Abstract
Injury to the extrahepatic biliary tree is uncommon, but also deadly given adjacent anatomy. Cholecystectomy is indicated for all trauma to the gallbladder. Full thickness common bile duct injuries generally necessitate a Roux-en-Y hepaticojejunostomy in the stable patient, whereas very minor injuries can occasionally be treated with primary repair. All patients displaying physiologic extremis should undergo initial damage control resuscitation/surgery by arresting ongoing hemorrhage and controlling the biliary fistula with an appropriate modality of drainage. Chronic biliary stenoses are managed in a manner similar to patients with a delayed diagnosis of bile duct injury. This chapter will outline the evidence and rationale behind each of these subject areas.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Despite their rarity, injuries to the extrahepatic biliary tree are always challenging and often deadly. More specifically, they occur in only 0.5 % of the subset of injured patients who actually require a laparotomy. In the context of trauma, the extrahepatic biliary tract is also a component of the anatomical region commonly referred to as the “surgical soul.” Whether you are a Trauma or Hepatobiliary surgeon, these injuries will engage all of your senses, test your technical skills, require the utmost focus, and demand great teamwork from you and your colleagues.
Extrahepatic Biliary Tract Injuries
Gallbladder Injuries
The dominant mechanism causing extrahepatic biliary tract injuries remains penetrating trauma (gunshots and stabbings). Despite its relatively protected location (surrounded by the liver, omentum, intestines, and thoracic cage), the vast majority of these injuries involve the gallbladder itself [1, 2]. This also explains the observation that gallbladder injuries are typically accompanied by trauma to additional organs within the torso [1, 3]. Fortunately, management is simple and follows the general axiom that all injuries to the gallbladder represent an absolute indication for subsequent cholecystectomy. This includes unusual cases of blunt injury where the gallbladder is filled with hemorrhage/clot, leading to cholecystitis secondary to a blocked cystic duct. Although primary repair and/or tube drainage is occasionally described in case series and dated textbooks, it is almost never indicated outside of a true damage control scenario for patients in the throes of physiologic extremis [1]. While the diagnosis of gallbladder trauma is most often confirmed during a laparotomy for associated injuries, which demand immediate operative intervention, ultrasonography and/or cross sectional imaging may be helpful diagnostic tools as well.
Acute Management of Trauma-Related Biliary Injuries
Although non-gallbladder, extrahepatic biliary tract injuries are also incredibly uncommon, the dominant and most urgent issue in the acute scenario remains trauma to other structures that reside in close proximity within the porta hepatis [4]. More specifically, concurrent injuries to the hepatic artery, portal vein, and/or vena cava must be addressed first [5]. While these injuries are not the focus of this chapter, they do require significant knowledge of regional anatomy as well as damage control and vascular reconstruction techniques [6–8]. The dominant challenge inherent in managing patients with biliary trauma is therefore addressing hemodynamic instability secondary to ongoing hemorrhage, as well as gastrointestinal leakage (duodenum, stomach, pancreas, liver) from regional structures. These patients often present in physiologic extremis and require damage control resuscitation techniques [6]. Early recognition of their critical condition, as well as immediate hemorrhage control, is essential to survival. Immediate, definitive repair of the biliary injury is not the emphasis in this scenario.
Once ongoing hemorrhage has been temporized, the surgeon can then begin to address the biliary tract injury itself. In patients who remain in shock and physiologic extremis due to concurrent trauma (i.e., major liver and/or vascular injuries), deploying damage control resuscitation principles is paramount [6]. This life-saving concept mandates early truncation of all operative interventions once persistent hemorrhage has been arrested and gastrointestinal contents are controlled. This typically includes intraperitoneal packing and the educated placement of closed suction drainage in the region of the injured bile duct to control any persistent bile leakage. These patients also often require negative suction wound therapy (i.e., temporary abdominal closure) to preserve fascial integrity and avoid abdominal compartment syndrome [6]. Once the patient’s abnormal physiology (coagulopathy, acidosis, hypothermia) has been reversed in the critical care suite, re-exploration can be initiated in the context of skilled surgeons with discrete experience operating on the biliary tract. In summary, the true damage control response to an injured and leaking biliary tract is adequate drainage and an eventual return to the operating theater with experienced assistance once patient physiology and hemodynamics are stabilized.
