009 performed free fasciocutaneous infragluteal flap [50]. These plastic surgical procedures may provide better cosmesis; however, they cannot reduce compression on hearts and lungs from the sternal depressions. Hence, they are not suitable for symptomatic patients. Moreover, implantations of foreign body are not free from complications and always bear the risk of infection and displacement.
Outcomes
Since there are numerous surgical procedures that have been designed and performed with modifications for pectus excavtum, comparison between the procedures is not possible. Any new procedure that evolves is always ‘mistakenly’ compared to the ‘classical’ Ravitch procedure of the 1950s; a procedure which has undergone hundreds of modifications and if performed is reported as ‘modified’ Ravitch procedure. The future course of pectus excavtum surgery will require well-controlled evidence based trials which should compare procedures with more effective and less radical ones.
Evaluation of Large Series with Open Repairs
In order to evaluate the complications, larger series in the hands of experienced surgeons need to be evaluated. Table 27.1 presents the list of authors with large experience in open repair of pectus excavutum deformities. However, the complications and the outcome in these series present large variations in patient populations are not uniformly presented.
In the series of operations reported by Ravitch, there were two patients with staphylococcal infection, in one of these patients the removal of the sequester was necessary. No other complications were mentioned in this series [51]. In the series reported by Haller, morbidity was reported to be less than 5 with 10 % patients requiring redo procedures for recurrences during the evolution of the technique [38]. After the evolution of the technique, unsatisfactory results were reported in 3 of 352 procedures and good to excellent results were achieved in 95 % of the patients.
In the series reported by Shamberger using the Welch procedure, the repairs were completed with a low complication rate of 4.4 % [35]. Six complications were associated with Steinman pin fixation which was employed in the initial 28 patients. Major recurrence occurred in 17 patients (2.7 %) and with revisions necessary in 12. Satisfactory long-term results were achieved in the remaining 97.6 % of the patients, with follow-up ranging from 2 weeks to 27 years.
In the series reported by Robicsek [4], relevant postoperative complications were bleeding from the internal thoracic artery, infection, and seroma formations. The frequencies of these complications were not reported.
The series reported by Saxena et al. had a complication of 5.7 %. This series reported on long-term follow up and evaluation of late results which demonstrated a 1.4 % rate of major recurrences requiring surgical corrections. In this series mild recurrences were observed in 3.6 % patients, and these patients did not undergo surgical corrections. Furthermore, subjective complaints of the patients before the procedures were reported to be eliminated in 97 % of the patients.
In the series reported by Hu, early removal of metal bar due to dislodgement was necessary in four patients [42]. Whereas, recurrent depression was observed in three patients (0.75 %), a protrusion of 2nd or the 3rd costal cartilages was seen in five patients (1.26 %). Reconstructive procedures were successful in 98.7 % patients. Hu further reported the cardiac functions in these patients returned to normal level as observed by healthy individuals of comparable ages.
Fonkalsrud reported his series with a complication rate of 8 % [52]. Recurrences were reported in 5 (17 %) patients in Series-I, 15 (4.3 %) patients in Series-II, 7 (3 %) patients in Series-III and 4 (1.3 %) patients in Series-IV. From the four Series combined, a total of 22 (2.4 %) patients underwent surgery for recurrences. Surgeries for recurrences were reported to decrease during the learning curve. Satisfaction of surgical outcomes was evaluated and 94.2 % the patients or parents considered the results to be very good or excellent.
Masaoka reported 34 (11 %) patients with complications in his series of 307 patients [43]. He reported on six different series of procedural variations with variable groups of patients in each series, hence comparison of results is not possible.
Evaluation of Large Series with Minimal Access Repairs
With the advent of minimal access repair of pectus excavatum (MARPE) of 1998, complications and outcomes of this procedure are also difficult to evaluate, due to the evolution of this procedure over the past decade and the learning curve of the surgeons that performed such procedures.
Kelly in 2010 reported the outcomes of MARPE on 1215 patients in 2010 with an evaluation based on grades of satisfaction of the patients or the parents [53]. Excellent results were gained in 85.3 %. In their series, the majority of complication were categorized as minor, except for the single case of hemothorax that occurred due to injury of the internal mammary vessels. These complications were related to the period immediately during or early after repairs. The late complications were mainly associated with the displacement of the bar in 64 (5.7 %) patients in whom 45 required repositioning of the bar. It was also observed that the bar displacement rate was 12 % when no stabilizer plate was used, 6 % when wires were used to secure the pectus bar to the stabilizer plate and 2 % when pericostal sutures were placed to secure the bars. Allergy due to the implanted pectus bars was reported in 3.1 % of the patients.
