Abstract
Epstein-Barr virus (EBV) infection is a common feature of B cell lymphoproliferative disorders (LPDs), including diffuse large B cell lymphoma. Approximately 10 % of DLBCLs are EBV-positive, with the highest incidence in immunocompromised and elderly patients. Here, we review the clinical, genetic, and pathologic characteristics of DLBCL and discuss the molecular role of EBV in lymphoma tumorigenesis. Using EBV-positive DLBCL of the elderly as a model, we describe the key features of EBV-positive DLBCL. Studies of EBV-positive DLBCL of the elderly demonstrate that EBV-positive DLBCL has a distinct biology, related to both viral and host factors. The pathogenic mechanisms noted in EBV-positive DLBCL of the elderly, including enhanced NFκB activity, are likely to be a generalizable feature of EBV-positive DLBCL. Therefore, we review how this information might be used to target the EBV or its host response for the development of novel treatment strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Epstein-Barr virus (EBV) has been linked to a wide number of human cancers. Among these neoplasms, B cell lymphoproliferative disorders (LPDs) are the most frequent and strongly associated. Diffuse large B cell lymphoma is the most common lymphoid malignancy in adults, accounting for nearly a third of non-Hodgkin’s lymphoma cases (NHL) globally (Fisher and Fisher 2004; Menon et al. 2012; Jemal et al. 2011).
DLBCL is characterized by rapidly proliferating cells expressing B cell-associated antigens CD19 , CD20, CD22, and CD79a (Martelli et al. 2013; Swerdlow et al. 2008). Despite these common features, DLBCL is a heterogeneous disease from the standpoints of biology and clinical outcome (Dave 2010). Prognosis reflects this heterogeneity, with long-term survival rates ranging between 30 and 90 %, dependent on clinical stage and disease subtype (Ziepert et al. 2010; Corti et al. 2010).
Roughly 10 % of DLBCLs are EBV-positive, with a significantly higher incidence in setting of immunocompromised and elderly patients (Heslop 2005). There are additional biological differences that distinguish EBV-positive DLBCLs from other DLBCLs, particularly the activation of the NF-kB and JAK /STAT signaling pathways (Montes-Moreno et al. 2012; Kato et al. 2014).
This chapter will review the challenges of classifying DLBCL, particularly with regard to EBV-positive lymphoid tumors. We will further review the clinical, genetic, and biological studies that have led to our current understanding of EBV-positive DLBCL. Finally, implications for these findings on treatment strategies and patient care will be considered.
2 Classification Challenges of DLBCL
The general organizing principles of DLBCL as it understood today were initially presented in the REAL classification of 1994, and were subsequently incorporated into the WHO classification (Menon et al. 2012) which is now the widely accepted standard. While these evolving classifications have provided a clearer categorization of these tumors, the diagnosis does not capture all the observed clinicopathologic heterogeneity that is commonly observed in the disease.
Significant effort has been dedicated to the subclassification of DLBCL into more clearly delineated disease entities (Swerdlow et al. 2008; Balague Ponz et al. 2008). Table 1 depicts the subtypes of DLBCL defined in the 2008 WHO classification. Details of each category, including cellular immunophenotype, cytogenetics, gene expression patterns, and EBV association, are provided. The complex subdivisions in this scheme highlight diverse characteristics such as anatomic location (DLBCL leg type), patient age (EBV-positive DLBCL of the elderly), and presence of viral coinfections (HHV8+ DLBCL arising in the setting of multicentric Castleman’s disease) (Swerdlow et al. 2008).
In addition to immunophenotyping and cytogenetics, microarray technology has provided new insight into molecular patterns of DLBCL through the examination of global gene expression alterations occurring in a given tumor. Gene expression profiling (GEP) of DLBCL tumors demonstrates that these tumors can be divided into two major subtypes based on their gene signatures (Alizadeh et al. 2000; Rosenwald et al. 2002; Lenz et al. 2008a). These two entities, germinal center B cell (GCB) and activated B cell (ABC), show distinct clinical behavior and treatment outcomes. The five-year overall survival of ABC and GCB DLBCL is 30 and 59 %, respectively (Lenz et al. 2008a). The complexity of processing and interpreting microarray data has restricted its global applicability and has thus far prevented GEP classification from being incorporating into the WHO classification (Balague Ponz et al. 2008). However, immunohistochemistry provides a useful surrogate to GEP (Hans et al. 2004; Choi et al. 2009). GEP surrogates are a reproducible, less expensive alternative to microarrays and have been widely adopted by pathologists. A combination of five immunohistochemical markers, GCTE1, CD10, BCL-6, IRF4, and FOXP1, predicted clinical outcome and achieved 90 % concordance with GEP (Choi et al. 2009).
GEP data suggest that most DLBCLs originate either during a B cell’s transit through the germinal center reaction (GCB type) or in post-germinal center B cells (ABC type) . Next-generation sequencing studies of DLBCL, including whole exome sequencing, genome copy number analysis, and RNA sequencing show that, in addition to having unique gene expression signatures, GCB and ABC tumors have different patterns of genetic mutation that likely reflect their distinct biology (Zhang et al. 2013; Morin et al. 2013; Pasqualucci et al. 2011). Distinct features of GCB and ABC DLBCL will be reviewed next.
Germinal centers (GCs) are transient structures that form in secondary lymphoid tissue in response to antigenic stimulation. During their passage through the GC, B cells undergo rapid proliferation, somatic hypermutation (SHM) of the variable chains of their immunoglobulin genes, class-switch recombination (CSR), and affinity selection (Victora and Nussenzweig 2012). The GC reaction is the process by which mature B cells are generated, and is thus absolutely critical to adaptive immunity. It is also a common site of lymphomagenesis. B cell transformation can occur during the GC reaction from the acquisition of mutations that either promote sustained proliferation or impair apoptosis. These mutations may be acquired during repeated cycle cellular replication or may result from off target effects of activation-induced cytidine deaminase (AID) , the enzyme that initiates the processes of SHM and CSR in GC B cells (Orthwein and Di Noia 2012).
Gene mutations that occur more frequently in GCB compared to ABC-type DLBCL include C-MYC, EZH2 , and GNA13 (Zhang et al. 2013). BCL2 translocations have also been identified in roughly one-quarter of GCB tumors (Schuetz et al. 2012). BCL2 activation protects cells from programmed cell death (Kroemer 1997). Chromosomal rearrangements involving C-MYC, or gain of function mutations, promote unregulated cellular proliferation in affected cells (Ott et al. 2013). Gain of function mutations in EZH2, a histone methyltransferase, promote lymphoma by silencing cell cycle regulation genes and tumor suppressor genes (Béguelin et al. 2013). Loss of function mutations in GNA13, a G protein involved in cell–cell adhesion, enhance AKT signaling and cellular motility and are strongly associated with GCB DLBCL (Morin et al. 2013; Muppidi et al. 2014).
