Abstract
Epilepsy is a common, serious neurological disease characterized by recurring seizures. Such abnormal, excessive synchronous firing of neurons arises in part because of imbalances in excitation and inhibition in the brain. The process of epileptogenesis, during which the normal brain is transformed after injury to one capable of generating spontaneous seizures, is associated with large-scale changes in gene expression. These contribute to the remodelling of brain networks that permanently alters excitability. Components of the microRNA (miRNA) biogenesis pathway have been found to be altered in brain tissue from epilepsy patients and experimental epileptogenic insults result in select changes to miRNAs regulating neuronal microstructure, cell death, inflammation, and ion channels. Targeting key miRNAs has been shown to alter brain excitability and suppress or exacerbate seizures, indicating potential for miRNA-based therapeutics in epilepsy. Altered miRNA profiles in biofluids may be potentially useful biomarkers of epileptogenesis. In summary, miRNAs represent an important layer of gene expression control in epilepsy with therapeutic and biomarker potential.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Epilepsy is the most common neurological disease of childhood and adolescence and the second most common in adulthood after stroke. It is a chronic disease characterized by recurrent seizures, which are caused by sudden, usually brief, excessive electrical discharges in a group of neurons in the brain. The clinical manifestation of a seizure can vary from a brief lapse of attention or muscle jerks, to severe and prolonged convulsions. Several mechanisms underlying the process that transforms the normal brain into one that generates spontaneous recurrent seizures are known [1, 2]. However, much remains unknown about the observed changes as cause or consequence of epilepsy, and how they mutually interact. Identifying the involved pathways and the molecular mechanisms coordinating gene expression is crucial to a better understanding of the pathogenic process and to develop new treatment approaches.
Seizures in a majority of patients can be successfully prevented with antiepileptic drugs (AED) but nearly one-third of patients are resistant to currently available therapies. Novel treatments are urgently needed for this patient group. In addition, we need anti-epileptogenic treatments that can prevent epilepsy developing in at-risk patients, for example, following insults to the brain that lead to epilepsy (e.g., traumatic brain injury). Or a treatment which modifies the disease’s natural course, slowing progression and alleviating symptoms rather than acting simply to suppress seizures as do conventional AEDs.
microRNAs (miRNA) are an endogenous class of small noncoding RNAs that play an important role in multiple biological processes via posttranscriptional control of gene expression. They mainly function to reduce protein levels in cells through sequence-specific binding to target mRNAs, leading to transcript degradation or translational repression. The brain has an abundant and diverse contingent of miRNAs, which are crucial for normal development, and establishment and maintenance of cell phenotype. Acute and chronic nervous system diseases, including epilepsy, are associated with mis-regulation of key components of the miRNA biogenesis pathway and altered expression of miRNA. The first reports on epilepsy and miRNA appeared in 2010, followed by large-scale miRNA profiling studies characterizing the alterations in miRNA expression in experimental and human epilepsy. More recently, functional studies in rodents have shown single miRNAs can exert powerful effects on brain excitability, seizures, and epilepsy.
The present chapter provides an overview on epilepsy followed by a focus on the main discoveries on miRNA biogenesis and expression in experimental and human epilepsy. Thereafter, functional studies of epilepsy-related miRNAs will be described focusing on those with proven effects in promoting epilepsy and candidate drug and/or targets for prevention or modification of the disease.
Epilepsy
Epilepsy is a brain disease characterized by an enduring predisposition to generate seizures, and by neurological, cognitive, and psychological consequences inherent of this condition [3, 4]. It is estimated that around 65 million people worldwide have epilepsy [5]. Seizures are the hallmarks of epilepsy, and have been defined by the International League Against Epilepsy (ILAE) as “a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain” [6]. Seizures are believed to result from an imbalance between excitatory and inhibitory neurotransmission. It may be focally limited to an area or cerebral hemisphere (focal epileptic seizures) or appear bilaterally (generalized epileptic seizures) [4]. Clinically, focal seizures present features such as discrete motor movements, automatisms, altered awareness, and responsiveness. Generalized seizures are related with tonic-clonic, atonic, myoclonic and absence seizures, as well as loss of consciousness [3].
Most seizures last only a few minutes or less, terminating due to endogenous anticonvulsant mechanisms in the brain (which are themselves poorly understood). Status epilepticus (SE) is a life-threatening, neurologic emergency previously defined as “seizure that persists for a sufficient length of time or is repeated frequently enough that recovery between attacks does not occur” [7]. It has been shown that seizures that do not spontaneously terminate within 5–10 min are unlikely to end without pharmacological intervention [8, 9]. Therefore, SE has been clinically defined as a seizure longer than 5 min or more than one seizure within a 5 min period without recovery of consciousness [10]. If seizures persist for 30 min or more this can produce irreversible brain injury [11].
Epilepsies are often classified according to their causes as: (1) genetic, where genetic factors have a major causal role in the disease (with Mendelian or complex patterns of inheritance or the result of de novo mutations); (2) structural or metabolic, where acquired epilepsy is the result of changes in neuronal network excitability that follow an initial precipitating insult to the brain (i.e., traumatic brain injury (TBI), stroke, tumor, developmental malformations, febrile seizures); and (3) unknown or idiopathic, where no cause has been identified [12, 13].
Epidemiology
The incidence of epilepsy shows significant differences between developing compared with developed countries. This is due to the high levels of parasitic infections, untreated childhood epilepsy, and problems during childbirth [14]. In Africa and South America the highest incidence of epilepsy is in young adults [4]. In developed countries, epilepsy is more common in children (congenital) and the elderly (associated with chronic conditions, such as tumors and Alzheimer’s disease) [15].
There does not appear to be a strong sex difference in the risk of epilepsy, although there is a lack of consistency among the majority of incidence studies. Generally, incidence of epilepsy or of unprovoked seizures is more prevalent in males than in females (50.7 vs. 46.2 per 100,000, respectively) [16, 17]. It has been reported that males are more predisposed to develop partial epilepsies [18, 19], and it is associated with the higher prevalence of lesional epilepsy in men than women [18]. In contrast, cryptogenic temporal lobe epilepsy (TLE) seems to be more prevalent in females [18, 19]. Recent reviews suggest these differences only exist in some forms of epilepsy [20], and are not prominent.
Diagnosis
Epilepsy is not always easily diagnosed. An accurate diagnosis requires a clear differentiation between seizures and other factors that may alter consciousness, and discrimination between spontaneous unprovoked seizures from provoked seizures. It is necessary to classify seizure type and epilepsy syndrome, determining etiology where possible, age of onset of seizure, EEG patterns and brain imaging profiles, and associated behavior. Prognosis can vary widely from benign syndromes which resolve in later childhood to life-threatening epileptic encephalopathies. While a delay in the diagnosis of authentic epilepsy seldom causes problems, a false-positive diagnosis may have serious implications for the patient [21]. Unfortunately, cases of misdiagnosis are common worldwide—around 20–30 % of patients. Aiming to reduce these rates, an ILAE Task Force formulated conceptual definitions of “seizure” and “epilepsy” [6], which have been recently adapted into a global concept and translated into practical definitions [3]. It has been proposed that epilepsy is a brain disease defined by any of the following conditions: “(1) At least two unprovoked seizures occurring more than 24 h apart; (2) one unprovoked seizure and a probability of further seizures similar to the general recurrence risk (at least 60 %) after two unprovoked seizures, occurring over the next 10 years; (3) diagnosis of an epilepsy syndrome.” Epilepsy might be considered resolved (but not necessarily cured) for patients who either had an age-dependent epilepsy syndrome but are now past the applicable age, or who have remained seizure- and medication-free for the last 10 and 5 years, respectively [3]. An epilepsy diagnosis does not obligatorily require treatment. Conversely, the decision for treatment may be prophylactic considering predisposition for more seizures.
Treatment
Phenobarbital was introduced in 1912 as the first modern antiseizure medication followed by phenytoin. Second generation treatments included carbamazepine, acetazolamide, and sodium valproate and were introduced between 1950s and 1960s. A further surge in new AEDs, the so-called third generation, appeared in the 1990s. These included vigabatrin, lamotrigine, topiramate, levetiracetam, oxcarbazepine, zonisamide, gabapentin, pregabalin, and lacosamide.
Generally, around 70 % of patients with epilepsy achieve seizure freedom with the first prescribed antiseizure medication. Choice of first-line drug takes into account factors such as seizure types and syndrome (focal vs. generalized), age and sex (childbearing age, pregnancy, breast-feeding), and drug interactions (i.e., patients with learning disability or under other medications). The majority of AEDs share one or more mechanism of action in common. These are enhancing inhibitory (γ-amino butyric acid; GABA) transmission, suppressing excitatory signaling, or blocking voltage-dependent ion channels. However, AEDs with other mechanisms of action are known, including levetiracetam which targets part of the synaptic vesicle release machinery [22]. Perampanel, which acts as a selective noncompetitive antagonist of AMPA receptors, is the most recently licensed adjunctive drug [23].
For the remaining ~30 % of patients who are refractory to the currently available drug treatments (one or more drugs) [24] some may be suitable for non-pharmacological treatments, such as surgical resection and vagus nerve stimulation (VNS). Unfortunately, surgical removal of the epileptic focus is only suitable for a minority of the patients. The efficacy of brain stimulation is also suboptimal. VNS was mainly developed as a palliative treatment for those patients, and only 5 % of the patients achieve seizure freedom [25].