In cases of moderate patient stability and/or surgeon inexperience with biliary tract injuries, other temporizing measures include insertion of a soft T-tube into the site of injury [9]. This technique is simple and will control the biliary injury/fistula until the patient is ready for repair, or the team has included a member with advanced biliary knowledge. It should also be noted that intentional occlusion of the common bile duct in the event of a complete traumatic transection is not helpful. More specifically, upstream dilation of the proximal bile duct in preparation for an “easier” reconstruction does not occur in a predictable fashion. When occluded, this more often leads to necrosis of the distal duct and therefore an elevation of the injury to a more proximal location [10]. Impaired hepatic physiology may also ensue. Intentional occlusion of more proximal bile ducts (e.g., right or left hepatic ducts, secondary bile ducts) via suture ligature or clipping has also been described. Similarly, this misguided approach typically results in chronically obstructed hepatic segment(s), parenchymal atrophy, and most concerning, an infected (i.e., cholangitic) liver that eventually requires formal resection with a partial hepatectomy after prolonged patient suffering. Complete external drainage via soft catheters/tubes with a planned/delayed definitive reconstruction and/or resection is a much preferred option.
If the patient is completely stable and definitive repair of the biliary injury is contemplated, multiple options are available. It must be remembered however that these injuries typically occur in the context of normal sized (small, nondilated) bile ducts that often require advanced reconstruction techniques to avoid long-term biliary stenoses and/or occlusions. It should also be noted that textbooks and journals are littered with accounts of a complex hierarchy of operative interventions aimed at repairing partial bile duct injuries. These include, but are not limited to, the generous insertion of large T-tubes for small primary ductal repairs, cystic duct tissue rotations, gallbladder wall tissue transpositions, and saphenous vein or prosthetic material patches to close various bile duct defects. These maneuvers have largely been abandoned due to the high incidence of long-term stenosis. As a result, most experienced biliary surgeons recommend two dominant techniques . The first is a simple interrupted primary repair for small lacerations (5 or 6-0 PDS). This approach should only be considered in the context of non-gunshot and non-cautery injuries (i.e., no concern for the vascular integrity of the ductal wall). The second option is a Roux-en-y choledocho- or hepaticojejunostomy [4, 11, 12]. This technique is preferred in the context of ductal transections, significant ductal tissue loss, and/or complex lacerations of the extrahepatic bile duct.
Although tension-free end-to-end primary anastomoses have been advocated by some authors in the context of both laparoscopic cholecystectomy-related bile duct injuries and trauma-induced transections of the common bile duct, this approach is clearly associated with a higher risk of long-term ductal strictures [13–15]. Unlike the case with hepatic transplantation, these patients do not suffer the benefits of low stricture rates facilitated by chronic pharmacologic immunosuppression. It should also be noted that the concurrent insertion of a T-tube for “control” of the anastomosis is generally not necessary, and potentially problematic, in patients who are reconstructed with a hepaticojejunostomy by an experienced surgeon. Placing small T-tubes in normal sized bile ducts is fraught with difficulties (tearing the duct, occluding the ductal lumen, damaging the vascular supply, ejection of the T-tube) and therefore should be avoided if possible. Although most high-volume HPB surgeons do not utilize closed suction drainage for their hepaticojejunostomies or other biliary reconstructions, injury in the context of patients with additional trauma and physiologic stressors may provide an indication for drainage in some scenarios.
It should also be noted that the classic cholecystojejunostomy is a rarely required, but potentially helpful salvage maneuver in the scenario of a complete inability to restore biliary continuity from within the porta hepatis (e.g., extensive portal varices) [16]. Prior to performing this anastomosis however, patency of the cystic duct must be ensured by the presence of significant bile within the gallbladder itself and/or formal cholangiography.
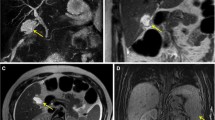
Another consideration of vital importance in selecting the correct biliary reconstruction option is the status of the right hepatic artery. It remains clear that concurrent injuries to the right hepatic artery lead to delayed strictures of the biliary-enteric anastomosis [17]. As a result, a high/proximal hepaticojejunostomy that incorporates the hilar plate (crossing arterial plexus) is essential to ensure durable long-term patency. Techniques such as a modified biliary hilum Carrel patch and/or Blumgart-Kelly anastomosis can be helpful [18] (Fig. 12.1). As a final note, the ability to dilate chronic strictures within the biliary tree using either endoscopic or percutaneous approaches (balloon and/or stent techniques) has improved substantially over the past decade. This has led to a re-contemplation of the potential role of end-to-end primary anastomoses in some scenarios, with the potential for salvage with a minimally invasive approach, should a stricture eventually manifest.
Blumgart-Kelly anastomosis . The anterior ductal wall sutures are placed through the bile duct first and then suspended superiorly to “open” the duct and allow excellent visualization of the posterior wall. Once the posterior wall sutures are placed and tied, the front wall is completed with the corresponding intestinal suture bites
Complex distal biliary injuries are treated with a pancreatoduodenectomy. Similarly, combined complex duodenal, pancreatic head and biliary injuries also benefit from a single stage pancreatoduodenectomy by an experienced surgeon. Young patients clearly have improved long-term quality of life measures if the injury is managed in a single definitive approach. Textbooks are ripe with descriptions of local repairs utilizing transduodenal sphincteroplasties, distal biliary diversions, and other exotic case report techniques. These procedures should be avoided unless the surgeon of record has significant expertise using them within the biliary tree. It must also be restated that the damage control and/or temporizing approach to distal biliary tract injuries remains controlled drainage and delayed resection and/or reconstruction by an experienced surgeon. Attempts at pancreatoduodenectomy in the immediate traumatic setting are not advocated unless absolutely necessary.