In contrast to GCB DLBCL, ABC tumors have gene expression profiles similar to those seen in activated B cells (Lenz et al. 2008a). The hallmark of ABC biology is believed to be chronically active B cell receptor signaling, leading to upregulated NFκB activity (Davis et al. 2001; Lenz et al. 2008b). Gene expression profiling in primary tumor samples, as well as ABC lymphoma-derived cell lines, demonstrates enhanced expression of NFκB target genes (Bea et al. 2005; Rosenwald and Staudt 2003). Augmented NFκB activity is driven by activating mutations in signaling proteins downstream of the B cell receptor and/or Toll-like receptors. Common genetic defects in the ABC subtype of DLBCL include gain of function mutations in CD79B (B cell receptor), MyD88, MALT1, and Card11, all of which promote canonical NFκB activity (Zhang et al. 2013; Morin et al. 2013). A20 , a negative NFκB regulator, is subject to inactivating mutations (Kato et al. 2009). These events promote oncogenesis by enhancing cell proliferation and suppressing apoptotic signals. Constitutive NFκB activity may also explain the post-germinal center phenotype of ABC DLBCL. NFκB promotes enhanced expression of IRF4 (interferon regulatory factor-4), a transcription factor that drives the plasmablastic differentiation (Staudt 2010). Another important aspect of ABC biology is IL-6 and IL-10 generation. These cytokines exert autocrine effects on the tumor cells, resulting in the activation of STAT3 (Ding et al. 2008). A subset of DLBCL tumors have high STAT3 target gene expression and nuclear localization of phosphorylated STAT3. These tumors also demonstrate higher expression of NFκB target genes (Lam et al. 2008).
At a molecular level, constitutive NFκB activity is related to activating mutations in proteins upstream of NFκB. In B cells, CARD11, MALT1, and BCL10 form a signaling complex regulated by activation of the B cell receptor (Schulze-Luehrmann and Ghosh 2006). Upon antigen stimulation, cytoplasmic CARD11 is phosphorylated by PKCβ (Tan and Parker 2003). CARD11 is then recruited to the plasma membrane, where it serves as a molecular scaffold for the assembly of MALT1 and BCL10. This recruits the NFκB IKK complex, eventually leading to the activation of IKKβ. IKKβ is a kinase that phosphorylates the tonic NFκB inhibitor IκBα. The inhibitor then dissociates with NFκB subunits p50/p65, leaving them free to dimerize, translocate to the nucleus, and activate target genes (Staudt 2010). This process is critical for clonally expanding populations of antibody-producing B cells in response to an antigenic challenge. ABC tumors co-opt BCR signaling with activating mutations in CARD11 or CD79A /B (Lenz et al. 2008c; Davis et al. 2010). Unbound to antigenic stimulation, affected B cells are now capable of sustained NFκB activity. This leads to the enhanced proliferation and evasion of cell death, both hallmarks of cancer.
2.1 Disease Etiology
DLBCL usually occurs as a de novo malignancy, or less frequently through the “transformation” of an indolent B cell neoplasm, such as follicular lymphoma or chronic lymphocytic leukemia (CLL). In latter instance, acquisition of additional mutations results in transformation to a more aggressive neoplasm, often referred to as Richter’s transformation (Giles et al. 1998).
A causative agent is not identifiable for most cases of DLBCL, though there are a number of known risk factors associated with its development, including mutagens, toxins, immune dysfunction, and infections (Martelli et al. 2013). Chemical exposures including alkylating chemotherapeutics, industrial chemicals, pesticides, and fertilizers have been shown to increase a person’s risk of developing DLBCL (Fisher and Fisher 2004). This is due to the ability of these agents to mutagenize DNA. The high proliferation rate of hematopoietic cells renders them particularly vulnerable to these toxins.
Problems of immune dysregulation are common in patients with DLBCL (Smedby et al. 2006; Miranda et al. 2013). These include genetic and acquired causes of immunodeficiency, chronic inflammation, and autoimmune disease. The cause of this association is likely multifactorial, but T cell suppression resulting in impaired antitumor immunity is felt to play an important role (Yang et al. 2006). Immune suppression also permits the reactivation of lymphoma-associated viral pathogens, particularly EBV (Rickinson 2014).
Viral infections that increase the risk of DLBCL development include EBV, human immunodeficiency virus (HIV) , hepatitis C (HCV), and human herpesvirus-8(HHV8) (Rickinson 2014). Viral infections can increase the risk of lymphoma through diverse mechanisms. They can alter T cell suppressor function, such as in the case of HIV, which diminishes the body’s immune-mediated antitumor surveillance (Carbone and Gloghini 2005). Viruses can also promote lymphoma by driving B cell hyperstimulation, as is the case with EBV infection (discussed in detail below), HCV, and HHV8 (Rickinson 2014).
Environmental exposures, immune dysfunction, and infections can operate synergistically to promote mutagenesis, suppress T cell function, and activate B cell stimulation. The cumulative effects of these processes increase the likelihood of lymphoma development.
2.2 EBV and Lymphoma
Over 90 % of the world’s population is infected with EBV, though this infection is asymptomatic in the vast majority of individuals (Niederman et al. 1970). However, the oncogenic potential of EBV is undeniable, as it has been linked to a broad range of tumor subtypes, most of which are of B cell origin (De Martel et al. 2012). The addition of EBV to primary B cells grown in culture leads to growth transformation and the generation of immortalized lymphoblastoid B cell lines (Nilsson et al. 1971). B cell neoplasms linked to EBV infection include DLBCL, post-transplant lymphoproliferative disease (PTLD) , Burkitt lymphoma (BL), AIDS-related lymphoma (Primary CNS Lymphoma) , plasmablastic lymphoma, and primary effusion lymphoma . These tumors are characterized by malignant B cells that frequently express EBV transcripts and proteins indicating EBV infection.
In PTLD, rates of EBV infection range from 70 to 100 % and are related to the length and degree of immunosuppression (Juvonen et al. 2003; Taylor et al. 2005). In the HIV -positive population, 80 % of DLBCL is EBV-positive (Park et al. 2007) and 100 % of primary CNS lymphomas are EBV-positive (Swerdlow et al. 2008; Gloghini et al. 2013). Primary effusion and plasmablastic lymphomas, which mostly occur in HIV-positive patients, are also positive for EBV in most cases (Hsi et al. 2011; Verma et al. 2005). Immunosuppression is a common pathogenic cofactor in these B cell neoplasms, and the relevance of this association requires a discussion of EBV virology.
EBV is a gamma-1-type herpesvirus that first discovered fifty years ago in Burkitt lymphoma tumors from pediatric patients in equatorial Africa (Epstein et al. 1964). EBV is similar to other herpesviridae in its capacity to persist in a latent state in infected cells. It is distinctive from other herpesvirus genera in its restriction to primate hosts, its tropism for establishing latency in B lymphocytes, and its ability to promote oncogenic transformation of B lymphocytes through its latent gene expression repertoire (Rickinson 2014; Nilsson et al. 1971).
EBV infection in humans occurs in three distinct stages: lytic phase, latent phase, and reactivation. First, EBV enters a host by infecting the polarized respiratory epithelial cells of the nasopharynx. This initial infection is followed by the entry of EBV into the surrounding mucosal lymphoid cells through transcytosis, leading to infection of B cells. This initial lytic phase results in the cell death, sloughing of the respiratory epithelial cells and release of high titers of virus, a process that can also occur during viral reactivation (Lemon et al. 1977). During this phase, EBV binds to CD21 receptors on naive B lymphocytes (Carel et al. 1990). Once EBV infects a B lymphocyte, the expression of viral genes initially promotes growth transformation in the infected cell. Transformed B cells are then believed to transit though the germinal center reaction, differentiating into long-lived quiescent memory B cells (Thorley-Lawson and Gross 2004; Roughan and Thorley-Lawson 2009). At this stage, the viral genome persists in an episomal state, expressing only a limited number of viral antigens (Young and Rickinson 2004). This is the latent phase of infection.