Experimental Models of Epilepsy
For complete reviews on experimental models of epilepsy the reader is referred elsewhere [26–29]. Animal models of epilepsy and status epilepticus have been enormously helpful to understand neuronal mechanisms of normal and abnormal brain function [30], explore new diagnostic approaches, or to test new therapeutic targets. There is a wide range of different experimental models available (in vitro and in vivo) with selection based on the particular questions being asked. Summarily, animal models can be divided in: (1) acute seizure models—in which an acute ictal activity is provoked by an insult (i.e., chemical or electrical), allowing researchers to investigate the fundamental basis of ictal discharges, effects of seizures on the brain, and seizure termination; (2) chronic epilepsy models—which mimic epilepsy (mainly TLE), and are relevant to study interictal activity and potential mechanisms (i.e., excitotoxicity and synaptic reorganization, etc.). In this section, we will briefly present some of the most widely used models.
Kainic Acid
Kainic acid (KA) is a neurotoxin [31] and structural analogue of glutamate, which preferentially binds and activates the KA subtype of ionotropic glutamate receptor [32]. These receptors are abundantly present in the hippocampus (mainly in the CA3 region), amygdala, perirhinal, and entorhinal cortex [33]. Systemic administration of KA leads to synchronous firing of neurons within the limbic system that typically develops into status epilepticus. Intrahippocampal [34] and intra-amygdala [35] delivery are also common approaches to trigger seizures which avoids exposure of the whole brain to the toxin and produces more restricted lesions within the hippocampus. KA models are considered an important tool to study complex partial seizures with secondary generalization [4, 36] as well as model epileptogenesis [37, 38]. The prolonged seizures typically produce hippocampal pathology with similarities to that seen in patients with mesial temporal sclerosis, including loss of excitatory and inhibitory neurons and gliosis. Among limitations of this model is the sometimes poor correlation between motor and electroencephalographic (EEG) activity, and the inter-strain variability in seizure and histopathological responses [39, 40].
Pilocarpine
Pilocarpine is a cholinergic muscarinic agonist that is usually delivered by systemic injection into rodents. Pilocarpine elicits seizures through metabotropic acetylcholine receptors, which are expressed in the hippocampus, striatum, and cortex [41]. However, research suggests that pilocarpine first causes a local inflammation process and consequent blood–brain barrier (BBB) disruption, which contributes to the CNS hyperexcitability [42–44]. Seizures induced by pilocarpine have limbic features including facial automatisms and tonic-clonic components which become long-lasting and develop into SE. Pilocarpine-induced SE typically produces damage to the CA1 and hilar region of the hippocampus but also extensive extra-hippocampal pathology and often high mortality [40].
Pentylenetetrazole
Pentylenetetrazole (PTZ) is a GABAergic antagonist which induces short-lasting seizures by binding to the benzodiazepine and picrotoxin sites of the GABAA receptor and blocking endogenous inhibitory control in the brain. The drug is given in one or more systemic injections, and elicits stereotypical behaviors (freezing, myoclonic twitches, clonic seizures, and tonic-clonic generalized seizures) and corresponding EEG patterns (i.e., epileptiform spiking). The PTZ model has been popular for screening putative AEDs but is also suitable for studies of the effects of single seizures on the brain. Other GABAA antagonists (e.g., bicuculline and picrotoxin) are also used occasionally to produce seizures, working via the same mechanism [40].
Kindling
Kindling refers to models in which a progressive and permanent reduction of seizure threshold is generated in response to intermittent and repeated subconvulsant stimuli (electrical or chemical) [27, 45, 46]. Kindling initially models focal partial seizures; however, with the reduction of seizure threshold precipitates the spread of seizures to produce a model of complex partial seizures with secondary generalization [27, 47]. Kindling has been successful at identifying mechanisms of epileptogenesis and also for screening AEDs. It has been reported that spontaneous seizures can result from the repeated stimulation, but studies have shown conflicting findings and its applicability to human epilepsy is controversial [48].
Mechanisms Underlying Epilepsy
Genetic Mutations
Genetic factors have a major causal role in epilepsy with a number identified which have Mendelian (familial) inheritance patterns. Albeit pure epilepsy syndromes are rare, the study of these mutations has provided great insights into molecular mechanisms of epilepsy [49, 50]. Most familial cases involve mutations in genes encoding ion channels and neurotransmitter receptors. This fits with our current thinking that seizures arise due to an imbalance between excitatory and inhibitory pathways. This does not explain, of course, why seizures are sporadic despite a permanent genetic mutation. An autosomal dominant mutation in the KCNQ2/3 genes is an example of benign familial neonatal epilepsy. Hyperexcitability is increased because of reduced potassium efflux during plasma membrane repolarization [49, 51]. Epileptic encephalopathies are a devastating group of severe childhood epilepsy disorders for which the cause is often unknown. De novo mutations are those present in an affected child only and include epileptic encephalopathies such as Lennox-Gastaut and Dravet syndromes. The majority of Dravet syndrome cases (which are considered an intractable and uncontrollable epilepsy) result from mutations of the SCN1A gene which encodes a voltage-gated sodium channel [52]. Nevertheless, mutations have been discovered in genes without obvious links to excitability including topoisomerase II (TOP2), which is involved in DNA stress and repair [53], and ALG13 which encodes an enzyme involved in N-linked glycosylation [52]. Interestingly, a number of diseases in which epilepsy is a common comorbidity result from mutations in genes closely related with miRNA function. For example, Fragile-X syndrome, a disease which results in epilepsy in about 15 % of the cases, is a result of mutations in the FMR1 gene, the product of which interacts with proteins involved in miRNA biogenesis and function [54]. Likewise, deletions of 22q11.2 which includes DCGR8 (DiGeorge syndrome critical region 8; a microprocessor complex subunit required for miRNA processing) is directly associated with seizures and childhood epilepsy [55, 56].
Acquired Epilepsy
Changes in neuronal network excitability may be a consequence of an initial precipitating insult to the brain. Traumatic brain injury, infection, stroke, tumors, and prolonged febrile seizures are leading causes of acquired epilepsy. TLE is often attributed to an earlier brain insult and is one of the most common forms of epilepsy in humans. This type of epilepsy is generally accompanied by hippocampal sclerosis, which is histopathologically marked by neuronal cell loss, gliosis, and synaptic reorganization [57, 58]. These changes are thought to be important in the pathogenesis and maintenance of the epileptic state. Here we summarize current concepts on how cell and molecular changes may promote epileptogenesis.
Neuronal Cell Loss
Neuronal cell death is a common feature in mesial TLE patients’ hippocampi [59]. It is commonly associated with each stage of the epileptogenesis process [60], particularly when the trigger is a traumatic [61] or other brain insult (e.g., SE). Although select cell death is thought to promote epilepsy, some studies have failed to observe an antiepileptogenic effect of neuroprotection [62, 63]. Loss of cells may promote epilepsy by creating an imbalance between excitatory and inhibitory inhibition [64] or by provoking reactive gliosis and inflammation [2]. In line with this view, seizure-mediated neuronal loss is not essential to generate inflammation, but proinflammatory cytokine release can contribute to cell loss; thus, dying cells may maintain inflammation [2, 65]. Additionally, apoptosis-related signaling pathways are prominently activated in experimental and human TLE supporting a role of cell death in epileptogenesis [66, 67].
Neuroinflammation: Microglia and Astrocyte Activation
There is strong evidence to support the involvement of inflammatory processes in the pathogenesis of seizures and epileptogenesis [2, 68, 69], regardless of an immune-mediated or infectious cause [65]. Expression of genes associated with inflammatory and immune pathways are markedly upregulated in human and experimental TLE [70]. This includes cytokines such as interleukin (IL)-1β, tumor necrosis factor (TNF)-α, and IL-6, which are rapidly induced in locally activated astrocytes and microglia [2]. Microglia are the resident immune cells in the CNS and these cells become activated after brain injury or immunological stimuli [71]. Microglia activation has been frequently found in resected brain tissue from patients with epilepsy [68, 72] and after experimental SE in rodents [73, 74]. Microglial activation and the consequent neuroinflammation are also linked to the progression of neurodegeneration [75]. The microglial inflammatory response has also been suggested to promote BBB damage, which further promotes seizures by disrupting ionic balances, neurotransmitters, and cell metabolism [76].
Astrocytes are highly abundant cells in the brain and are co-responsible for CNS homeostasis, exerting functions such as structural support, ionic balance and BBB maintenance, and clearance of neurotransmitters. Human and experimental TLE is invariably associated with astrocytosis within the seizure focus, which is thought to promote ionic and neurotransmitter imbalances and consequent enhancement of seizure susceptibility [77]. Other pro-inflammatory molecules released by glia include complement factors [78], products of cyclooxygenase (COX)-2 pathway [68, 79, 80], and damage-activated molecular patterns (DAMPS/danger signals) such as high mobility group box 1 (HMGB1) [81]. Seizure-induced brain inflammation can persist for days after seizure termination [2, 65] leading to transcriptional events which may contribute to long-lasting decreases in seizure threshold and further promoting neuroinflammation [2, 65].
Neuroinflammation is not invariably bad for the brain. The brain uses the inflammation process to protect cells by ensuring rapid resolution of tissue damage after injury. For instance, a neuroprotective inflammatory response is generated by purinergic receptor signaling after TBI [82]. Also, stress-hormone-dependent mechanisms trigger an amplification of Th2 and a suppression of Th1 immune responses in the brain, which increases the production of anti-inflammatory cytokines such as IL-10 [68].