A final acute scenario of interest remains the patient who inadvertently requires or sustains complete occlusion of a major bile duct (common and/or right/left hepatic duct). This most commonly occurs when massive porta hepatis or hilar hemorrhage requires life-saving, nontargeted suture ligation. The salvage methodology for achieving biliary decompression in these patients remains insertion of a percutaneous transhepatic catheter [19]. These tubes provide both biliary drainage and cholangiographic planning for a delayed reconstruction. It must also be noted that in some centers where this technique is less commonly performed, the procedure may have to be delayed for up to 1 week to allow progressive dilation of the intrahepatic biliary tree and therefore easier targeting for our interventional radiology colleagues.
Delayed Diagnosis of Trauma-Related Biliary Tract Injuries
Unlike the acute diagnosis of extrahepatic biliary tract injuries that occur at the time of an urgent laparotomy for concurrent injuries (i.e., identification of bile within the peritoneal cavity), delayed diagnoses typically present as a consequence of bilomas in the setting of an otherwise sterile field. Patient symptoms will consist of nausea, mild right upper quadrant discomfort, and often an ileus. Their white blood cell count and bilirubin levels may also be elevated. These patients require identification of the biloma with either ultrasound or computed tomography, in addition to subsequent percutaneous drainage and cholangiography. In scenarios of very small partial wall common bile duct injuries, placement of an intrabiliary stent via ERCP may be sufficient. With any significant injury however, immediate control of sepsis and subsequent, appropriately timed exploration by an HPB surgeon are warranted [20]. These principles are analogous to those presented elsewhere in this book regarding the management of biliary injury incurred during cholecystectomy.
In the setting of physiologic stability, the delayed diagnosis of an extrahepatic biliary tract injury/stenosis mandates complete cholangiography (MRCP, tube cholangiogram) prior to any operative exploration [21]. Similar to bile duct injuries generated during a laparoscopic cholecystectomy, an experienced colleague and/or team approach is crucial to ensure a single successful repair and therefore a normal quality of life for the patient [20, 22]. It should also be noted that although the classification of extrahepatic biliary tree injuries (American Association for the Surgery of Trauma injury scale) is helpful with regard to a lexicon for communication and research, it does not correlate well with the potential level of difficulty predicted during biliary reconstruction for higher grade injuries (grades IV and V) [23] (Table 12.1).
Postoperative Management , Complications, and Follow-Up
The dominant long-term potential complications associated with biliary injuries and/or reconstructions remain stenosis of the biliary anastomosis and occasional biliary fistulas. Strictures are particularly plausible in the context of hepaticojejunostomies required for very youthful patients with a long life expectancy (i.e., the typical trauma patient). As a result, these operations mandate a detailed discussion with the patient prior to discharge (i.e., risks and symptoms of potential stenosis (cholangitis, jaundice)). Fortunately, chronic strictures in this scenario are often amenable to dilation with either an endoscopic or percutaneous approach given a significantly improved rate of success over the past decade [24, 25]. However, definitive surgical revision may be required for some.
Biliary fistulas may result from incomplete repairs (poor technique, progressive necrosis of tissue due to poor vascular supply), missed injuries, prolonged external drainage through a T-tube or drain site, and/or the omission or inability to ligate the distal bile duct in the context of more proximal biliary diversions. These leaks must be rapidly converted into controlled biliary fistulae, in combination with resolution of sepsis, optimized nutrition, and complete cholangiography (MRCP, drain cholangiography, ultrasound, ERCP). For chronic fistulae that do not close, operative intervention by an experienced biliary surgeon may be required. For those that do close, the patient must be counseled regarding potential signs and symptoms of long-term biliary strictures. Planned surveillance using cross-sectional imaging (e.g., CT) is not required for repaired biliary tract injuries (as opposed to splenic injuries). Repeat imaging should, instead, be based on any deterioration in laboratory tests or patient symptoms.
Conclusion
Injury to the extrahepatic biliary tree is unusual. Cholecystectomy is indicated for all trauma to the gallbladder. Full thickness common bile duct injuries require a Roux-en-Y hepaticojejunostomy in the stable patient, whereas very minor injuries can occasionally be treated with primary repair. All patients displaying physiologic extremis should undergo initial damage control resuscitation/surgery by arresting ongoing hemorrhage and controlling the biliary fistula with an appropriate modality of drainage. Chronic biliary stenoses can be managed in a manner similar to patients with a delayed diagnosis of bile duct injury (complete cholangiography, potential balloon or stent dilation, and/or operative biliary reconstruction by an experienced surgeon).