The latent infection is often punctuated by brief periods of viral reactivation caused by perturbations in the EBV-infected memory B cell pool. EBV-positive memory B cells are thought to function similarly to other memory B cells. Thus, if a given cell encounters cognate antigen, it will awake from its resting state and undergo plasma cell differentiation. Plasma cell differentiation is a trigger of viral reactivation (Laichalk and Thorley-Lawson 2005). Reactivation is believed to occur as a result of the actions of XBP-1, a B cell transcription factor critical for plasma cell differentiation. XBP-1 is capable of activating the viral BZLF promoter, which controls the expression of viral lytic genes (Sun and Thorley-Lawson 2007). During this process, infected cells reinitiate the expression of viral antigens on their cell surface. In immunocompetent individuals, viral reactivation results in brisk humoral and cell-mediated immune responses (Jones and Straus 1987; Rickinson and Moss 1997). While antibodies to viral membrane proteins decrease viral shedding and infectivity, CD4 and CD8+ T cells are primarily responsible for suppressing lytic and latent EBV infections (Jones and Straus 1987). The immune system ensures that EBV-positive B cells that reactivate are promptly eliminated, thus re-establishing the steady state of latent infection. This is the usual cycle of EBV infection present in a normal, healthy individual.
Immunosuppressive states upset the virus–host balance by weakening the body’s principle defense against EBV reactivation: cell-mediated immunity. In the absence of the CD8+ T cell response, EBV-positive B cells are able to proliferate and express viral antigens. Hence, patients suffering from immune-deficient states associated with T cell dysfunction are particularly vulnerable to EBV reactivation. These include HIV infection and post-transplant immunodeficiency, where medication-induced T cell suppression is necessary to prevent graft rejection. Aging can also result in T cell dysfunction due to reduced numbers of CD4/8+ T cells and reduction in naïve T cell receptor diversity (Miller 1996). Immune senescence is defined as age-related immune alterations that result in increased infections, autoimmunity, cancer, and reduced response to prophylactic vaccines. Consistent with these observations, the incidence of polyclonal EBV-positive lymphoproliferative disease increases with age, as does the risk of DLBCL133. Figure 1 summarizes the effect of EBV on the pathogenesis of lymphoma formation.
The relationship of EBV to the pathogenesis of lymphoma. Naive B lymphocytes are infected with EBV and subsequently undergo transformation to memory cells via transit through the GC reaction. EBV establishes a latent infection in memory B cells. Upon memory B cell reactivation, EBV enters the lytic stage of infection, where it expresses viral antigens on the surface of the infected cell. In immune competent hosts (green), this activates cell-mediated immunity and the lytic phase cells are targeted for destruction. By contrast, immune compromise is associated with deficiency in cell-mediated immunity. In these individuals, EBV sets up a program of proliferation and increased cell survival which promotes polyclonal lymphocyte expansions or lymphoproliferative disease (red). Ongoing rounds of cellular division lead to the acquisition of additional mutations. If a sufficient number of oncogenic driver and tumor suppressor mutations are achieved, then lymphoma occurs
The oncogenic effect of EBV on B cells occurs through the action of a number of viral microRNAs and the protein LMP-1 (Rickinson 2014). EBV produces 44 viral microRNAs, which are believed to regulate viral and cellular mRNA during the latent phase of infection (Lopes et al. 2013). These noncoding RNAs promote cell growth and immune evasion and prevent the transcription of proapoptotic signaling molecules. LMP-1 is a well-studied viral oncogene that is believed to be the prime actor in EBV-mediated B cell transformation (Kaye et al. 1993).
LMP-1 is expressed during the latent and lytic phases of infection and is present in tumors corresponding to higher degrees of immune compromise (latency pattern II and III). LMP-1 is an integral membrane protein that behaves as a functional mimic of CD40 , a costimulatory receptor required for B cell activation (Uchida et al. 1999; Eliopoulos et al. 1997; Huen et al. 1995). Under physiologic conditions, helper T cells recognize antigens presented by B cells. During this interaction, the extracellular portion of CD40 binds its ligand on the T cell membrane. This activates CD40, inducing conformational shape changes that promote receptor oligomerization and nucleation of TRAF signaling proteins to its cytoplasmic domain (Tsubata et al. 1993). This leads to activation of canonical NFκB pathway signaling, cell cycle entry, and protection against apoptosis. Under normal conditions, these processes lead to adaptive immunity, resulting in the rapid generation of high affinity antibodies against foreign antigens. The viral LMP-1 protein co-opts this process by behaving as a constitutively active CD40 (Uchida et al. 1999). In doing so, LMP1 uncouples B cell activation from antigen selection and activates AICDA (activation-induced cytidine deaminase), and leads to polyclonal lymphocytosis and the acquisition of additional mutations that increase the likelihood of transformation into overt lymphoma.
Dependent on the degree of host immune compromise, transformed B cells may express all, or just a portion of the EBV latency genes (Tierney et al. 1994). Latency I pattern corresponds to the expression profile present in a typical active infection, latency II pattern is marked by the presence of a subset of viral antigens, and latency III pattern results in the expression of the entire EBV repertoire (Young and Murray 2003). There may also be a role for viral genetic variation in the efficiency of B cell transformation; however, this remains to be fully defined through a careful study of cases and controls. Latency patterns may be significant as they may reflect distinct aspects of tumor biology. Table 2 depicts the proteins associated with each latency pattern and shows the malignancies possessing each pattern. The EBV latency patterns associated with different DLBCL subsets are indicated in Table 1.
3 Clinical and Pathologic Aspects of EBV-Positive DLBCL
3.1 EBV-Positive DLBCL as a Disease Model
Much of our current understanding of the clinical impact of EBV in DLBCL comes from studies of EBV-positive DLBCL of the elderly. This DLBCL classification appeared first in the WHO classification of tumors in 2008 as a provisional entity (Swerdlow et al. 2008). EBV-positive DLBCL is defined as an EBV-positive monoclonal large B cell lymphoproliferation occurring in an immunocompetent patient greater than 50 years of age with no history of prior lymphoma. The age cutoff emphasizes the tendency of these tumors to arise in individuals of advanced age (Balague Ponz et al. 2008; Cho et al. 2008; Cohen et al. 2014), though EBV-positive DLBCL has been reported in younger immunocompetent patients, albeit rarely (Cohen et al. 2014; Ao et al. 2014; Beltran et al. 2011a). It is presently unclear whether elderly patients can be truly considered immune competent, and thus distinct from other EBV-positive DLBCL subtypes, or whether the EBV reactivation in these patients is due to age-related T cell dysfunction (Miller 1996). Regardless, compared to other EBV-positive DLBCL subtypes, EBV-positive DLBCL of the elderly is not associated with concomitant immunosuppression, or use of transplant rejection medications, HIV or HHV8 coinfection, secondary malignancies, or chronic inflammatory disease. For this reason, EBV-positive DLBCL of the elderly appears to be a good model for the study of how EBV affects DLBCL disease course and treatment response and it is instructive to review this disease entity in some detail.