Park compared the results of 1170 patients in two series with procedures performed between 1999 and 2002 to those performed between 2006 and 2008 [46]. A decrease in the total number of complications from 17 to 7.5 % was observed between the two periods. Decrease in the rates of pneumothorax from 7.5 to 0.8 %, bar displacement from 3.8 to 0.5 % and reoperation from 5.1 to 0.8 % were also evident in the two periods respectively.
Pilegaard reported on a series of 383 patients with 178 (49 %) pneumothorax, two bleeds, four pleural effusion, 11 seroma formations and in 11, and eight deep infection in eight [54]. Seven (1.8 %) patients were required surgical repositioning for displaced bars, whereas an additional 13 patients the stabilizer plate required removal because of pain.
The potential of injury to the heart or the great vessels that is associated with massive haemorrhage is the most dreaded complication of MARPE [55, 56]. This complication could be life-threatening and require emergency surgery. This complication could occur during the surgical procedure, or in the late period of the postoperative course or at the time of bar removal [57, 58]. Despite the evolution of MARPE these complication still occur and are being increasingly reported.
Standardization of Results
The scenario in the repair of pectus excavtum type of deformities has had an enormous shift in the change of indication which has moved from the treatment of symptomatic patients in the past to the more contemporary esthetic and psycho-sociological indication for repair. The evolution of diagnostic and imaging technology such as computed tomography 3D reconstructions (that cannot be performed repeatedly due to associated concerns with radiation) to non-invasive non-radiation associated videostereoraster among others have to be standardized in order to compare results being reported (Figs. 27.23 and 27.24). Comparison of results will have to take into account the following factors prior to and after surgery before data interpretation based on evidence is possible:
-
1.
Type of pectus deformity (symmetric/asymmetric)
-
2.
Shape of the thorax (presence/absence of platytorax)
-
3.
Presence of combined deformities
-
4.
Lower rib eversion (Fig. 27.25)
-
5.
Age of the patient at the time of surgery
-
6.
Cardiovascular evaluations
-
7.
Pulmonary evaluation
-
8.
Imaging (Computed tomography/Videosteroraster/Caliper/Flexible ruler)
-
9.
Evaluation of result by patient/parent
-
10.
Evaluation of the result by surgeon
-
11.
Psychological evaluation
-
12.
Use of a standardized procedure
-
13.
Complications during and immediately after the procedure
-
14.
Late complications
-
15.
Complications during bar removal (if metal is used)
-
16.
Long-term follow up
The channeling of the variations in the presentation of pectus excavatum type of deformities, standardization of perioperative diagnostic investigations and clear guidelines for outcome criteria need to be established for the proper evaluation of results.
References
Wachtel FW, Ravitch MM, Griswhman A. The relation of pectus excavatum to heart disease. Am Heart J. 1956;22:121–37.
Lester CW. Surgical treatment of funnel chest. Ann Surg. 1946;126:1003–7.
Saxena AK, Schaarschmidt K, Schleef J, et al. Surgical correction of pectus excavatum: the Munster experience. Langenbeck’s Arch Surg. 1999;384:187–93.
Robicsek F. Surgical treatment of pectus excavatum. Chest Surg Clin N Am. 2000;10:277–96.
Haller Jr JA, Colombani PM, Humphries CT, Azizkhan RG, Loughlin GM. Chest wall constriction after too extensive and too early operations for pectus excavatum. Ann Thorac Surg. 1996;61:1618–24.
Saxena AK, Willital GH. Valuable lessons from two decades of pectus repair with the Willital-Hegemann procedure. J Thorac Cardiovasc Surg. 2007;134:871–6.
Fonkalsrud EW, DeUgarte D, Choi E. Repair of pectus excavatum and carinatum in 116 adults. Ann Surg. 2002;236:304–14.
Shamberger RC, Welch KJ. Mitral valve prolapse with pectus excavatum. J Pediatr. 1987;111:404–6.
