Abstract
It has long been recognized that complex crosstalk between the lung endoderm and its adjacent mesoderm is not only responsible firstly for the induction of the primitive lung anlagen, containing lung-specific progenitor or stem cells, from the floor of the primitive pharynx, but subsequently also for the induction and maintenance of distal populations of epithelial progenitors that are responsible for the stereotypic epithelial branching morphogenetic events that establish the pattern of the airways. Thus, temporo-spatial epithelial–mesenchymal crosstalk is essential for the correct stereotypic organization of the bronchial epithelial tree and subsequently, although not discussed in detail here, the alveoli. Within the mesenchyme, correct organization and function of the capillaries and nerves is likewise essential to achieve a fully functional lung. Molecular mechanisms of these interactions are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Mesenchyme Crosstalk to Epithelium
Alescio and Cassini [1] showed that ectopic branching of the embryonic mouse trachea can be induced by transplantation of distal lung mesenchyme to a more proximal location next to the tracheal epithelium , while conversely proximal epithelium can suppress distal branching. These classic experiments have been widely repeated by Shannon [2] and others so that the concept that distal lung mesenchyme can induce and control stereotypic branching morphogenesis of the airway epithelium has become well established.
Growth Factors in Epithelial–Mesenchymal Crosstalk
Subsequent work by ourselves and many other groups have further established that mesenchymal–epithelial induction of branching morphogenesis of the lung epithelium is mediated by peptide growth factors emanating from the mesenchyme and stimulating their cognate receptors upon the epithelium and vice versa. Among these factors BMP4, EGF, FGF7 and 10, HGF, PDGF, Shh, TGFβ, VEGF, and Wnt-β-catenin signaling have been found to play complex interlocking roles in this process (reviewed in [3–5]). FGF signaling is likewise a highly conserved branch induction mechanism, which is also inductive in fruit fly tracheal morphogenesis [6, 7].
Actually, I tend to think of growth factor-mediated branching morphogenesis as a default mechanism of airway epithelium . For example, FGF10 is capable of inducing vigorous but randomly directional branching of isolated embryonic lung epithelium in the absence of lung mesenchyme [8]. Therefore, stereotypy must be what is conferred by the lung mesenchyme, suppressing branching where it is not needed.
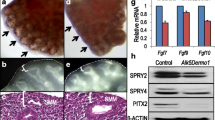
There are several theories about how this might work. One is that Turing morphogenetic gradients must exist within the lung mesenchyme, that chemoattract epithelial tips up the gradient to extend and branch in the direction of the ascending morphogenetic gradient [9]. This is in fact quite likely to be the case for the first few rounds of morphogenetic branching, because pools of FGF10 expression in the right place and at the right time can be identified by in situ hybridization, and ectopic branching can be induced by FGF10-soaked beads [10]. Moreover, the rate of branching can be manipulated by Sprouty genes that function as inducible inhibitors of FGF signaling [7]. However, it is not really known exactly how the subsequent rounds of stereotypic branching (up to 9 in mouse and 16 in human ), let alone the subsequent rounds of non-stereotypic, the so-called fractal branching (branches 9–11 in mouse, 16–21 in humans). Although we do know that EGF signaling must have something important to do with it, since EGF null mutation cuts the rate of branching in half [11]. Whereas, conversely increased luminal pressure brought on by tracheal obstruction increases branching via an FGF10-FGF receptor-dependent mechanism [12].
Epithelial–Mesenchymal Clocks
Another very interesting question is how does the epithelial branch timing clock work? We do now know from our recent experiments that rhythmic calcium waves within the epithelium that are driven from proximal bronchial epithelial pacemakers are important, because reversible inhibition of these waves with SERCA pump inhibitors can reversibly alter the rate of epithelial branching, thus determining the inter branch length [13]. Substances such as nicotine can also speed up branching morphogenesis and indeed overall lung maturation [14]. Certainly, there are important interspecies differences in the timing of stereotypic branching. In mouse, the branching clock strikes frequently so that interbranch lengths are short. Of course, the mature mouse lung is also relatively small. Interbranch lengths in human embryonic lung are much longer than mouse, which raises the question of why this might be and how interbranch lengths are matched to eventual respiratory surface area and body size. I wonder how these scaling rules work in whales and dinosaurs?