BBB Disruption
Experimental models and human studies have linked damage and leakage of the BBB to seizure development [44, 83–85]. Also, it has been shown that the occurrence of seizures and neuroinflammation directly enhance BBB permeability. Summarily, some mechanisms have been proposed to directly link hyperexcitability and epileptic focus to BBB disruption: (1) Astrocyte activation due to blood-derived protein extravasation to the CNS [86, 87]; (2) Inflammation and enhancement of leukocyte adhesion proteins [2, 42–44]; (3) Epileptic activity itself that upregulates the endothelial efflux transporter P-glycoprotein, which is an essential BBB gatekeeper [78, 88].
Neuronal Plasticity
The brain is capable of profound structural changes in response to insults. Structural modifications involving dendritic and axonal reorganization have been reported in hippocampi of experimental and human epileptic tissue (reviewed by [77]). Mossy fiber sprouting (MFS) —the growth of new axon collaterals from granule cells of the dentate gyrus—is a feature observed in tissue from epilepsy patients and experimental models [89–91]. There is also significant evidence of dendritic structural changes in human and rodents hippocampus. In vivo imaging shows both short- and long-term changes to dendritic spines following seizures and this may modulate excitability by adding, adjusting the strength, or removing synaptic contacts [96, 97]. However, although this structural reorganization seems to be common, it is not agreed how important it is for aberrant neuronal networks [92, 93], and remains a point of some controversy [94, 95]. Recently, experiments using rapamycin showed this blocked MFS but did not stop epileptogenesis in TLE [95]. It remains undecided whether MFS promotes or inhibits the occurrence of spontaneous seizures.
microRNAs and CNS
microRNA Biogenesis and Mechanisms of Action
microRNA (miRNA) is a class of small (~22 nucleotides) non-protein-coding RNA molecules that regulate gene expression either by promoting mRNA degradation or by attenuating protein translation at the posttranscriptional level [96]. Briefly, miRNAs are initially transcribed as primary transcripts (pri-miRNA) by polymerase II (Pol II), processed to pre-miRNA and finally to mature miRNA by the actions of Drosha and Dicer, respectively. The functional strand of the mature miRNA is uploaded into the RNA-induced silencing complex (RISC) which contains the protein Argonaute 2 (Ago-2). The RISC-loaded miRNA is then guided to silence a target mRNA through mRNA degradation or translational inhibition. It is estimated that a third or more mRNAs are regulated by miRNA, particular those with long 3′UTRs (see Chap. 2 of the volume “microRNA: Basic Science” for a detailed discussion of miRNA machinery). A given miRNA can have several binding sites to the same mRNA and a single mRNA may be targeted by multiple miRNAs, thereby producing stronger effects [97]. In line with this view, a single miRNA is able to regulate the expression of possibly hundreds of genes, thereby exerting important effects on cellular functions [98].
Around 50 % of all identified miRNAs are expressed in the mammalian brain [99, 100]. Individual miRNAs display specific cell type and brain region distribution which contributes to their important roles in brain development and function [101–103]. In the brain, miRNAs and their biogenesis components are selectively localized within dendrites in addition to the cell soma in neurons. This allows local and activity-dependent miRNA production and regulation of protein levels at individual synapses [102, 104]. The importance of miRNA in brain development and function is exemplified by studies of mice with constitutive or conditional deletion of Drosha or Dicer [105–109]. Deletion of DGCR8 produces a reduction in brain size and loss of inhibitory synaptic neurotransmission [107, 110]. Ago-2 deficiency in mice results in death during early embryogenesis or mid-gestation [111]. Selective Dicer ablation in the CNS at later embryonic stages strongly impairs migration of late-born neurons in the cortex and oligodendrocyte precursor expansion and differentiation in the spinal cord [112].
miRNA biogenesis components have been found to be altered in experimental and human epilepsy. Whereas Drosha levels were normal in resected hippocampus from TLE patients [113] and mouse hippocampus soon after SE [113, 114], Dicer levels were decreased in some sclerotic hippocampi from experimental and human TLE [113]. Supporting the loss of Dicer as pathogenic, mice lacking Dicer have been found to develop seizures and neurodegeneration [108]. The mechanism which explains the lower Dicer levels in certain TLE hippocampi is unknown but Dicer is a caspase-3 substrate [115], and caspase-3 is activated in sclerotic hippocampi from TLE patients [116]. Ago-2 protein levels were found to be higher in hippocampus and neocortex of TLE patients [113], although were not altered after SE or TLE in mice [113, 114, 117]. Therefore, alterations in one or more components of the miRNA biogenesis pathway may directly contribute to epileptogenesis or established epilepsy.
miRNAs Regulate Key Processes in Epilepsy
The ability of individual miRNAs to have several targets within the same cell, and thus potentially exert effects on multiple pathways, make them attractive to interrupt or modify epilepsy [118]. Indeed, preclinical tests of compounds targeting single protein-coding genes have largely failed to disrupt the epileptogenesis process [119]. It has been shown that certain miRNAs (e.g., miR-132) control several epileptogenesis-related processes, such as cell death and neuroinflammation [120, 121]. Analysis of gene expression in mice lacking miR-128 revealed alterations to over 100 protein-coding genes including multiple channels and signaling components within the ERK2 signaling network [122]. Recent work has shown that miR-92a regulates AMPA receptor expression [123], and miR-128, miR-132, and miR-134 are implicated in the regulation of dendritic spines, the major contact points for excitatory communication in the CNS [124]. miR-21 and miR-146a target inflammatory components within innate and adaptive immune responses [125, 126]. miR-21 upregulation is induced by inflammatory insults, and several inflammatory targets (i.e., interleukins) were identified [129]. miR-146a was the first inflammation-associated miRNA linked to epilepsy [126]. It is the most consistently upregulated miRNA in epilepsy studies, with enhanced hippocampal levels after SE (experimentally) and in resected hippocampus from intractable TLE patients [126–129]. The mechanism that induces miR-146a level increases is possibly driven by IL-1β and inflammation-associated transcription factors including nuclear factor kappa B [129, 130] (see dedicated Chap. 9 in the volume “microRNA: Basic Science”).
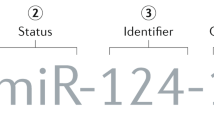
miRNA Profiling in Status Epilepticus and Epilepsy
Gene expression profiling has been a powerful tool to capture the altered molecular environment of the epileptic brain [119]. Profiling studies have investigated relevant pathways linked to the process of epileptogenesis and epilepsy and many are predicted to be under miRNA control [2, 119, 131]. The majority of experimental data come from studies which profiled miRNA responses in rodent hippocampus shortly after SE [114, 132–135]. Combined, studies to date have found altered expression levels of over 100 miRNAs after SE. This number is likely to increase as genome-wide and RNAseq studies allow more complete coverage of the miRNAome. The large numbers indicate that perhaps 30–50 % of all miRNAs are altered in the epileptic brain. These studies also reveal brain-region specific temporal changes to miRNA expression in the wake of SE (Table 4.1). That is, unique as well as overlapping miRNA expression responses are found within subfields of the hippocampus after SE and in chronic epilepsy [133]. It must be remembered, however, that all miRNA profiling studies to date have used a tissue “pool” of cells so it is difficult to know whether the miRNAs are really functional (uploaded to the RISC) or active in specific cells types [121]. Moreover, few studies have paired miRNA profiling with analysis of mRNA from the same tissue. Regardless, a subset of miRNAs with changed expression after SE in at least two profiling studies have emerged. This list includes miRNAs -21, -30c, 125b, -132, -146a, -199a, and -375 among those upregulated and miRNAs -10b, -29a, -98, -181b,c, -374, -381, -450a, and -497 downregulated. Several appear in multiple studies including miR-132 and miR-146a which are consistently upregulated across models [114, 132, 133, 135]. In some cases, however, miRNAs have displayed bidirectional responses. For example, miR-21 has been reported to have protective effects against brain injury [136] was found down- [135] and upregulated [114].
In addition to expression profiling work, a number of studies focused on changes to individual miRNAs after SE. These include miRNAs -9, -34a, -125a, -134, -145, -150, and -155 [137–141]. In these cases, expression was invariably examined using real time quantitative PCR and Taqman-type assays. The insights from such studies remain rather limited in the absence of evidence of their upload to the RISC or binding to target mRNAs.
A number of studies have profiled miRNA changes in experimental epilepsy and a subset of miRNAs have been repeatedly found to be altered. Levels of miR-146a, which are consistently increased at later time points after SE [126, 127, 133, 137], was also reported to be upregulated in the hippocampus of epileptic rats [126]. Song and collaborators [142] reported that 18 miRNAs were upregulated and 5 miRNAs were downregulated in rat hippocampus 2 months after pilocarpine-induced SE. This is a consistent pattern, with upregulation of miRNAs being more common than downregulation in experimental epilepsy [132]. Others have found miR-146a increased in epilepsy [132, 138], and other miRNAs upregulated acutely after SE such as miR-132 and miR-134, remain elevated in established epilepsy [142]. miR-21 again features among the upregulated list in epilepsy [132] and has also been reported to be increased in models of prolonged seizures in immature rats [139].