Zahradnicek J. Funnel shaped chest. JAMA. 1926;36:456.
Meyer WL. Zur chirurgischen Behandlung der angeborenen Trichterbrust. Berl Klin Wschr. 1911;84:1563–6.
Sauerbruch F. Operative Beseitigung der angeborenen Trichterbrust. Deutsch Zeitschr Chirurgie. 1931;234:760–4.
Ochsner JL, Ochsner A. Funnel chest (chone-chondrosternon). Surg Clin North Am. 1966;46:1493–500.
Alexander J. Traumatic pectus excavatum. Ann Surg. 1931;93:489–94.
Nissen R. Osteoplastic procedure for correction of funnel chest. Am J Surg. 1943;43:169–73.
Judet J, Judet R. Thorax en entonnoir. Rev Orthop. 1954;40:248–57.
Wada J, Ikeda T, Iwa T, Ikeda K. An advanced new surgical method to correct funnel chest deformity. J Znt Coll Surg. 1965;44:69.
Laituri CA, Garey CL, St Peter SD. Review of the technical variants in the repair of pectus excavatum. Eur J Pediatr Surg. 2010;20:217–21.
Ninkovic M, Schwabegger A, Gardetto A, Moser-Rummer A, Rieger M, Ninkovic M, Rainer C. Free sternum turnover flap for correction of pectus excavatum deformity. Plast Reconstr Surg. 2003;112:1355–61.
Brown AL. Pectus excavatum (funnel chest). J Thorac Surg. 1939;9:164–84.
Sweet RH. Pectus excavatum. Report of two cases successfully operated upon. Ann Surg. 1944;119:922–34.
Brodkin HA. Congenital chondrosternal depression (funnnel chest). Am J Surg. 1948;75:76–80.
Ravitch MM. The operative treatment of pectus excavatum. Ann Surg. 1949;129:429–44.
Adams HD. Costosternoplasty with rib strut support for funnel chest in adults. Lahey Clin Bull. 1951;7:111–6.
Dailey JE. Repair of funnel chest using substernal osteo-petriostal rib graft strut. JAMA. 1952;150:1203–4.
Adkins PC, Gwathmey O. Pectus excavatum: an appraisal of surgical treatment. J Thorac Surg. 1958;16:714–28.
Sicard A, Perez C. Traitement chirurgical du thorax entonnoir. Nouvelle technique de correction esthetique par greffons superposes. J de Chirurgie. 1959;77:306–22.
Ravitch MM. Operative treatment of congenital deformities of the chest. Am J Surg. 1961;101:277–96.
Masson JK, Payne WD, Gonzales JB. Pectus excavatum: use of preformed prosthesis for correction in the adult. Plast Reconstr Surg. 1970;46:399–402.
Ravitch MM. Congenital deformities of the chest wall and their operative correction. Philadelphia: W. B. Saunders; 1977.
Soto L, Kirzeder D, Larsen D, Saltzman D, Leonard D. The Leonard modification of the Ravitch procedure for pectus excavatum repair. J Am Coll Surg. 2003;197:S32.
Robicsek F, Sanger PW, Taylor FH, Stam RE. Xiphoid interposition. A modification for the repair of pectus excavatum. Am Surg. 1960;26:329–31.
Baronofsky ID. Technique for the correction of pectus excavatum. Surgery. 1957;42:884–90.
Robicsek F, Fokin AA, Watts LT, et al. Complications of pectus deformity repair. In: Patterson GA, editor. Pearson’s thoracic and esophageal surgery, vol. I. Philadelphia, PA: Churchill Livingston; 2008. p. 1340–50.
Welch KJ. Satisfactory surgical correction of pectus excavatum deformity in childhood. J Thorac Surg. 1958;36:697–713.
Shamberger RC, Welch KJ. Surgical repair of pectus excavatum. J Pediatr Surg. 1988;23:615–22.
Mangiardi JL. A simple surgical appliance for pectus excavatum. Surgery. 1956;39:261–4.
Willtal GH. Operationsindikation-Operationstechnik bei Brustdeformierung. Z Kinderchir. 1981;33:244–52.
Haller Jr JA, Scherer LR, Turner CS, Colombani PM. Evolving management of pectus excavatum based on a single institutional experience of 664 patients. Ann Surg. 1989;209:578–82.