3.2 Historical Perspective
EBV-positive DLBCL was initially described by Oyama et al. in 2003 as “senile EBV-positive lymphoproliferative disorder” (Oyama et al. 2003). In that case series of 22 Japanese patients, the authors described a spectrum of EBV-positive lymphoproliferative disease (LPD) ranging from polyclonal B cell lymphocytosis to DLBCL. Compared to EBV-negative LPD, patients with EBV-positive tumors had a higher rate of extranodal involvement, a more aggressive clinical course, frequent refractory disease or early relapse, and worse overall survival. Since this initial observation, groups in other countries have confirmed the existence of DLBCL patients with EBV-positive tumors and without known immunodeficiency (Gibson and Hsi 2009; Beltran et al. 2011; Hoeller et al. 2010; Hofscheier et al. 2011; Uner et al. 2011; Al-Humood et al. 2014). Consistent with the initial report, these EBV-positive immune competent individuals are almost exclusively elderly.
3.3 Epidemiology
Though there have been a number of studies assessing the prevalence rate of EBV positivity in DLBCL tumors from elderly, immune competent patients, the geographic prevalence of the disease appears variable. Groups from the USA and European countries have reported incidences <5 % (Gibson and Hsi 2009; Hoeller et al. 2010; Hofscheier et al. 2011) and some Asian and Latin American countries report rates as high as 10–15 % of DLBCLs (Beltran et al. 2011b; Hofscheier et al. 2011), implicating potential genetic polymorphisms, coinfections, or environmental factors in these geographic differences. However, some studies have demonstrated significant variability within the same geographic region (Wada et al. 2011), suggesting that there might be an additional confounding variable in the lack of standardized criteria for determining EBV positivity in clinical cases.
Laboratories use differing cutoffs for the percentage of antigen expressing cells necessary for a tumor to be deemed EBV-positive (20 % vs. 50 %) (Wada et al. 2011). Furthermore, sample processing is not uniform. For example, there are various methods for separating EBV-positive tumor cells from contaminating background cells (Ok et al. 2013) and these methods are not always applied consistently. Finally, there are different means of detecting EBV infection (EBER in situ hybridization or LMP-1 immunohistochemistry) that may affect the assay sensitivity. Universal standardization of EBV testing is needed before definitive conclusions about geographic variation of this disease can be made.
3.4 Clinical Characteristics
The median age for EBV-positive DLBCL is 71, with the greatest proportion (20–25 %) of cases occurring in patients greater than age 90 (Ok et al. 2013; Castillo et al. 2011). Initial descriptions of EBV-positive DLBCL of the elderly stressed that patients presented in later stage of the disease, measured by IPI and Ann Arbor stage, and possessed a high degree of extranodal involvement (Oyama et al. 2003, 2007). Extranodal extension to GI tract, lung, liver, skin, soft tissue and bone were described. However, later studies in North American patients showed that, similar to EBV-negative DLBCL, both nodal and extranodal disease sites are common (Gibson and Hsi 2009; Hoeller et al. 2010; Hofscheier et al. 2011). No distinguishing clinical features have been reliably associated with EBV positivity, except a trend toward higher Ann Arbor stage at presentation (Gibson and Hsi 2009).
Studies in Asia and Europe demonstrate that patients with EBV-positive DLBCL of the elderly respond poorly to treatment and have worse overall survival compared to those with EBV-negative tumors (Park et al. 2007; Hofscheier et al. 2011; Oyama et al. 2007; Chang et al. 2014). Age, by itself, is a risk for poorer outcomes in DLBCL. However, EBV-positive DLBCL is also associated with an ABC GEP, which is known to have a worse outcome than GCB tumors (Kato et al. 2014; Ok et al. 2014). Montes-Moreno et al. (2012) explored whether the difference in survival was merely due to a higher prevalence of ABC phenotype. They compared elderly patients with either EBV-positive DLBCL or EBV-negative DLBCL stratified by ABC versus GCB GEP and found that EBV positivity conferred a worse outcome than ABC subtype alone, suggesting that EBV is an independent risk factor for poor outcome.
One caveat to the survival studies is that most patients were treated prior to the time when rituximab, a monoclonal antibody directed against CD20, became a standard addition to chemotherapy regimens targeting B cell lymphoma. A study performed on DLBCL patients treated with R-CHOP demonstrated no survival difference between EBV-positive and EBV-negative patients, suggesting that rituximab alone may overcome the survival difference noted in previous reports (Montes-Moreno et al. 2012). The possibility of rituximab having activity in EBV-positive DLBCL is not unexpected, since rituximab monotherapy effectively eliminates the majority of mature B cells and is a highly effective treatment for EBV-positive PTLD (Taylor et al. 2005). More studies are needed to clarify the impact of rituximab on the clinical outcomes of this lymphoma.
3.5 Histopathology
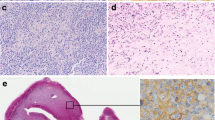
EBV-positive DLBCLs typically demonstrate an effacement of nodal and extranodal tissue architecture by large, rapidly proliferating immunoblasts with interdispersed areas of geographic necrosis (Al-Humood et al. 2014; Oyama et al. 2007; Dojcinov et al. 2011). The cellular makeup of the tumor is variable, with both polymorphic and monomorphic subtypes described. Polymorphic tumors display numerous reactive cells, including histiocytes, plasma cells , and normal lymphocytes intermingled with malignant large cells. The monomorphic subtype is characterized by sheets of uniform-appearing large cells with minimal reactive component. Both entities may contain Reed–Sternberg cells (Oyama et al. 2007), which are commonly present in Hodgkin’s lymphoma, another B cell tumor associated with EBV. Despite differing appearances, histological subtypes do not have prognostic significance (Oyama et al. 2007).
The immunophenotype of EBV-positive DLBCL is that of an aggressive B cell tumor of post-germinal center origin. Malignant cells are typically positive for B cell markers CD19 , CD20, CD79a , and PAX-5. Ki67, a marker of proliferation, is usually present in greater than 50 % of tumor cells (Swerdlow et al. 2008; Montes-Moreno et al. 2012; Al-Humood et al. 2014). Using immunohistochemical markers, post-germinal center (ABC-associated) proteins IRF4 , MUM1, are typically positive. GC markers CD10 and BCL6 are usually negative (Montes-Moreno et al. 2012). In comparison with Reed–Sternberg cells found in Hodgkin’s lymphoma, CD15 immunostaining of the neoplastic cells in EBV-positive DLBCL is negative, though most specimens (50–89 %) are CD30 positive (Montes-Moreno et al. 2012).
EBV positivity is measured either by fluorescent in situ hybridization of the EBER RNA (Chang et al. 1992) or by immunohistochemical detection of the LMP-1 protein (Gulley 2001). The expression of EBV latency genes in EBV-positive DLBCL reveals EBNA-1 and LMP-1 expression in >90 % of tumors, and 28 % positive for EBNA2, which is consistent with a viral latency II or III pattern, similar to that seen in PTLD (Oyama et al. 2003; Hofscheier et al. 2011; Oyama et al. 2007; Nguyen-Van et al. 2011; Shimoyama et al. 2008).
3.6 Genetics
Cytogenetic and FISH studies in tumors from EBV-positive DLBCL of the elderly have revealed no characteristic abnormalities (Al-Humood et al. 2014). Chromosomal translocations involving the heavy chain locus occur in approximately 15 % of samples (Montes-Moreno et al. 2012). Cytogenetic alterations have been reported, including copy number gains of the C-MYC, BCL2 , and BCL6 loci (Dojcinov et al. 2011). Al-Humood et al. (2014) reported that the mean total number of chromosomal alternations per case was less than that seen for EBV-negative disease. This suggests that the EBV itself, rather than acquired mutations, may be driving the pathogenesis of infected tumor cells.