Mesenchyme is Not Boring But Busy
In the same era as Alescio and Cassini [1], when I was at medical school (1967–1973), the mesenchyme in general, we were taught, is regarded as rather a boring jelly-like substance in which not much was happening. Now, of course, we realize that the mesenchyme, particularly in the developing lung , is in fact a very busy place, with highly dynamic cell movements as well as comprising several essential tissues including blood vessels, lymphatics, immune cells, smooth muscle cells, and nerves. Our recent studies show that the tiny nerve axon projections that stereotypically accompany the developing airways in fact play an essential role in controlling branching morphogenesis, but not seemingly via parasympathetic neurotransmission [15]. It remains to be seen exactly how this system works. Likewise, we have shown that interfering with hemangioblast development into capillary networks by blocking VEGF signaling has important regional effects, not only on angio- and vasculogenesis, but also on epithelial branching morphogenesis in the embryonic lung. In particular, blockade of VEG signaling with a dominant negative decoy receptor approach impairs the induction of anterior epithelial branches from the major bronchi, which normally arise from populations of stem and/or progenitor cells expressing Sox9, which should arise at intervals along the anterior surface of the major bronchi [16, 17]. These condensations fail to appear in the presence of VEGF blockade and the absence of a correctly organized capillary vasculature.
Development of the smooth muscle cells within the mesenchyme of the lung also has important functional implications for the subsequent development of wheezing in childhood and indeed asthma. We have shown that some of the peripheral smooth muscle cells surrounding the bronchi actually arise from erstwhile FGF10 expressing cells, originally located within the peripheral mesenchyme, which translocate to surround and invest the distal bronchi [8]. Other populations of smooth muscle cells appear to originate from Sox9-positive mesenchymal progenitors that surround the distal trachea [18].
Pericytes are another class of mesenchymal cell that invest and maintain the capillary endothelium during embryonic development . We have recently discovered that pericytes arise from a distinct population of mesenchymal stem/progenitor cells that express Tbx4 and invade the lung from outside. Tbx4 expression also marks a subpopulation of smooth muscle cells that arrive in the embryonic lung [19].
Another important part of the lung where epithelial–mesenchymal crosstalk is key is the trachea . We and others recently reported that lung mesenchymal expression of Sox9 is essential for correct induction of the tracheal cartilages as well as for correct tracheal epithelial development [18].
An equally fundamental concept in epithelial–mesenchymal crosstalk in lung development is that timing and location are everything. This has been referred to as temporo-spatial control of inductive gene expression. Key examples of this include: retinoic acid signaling, in the absence of which no lung forms [20]; FGF10 signaling, in the absence of which no lung forms distal to the major bronchial origins [21]; and BMP4 signaling, which controls critical events at the time of transition to air breathing [22]. TGF beta signaling also plays important compartment and temporo-spatial specific roles in the epithelium versus the mesenchyme that may become manifest at later stages of lung development such as the alveolar phase [23].
Conclusion
In summary, temporo-spatial epithelial–mesenchymal crosstalk is essential for the correct stereotypic organization of the bronchial epithelial tree and subsequently, although not discussed in detail here, the alveoli . Within the mesenchyme, correct organization and function of the capillaries and nerves is likewise essential to achieve a fully functional lung (Fig. 2.1). Dysfunction of epithelial–mesenchymal crosstalk can lead to respiratory defects from absence of the lung through gross malformation of the lobes, through alveolar capillary dysplasia. Successful treatment of defects caused by defective epithelial–mesenchymal crosstalk has so far eluded small molecule approaches because of the exigency of repairing this complex signaling network. Surgical approaches such as controlled tracheal obstruction have achieved some mixed success, resulting in a large but grossly dysfunctional lung that is incapable of sustained gas exchange. Thus, significant challenges remain in fully parsing the mechanisms of epithelial–mesenchymal crosstalk in lung development . However, the effort may eventually pay off if we can re-entrain these developmental mechanisms to slow or reverse the decline in lung function that occurs over the advancing years of the full human life span.