A majority of expression profiling studies have used PCR- and microarray-based platforms to profile miRNA responses but a recent study used RNA sequencing. Unexpectedly, this resulted in rather few significantly differentially expressed miRNAs being detected in the hippocampus of epileptic rats (Increased: miR-455-3p, miR-345-3p, miR-423-3p, miR-54, miR-365-5p; Decreased: miR-296-5p) [143]. It is likely that small group sizes and low statistical power are responsible for the limited detection of differentially expressed miRNA in this study which should be carefully factored in any future RNAseq work.
miRNAs have also been profiled in resected human brain tissue from epileptic patients (Table 4.1). The first study, by Kan and collaborators, analyzed 20 mesial TLE patients’ hippocampi (with and without sclerosis) and compared results to ten autopsy control tissue samples [144]. In this study, they reported similar numbers of up- and downregulated miRNAs with a total of 51 miRNAs differentially expressed by over twofold between epileptic and control groups. In contrast, the resected sclerotic human hippocampal samples analyzed by McKiernan and colleagues showed mainly downregulation of miRNAs. The collapse in miRNA production was attributed to the loss of Dicer in the tissue [113]. miRNA changes have also been reported in cortical dysplasia, another common cause of epilepsy [145]. Recently, 12 miRNAs were differentially expressed in sclerotic hippocampi samples from two groups of TLE patients with and without granule cell dispersion [146]. Among these miRNAs, miR-487a was highly expressed in an extended cohort of patients. ANTXR1, an adhesion molecule, was suggested as the possible target of miR-487a [146].
Molecular Mechanisms of miRNA Expression Control in Epilepsy
Almost nothing is known about what is driving the up- and downregulation of miRNAs in epilepsy. For some of the epilepsy-linked miRNAs such as miR-134, transcriptional mechanisms are known. Mef2 is known to be activated by neuronal activity and drives miR-134 expression in neurons [147]. However, in a majority of cases we do not yet know what promotes or represses miRNA expression in epilepsy. A recent study provided evidence that epigenetic mechanisms may be important regulators of miRNA expression in epilepsy. Epigenetic processes include DNA methylation and histone modifications. Together these have powerful effects on the transcriptional state of chromatin, increasing or decreasing the degree of compaction and providing or restricting access to transcriptional machinery. Such epigenetic mechanisms are emerging as explanations of gene regulation in health and disease, including in epilepsy [148, 149].
Miller-Delaney and collaborators performed the first genome-wide analysis of DNA methylation in human epilepsy. The researchers found that 146 protein-coding genes exhibited altered DNA methylation in hippocampi of patients with TLE, with 81.5 % of methylation differences being hypermethylation [150]. They also investigated expression of miRNA in the same samples and correlated the degree of methylation with the corresponding expression (transcript level) of the miRNA. This identified a panel of 13 methylation-sensitive miRNA in the TLE samples whereby increased methylation was associated with lower expression of the miRNA. This included miR-27a, miR-193a-5p, and miR-876-3p. Differential methylation of long noncoding RNA in human TLE was also documented for the first time [150].
In summary, profiling analysis of experimental and human SE and epilepsy shows a select group of miRNAs undergo expression changes (Table 4.1). miRNA upregulation is the predominant response in both SE and epilepsy possibly contributing to reducing protein levels in the damaged brain. These studies provide rather limited insight into what the targets of these miRNAs are and whether they have causal roles in the pathogenesis of the epileptic state. Fortunately, a number of groups have undertaken functional studies on epilepsy-regulated miRNAs, results from which demonstrate miRNAs have a causal role in the epileptogenic process and epilepsy.
miRNA and Epilepsy: An Overview About Functional Studies
Researchers have several options available to manipulate miRNAs in vivo and verify whether they are relevant for epilepsy. The techniques mainly involve the use of genetic and oligonucleotide-based targeting of the miRNA [164, 165]. Mimics are used to increase miRNAs levels, while antagomirs , which bind to a specific miRNA inhibiting its function, can be used to decrease levels [165]. There are a number of transgenic and knockout mice available but these have not yet been studied in epilepsy [164, 165].
The first miRNA for which functional studies were performed in a seizure model was miR-132. Expression of miR-132 is consistently reported as upregulated after SE and epilepsy and Ago-2 pull-downs after SE in mice confirmed that miR-132 was uploaded to the RISC [114]. It is thought that higher levels of miR-132 may promote excitability. Indeed, it has been reported that miR-132 enhances the frequency and amplitude of excitatory currents in neurons [166], and increases dendritic length and branching by targeting p250GAP [167]. In vivo silencing of miR-132 through intracerebroventricular injection of antagomirs in mice was demonstrated to reduce hippocampal damage caused by intra-amygdala KA-induced SE [114]. In more recent work, miR-132 inhibition was reported to reduce spontaneous seizures in rats and this was associated with reduced neuronal death [168]. However, treatment was initiated before SE therefore it remains unclear whether the reduction in spontaneous seizures was due to a modification of the initial insult or a truly disease-modifying effect on epilepsy.
The first miRNA for which a role in apoptosis was demonstrated was miR-34a [169]. It has been shown that miR-34a expression is controlled by p53, which is upregulated and contributes to neuronal death induced by seizures [170, 171]. Increased expression of miR-34a has been found in several reports and two studies have explored effects of antagomirs targeting miR-34a in seizure models. In one study silencing miR-34a reduced hippocampal damage after SE, but another study failed to detect such an effect. This may reflect model-specific contributions or other differences in the dosing or targeting of the miRNA [137, 141].
There has also been a single functional study on miR-184. This miRNA was identified as the most upregulated miRNA in the hippocampus after an episode of brief, non-harmful seizures, a model of epileptic preconditioning and a rich source of neuroprotective pathways [172]. McKiernan and colleagues showed that silencing miR-184 significantly increased seizure-induced neuronal death in two animal models of SE. This suggests that miR-184 may function to protect against seizure damage in the mouse [172].
A recent study revealed a strong link between miR-128 and convulsive behavior in mice. Mice with a conditional deletion of miR-128 were found to develop fatal epilepsy, which was fully prevented by treatment with an AED [122]. The mechanism was linked to increased excitatory transmission and mice lacking miR-128 displayed increased spine density. Complementing these findings, overexpression of miR-128 was able to suppress seizures triggered by kainic acid and effects were linked to the targets of miR-128 in the ERK2 network [122].
Another miRNA for which a comprehensive link to epilepsy has been demonstrated is for miR-134 (Fig. 4.1) [152]. miR-134 is a brain-enriched miRNA over-expressed after SE and in experimental and human epilepsy [152, 173]. Silencing miR-134 via antagomirs strongly reduced intra-amygdala KA-induced seizures with long-lasting protection [152] (Fig. 4.1). Recently, these protective effects were ratified using the pilocarpine model in mice [174]. In vitro antiseizure effects of targeting this miRNA have also been reported [175]. The mechanism of the antiseizure effect is uncertain but silencing miR-134 resulted in a slight decrease in hippocampal dendritic spine number in vivo which may reduce excitability [173]. This may relate to the target Limk-1, silencing of which obviated the protective effect of miR-134 in vitro [173]. Most importantly, intracerebroventricular injection of antagomirs targeting miR-134 reduced the occurrence of spontaneous seizures after SE in mice. This offers direct evidence for potential disease-modifying, anti-epileptogenic effects of targeting a miRNA (Fig. 4.1). Altogether, these data suggest that miR-134 may be a promising target to develop an antiepileptic therapy.
Antagomir silencing of miR-134. (a) Analysis of miR-134 expression in the mouse hippocampus at various time points after a single intracerebroventricular injection of antagomirs targeting miR-134 showing long-lasting silencing in mouse hippocampus. (b) Representative EEG spectrograms show that antagomir silencing of miR-134 reduces seizure severity during status epilepticus. (c) Graphs show the number of generalized tonic clonic seizures each day for individual mice during two periods of 5 days of continuous video monitoring (1 and 2 months after kainic acid-induced SE) for scramble (Scr)- and antagomir (Ant)-injected mice. Ant-134 after status epilepticus reduces the number of epileptic seizures and protects against progressive TLE pathology (adapted and modified with permission from [152])
miRNA as Biomarkers of Epilepsy
An additional application of miRNAs in epilepsy relates to their potential use as biomarkers. Biomarkers are important diagnostic tools that reflect health or disease and which can be measured in a simple, ideally minimally invasive manner. There is a strong and urgent need for biomarkers of epilepsy. A biomarker or panel of biomarkers, found in biofluids such as blood would allow doctors to identify at-risk patients after insults to the brain, predict seizure occurrence in patients with existing epilepsy, support prognosis and optimize or support discovery of therapies. There is a growing application of miRNAs as disease biomarkers using biofluid profiling [176, 177]. Biofluid miRNAs circulate in several forms, including enclosed in microparticles such as exosomes or complexed to Ago-2 and this seems to confer stability and a high reliability of detection. miRNAs are also ideal biomarkers because of their tissue-specific expression and roles in normal physiology and disease. There is a strong association between circulating and tissue levels although the sources of circulating miRNAs are still not well understood. It has been suggested that under healthy conditions miRNAs might be released from cells into the circulatory system. In disease or following injury, miRNAs derive from pathological processes within tissues [178, 179], for example, as by-products of necrotic or apoptotic cells [180]. There is also evidence that miRNAs are actively packaged and released in exosomes, functioning in a manner similar to hormones and cytokines in distant cell-to-cell communication [181].
A number of studies have investigated miRNA expression in blood after SE [134, 178], epileptogenesis, chronic epilepsy [178], stroke, intracerebral hemorrhage, and TBI [134, 179, 180]. They suggest there are unique miRNAs or groups of miRNAs which may reflect specific injuries to the brain or different phases of the epileptogenic process. These findings, whether validated in humans, might support diagnosis, prognosis, and patient treatment decisions not only in epilepsy, but also in other CNS disorders.
For complete review on circulating miRNAs as potential biomarkers in diagnosing CNS diseases the reader is referred elsewhere [121, 182–185].