B cell clonality in EBV-positive DLBCL is common, as measured by PCR of VH-JH rearrangements in the Ig locus. Most patients demonstrate light chain restriction by Kappa and Lambda immunostaining (Al-Humood et al. 2014). The EBV genomes of these specimens also demonstrate clonality, as evidenced by FISH probes design to detect the EBV terminal repeat regions (Oyama et al. 2007).
There is also a high incidence of T cell clonality in EBV-positive DLBCL patients, with 24 % of cases demonstrating monoclonality in at least one TCR-gamma gene (Oyama et al. 2007). The significance of this finding is unclear, however, since clonal T cells have also been demonstrated in many healthy elderly individuals. Some reports show a prevalence of T cell clones greater than 80 % in asymptomatic patients over the age of 75 years (Hadrup et al. 2006). These clones are believed to reflect the reduction of T cell diversity inherent to age-related immune senescence.
3.7 Biology
EBV-positive DLBCL is associated with ABC phenotype, which is characterized by upregulated NFκB signaling (Staudt 2010). In 2012, Montes Moreno et al. assessed the state of NFκB activation in EBV-positive DLBCL tumors by Western blot analysis and subcellular localization of classical NFκB subunits p105/p50 and alternative pathway subunits p100/p52 (Montes-Moreno et al. 2012). They found nuclear localization of these factors in 79 and 74 % of tumors, respectively. Over half of tumors demonstrated nuclear expression of both canonical and alternative NFκB pathways, significantly greater NFκB activity than that seen in ABC lymphoma alone. Furthermore, Kato et al. (2014) found that infecting human ABC DLBCL-derived cell lines with EBV enhanced NFκB activity measured by electrophoretic mobility shift assay.
There is only one report of gene expression profiling for EBV-positive DLBCL thus far. Kato et al. (2014) studied a total of 61 patients meeting criteria for the diagnosis of EBV-positive DLBCL of the elderly and compared these tumors to 36 EBV-negative DLBCL specimens. The authors found that immune and inflammatory gene pathways are highly expressed in EBV-positive DLBCL of the elderly, including NFκB, JAK /STAT , NOD receptor, and Toll-like receptor signaling pathways. Expression analysis of the transcriptional targets of NFκB and STAT3 signaling revealed that these pathways are overactive in EBV-positive tumors. The authors went on to evaluate the effect of EBV status on the subset of ABC tumors. They found that NFκB and STAT3 expression gene sets were enriched in EBV-positive tumors. Finally, the authors evaluated other EBV-positive lymphoma subtypes to determine whether EBV positivity promoted NFκB and JAK/STAT signaling in other tumor types. NFκB target gene enrichment was the characteristic of HIV- associated DLBCL, EBV-positive Hodgkin’s lymphoma, and NK cell lymphoma , whereas the STAT3 signature was only associated with B cell lymphoma subtypes. These data suggest that NFκB and STAT3 activity may be defining features of EBV pathogenesis as it relates to lymphoma.
4 Novel Treatment Approaches for EBV-Positive DLBCL
Recent insights into the biology of EBV-positive DLBCL of the elderly have revealed the distinct biology of B cell lymphomas that arise in the setting of EBV infection. Further, there are many reports suggesting that patients with EBV-positive lymphoma have worse prognosis than their EBV-negative counterparts. For these reasons, new treatments are needed to address the unique pathogenesis of this disorder. Possible therapeutic approaches include the following: antiviral strategies, EBV-targeted adoptive immunotherapy, and/or agents that target the NFκB or STAT3 signaling pathways.
4.1 Antiviral Therapy
Antiviral drugs offer clear potential for the treatment of EBV-positive lymphoma. There are other lymphoma subtypes that have previously demonstrated response to iradication of an associated microorganism. Gastric MALT (mucosa-associated lymphoma) is an extranodal marginal zone lymphoma that is highly associated with Helicobacter pylori infection and can be effectively treated with antibiotics in 70 % of patients (Bayerdörffer et al. 1995). Owing to its potential for latent infection in resting B cells, EBV is a less straightforward treatment target than H. pylori. Treatment of EBV with antiviral medications would first require activation of the virus into the lytic phase of infection. Known EBV lytic phase inducers include DNA methylase transferase inhibitors, HDAC inhibitors, and chemotherapeutics (Feng et al. 2004). Recently, HDAC inhibitors panobinostat and vorinostat have demonstrated potent induction of EBV lytic genes in cell lines (Ghosh et al. 2012), as well as activity in EBV-associated lymphoma (Piekarz et al. 2011; Younes 2009). Induction therapy with an EBV lytic phase inducing agent, followed by EBV antiviral therapy, would provide a potential solution to the latency issue.
4.2 EBV-Targeted Adoptive Immunotherapy
EBV-targeted adoptive immunotherapy is a strategy in which T cells isolated from a patient’s peripheral blood are expanded in vitro and activated by exposure to EBV-specific antigens. These cells are then re-introduced into the patient, where they colonize tissues and attack lymphoma cells expressing EBV antigens (Gattinoni et al. 2006). Adoptive transfer of EBV-specific CD8+ T cells in solid organ transplant recipients has been undertaken successfully (Sherritt et al. 2003). Adoptive immunotherapy used in combination with DLBCL chemotherapy regimens may result in improved response compared to chemotherapy alone for patients with EBV-postive DLBCL.
4.3 Biology of Targeted Therapies
The NFκB and JAK /STAT pathways are attractive therapeutic targets in EBV-positive DLBCL. If given in combination with traditional DLBCL regimens, targeted agents may mitigate the survival differences seen between EBV-positive and EBV-negative tumors. Therapeutic strategies that directly inhibit NFκB signaling have been fraught with difficulties. NFκB is critical to physiologic processes in many cells. Deficiency in genes IKKβ and p65 provokes massive hepatocyte apoptosis during development (Strnad and Burke 2007). Adult hepatocytes are less perturbed by reductions in these proteins, but still show high sensitivity to toxin and cytokine-related injury. It is still possible that these inhibitors could be useful in tumors that are highly reliant on NFκB activity and provided that the appropriate concentration of inhibitor can be achieved. Bortezomib is a proteasome inhibitor that is capable of inhibiting both canonical and noncanonical NFκB signaling (Staudt 2010). Bortezomib is widely used in the treatment of multiple myeloma as is well tolerated both alone and in combination with other agents. Bortezomib suppresses NFκB activation by degrading IαBα, an inhibitor of NFκB nuclear translocation. Bortezomib is cytotoxic to human EBV-infected lymphoblastoid cell lines (Zou et al. 2007). Drugs that target JAK /STAT signaling would also be of potential therapeutic benefit to EBV-positive DLBCL. At present, there is much interest in the development of potent, selective STAT3 inhibitors for the treatment of lymphoid malignancies.
5 Conclusions
In this chapter, the clinical, genetic, and pathologic characteristics of DLBCL were presented, followed by an explanation of the role of EBV in DLBCL tumorigenesis. Using EBV-positive DLBCL of the elderly as a model, we describe the key clinical and pathologic characteristics of EBV-positive DLBCL. We also discussed the recent insights into EBV-positive lymphoma biology and potential treatment strategies.