Fonkalsrud EW. Open repair of pectus excavatum with minimal cartilage resection. Ann Surg. 2004;240:231–5.
Rehbein F, Wernicke HH. The operative treatment of the funnel chest. Arch Dis Child. 1957;32:5–8.
Saxena AK. Pectus less invasive extrapleural repair (PLIER). J Plast Reconstr Aesthet Surg. 2009;62:663–8.
Hu TZ, Li Y, Liu WY, Wu XD, Feng JX. Surgical treatment of pectus excavatum: 30 years 398 patients of experiences. J Pediatr Surg. 2008;43:1270–4.
Masaoka A, Kondo S, Sasaki S, Hara F, Mizuno T, Yamakawa Y, Kobayashi T, Fujii Y. Thirty years’ experience of open-repair surgery for pectus excavatum: development of a metal-free procedure. Eur J Cardiothorac Surg. 2012;41:329–34.
Nuss D, Kelly JR, Croitoru DPA. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998;33:542–52.
Schaarschmidt K, Kolberg-Schwerdt A, Dimitrov G, Srauss J. Submuscular bar: multiple bar fixation, bilateral thoracoscopy: a modified Nuss repair in adolescents. J Pediatr Surg. 2002;37:1276–80.
Park HJ, Jeong JY, Jo WM, Shin JS, Lee IS, Kim KT, Choi YH. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg. 2010;139:379–86.
Pilegaard HK, Licht PB. Can absorbable stabilizers be used routinely in the Nuss procedure? Eur J Cardiothorac Surg. 2009;35:561–4.
Harrison MR, Curran PF, Jamshidi R, Christensen D, Bratton BJ, Fechter R, Hirose S. Magnetic mini-mover procedure for pectus excavatum II: initial findings of a food and drug administration-sponsored trial. J Pediatr Surg. 2010;45:185–91.
Snel BJ, Spronk CA, Werker PM, van der Lei B. Pectus excavatum reconstruction with silicone implants: long-term results and a review of the English-language literature. Ann Plast Surg. 2009;62:205–9.
Michlits W, Windhofer C, Papp C. Pectus excavatum and free fasciocutaneous infragluteal flap: a new technique for the correction of congenital asymptomatic chest wall deformities in adults. Plast Reconstr Surg. 2009;124:1520–8.
Ravitch MM. Technical problems in the operative correction of pectus excavatum. Ann Surg. 1965;162:29–33.
Fonkalsrud EW. 912 open pectus excavatum repairs: changing trends, lessons learned: one surgeon’s experience. World J Surg. 2009;33:180–90.
Kelly Jr RE, Goretsky MJ, Obermeyer R, Kuhn MA, Redlinger R, Haney TS, Moskowitz A, Nuss D. Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg. 2010;252:1072–81.
Pilegaard HK, Licht PB. Early results following the Nuss operation for pectus excavatum—a single-institution experience of 383 patients. Interact Cardiovasc Thorac Surg. 2008;7:54–7.
Bouchard S, Hong AR, Gilchrist BF, Kuenzler KA. Catastrophic cardiac injuries encountered during the minimally invasive repair of pectus excavatum. Semin Pediatr Surg. 2009;18:66–72.
Aydemir B, Sokullu O, Hastaoglu O, Bilgen F, Celik M, Dogusoy I. Aorta-to-right ventricular fistula due to pectus bar migration. Thorac Cardiovasc Surg. 2011;59:51–2.
Jemielity M, Pawlak K, Piwkowski C, Dyszkiewicz W. Life-threatening aortic haemorrhage during pectus bar removal. Ann Thorac Surg. 2011;91:593–5.
Haecker FM, Berberich T, Mayr J, Gambazzi F. Near-fatal bleeding after transmyocardial ventricle lesion during removal of the pectus bar after the Nuss procedure. J Thorac Cardiovasc Surg. 2009;138:1240–1.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Saxena, A.K. (2017). Overview of Repair of Pectus Excavatum Type of Deformities. In: Saxena, A. (eds) Chest Wall Deformities. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53088-7_27
Download citation
DOI: https://doi.org/10.1007/978-3-662-53088-7_27
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53086-3
Online ISBN: 978-3-662-53088-7
eBook Packages: MedicineMedicine (R0)