Conclusion
There is now strong evidence supporting a role for miRNAs in the pathophysiology of epilepsy. Profiling work is increasingly providing a complete description of the expression levels and pathways under miRNA control in epilepsy. Concomitantly, researchers are establishing the in vivo functions of epilepsy-associated miRNAs and deploying RNA-based therapeutics as a novel approach to treatment. The use of miRNA inhibitors is already appearing in the medical literature. The first of these, miravirsen, was an antagomir blocking liver-expressed miR-122 which was found to be safe and effective in clinical trials of hepatitis C in humans [186]. Certainly, targeting miRNAs in CNS disorders will pose an additional challenge [187, 188]. This is because antagomirs are macromolecules that do not cross an intact blood brain barrier, which is essential for clinical use. Likewise, we need more data on the effects of antagomirs on the targets of the miRNAs and how to avoid off-targets effects. miRNAs also offer potential as biomarkers of epilepsy which may lead to novel diagnostics. In summary, miRNAs have emerged as important contributors to gene expression control in the brain. They offer a perhaps unique combination of therapeutic opportunities and co-developed molecular diagnostics for epilepsy.
References
Loscher W, Brandt C. Prevention or modification of epileptogenesis after brain insults: experimental approaches and translational research. Pharmacol Rev. 2010;62:668–700.
Vezzani A, French J, Bartfai T, Baram TZ. The role of inflammation in epilepsy. Nat Rev Neurol. 2011;7:31–40.
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475–82.
Engel Jr J. Classification of epileptic disorders. Epilepsia. 2001;42:316.
Thurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, Ding D, et al. Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia. 2011;52 Suppl 7:2–26.
Fisher RS, van Emde BW, Blume W, Elger C, Genton P, Lee P, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46:470–2.
Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the commission on classification and terminology of the international league against epilepsy. Epilepsia. 1981;22:489–501.
Jenssen S, Gracely EJ, Sperling MR. How long do most seizures last? A systematic comparison of seizures recorded in the epilepsy monitoring unit. Epilepsia. 2006;47:1499–503.
Shinnar S, Berg AT, Moshe SL, Shinnar R. How long do new-onset seizures in children last? Ann Neurol. 2001;49:659–64.
Al-Mufti F, Claassen J. Neurocritical care: status epilepticus review. Crit Care Clin. 2014;30:751–64.
Meldrum BS, Brierley JB. Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch Neurol. 1973;28:10–7.
Moshe SL, Perucca E, Ryvlin P, Tomson T. Epilepsy: new advances. Lancet. 2015;385(9971):884–98.
Thomas RH, Berkovic SF. The hidden genetics of epilepsy-a clinically important new paradigm. Nat Rev Neurol. 2014;10:283–92.
Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51:883–90.
Savage N. Epidemiology: the complexities of epilepsy. Nature. 2014;511:S2–3.
Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935–1984. Epilepsia. 1993;34:453–68.
Kotsopoulos IA, van Merode T, Kessels FG, de Krom MC, Knottnerus JA. Systematic review and meta-analysis of incidence studies of epilepsy and unprovoked seizures. Epilepsia. 2002;43:1402–9.
Christensen J, Kjeldsen MJ, Andersen H, Friis ML, Sidenius P. Gender differences in epilepsy. Epilepsia. 2005;46:956–60.
McHugh JC, Delanty N. Epidemiology and classification of epilepsy: gender comparisons. Int Rev Neurobiol. 2008;83:11–26.
Savic I. Sex differences in human epilepsy. Exp Neurol. 2014;259:38–43.
Benbadis S. The differential diagnosis of epilepsy: a critical review. Epilepsy Behav. 2009;15:15–21.
Rogawski MA. Diverse mechanisms of antiepileptic drugs in the development pipeline. Epilepsy Res. 2006;69:273–94.
Rogawski MA, Hanada T. Preclinical pharmacology of perampanel, a selective non-competitive AMPA receptor antagonist. Acta Neurol Scand Suppl. 2013:19–24.
Perucca E, French J, Bialer M. Development of new antiepileptic drugs: challenges, incentives, and recent advances. Lancet Neurol. 2007;6:793–804.
Fisher RS. Therapeutic devices for epilepsy. Ann Neurol. 2012;71:157–68.
Pitkänen A, Schwartzkroin PA, Moshé SL. Models of seizures and epilepsy. Oxford: Elsevier Academic Press; 2006. 712 p.
Coppola A, Moshe SL. Animal models. Handb Clin Neurol. 2012;107:63–98.
Loscher W. Critical review of current animal models of seizures and epilepsy used in the discovery and development of new antiepileptic drugs. Seizure. 2011;20:359–68.
Simonato M, Brooks-Kayal AR, Engel Jr J, Galanopoulou AS, Jensen FE, Moshe SL, et al. The challenge and promise of anti-epileptic therapy development in animal models. Lancet Neurol. 2014;13:949–60.
Engel Jr J, International League Against Epilepsy. A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE Task Force on Classification and Terminology. Epilepsia. 2001;42:796–803.
McGeer PL, McGeer EG. Intracerebral injections of kainic acid and tetanus toxin: possible models for the signs of chorea and dystonia. Adv Neurol. 1978;21:331–8.
Coyle JT. Kainic acid: insights into excitatory mechanisms causing selective neuronal degeneration. Ciba Found Symp. 1987;126:186–203.
Miller LP, Johnson AE, Gelhard RE, Insel TR. The ontogeny of excitatory amino acid receptors in the rat forebrain—II. Kainic acid receptors. Neuroscience. 1990;35:45–51.
Schwarcz R, Zaczek R, Coyle JT. Microinjection of kainic acid into the rat hippocampus. Eur J Pharmacol. 1978;50:209–20.
Rondouin G, Bockaert J, Lerner-Natoli M. L-nitroarginine, an inhibitor of NO synthase, dramatically worsens limbic epilepsy in rats. Neuroreport. 1993;4:1187–90.
Ben-Ari Y. Limbic seizure and brain damage produced by kainic acid: mechanisms and relevance to human temporal lobe epilepsy. Neuroscience. 1985;14:375–403.
Cavalheiro EA, Riche DA, Le Gal La Salle G. Long-term effects of intrahippocampal kainic acid injection in rats: a method for inducing spontaneous recurrent seizures. Electroencephalogr Clin Neurophysiol. 1982;53:581–9.
Stafstrom CE, Thompson JL, Holmes GL. Kainic acid seizures in the developing brain: status epilepticus and spontaneous recurrent seizures. Brain Res Dev Brain Res. 1992;65:227–36.
Giorgi FS, Malhotra S, Hasson H, Veliskova J, Rosenbaum DM, Moshe SL. Effects of status epilepticus early in life on susceptibility to ischemic injury in adulthood. Epilepsia. 2005;46:490–8.
Velisek L. Models of chemically-induced acute seizures. In: Pitkanen A, Schwartzkroin PA, Moshé S, editors. Models of seizure and epilepsy. Elsevier Academic Press: Oxford; 2006. p. 127–52.
Kuhar M, Yamamura HI. Localization of cholinergic muscarinic receptors in rat brain by light microscopic radioautography. Brain Res. 1976;110:229–43.
Fabene PF, Navarro Mora G, Martinello M, Rossi B, Merigo F, Ottoboni L, et al. A role for leukocyte-endothelial adhesion mechanisms in epilepsy. Nat Med. 2008;14:1377–83.
Oby E, Janigro D. The blood–brain barrier and epilepsy. Epilepsia. 2006;47:1761–74.
Marchi N, Angelov L, Masaryk T, Fazio V, Granata T, Hernandez N, et al. Seizure-promoting effect of blood–brain barrier disruption. Epilepsia. 2007;48:732–42.
Goddard GV, McIntyre DC, Leech CK. A permanent change in brain function resulting from daily electrical stimulation. Exp Neurol. 1969;25:295–330.
McNamara JO, Byrne MC, Dasheiff RM, Fitz JG. The kindling model of epilepsy: a review. Prog Neurobiol. 1980;15:139–59.
Morrell F. Secondary epileptogenic lesions. Epilepsia. 1960;1:538–60.
Bertram E. The relevance of kindling for human epilepsy. Epilepsia. 2007;48 Suppl 2:65–74.
Chang BS, Lowenstein DH. Epilepsy. N Engl J Med. 2003;349:1257–66.
Hanna MG. Genetic neurological channelopathies. Nat Clin Pract Neurol. 2006;2:252–63.
Maljevic S, Lerche H. Potassium channel genes and benign familial neonatal epilepsy. Prog Brain Res. 2014;213:17–53.
Epi4K Consortium, Epilepsy Phenome/Genome Project, Allen AS, Berkovic SF, Cossette P, Delanty N, et al. De novo mutations in epileptic encephalopathies. Nature. 2013;501:217–21.
Gomez-Herreros F, Schuurs-Hoeijmakers JH, McCormack M, Greally MT, Rulten S, Romero-Granados R, et al. TDP2 protects transcription from abortive topoisomerase activity and is required for normal neural function. Nat Genet. 2014;46:516–21.
Jin P, Alisch RS, Warren ST. RNA and microRNAs in fragile X mental retardation. Nat Cell Biol. 2004;6:1048–53.
Piccione M, Vecchio D, Cavani S, Malacarne M, Pierluigi M, Corsello G. The first case of myoclonic epilepsy in a child with a de novo 22q11.2 microduplication. Am J Med Genet A. 2011;155A:3054–9.
Cheung EN, George SR, Andrade DM, Chow EW, Silversides CK, Bassett AS. Neonatal hypocalcemia, neonatal seizures, and intellectual disability in 22q11.2 deletion syndrome. Genet Med. 2014;16:40–4.
Wieser HG, ILAE Commission on Neurosurgery of Epilepsy. ILAE commission report. Mesial temporal lobe epilepsy with hippocampal sclerosis. Epilepsia. 2004;45:695–714.