Studies of EBV-positive DLBCL of the elderly have provided key insight into the pathogenic role that EBV plays in DLBCL. These data demonstrate that EBV-positive DLBCL has a distinct tumor biology, which is related to the tenuous relationship that the EBV virus establishes with its B cell host. The pathogenic mechanisms noted in EBV-positive DLBCL of the elderly, including enhanced NFκB activity, are likely to play a role in all forms of EBV-positive DLBCL.
More work is needed to determine whether EBV-positive DLBCLs occurring in distinct contexts of immune dysfunction are biologically different tumors. The current WHO classification scheme includes subgroups for plasmablastic DLBCL, DLBCL associated with chronic inflammation, and EBV-positive DLBCL of the elderly, all of which are EBV-positive DLBCL tumors. It would be interesting and informative to compare gene expression profiles from these subtypes to see whether they are similar. If EBV is contributing to the tumor pathogenesis in each case, the other subtypes may also demonstrate marked NFκB and JAK /STAT activation. This work would confirm that EBV-positive DLBCL has a unique biology and provide new clues to treating this disease by methods that disrupt the life cycle of EBV viral infection or the signaling pathways induced in these tumors.
References
Addis B, Isaacson P (1986) Large cell lymphoma of the mediastinum: a B-cell tumour of probable thymic origin. Histopathology 10:379–390
Al-Humood S, Alqallaf A, Al-Shemmari S, Al-Faris L, Al-Ayadhy B (2014) Genetic and immunohistochemical characterization of Epstein-Barr virus-associated diffuse large B-cell lymphoma. Acta Haematol 131:1–10
Alizadeh AA et al (2000) Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature 403:503–511
Ao Q, Wang Y, Xu S, Tian Y, Huang W (2014) A case of EBV positive diffuse large B-cell lymphoma of the adolescent. Int J Clin Exp Med 7:307–311
Balague Ponz O et al (2009) Commentary on the WHO classification of tumors of lymphoid tissues (2008): aggressive B-cell lymphomas. J Hematop 2:83–87
Bayerdörffer E et al (1995) Regression of primary gastric lymphoma of mucosa-associated lymphoid tissue type after cure of Helicobacter pylori infection. The Lancet 345:1591–1594
Bea S et al (2005) Diffuse large B-cell lymphoma subgroups have distinct genetic profiles that influence tumor biology and improve gene-expression-based survival prediction. Blood 106:3183–3190
Béguelin W et al (2013) EZH2 is required for germinal center formation and somatic EZH2 mutations promote lymphoid transformation. Cancer Cell 23:677–692
Beltran BE et al (2011a) EBV-positive diffuse large B-cell lymphoma in young immunocompetent individuals. Clin Lymphoma Myeloma Leuk 11:512–516
Beltran BE et al (2011b) EBV-positive diffuse large B-cell lymphoma of the elderly: a case series from Peru. Am J Hematol 86:663–667
Capello D et al (2010) Genome wide DNA-profiling of HIV-related B-cell lymphomas. Br J Haematol 148:245–255
Carbone A, Gloghini A (2005) AIDS-related lymphomas: from pathogenesis to pathology. Br J Haematol 130:662–670
Carel J, Myones B, Frazier B, Holers VM (1990) Structural requirements for C3d, g/Epstein-Barr virus receptor (CR2/CD21) ligand binding, internalization, and viral infection. J Biol Chem 265:12293–12299
Castillo J, Pantanowitz L, Dezube BJ (2008) HIV-associated plasmablastic lymphoma: Lessons learned from 112 published cases. Am J Hematol 83:804–809
Castillo JJ et al (2011) Epstein-barr virus-positive diffuse large B-cell lymphoma of the elderly: what we know so far. Oncologist 16:87–96
Cazals-Hatem D et al (1996) Primary mediastinal large B-cell lymphoma: A clinicopathologic study of 141 cases compared with 916 nonmediastinal large B-cell lymphomas, a GELA (“Groupe d’Etude des Lymphomes de l’Adulte”) study. Am J Surg Pathol 20:877–888
Chang KL, Chen Y-Y, Shibata D, Weiss LM (1992) Description of an in situ hybridization methodology for detection of Epstein-Barr virus RNA in paraffin-embedded tissues, with a survey of normal and neoplastic tissues. Diagn Mol Pathol 1:246–255
Chang ST et al (2014) Epstein-Barr virus is rarely associated with diffuse large B cell lymphoma in Taiwan and carries a trend for a shorter median survival time. J Clin Pathol 67:326–332
Cho EY et al (2008) The spectrum of Epstein-Barr virus-associated lymphoproliferative disease in Korea: incidence of disease entities by age groups. J Korean Med Sci 23:185–192
Choi WW et al (2009) A new immunostain algorithm classifies diffuse large B-cell lymphoma into molecular subtypes with high accuracy. Clin Cancer Res Off J Am Assoc Cancer Res 15:5494–5502
Cohen M et al (2014) Epstein-Barr virus-positive diffuse large B-cell lymphoma association is not only restricted to elderly patients. Int J Cancer
Corti M et al (2010) AIDS related lymphomas: histopathological subtypes and association with Epstein Barr virus and human herpes virus type-8. Medicina 70:151–158
Dave SS (2010) Host factors for risk and survival in lymphoma. In: ASH Education Program Book, pp. 255–258
Davis RE, Brown KD, Siebenlist U, Staudt LM (2001) Constitutive nuclear factor κB activity is required for survival of activated B cell-like diffuse large B cell lymphoma cells. J Exp Med 194:1861–1874
Davis RE et al (2010) Chronic active B-cell-receptor signalling in diffuse large B-cell lymphoma. Nature 463:88–92
De Martel C et al (2012) Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol 13:607–615
Ding BB et al (2008) Constitutively activated STAT3 promotes cell proliferation and survival in the activated B-cell subtype of diffuse large B-cell lymphomas. Blood 111:1515–1523
Dojcinov SD et al (2011) Age-related EBV-associated lymphoproliferative disorders in the Western population: a spectrum of reactive lymphoid hyperplasia and lymphoma. Blood 117:4726–4735
Eliopoulos AG et al (1997) Epstein-Barr virus-encoded LMP1 and CD40 mediate IL-6 production in epithelial cells via an NF-κB pathway involving TNF receptor-associated factors. Oncogene 14:2899–2916
Epstein MA, Achong BG, Barr YM (1964) Virus particles in cultured lymphoblasts from Burkitt’s lymphoma. The Lancet 283:702–703
Feng W-H, Hong G, Delecluse H-J, Kenney SC (2004) Lytic induction therapy for Epstein-Barr virus-positive B-cell lymphomas. J Virol 78:1893–1902
Fisher SG, Fisher RI (2004) The epidemiology of non-Hodgkin’s lymphoma. Oncogene 23:6524–6534
Franke S et al (2002) Comparative genomic hybridization pattern distinguishes T-cell/histiocyte-rich B-cell lymphoma from nodular lymphocyte predominance Hodgkin’s lymphoma. Am J Pathol 161:1861–1867
Gattinoni L, Powell DJ, Rosenberg SA, Restifo NP (2006) Adoptive immunotherapy for cancer: building on success. Nat Rev Immunol 6:383–393
