Abstract
This chapter focuses on the IT capabilities required by patient-centered medical homes, including electronic registries and associated applications that enable care teams to automate processes and provide continuous care to their patient populations. In addition, the chapter explores new technology options, including patient portals, remote monitoring, mobile health apps, and cognitive computing. Our goal is to show how patient-centered medical homes can use automation tools, analytics, and big data to improve population health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Patient centered medical home
- PCMH
- Population health
- Healthcare transformation primary care transformation
- Medical home
- Primary care Health It in PCMH
- Health it in population health management
1 Introduction
As chronic disease management consumes over three-quarters of US health costs [5], there is a need to redesign primary care, to change the emphasis from episodic acute care to a continuous, comprehensive preventive approach, to improve health and reduce costs [44]. The core of this redesign is the patient-centered medical home (PCMH). The PCMH model [3], a building block of Accountable Care Organizations (ACOs), organizes and optimizes care across time and medical neighborhoods (local hospitals, consultants and services) (Grundy et al. [16]), and comprises 20–25 % of US primary care practices.
2 The Patient Centered Medical Home
The PCMH provides comprehensive primary care based on ongoing, stable relationships between patients and physician-directed integrated care teams. PCMHs charge is to enhance access, coordinate care and improve quality through the use of disease registries and health information technology [26]. The components of a PCMH [3, 27] include:
-
A physician-led primary care provider/team that provides first contact and high-quality, continuous, comprehensive care for and in partnership with patients and families
-
Patient-centered care with continuous (24/7) access to care providers
-
Care coordination across time, settings (inpatient/ambulatory) and services
-
Formal recognition: certification and reimbursement that reflects the value of these services
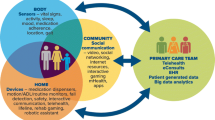
3 Physician-Led Care Teams
PCMHs use a physician-led, multidisciplinary (nurses, managers, health coaches, and others), team-based care model to ensure that all patients are cared for in the right place, at the right time, and in the manner most appropriate to the patient [25] to help them navigate the system and achieve agreed-upon health goals. Teams may be broadened to include professionals in the home, including specialists (especially behavioral health services), home health nurses, educators, therapists, pharmacists, social workers and increasingly, family caregivers [27, 28].
4 Patient Access
A National Committee on Quality Assurance (NCQA) recognized PCMH must provide:
-
Timely appointments and enhanced access to care patients (same-day appointments, extended hours) and self-scheduling
-
Access to clinical advice on a 24/7 access. Clinicians on call must have access to the EHR with phone or secure messaging
These functions may be provided through a patient portal through which patients must be able to schedule appointments, refill prescriptions, viewing lab results and access records.
5 Care Coordination
Care coordination, a PCMH requirement, is assurance of a patient’s navigation through the medical neighborhood to reach specified and agreed-upon care plan goals. The assignment of roles and tasks to specific stakeholders (patient, provider, team members, consultants, service providers) helps to improve outcomes and to reduce waste and inefficiency. Care coordination extends the care team and requires the cooperation of all stakeholders in the medical neighborhood providing services to the patient. As the health status of the patient evolves, revisions in the care plan must be shared with all participants in a timely fashion.
-
Test and results tracking and follow-up
PCMHs must record test (laboratory, imaging, etc.) orders in an EHR and capture and store results in structured data fields. NCQA also requires tracking of and follow-up on all ordered tests, which may be supported by EHR-S alerts for missing results. Another supporting EHR-S functionality is providing patient access to results and to information about their meaning [6].
-
Referrals and follow-up
PCMHs must send electronic summaries of care that include the care plan and pertinent test results to other providers in more than 50 % of referrals (This is also a requirement of Stage 2 Meaningful Use). Referrals must be tracked until consultant reports are received. Some EHRs have features that allow this to be done automatically. While NCQA-recognized PCMHs meet these referral requirements, the online exchange of health information continues to be problematic.
-
Care transitions
PCMHs must exchange key clinical information electronically with other care providers, such as hospitals, EDs, and nursing homes, at transitions of care. They must identify patients with unplanned hospital and emergency department admissions, share clinical information with admitting hospitals and EDs and consistently obtain patient discharge summaries.
Although, many hospitals still do not send timely discharge summaries to primary care physicians, a few institutions have modified their admission-discharge-transfer (ADT) systems to let patients’ doctors know when they’ve been admitted and discharged (early notification system).
6 Formal Recognition
While several organizations certify patient-centered medical homes, the National Committee on Quality Assurance (NCQA) is the principal agency for PCMH recognition [13]. As of September 2014, NCQA recognized 8,112 practice sites encompassing 40,841 clinicians as PCMHs [34]. By November 2014, close to a quarter of US primary care physicians were at some stage of creating a PCMH. This growth is fueled by financial incentives from health plans that offer higher payment rates, care coordination fees, pay for performance, and shared savings [13] for recognized PCMHs. As of 2012, over 90 insurers recognized PCMHs and over four million Blue Cross Blue Shield members in 39 states were served by a PCMH [36]. A 2013 survey counted 114 payer reform initiatives for PCMHs, covering 20 million lives [13], with Medicare and Veterans Health pilots underway [36, 24].