Thom M, Blumcke I, Aronica E. Long-term epilepsy-associated tumors. Brain Pathol. 2012;22:350–79.
Thom M. Review: hippocampal sclerosis in epilepsy: a neuropathology review. Neuropathol Appl Neurobiol. 2014;40:520–43.
Okamoto OK, Janjoppi L, Bonone FM, Pansani AP, da Silva AV, Scorza FA, et al. Whole transcriptome analysis of the hippocampus: toward a molecular portrait of epileptogenesis. BMC Genomics. 2010;11:230.
Kharatishvili I, Pitkanen A. Association of the severity of cortical damage with the occurrence of spontaneous seizures and hyperexcitability in an animal model of posttraumatic epilepsy. Epilepsy Res. 2010;90:47–59.
Ebert U, Brandt C, Loscher W. Delayed sclerosis, neuroprotection, and limbic epileptogenesis after status epilepticus in the rat. Epilepsia. 2002;43 Suppl 5:86–95.
Andre V, Ferrandon A, Marescaux C, Nehlig A. Electroshocks delay seizures and subsequent epileptogenesis but do not prevent neuronal damage in the lithium-pilocarpine model of epilepsy. Epilepsy Res. 2000;42:7–22.
Sloviter RS, Bumanglag AV. Defining “epileptogenesis” and identifying “antiepileptogenic targets” in animal models of acquired temporal lobe epilepsy is not as simple as it might seem. Neuropharmacology. 2013;69:3–15.
Vezzani A, Aronica E, Mazarati A, Pittman QJ. Epilepsy and brain inflammation. Exp Neurol. 2013;244:11–21.
Engel T, Murphy BM, Hatazaki S, Jimenez-Mateos EM, Concannon CG, Woods I, et al. Reduced hippocampal damage and epileptic seizures after status epilepticus in mice lacking proapoptotic Puma. FASEB J. 2010;24:853–61.
Engel T, Sanz-Rodgriguez A, Jimenez-Mateos EM, Concannon CG, Jimenez-Pacheco A, Moran C, et al. CHOP regulates the p53-MDM2 axis and is required for neuronal survival after seizures. Brain. 2013;136:577–92.
Vezzani A, Granata T. Brain inflammation in epilepsy: experimental and clinical evidence. Epilepsia. 2005;46:1724–43.
Pitkanen A, Sutula TP. Is epilepsy a progressive disorder? Prospects for new therapeutic approaches in temporal-lobe epilepsy. Lancet Neurol. 2002;1:173–81.
Aronica E, Gorter JA. Gene expression profile in temporal lobe epilepsy. Neuroscientist. 2007;13:100–8.
Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996;19:312–8.
Choi J, Nordli Jr DR, Alden TD, DiPatri Jr A, Laux L, Kelley K, et al. Cellular injury and neuroinflammation in children with chronic intractable epilepsy. J Neuroinflammation. 2009;6:38.
Jorgensen MB, Finsen BR, Jensen MB, Castellano B, Diemer NH, Zimmer J. Microglial and astroglial reactions to ischemic and kainic acid-induced lesions of the adult rat hippocampus. Exp Neurol. 1993;120:70–88.
Borges K, Gearing M, McDermott DL, Smith AB, Almonte AG, Wainer BH, et al. Neuronal and glial pathological changes during epileptogenesis in the mouse pilocarpine model. Exp Neurol. 2003;182:21–34.
da Fonseca AC, Matias D, Garcia C, Amaral R, Geraldo LH, Freitas C, et al. The impact of microglial activation on blood–brain barrier in brain diseases. Front Cell Neurosci. 2014;8:362.
Obermeier B, Daneman R, Ransohoff RM. Development, maintenance and disruption of the blood–brain barrier. Nat Med. 2013;19:1584–96.
Varvel NH, Jiang J, Dingledine R. Candidate drug targets for prevention or modification of epilepsy. Annu Rev Pharmacol Toxicol. 2015;55:229–47.
Ravizza T, Gagliardi B, Noe F, Boer K, Aronica E, Vezzani A. Innate and adaptive immunity during epileptogenesis and spontaneous seizures: evidence from experimental models and human temporal lobe epilepsy. Neurobiol Dis. 2008;29:142–60.
Oliveira MS, Furian AF, Royes LF, Fighera MR, Fiorenza NG, Castelli M, et al. Cyclooxygenase-2/PGE2 pathway facilitates pentylenetetrazol-induced seizures. Epilepsy Res. 2008;79:14–21.
Rojas A, Jiang J, Ganesh T, Yang MS, Lelutiu N, Gueorguieva P, et al. Cyclooxygenase-2 in epilepsy. Epilepsia. 2014;55:17–25.
Maroso M, Balosso S, Ravizza T, Liu J, Aronica E, Iyer AM, et al. Toll-like receptor 4 and high-mobility group box-1 are involved in ictogenesis and can be targeted to reduce seizures. Nat Med. 2010;16:413–9.
Roth TL, Nayak D, Atanasijevic T, Koretsky AP, Latour LL, McGavern DB. Transcranial amelioration of inflammation and cell death after brain injury. Nature. 2014;505:223–8.
Fieschi C, Lenzi GL, Zanette E, Orzi F, Passero S. Effects on EEG of the osmotic opening of the blood–brain barrier in rats. Life Sci. 1980;27:239–43.
Uva L, Librizzi L, Marchi N, Noe F, Bongiovanni R, Vezzani A, et al. Acute induction of epileptiform discharges by pilocarpine in the in vitro isolated guinea-pig brain requires enhancement of blood–brain barrier permeability. Neuroscience. 2008;151:303–12.
van Vliet EA, da Costa AS, Redeker S, van Schaik R, Aronica E, Gorter JA. Blood–brain barrier leakage may lead to progression of temporal lobe epilepsy. Brain. 2007;130:521–34.
Ivens S, Kaufer D, Flores LP, Bechmann I, Zumsteg D, Tomkins O, et al. TGF-beta receptor-mediated albumin uptake into astrocytes is involved in neocortical epileptogenesis. Brain. 2007;130:535–47.
David Y, Cacheaux LP, Ivens S, Lapilover E, Heinemann U, Kaufer D, et al. Astrocytic dysfunction in epileptogenesis: consequence of altered potassium and glutamate homeostasis? J Neurosci. 2009;29:10588–99.
Loscher W, Potschka H. Drug resistance in brain diseases and the role of drug efflux transporters. Nat Rev Neurosci. 2005;6:591–602.
Tauck DL, Nadler JV. Evidence of functional mossy fiber sprouting in hippocampal formation of kainic acid-treated rats. J Neurosci. 1985;5:1016–22.
Cavazos JE, Golarai G, Sutula TP. Mossy fiber synaptic reorganization induced by kindling: time course of development, progression, and permanence. J Neurosci. 1991;11:2795–803.
Nadler JV, Perry BW, Gentry C, Cotman CW. Degeneration of hippocampal CA3 pyramidal cells induced by intraventricular kainic acid. J Comp Neurol. 1980;192:333–59.
Sutula T, Cascino G, Cavazos J, Parada I, Ramirez L. Mossy fiber synaptic reorganization in the epileptic human temporal lobe. Ann Neurol. 1989;26:321–30.
Cronin J, Dudek FE. Chronic seizures and collateral sprouting of dentate mossy fibers after kainic acid treatment in rats. Brain Res. 1988;474:181–4.
Masukawa LM, Uruno K, Sperling M, O’Connor MJ, Burdette LJ. The functional relationship between antidromically evoked field responses of the dentate gyrus and mossy fiber reorganization in temporal lobe epileptic patients. Brain Res. 1992;579:119–27.
Heng K, Haney MM, Buckmaster PS. High-dose rapamycin blocks mossy fiber sprouting but not seizures in a mouse model of temporal lobe epilepsy. Epilepsia. 2013;54:1535–41.
Schirle NT, MacRae IJ. The crystal structure of human Argonaute2. Science. 2012;336:1037–40.
Esquela-Kerscher A, Slack FJ. Oncomirs—microRNAs with a role in cancer. Nat Rev Cancer. 2006;6:259–69.
Selbach M, Schwanhausser B, Thierfelder N, Fang Z, Khanin R, Rajewsky N. Widespread changes in protein synthesis induced by microRNAs. Nature. 2008;455:58–63.
Lagos-Quintana M, Rauhut R, Yalcin A, Meyer J, Lendeckel W, Tuschl T. Identification of tissue-specific microRNAs from mouse. Curr Biol. 2002;12:735–9.
Krichevsky AM, King KS, Donahue CP, Khrapko K, Kosik KS. A microRNA array reveals extensive regulation of microRNAs during brain development. RNA. 2003;9:1274–81.
Jimenez-Mateos EM, Henshall DC. Epilepsy and microRNA. Neuroscience. 2013;238:218–29.
O’Carroll D, Schaefer A. General principals of miRNA biogenesis and regulation in the brain. Neuropsychopharmacology. 2013;38:39–54.
Siegel C, Li J, Liu F, Benashski SE, McCullough LD. miR-23a regulation of X-linked inhibitor of apoptosis (XIAP) contributes to sex differences in the response to cerebral ischemia. Proc Natl Acad Sci U S A. 2011;108:11662–7.
Lugli G, Torvik VI, Larson J, Smalheiser NR. Expression of microRNAs and their precursors in synaptic fractions of adult mouse forebrain. J Neurochem. 2008;106:650–61.
Davis TH, Cuellar TL, Koch SM, Barker AJ, Harfe BD, McManus MT, et al. Conditional loss of Dicer disrupts cellular and tissue morphogenesis in the cortex and hippocampus. J Neurosci. 2008;28:4322–30.