Epithelial-mesenchymal-endothelial-nerve-matrix crosstalk in early mouse lung . This concept figure diagrams many of the known interactions between these compartments in lung morphogenesis. In the proximal lung, Sox9-positive mesenchymal progenitors play a key role in inducing tracheal cartilage, which in turn plays an inductive role on tracheal epithelial progenitors. In the first generation of airways, FGF10 signaling from the mesenchyme exerts an inductive and chemoattractive effect on the lung epithelium , which are both required for the subsequent induction of the distal epithelial progenitors as well as organization of all the distal lung structures. In the peripheral epithelium, FGF10 is still an important inductive signal for peripheral progenitors as well as for branching. FGF10 progenitors in the peripheral mesenchyme also act as progenitors for distal airway smooth muscle under the influence of Shh and BMP4 signaling. Wnt signaling from distal epithelium induces fibronectin to be laid down in potential distal clefts and this is essential for cleft formation. The early pulmonary arteries connect with early distal capillaries that form from hemangioblasts under the control of VEGF secreted by the epithelium. The formation of capillary plexi is likewise essential for the sprouting of side branches from condensation so Sox9-positive epithelial progenitor cells . Sympathetic nerve fibers arise from ganglia in the mediastinum, cross the proximal airway and early pulmonary arteries in a stereotypic manner and then follow the superior surface of the airway all the way to the periphery of the lung. Both nerve twigs and single capillary branches can be found between each lung epithelial cleft. FGF9 is expressed by the primitive mesothelium and induces FGF10 within the subjacent distal mesenchyme. Calcium ion waves arise from pacemakers in the mediastinum and proximal bronchi and pass down the bronchi toward the periphery, orchestrating distal-wards peristaltic waves that increase pressure within the peripheral airway tips. Peripheral tip progenitors can be identified by the co-expression of large number of characteristic transcriptional factors, growth factor receptors, and downstream signaling molecules that control their behavior
References
Alescio T, Cassini A (1962) Induction in vitro of tracheal buds by pulmonary mesenchyme grafted on tracheal epithelium. J Exp Zool 150:83–94
Shannon JM (1994) Induction of alveolar type II cell differentiation in fetal tracheal epithelium by grafted distal lung mesenchyme. Dev Biol 166(2):600–614
Warburton D, Schwarz M, Tefft D, Flores-Delgado G, Anderson KD, Cardoso WV (2000) The molecular basis of lung morphogenesis. Mech Dev 92(1):55–81
Warburton D, Bellusci S, Del Moral PM, Kaartinen V, Lee M, Tefft D, Shi W (2003) Growth factor signaling in lung morphogenetic centers: automaticity, stereotypy and symmetry. Respir Res 4:5
Warburton D, El-Hashash A, Carraro G, Tiozzo C, Sala F, Rogers O et al (2010) Lung organogenesis. Curr Top Dev Biol 90:73–158
Tefft JD, Lee M, Smith S, Leinwand M, Zhao J, Bringas P Jr et al (1999) Conserved function of mSpry-2, a murine homolog of Drosophila sprouty, which negatively modulates respiratory organogenesis. Curr Biol 9(4):219–222
Mailleux AA, Tefft D, Ndiaye D, Itoh N, Thiery JP, Warburton D, Bellusci S (2001) Evidence that SPROUTY2 functions as an inhibitor of mouse embryonic lung growth and morphogenesis. Mech Dev 102(1–2):81–94
Ramasamy SK, Mailleux AA, Gupte VV, Mata F, Sala FG, Veltmaat JM et al (2007) Fgf10 dosage is critical for the amplification of epithelial cell progenitors and for the formation of multiple mesenchymal lineages during lung development. Dev Biol 307(2):237–247
Warburton D (2008) Developmental biology: order in the lung. Nature 453(7196):733–735