Ghosh SK, Perrine SP, Williams RM, Faller DV (2012) Histone deacetylase inhibitors are potent inducers of gene expression in latent EBV and sensitize lymphoma cells to nucleoside antiviral agents. Blood 119:1008–1017
Gibson SE, Hsi ED (2009) Epstein-Barr virus-positive B-cell lymphoma of the elderly at a United States tertiary medical center: an uncommon aggressive lymphoma with a nongerminal center B-cell phenotype. Hum Pathol 40:653–661
Giles FJ, O’Brien SM, Keating MJ (1998) Chronic lymphocytic leukemia in (Richter’s) transformation. Semin Oncol 25:117–125
Gloghini A, Dolcetti R, Carbone A (2013) Lymphomas occurring specifically in HIV-infected patients: from pathogenesis to pathology. Semin Cancer Biol 23:457–467
Gulley ML (2001) Molecular diagnosis of Epstein-Barr virus-related diseases. J Mol Diagn 3:1–10
Hadrup SR et al (2006) Longitudinal studies of clonally expanded CD8 T cells reveal a repertoire shrinkage predicting mortality and an increased number of dysfunctional cytomegalovirus-specific T cells in the very elderly. J Immunol 176:2645–2653
Hans CP et al (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103:275–282
Heslop HE (2005) Biology and treatment of Epstein-Barr virus-associated non-Hodgkin lymphomas. In: Hematology/The Education Program of the American Society of Hematology. American Society of Hematology. Education Program, pp 260–266
Hoeller S, Tzankov A, Pileri SA, Went P, Dirnhofer S (2010) Epstein-Barr virus–positive diffuse large B-cell lymphoma in elderly patients is rare in Western populations. Hum Pathol 41:352–357
Hofscheier A et al (2011) Geographic variation in the prevalence of Epstein-Barr virus-positive diffuse large B-cell lymphoma of the elderly: a comparative analysis of a Mexican and a German population. Mod Pathol 24:1046–1054
Hsi ED, Lorsbach RB, Fend F, Dogan A (2011) Plasmablastic lymphoma and related disorders. Am J Clin Pathol 136:183–194
Huen D, Henderson S, Croom-Carter D, Rowe M (1995) The Epstein-Barr virus latent membrane protein-1 (LMP1) mediates activation of NF-κB and cell surface phenotype via two effector regions in its carboxy-terminal cytoplasmic domain. Oncogene 10:549–560
Igarashi M, Kawaguchi Y, Hirai K, Mizuno F (2003) Physical interaction of Epstein-Barr virus (EBV) nuclear antigen leader protein (EBNA-LP) with human oestrogen-related receptor 1 (hERR1): hERR1 interacts with a conserved domain of EBNA-LP that is critical for EBV-induced B-cell immortalization. J General Virol 84:319–327
Jemal A et al (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Jones JF, Straus SE (1987) Chronic epstein-barr virus infection. Annu Rev Med 38:195–209
Juvonen E et al (2003) High incidence of PTLD after non-T-cell-depleted allogeneic haematopoietic stem cell transplantation as a consequence of intensive immunosuppressive treatment. Bone Marrow Transplant 32:97–102
Kato M et al (2009) Frequent inactivation of A20 in B-cell lymphomas. Nature 459:712–716
Kato H et al (2014) Gene expression profiling of Epstein-Barr virus-positive diffuse large B-cell lymphoma of the elderly reveals alterations of characteristic oncogenetic pathways. Cancer Sci 105:537–544
Kaye KM, Izumi KM, Kieff E (1993) Epstein-Barr virus latent membrane protein 1 is essential for B-lymphocyte growth transformation. Proc Natl Acad Sci 90:9150–9154
Kroemer G (1997) The proto-oncogene Bcl-2 and its role in regulating apoptosis. Nat Med 3:614–620
Laichalk LL, Thorley-Lawson DA (2005) Terminal differentiation into plasma cells initiates the replicative cycle of Epstein-Barr virus in vivo. J Virol 79:1296–1307
Lam LT et al (2008) Cooperative signaling through the signal transducer and activator of transcription 3 and nuclear factor-κB pathways in subtypes of diffuse large B-cell lymphoma. Blood 111:3701–3713
Lenz G et al (2008a) Stromal gene signatures in large-B-cell lymphomas. N Engl J Med 359:2313–2323
Lenz G et al (2008b) Molecular subtypes of diffuse large B-cell lymphoma arise by distinct genetic pathways. Proc Natl Acad Sci USA 105:13520–13525
Lenz G et al (2008c) Oncogenic CARD11 mutations in human diffuse large B cell lymphoma. Science 319:1676–1679
Lemon SM, Hutt LM, Shaw JE, Li, J-LH, Pagano JS (1977) Replication of EBV in epithelial cells during infectious mononucleosis
Lim MS et al (2002) T-cell/histiocyte-rich large B-cell lymphoma: a heterogeneous entity with derivation from germinal center B cells. Am J Surg Pathol 26:1458–1466
Loong F et al (2010) Diffuse large B-cell lymphoma associated with chronic inflammation as an incidental finding and new clinical scenarios. Mod Pathol 23:493–501
Lopes LF et al (2013) Epstein-Barr virus (EBV) microRNAs: involvement in cancer pathogenesis and immunopathology. Int Rev Immunol 32:271–281
Martelli M et al (2013) Diffuse large B-cell lymphoma. Critical Rev Oncol Hematol 87:146–171
Menon MP, Pittaluga S, Jaffe ES (2012) The histological and biological spectrum of diffuse large B-cell lymphoma in the World Health Organization classification. Cancer J (Sudbury, Mass.) 18:411–420
Miller RA (1996) The aging immune system: primer and prospectus. Science 273:70–74
Miranda RN, Khoury JD, Medeiros LJ (2013) Lymphoproliferative disorders associated with primary immune disorders. Atlas Lymph Node Pathol 383–397
Montes-Moreno S et al (2012) EBV-positive diffuse large B-cell lymphoma of the elderly is an aggressive post-germinal center B-cell neoplasm characterized by prominent nuclear factor-kB activation. Mod Pathol 25:968–982
Morin RD et al (2013) Mutational and structural analysis of diffuse large B-cell lymphoma using whole-genome sequencing. Blood 122:1256–1265
Muppidi JR et al (2014) Loss of signalling via Galpha13 in germinal centre B-cell-derived lymphoma. Nature
Murase T et al (2007) Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood 109:478–485
Nakatsuka S-I et al (2002) Pyothorax-associated lymphoma: a review of 106 cases. J Clin Oncol 20:4255–4260
Narimatsu H et al (2007) Clinicopathological features of pyothorax-associated lymphoma; a retrospective survey involving 98 patients. Ann Oncol 18:122–128
Nguyen-Van D et al (2011) Epstein-Barr virus-positive diffuse large B-cell lymphoma of the elderly expresses EBNA3A with conserved CD8 T-cell epitopes. Am J Blood Res 1:146–159
Niederman J, Evans A, Subrahmanyan L, McCollum R (1970) Prevalence, incidence and persistence of EB virus antibody in young adults. N Engl J Med 282:361–365
Nilsson K, Klein G, Henle W, Henle G (1971) The establishment of lymphoblastoid lines from adult and fetal human lymphoid tissue and its dependence on EBV. Int J cancer 8:443–450
Ok CY, Papathomas TG, Medeiros LJ, Young KH (2013) EBV-positive diffuse large B-cell lymphoma of the elderly. Blood 122:328–340