De Pietri TD, Pulvers JN, Haffner C, Murchison EP, Hannon GJ, Huttner WB. miRNAs are essential for survival and differentiation of newborn neurons but not for expansion of neural progenitors during early neurogenesis in the mouse embryonic neocortex. Development. 2008;135:3911–21.
Babiarz JE, Hsu R, Melton C, Thomas M, Ullian EM, Blelloch R. A role for noncanonical microRNAs in the mammalian brain revealed by phenotypic differences in Dgcr8 versus Dicer1 knockouts and small RNA sequencing. RNA. 2011;17:1489–501.
Tao J, Wu H, Lin Q, Wei W, Lu XH, Cantle JP, et al. Deletion of astroglial Dicer causes non-cell-autonomous neuronal dysfunction and degeneration. J Neurosci. 2011;31:8306–19.
Knuckles P, Vogt MA, Lugert S, Milo M, Chong MM, Hautbergue GM, et al. Drosha regulates neurogenesis by controlling neurogenin 2 expression independent of microRNAs. Nat Neurosci. 2012;15:962–9.
Hsu R, Schofield CM, Dela Cruz CG, Jones-Davis DM, Blelloch R, Ullian EM. Loss of microRNAs in pyramidal neurons leads to specific changes in inhibitory synaptic transmission in the prefrontal cortex. Mol Cell Neurosci. 2012;50:283–92.
Morita S, Horii T, Kimura M, Goto Y, Ochiya T, Hatada I. One Argonaute family member, Eif2c2 (Ago2), is essential for development and appears not to be involved in DNA methylation. Genomics. 2007;89:687–96.
Kawase-Koga Y, Otaegi G, Sun T. Different timings of Dicer deletion affect neurogenesis and gliogenesis in the developing mouse central nervous system. Dev Dyn. 2009;238:2800–12.
McKiernan RC, Jimenez-Mateos EM, Bray I, Engel T, Brennan GP, Sano T, et al. Reduced mature microRNA levels in association with dicer loss in human temporal lobe epilepsy with hippocampal sclerosis. PLoS One. 2012;7, e35921.
Jimenez-Mateos EM, Bray I, Sanz-Rodriguez A, Engel T, McKiernan RC, Mouri G, et al. miRNA Expression profile after status epilepticus and hippocampal neuroprotection by targeting miR-132. Am J Pathol. 2011;179:2519–32.
Nakagawa A, Shi Y, Kage-Nakadai E, Mitani S, Xue D. Caspase-dependent conversion of Dicer ribonuclease into a death-promoting deoxyribonuclease. Science. 2010;328:327–34.
Schindler CK, Pearson EG, Bonner HP, So NK, Simon RP, Prehn JH, et al. Caspase-3 cleavage and nuclear localization of caspase-activated DNase in human temporal lobe epilepsy. J Cereb Blood Flow Metab. 2006;26:583–9.
Bicker S, Lackinger M, Weiss K, Schratt G. MicroRNA-132, -134, and -138: a microRNA troika rules in neuronal dendrites. Cell Mol Life Sci. 2014;71:3987–4005.
Friedman RC, Farh KK, Burge CB, Bartel DP. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19:92–105.
Pitkanen A, Lukasiuk K. Mechanisms of epileptogenesis and potential treatment targets. Lancet Neurol. 2011;10:173–86.
Dogini DB, Avansini SH, Vieira AS, Lopes-Cendes I. MicroRNA regulation and dysregulation in epilepsy. Front Cell Neurosci. 2013;7:172.
Henshall DC. MicroRNAs in the pathophysiology and treatment of status epilepticus. Front Mol Neurosci. 2013;6:37.
Tan CL, Plotkin JL, Veno MT, von Schimmelmann M, Feinberg P, Mann S, et al. MicroRNA-128 governs neuronal excitability and motor behavior in mice. Science. 2013;342:1254–8.
Letellier M, Elramah S, Mondin M, Soula A, Penn A, Choquet D, et al. miR-92a regulates expression of synaptic GluA1-containing AMPA receptors during homeostatic scaling. Nat Neurosci. 2014;17:1040–2.
Siegel G, Saba R, Schratt G. microRNAs in neurons: manifold regulatory roles at the synapse. Curr Opin Genet Dev. 2011;21:491–7.
Sheedy FJ, O’Neill LA. Adding fuel to fire: microRNAs as a new class of mediators of inflammation. Ann Rheum Dis. 2008;67 Suppl 3:iii50–5.
Aronica E, Fluiter K, Iyer A, Zurolo E, Vreijling J, van Vliet EA, et al. Expression pattern of miR-146a, an inflammation-associated microRNA, in experimental and human temporal lobe epilepsy. Eur J Neurosci. 2010;31:1100–7.
Omran A, Peng J, Zhang C, Xiang QL, Xue J, Gan N, et al. Interleukin-1beta and microRNA-146a in an immature rat model and children with mesial temporal lobe epilepsy. Epilepsia. 2012;53:1215–24.
de Araujo MA, Marques TE, Taniele-Silva J, Souza FM, de Andrade TG, Garcia-Cairasco N, et al. Identification of endogenous reference genes for the analysis of microRNA expression in the hippocampus of the pilocarpine-induced model of mesial temporal lobe epilepsy. PLoS One. 2014;9, e100529.
Iyer A, Zurolo E, Prabowo A, Fluiter K, Spliet WG, van Rijen PC, et al. MicroRNA-146a: a key regulator of astrocyte-mediated inflammatory response. PLoS One. 2012;7, e44789.
Taganov KD, Boldin MP, Chang KJ, Baltimore D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci U S A. 2006;103:12481–6.
Henshall DC. MicroRNAs in the pathophysiology and treatment of status epilepticus. Front Mol Neurosci. 2013;6:1–11.
Risbud RM, Porter BE. Changes in microRNA expression in the whole hippocampus and hippocampal synaptoneurosome fraction following pilocarpine induced status epilepticus. PLoS One. 2013;8, e53464.
Gorter JA, Iyer A, White I, Colzi A, van Vliet EA, Sisodiya S, et al. Hippocampal subregion-specific microRNA expression during epileptogenesis in experimental temporal lobe epilepsy. Neurobiol Dis. 2014;62:508–20.
Liu DZ, Tian Y, Ander BP, Xu H, Stamova BS, Zhan X, et al. Brain and blood microRNA expression profiling of ischemic stroke, intracerebral hemorrhage, and kainate seizures. J Cereb Blood Flow Metab. 2010;30:92–101.
Hu K, Zhang C, Long L, Long X, Feng L, Li Y, et al. Expression profile of microRNAs in rat hippocampus following lithium-pilocarpine-induced status epilepticus. Neurosci Lett. 2011;488:252–7.
Ge XT, Lei P, Wang HC, Zhang AL, Han ZL, Chen X, et al. miR-21 improves the neurological outcome after traumatic brain injury in rats. Sci Rep. 2014;4:6718.
Hu K, Xie YY, Zhang C, Ouyang DS, Long HY, Sun DN, et al. MicroRNA expression profile of the hippocampus in a rat model of temporal lobe epilepsy and miR-34a-targeted neuroprotection against hippocampal neurone cell apoptosis post-status epilepticus. BMC Neurosci. 2012;13:115.
Pichardo-Casas I, Goff LA, Swerdel MR, Athie A, Davila J, Ramos-Brossier M, et al. Expression profiling of synaptic microRNAs from the adult rat brain identifies regional differences and seizure-induced dynamic modulation. Brain Res. 2012;1436:20–33.
Peng J, Omran A, Ashhab MU, Kong H, Gan N, He F, et al. Expression patterns of miR-124, miR-134, miR-132, and miR-21 in an immature rat model and children with mesial temporal lobe epilepsy. J Mol Neurosci. 2013;50:291–7.
Ashhab MU, Omran A, Kong H, Gan N, He F, Peng J, et al. Expressions of tumor necrosis factor alpha and microRNA-155 in immature rat model of status epilepticus and children with mesial temporal lobe epilepsy. J Mol Neurosci. 2013;51:950–8.
Sano T, Reynolds JP, Jimenez-Mateos EM, Matsushima S, Taki W, Henshall DC. MicroRNA-34a upregulation during seizure-induced neuronal death. Cell Death Dis. 2012;3, e287.
Song YJ, Tian XB, Zhang S, Zhang YX, Li X, Li D, et al. Temporal lobe epilepsy induces differential expression of hippocampal miRNAs including let-7e and miR-23a/b. Brain Res. 2011;1387:134–40.
Li MM, Jiang T, Sun Z, Zhang Q, Tan CC, Yu JT, et al. Genome-wide microRNA expression profiles in hippocampus of rats with chronic temporal lobe epilepsy. Sci Rep. 2014;4:4734.
Kan AA, van Erp S, Derijck AA, de Wit M, Hessel EV, O’Duibhir E, et al. Genome-wide microRNA profiling of human temporal lobe epilepsy identifies modulators of the immune response. Cell Mol Life Sci. 2012;69:3127–45.
Lee JY, Park AK, Lee ES, Park WY, Park SH, Choi JW, et al. miRNA expression analysis in cortical dysplasia: regulation of mTOR and LIS1 pathway. Epilepsy Res. 2014;108:433–41.
Zucchini S, Marucci G, Paradiso B, Lanza G, Roncon P, Cifelli P, et al. Identification of miRNAs differentially expressed in human epilepsy with or without granule cell pathology. PLoS One. 2014;9, e105521.