Park WY, Miranda B, Lebeche D, Hashimoto G, Cardoso WV (1998) FGF-10 is a chemotactic factor for distal epithelial buds during lung development. Dev Biol 201(2):125–134
Miettinen PJ, Warburton D, Bu D, Zhao JS, Berger JE, Minoo P et al (1997) Impaired lung branching morphogenesis in the absence of functional EGF receptor. Dev Biol 186(2):224–236
Unbekandt M, del Moral PM, Sala FG, Bellusci S, Warburton D, Fleury V (2008) Tracheal occlusion increases the rate of epithelial branching of embryonic mouse lung via the FGF10-FGFR2b-Sprouty2 pathway. Mech Dev 125(3–4):314–324
Jesudason EC, Keshet E, Warburton D (2010) Entrained pulmonary clocks: epithelium and vasculature keeping pace. Am J Physiol Lung Cell Mol Physiol 299(4):L453–L454
Wuenschell CW, Sunday ME, Singh G, Minoo P, Slavkin HC, Warburton D (1996) Embryonic mouse lung epithelial progenitor cells co-express immunohistochemical markers of diverse mature cell lineages. J Histochem Cytochem 44(2):113–123
Bower DV, Lee HK, Lansford R, Zinn K, Warburton D, Fraser SE, Jesudason EC (2014) Airway branching has conserved needs for local parasympathetic innervation but not neurotransmission. BMC Biol 12(1):92
Del Moral PM, Sala FG, Tefft D, Shi W, Keshet E, Bellusci S, Warburton D (2006) VEGF-A signaling through Flk-1 is a critical facilitator of early embryonic lung epithelial to endothelial crosstalk and branching morphogenesis. Dev Biol 290(1):177–188
Lazarus A, Del-Moral PM, Ilovich O, Mishani E, Warburton D, Keshet E (2011) A perfusion-independent role of blood vessels in determining branching stereotypy of lung airways. Development 138(11):2359–2368
Turcatel G, Rubin N, Menke DB, Martin G, Shi W, Warburton D (2013) Lung mesenchymal expression of Sox9 plays a critical role in tracheal development. BMC Biol 11:117
Zhang W, Menke DB, Jiang M, Chen H, Warburton D, Turcatel G et al (2013) Spatial-temporal targeting of lung-specific mesenchyme by a Tbx4 enhancer. BMC Biol 11:111
Chen F, Cao Y, Qian J, Shao F, Niederreither K, Cardoso WV (2010) A retinoic acid-dependent network in the foregut controls formation of the mouse lung primordium. J Clin Invest 120(6):2040–2048
Min H, Danilenko DM, Scully SA, Bolon B, Ring BD, Tarpley JE et al (1998) Fgf-10 is required for both limb and lung development and exhibits striking functional similarity to Drosophila branchless. Genes Dev 12(20):3156–3161
Sun J, Chen H, Chen C, Whitsett JA, Mishina Y, Bringas P Jr et al (2008) Prenatal lung epithelial cell-specific abrogation of Alk3-bone morphogenetic protein signaling causes neonatal respiratory distress by disrupting distal airway formation. Am J Pathol 172(3):571–582
Chen H, Zhuang F, Liu YH, Xu B, Del Moral P, Deng W et al (2008) TGF-beta receptor II in epithelia versus mesenchyme plays distinct roles in the developing lung. Eur Respir J 32(2):285–295
Acknowledgements
D.W. wishes to thank the NIH and, in particular, the US and UK taxpayers who over many years have provided continual support for his education, career development , and for the body of work summarized briefly here. As this is a short monograph, D.W. wishes to apologize for not having room to mention the many inspirational papers and important contributions by other colleagues in the field, but refers the reader to publications wherein he has reviewed as many as possible of them elsewhere.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Warburton, D. (2015). Epithelial–Mesenchymal Crosstalk in Lung Development. In: Bertoncello, I. (eds) Stem Cells in the Lung. Stem Cell Biology and Regenerative Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-21082-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-21082-7_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21081-0
Online ISBN: 978-3-319-21082-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)