Ok CY et al (2014) Prevalence and clinical implications of epstein-barr virus infection in de novo diffuse large B-cell lymphoma in Western countries. Clin Cancer Res Off J Am Assoc Cancer Res 20:2338–2349
Orthwein A, Di Noia JM (2012) Activation induced deaminase: how much and where? Semin Immunol 24:246–254
Ott G, Rosenwald A, Campo E (2013) Understanding MYC-driven aggressive B-cell lymphomas: pathogenesis and classification. Blood 122:3884–3891
Oyama T et al (2003) Senile EBV+ B-cell lymphoproliferative disorders: a clinicopathologic study of 22 patients. Am J Surg Pathol 27:16–26
Oyama T et al (2007) Age-related EBV-associated B-cell lymphoproliferative disorders constitute a distinct clinicopathologic group: a study of 96 patients. Clin Cancer Res Off J Am Assoc Cancer Res 13:5124–5132
Park S et al (2007) The impact of Epstein-Barr virus status on clinical outcome in diffuse large B-cell lymphoma. Blood 110:972–978
Pasqualucci L et al (2011) Analysis of the coding genome of diffuse large B-cell lymphoma. Nat Genet 43:830–837
Piekarz RL et al (2011) Phase 2 trial of romidepsin in patients with peripheral T-cell lymphoma. Blood 117:5827–5834
Pittaluga S, Jaffe ES (2010) T-cell/histiocyte-rich large B-cell lymphoma. Haematologica 95:352–356
Ponzoni M et al (2007) Definition, diagnosis, and management of intravascular large B-cell lymphoma: proposals and perspectives from an international consensus meeting. J Clin Oncol 25:3168–3173
Rickinson AB (2014) Co-infections, inflammation and oncogenesis: future directions for EBV research. Semin Cancer Biol 26:99–115
Rickinson AB, Moss DJ (1997) Human cytotoxic T lymphocyte responses to Epstein-Barr virus infection. Annu Rev Immunol 15:405–431
Rosenwald A, Staudt LM (2003) Gene expression profiling of diffuse large B-cell lymphoma. Leuk Lymphoma 44(Suppl 3):S41–S47
Rosenwald A et al (2002) The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med 346:1937–1947
Roughan JE, Thorley-Lawson DA (2009) The intersection of Epstein-Barr virus with the germinal center. J Virol 83:3968–3976
Schuetz JM et al (2012) BCL2 mutations in diffuse large B-cell lymphoma. Leukemia 26:1383–1390
Schulze-Luehrmann J, Ghosh S (2006) Antigen-receptor signaling to nuclear factor κB. Immunity 25:701–715
Sherritt MA et al (2003) Reconstitution of the latent T-lymphocyte response to Epstein-Barr virus is coincident with long-term recovery from posttransplant lymphoma after adoptive immunotherapy. Transplantation 75:1556–1560
Shimoyama Y et al (2008) Age-related Epstein-Barr virus-associated B-cell lymphoproliferative disorders: special references to lymphomas surrounding this newly recognized clinicopathologic disease. Cancer Sci 99:1085–1091
Smedby KE et al (2006) Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst 98:51–60
Staudt LM (2010) Oncogenic activation of NF-κB. Cold Spring Harb Perspect Biol 2:a000109
Stein H, Lennert K, Feller AC (1984) Immunohistological analysis of human lymphoma: correlation of histological and immunological categories. Adv Cancer Res 42:67–147
Strnad J, Burke JR (2007) IκB kinase inhibitors for treating autoimmune and inflammatory disorders: potential and challenges. Trends Pharmacol Sci 28:142–148
Sun CC, Thorley-Lawson DA (2007) Plasma cell-specific transcription factor XBP-1 s binds to and transactivates the Epstein-Barr virus BZLF1 promoter. J Virol 81:13566–13577
Swerdlow SH, Campo E, Harris NL et al (2008) WHO classification of tumours of haematopoetic and lymphoid tissues, 4th edn. IARC Press, Lyon
Tan S, Parker P (2003) Emerging and diverse roles of protein kinase C in immune cell signalling. Biochem J 376:545–552
Taylor AL, Marcus R, Bradley JA (2005) Post-transplant lymphoproliferative disorders (PTLD) after solid organ transplantation. Crit Rev Oncol Hematol 56:155–167
Thorley-Lawson DA, Gross A (2004) Persistence of the Epstein-Barr virus and the origins of associated lymphomas. N Engl J Med 350:1328–1337
Tierney R, Steven N, Young L, Rickinson A (1994) Epstein-Barr virus latency in blood mononuclear cells: analysis of viral gene transcription during primary infection and in the carrier state. J Virol 68:7374–7385
Tsubata T, Wu J, Honjo T (1993) B-cell apoptosis induced by antigen receptor crosslinking is blocked by a T-cell signal through CD40
Uchida J et al (1999) Mimicry of CD40 signals by Epstein-Barr virus LMP1 in B lymphocyte responses. Science 286:300–303
Uner A et al (2011) The presence of Epstein-Barr virus (EBV) in diffuse large B-cell lymphomas (DLBCLs) in Turkey: special emphasis on ‘EBV-positive DLBCL of the elderly’. APMIS : acta pathologica, microbiologica, et immunologica Scandinavica 119:309–316
Valera A et al (2010) IG/MYC rearrangements are the main cytogenetic alteration in plasmablastic lymphomas. Am J Surg Pathol 34:1686
Verma S et al (2005) Epstein-Barr virus- and human herpesvirus 8-associated primary cutaneous plasmablastic lymphoma in the setting of renal transplantation. J Cutan Pathol 32:35–39
Victora GD, Nussenzweig MC (2012) Germinal centers. Annu Rev Immunol 30:429–457
Wada N et al (2011) Epstein-barr virus in diffuse large B-Cell lymphoma in immunocompetent patients in Japan is as low as in Western Countries. J Med Virol 83:317–321
Yang Z-Z, Novak AJ, Stenson MJ, Witzig TE, Ansell SM (2006) Intratumoral CD4+ CD25+ regulatory T-cell-mediated suppression of infiltrating CD4+ T cells in B-cell non-Hodgkin lymphoma. Blood 107:3639–3646
Younes A (2009) Novel treatment strategies for patients with relapsed classical Hodgkin lymphoma. ASH Education Program Book 2009:507–519
Young LS, Murray PG (2003) Epstein-Barr virus and oncogenesis: from latent genes to tumours. Oncogene 22:5108–5121
Young LS, Rickinson AB (2004) Epstein-Barr virus: 40 years on. Nat Rev Cancer 4:757–768
Zhang J et al (2013) Genetic heterogeneity of diffuse large B-cell lymphoma. Proc Natl Acad Sci USA 110:1398–1403
Ziepert M et al (2010) Standard International prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clini Oncol Off J Am Soc Clin Oncol 28:2373–2380
Zou P, Kawada J, Pesnicak L, Cohen JI (2007) Bortezomib induces apoptosis of Epstein-Barr virus (EBV)-transformed B cells and prolongs survival of mice inoculated with EBV-transformed B cells. J Virol 81:10029–10036
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Healy, J.A., Dave, S.S. (2015). The Role of EBV in the Pathogenesis of Diffuse Large B Cell Lymphoma. In: Münz, C. (eds) Epstein Barr Virus Volume 1. Current Topics in Microbiology and Immunology, vol 390. Springer, Cham. https://doi.org/10.1007/978-3-319-22822-8_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-22822-8_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22821-1
Online ISBN: 978-3-319-22822-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)