References
Ball CG, Dixon E, Kirkpatrick AW, et al. A decade of experience with injuries to the gallbladder. J Trauma Manag Outcomes. 2010;4:3.
Posner MC, Moore EE. Extrahepatic biliary injury: operative management plan. J Trauma. 1985;25(9):833–7.
Zellweger R, Navsaria PH, Hess F, et al. Gallbladder injuries as part of the spectrum of civilian abdominal trauma in South Africa. ANZ J Surg. 2005;75:559–61.
Feliciano DV. Biliary injuries as a result of blunt and penetrating trauma. Surg Clin North Am. 1994;74:897–907.
Jurkovich GJ, Hoyt DB, Moore FA, et al. Portal triad injuries. J Trauma. 1995;39(3):426–34.
Ball CG. Damage control resuscitation: history, theory and technique. Can J Surg. 2014;57(1):55–60.
Ball CG, Wyrzykowski AD, Nicholas JM, et al. A decade’s experience with balloon catheter tamponade for the emergency control of hemorrhage. J Trauma. 2011;70(2):330–3.
Ball CG, Kirkpatrick AW, Rajani RR, et al. Temporary intravascular shunts: when are we really using them according to the NTDB? Am Surg. 2009;75(7):605–7.
Pachter HL, Liang HG, Hofstetter SR. Liver and biliary tract trauma. Trauma. 2nd ed. Norwalk, CT: Appleton and Lange; 1991. p. 441.
Mercado MA, Chan C, Jacinto JC, et al. Voluntary and involuntary ligature of the bile duct in iatrogenic injuries: a nonadvisable approach. J Gastrointest Surg. 2008;12(6):1029–32.
Yoshimi F, Ikeda M, Oka D, Asato Y. Reconstruction of small bile ducts using a parachute technique. Hepatogastroenterology. 2002;49(47):1213–5.
Sutherland F, Dixon E. Extramucosal hepaticojejunostomy. Am J Surg. 2005;189(6):667–9.
Jablonska B. End-to-end ductal anastomosis in biliary reconstruction: indications and limitations. Can J Surg. 2014;57(4):271–7.
Ivatury RR, Rohman M, Nallathambi M, et al. The morbidity of injuries to the extrahepatic biliary system. J Trauma. 1985;25:967.
Stewart L, Way L. Bile duct injuries during laparoscopic cholecystectomy: Factors that influence the results of treatment. Arch Surg. 1995;130(10):1123–8.
Weintraub S, Grunspan M, Singer D. Hepaticocholecystomy and cholecystojejunostomy for bile drainage. A palliative procedure. Am J Surg. 1980;139(3):441–2.
Strasberg SM, Helton WS. An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB (Oxford). 2011;13(1):1–14.
Blumgart LH, Kelley CJ. Hepaticojejunostomy in benign and malignant high bile duct stricture: approaches to the left hepatic duct. Br J Surg. 1984;71(4):257–61.
Saad WE. Transhepatic techniques for accessing the biliary tree. Tech Vasc Interv Radiol. 2008;11(1):21–42.
Lillemoe KD. Current management of bile duct injury. Br J Surg. 2008;95(4):403–5.
Ejaz A, Spolverto G, Kim Y, et al. Long-term health-related quality of life after iatrogenic bile duct injury repair. J Am Coll Surg. 2014;219(5):923–32.
Lillemoe KD, Meltoon GB, Cameron JL, et al. Postoperative bile duct strictures: management and outcomes in the 1990s. Ann Surg. 2000;232:430–5.
American Association for the Surgery of Trauma. Extrahepatic biliary tree injury scale. Table 9. 2014. http://www.aast.org/Library/TraumaTools/InjuryScoringScales.aspx#tree
Costa Magna G, Pandolfi M, Mutignani M, et al. Long-term results of endoscopic management of postoperative bile duct strictures with increasing number of stents. Gastrointest Endosc. 2001;54:162–7.
Pinto-Pais T, Pinho R, Procena L, et al. Iatrogenic biliary in a patient with Roux-en-Y hepaticojejunostomy: stenting repair with a single-balloon enteroscopy-assisted ERCP. Endoscopy. 2014;46 Suppl 1:E506–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ball, C.G. (2015). Traumatic Biliary Strictures. In: Dixon, E., Vollmer Jr., C., May, G. (eds) Management of Benign Biliary Stenosis and Injury. Springer, Cham. https://doi.org/10.1007/978-3-319-22273-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-22273-8_12
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22272-1
Online ISBN: 978-3-319-22273-8
eBook Packages: MedicineMedicine (R0)