Fiore R, Khudayberdiev S, Christensen M, Siegel G, Flavell SW, Kim TK, et al. Mef2-mediated transcription of the miR379-410 cluster regulates activity-dependent dendritogenesis by fine-tuning Pumilio2 protein levels. EMBO J. 2009;28:697–710.
Boison D, Sandau US, Ruskin DN, Kawamura Jr M, Masino SA. Homeostatic control of brain function—new approaches to understand epileptogenesis. Front Cell Neurosci. 2013;7:109.
Roopra A, Dingledine R, Hsieh J. Epigenetics and epilepsy. Epilepsia. 2012;53 Suppl 9:2–10.
Miller-Delaney SF, Bryan K, Das S, McKiernan RC, Bray IM, Reynolds JP, et al. Differential DNA methylation profiles of coding and non-coding genes define hippocampal sclerosis in human temporal lobe epilepsy. Brain. 2015;138:616–31.
Risbud RM, Lee C, Porter BE. Neurotrophin-3 mRNA a putative target of miR21 following status epilepticus. Brain Res. 2011;1424:53–9.
Jimenez-Mateos EM, Engel T, Merino-Serrais P, McKiernan RC, Tanaka K, Mouri G, et al. Silencing microRNA-134 produces neuroprotective and prolonged seizure-suppressive effects. Nat Med. 2012;18:1087–94.
Bot AM, Debski KJ, Lukasiuk K. Alterations in miRNA levels in the dentate gyrus in epileptic rats. PLoS One. 2013;8, e76051.
Sun Z, Yu JT, Jiang T, Li MM, Tan L, Zhang Q, et al. Genome-wide microRNA profiling of rat hippocampus after status epilepticus induced by amygdala stimulation identifies modulators of neuronal apoptosis. PLoS One. 2013;8, e78375.
Moon J, Lee ST, Choi J, Jung KH, Yang H, Khalid A, et al. Unique behavioral characteristics and microRNA signatures in a drug resistant epilepsy model. PLoS One. 2014;9, e85617.
Matos G, Scorza FA, Mazzotti DR, Guindalini C, Cavalheiro EA, Tufik S, et al. The effects of sleep deprivation on microRNA expression in rats submitted to pilocarpine-induced status epilepticus. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:159–65.
Li MM, Jiang T, Sun Z, Zhang Q, Tan CC, Yu JT, Tan L. Genome-wide microRNA expression profiles in hippocampus of rats with chronic temporal lobe epilepsy. Sci Rep. 2014; 4, 4734.
Kretschmann A, Danis B, Andonovic L, Abnaof K, van Rikxoort M, Siegel F, et al. Different microRNA profiles in chronic epilepsy versus acute seizure mouse models. J Mol Neurosci. 2015;55:466–79.
Sosanya NM, Brager DH, Wolfe S, Niere F, Raab-Graham KF. Rapamycin reveals an mTOR-independent repression of Kv1.1 expression during epileptogenesis. Neurobiol Dis. 2015;73:96–105.
Guo J, Wang H, Wang Q, Chen Y, Chen S. Expression of p-CREB and activity-dependent miR-132 in temporal lobe epilepsy. Int J Clin Exp Med. 2014;7:1297–306.
Kaalund SS, Veno MT, Bak M, Moller RS, Laursen H, Madsen F, et al. Aberrant expression of miR-218 and miR-204 in human mesial temporal lobe epilepsy and hippocampal sclerosis-convergence on axonal guidance. Epilepsia. 2014;55:2017–27.
Dombkowski AA, Batista CE, Cukovic D, Carruthers NJ, Ranganathan R, Shukla U, et al. Cortical tubers: windows into dysregulation of epilepsy risk and synaptic signaling genes by microRNAs. Cereb Cortex. 2014.
Jiang G, Zhou R, He X, Shi Z, Huang M, Yu J, et al. Expression levels of microRNA-199 and hypoxia-inducible factor-1 alpha in brain tissue of patients with intractable epilepsy. Int J Neurosci. 2014:1–29.
Brown BD, Naldini L. Exploiting and antagonizing microRNA regulation for therapeutic and experimental applications. Nat Rev Genet. 2009;10:578–85.
Bhalala OG, Srikanth M, Kessler JA. The emerging roles of microRNAs in CNS injuries. Nat Rev Neurol. 2013;9:328–39.
Edbauer D, Neilson JR, Foster KA, Wang CF, Seeburg DP, Batterton MN, et al. Regulation of synaptic structure and function by FMRP-associated microRNAs miR-125b and miR-132. Neuron. 2010;65:373–84.
Wayman GA, Davare M, Ando H, Fortin D, Varlamova O, Cheng HY, et al. An activity-regulated microRNA controls dendritic plasticity by down-regulating p250GAP. Proc Natl Acad Sci U S A. 2008;105:9093–8.
Huang Y, Guo J, Wang Q, Chen Y. MicroRNA-132 silencing decreases the spontaneous recurrent seizures. Int J Clin Exp Med. 2014;7:1639–49.
Welch C, Chen Y, Stallings RL. MicroRNA-34a functions as a potential tumor suppressor by inducing apoptosis in neuroblastoma cells. Oncogene. 2007;26:5017–22.
Morrison RS, Wenzel HJ, Kinoshita Y, Robbins CA, Donehower LA, Schwartzkroin PA. Loss of the p53 tumor suppressor gene protects neurons from kainate—induced cell death. J Neurosci. 1996;16:1337–45.
Engel T, Tanaka K, Jimenez-Mateos EM, Caballero-Caballero A, Prehn JH, Henshall DC. Loss of p53 results in protracted electrographic seizures and development of an aggravated epileptic phenotype following status epilepticus. Cell Death Dis. 2010;1, e79.
McKiernan RC, Jimenez-Mateos EM, Sano T, Bray I, Stallings RL, Simon RP, et al. Expression profiling the microRNA response to epileptic preconditioning identifies miR-184 as a modulator of seizure-induced neuronal death. Exp Neurol. 2012;237:346–54.
Schratt GM, Tuebing F, Nigh EA, Kane CG, Sabatini ME, Kiebler M, et al. A brain-specific microRNA regulates dendritic spine development. Nature. 2006;439:283–9.
Jimenez-Mateos EM, Engel T, Merino-Serrais P, Fernaud-Espinosa I, Rodriguez-Alvarez N, Reynolds J, et al. Antagomirs targeting microRNA-134 increase hippocampal pyramidal neuron spine volume in vivo and protect against pilocarpine-induced status epilepticus. Brain Struct Funct. 2015;220(4):2387–99.
Wang XM, Jia RH, Wei D, Cui WY, Jiang W. MiR-134 blockade prevents status epilepticus like-activity and is neuroprotective in cultured hippocampal neurons. Neurosci Lett. 2014;572:20–5.
Scholer N, Langer C, Dohner H, Buske C, Kuchenbauer F. Serum microRNAs as a novel class of biomarkers: a comprehensive review of the literature. Exp Hematol. 2010;38:1126–30.
De Smaele E, Ferretti E, Gulino A. MicroRNAs as biomarkers for CNS cancer and other disorders. Brain Res. 2010;1338:100–11.
Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18:997–1006.
Fichtlscherer S, De Rosa S, Fox H, Schwietz T, Fischer A, Liebetrau C, et al. Circulating microRNAs in patients with coronary artery disease. Circ Res. 2010;107:677–84.
Corsten MF, Dennert R, Jochems S, Kuznetsova T, Devaux Y, Hofstra L, et al. Circulating MicroRNA-208b and MicroRNA-499 reflect myocardial damage in cardiovascular disease. Circ Cardiovasc Genet. 2010;3:499–506.
Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–9.
Jin XF, Wu N, Wang L, Li J. Circulating microRNAs: a novel class of potential biomarkers for diagnosing and prognosing central nervous system diseases. Cell Mol Neurobiol. 2013;33:601–13.
Reid G, Kirschner MB, van Zandwijk N. Circulating microRNAs: association with disease and potential use as biomarkers. Crit Rev Oncol Hematol. 2011;80:193–208.
Creemers EE, Tijsen AJ, Pinto YM. Circulating microRNAs: novel biomarkers and extracellular communicators in cardiovascular disease? Circ Res. 2012;110:483–95.
Mo MH, Chen L, Fu Y, Wang W, Fu SW. Cell-free circulating miRNA biomarkers in cancer. J Cancer Educ. 2012;3:432–48.
Janssen HL, Reesink HW, Lawitz EJ, Zeuzem S, Rodriguez-Torres M, Patel K, et al. Treatment of HCV infection by targeting microRNA. N Engl J Med. 2013;368:1685–94.
Boudreau RL, Rodriguez-Lebron E, Davidson BL. RNAi medicine for the brain: progresses and challenges. Hum Mol Genet. 2011;20:R21–7.
Davidson BL, McCray Jr PB. Current prospects for RNA interference-based therapies. Nat Rev Genet. 2011;12:329–40.
Acknowledgements
The authors apologize to those authors whose relevant work was not cited here. microRNA research in the authors’ group is currently supported by grants from Health Research Board (HRA-POR-2013-325), European Union Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 602130, Science Foundation Ireland (12/RC/2272, 12/COEN/18, 13/IA/1891, 14/ADV/RC2721), and Irish Research Council (GOIPD/2014/566).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Reschke, C.R., Henshall, D.C. (2015). microRNA and Epilepsy. In: Santulli, G. (eds) microRNA: Medical Evidence. Advances in Experimental Medicine and Biology, vol 888. Springer, Cham. https://doi.org/10.1007/978-3-319-22671-2_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-22671-2_4
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22670-5
Online ISBN: 978-3-319-22671-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)