7 Impact on Practice
Research and industry studies have demonstrated strengths and challenges in implementation of the PCMH model:
-
Strong results
Payers have focused on the PCMH model because it saves them more than it costs. United Healthcare, for example, recently announced that its medical home programs in four states showed average third-year net savings of 6.2 % of medical costs, resulting in a return on investment of 6:1 [49]. Similarly, a medical home pilot at the UPMC Health Plan in Pittsburgh yielded an ROI of 160 % [42]. And Geisinger Health System (which includes a health plan) estimated its net savings from its PCMH model at $3.7 million, for a return on investment of more than 2:1 [15].
A recent peer-reviewed study found that PCMHs reduced Medicare payments by an average of $325 per patient, compared to a comparison group of non-PCMH practices. ED visits dropped by 7 % for the PCMHs, and hospitalizations of their sickest patients fell 4 %, although overall hospital admissions did not decline [33].
Much of the savings associated with the PCMH model come from avoided ED visits and hospitalizations. According to a summary of peer-reviewed PCMH studies by the Patient-Centered Primary Care Collaborative (PCPCC), 61 % of these studies reported fewer ED visits, 31 % reported fewer hospital admissions, and 13 % reported fewer readmissions [31]. The PCMH is also associated with improved access and quality. The PCPCC says that 31 % of the studies it reviewed showed improved patient access, 23 % reported higher patient satisfaction, 31 % found an increase in preventive services, and 31 % registered improvements in population health [31].
-
Areas for improvement
Not all PCMH studies have shown positive results. A RAND study of an early multi-payer PCMH [7] initiative in Pennsylvania found that the pilot was associated with improvement on only one of 11 quality measures and was not associated with lower ED or hospital utilization or a reduction in total costs over 3 years [14]. But a commentary by people involved in the program suggested that the results of this study might have “oversimplified” the experience of the Pennsylvania Chronic Care Initiative. The study failed to capture improvements in important intermediate outcomes such as blood pressure, LDL cholesterol and blood sugar control in diabetic patients, the authors said. Also, they pointed out, the program had initially made a mistake by not allocating funds to hire nurse care managers for high-risk patients—an oversight that was later corrected [8].
8 Population Health Management
By emphasizing continuous proactive care and providing collective information about the ongoing health of patients they serve, PCMHs offer the opportunity to manage and improve population health. Population health is defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within a group” [23].
Practice-based population health (PBPH) management uses information on specified subgroups of patients within one or a group of practices to improve the overall care and clinical outcomes of all patients within that practice ([2], 6).
Population health also depends on other factors, including health literacy, socioeconomic status, geographical location, access to care, transportation, and the physical environment in which patients live [30]. Population health management (PHM) has several domains:
-
Identification and characterization of subgroups of patients to stratify risk
-
Guidance and support for patients and providers to assure adherence
-
Measurement and feedback on practice patterns to improve performance
-
Information sharing among stakeholders to assure transparency and improve quality and safety
9 Identification, Characterization and Risk Stratification
The first step in managing population health of a practice is assessment and stratification of the health risks within the practice’s patient population. One method is to screen all patients proactively (health risk assessment, HRA) via questionnaires that may be distributed online at the PCMH level. If a PCMH is associated with a registry, health analytics may be able to use known indicators to identify patients at high risk [18]. Typically, 5 % of a patient population accounts for about 50 % of its health costs for a given risk [10].
10 Guidance and Support for Patients and Providers
The next step in PBPH is to identify gaps in preventive and chronic care for patients identified in population-wide registries. Analytics can identify patients that are overdue for specific services and can link them to their PCMH provider teams, customized to match the treatment preferences of patients and practices. Combined with automated messaging to patients about preventive or chronic care, analytic forecasting has been shown to increase patient adherence (Rai, et al. 2011). Combined with pre-visit prompts to providers and managers, practices can proactively assure that patients receive all appropriate, timely and up-to-date care during visits [21]. Examples of some organizations using registries today to identify patient care gaps include Group Health, Prevea and the Northeast Georgia Physicians Group.
11 Measurement and Feedback on Practice Patterns
An area of central importance in PBPH and PCMH management is ongoing measurement of practice performance, resource utilization and costs.
-
Disease-specific care quality
Beginning with disease-specific, risk prevalence data on populations within a registry (such as diabetes or hypertension), completion rates for clinical goals (HbA1c levels, BP measurements) and short and/or long-term health outcomes (hospitalizations, adverse events) for patients can be measured to assess performance of PCMHs and larger organizations on disease-specific targets. Registry analytics can drill down to completion of health goals and outcomes as linked to specific providers, practices or subcategories of patients and provide feedback to providers and care teams for lifelong learning and practice improvement. For long-term outcomes, PCMHs must link clinical data (HbA1c levels, BP measures) with patient-reported data (functional status, self-perceived health) and perceptions about the quality of health and the care received.
-
Utilization and Care Costs
Associated with performance measurement is cost management. Cost metrics are of particular importance if an organization or practice is providing care for patient populations at higher risk for high-cost care (or for other financial loss, ACO two-sided model). Economic forecasting of population care costs (how many patients will likely need expensive care) based on clinical and claims data can help guide organizations to allocate resources to meet the needs of high-cost segments and conditions within the population to anticipate and mitigate costs of Emergency Departments and hospital admissions.
12 Information Sharing Among Stakeholders
A key IT functionality needed in PBPH is timely and organized communication among stakeholders. Within the PCMH, EHR systems can facilitate internal communications and tasking, using alerts and secure messaging (via patient portals). Health information exchanges (HIEs) offer conduits for record sharing with other stakeholders in medical neighborhoods (however such HIEs and the protocols that support sharing (i.e., the Direct Protocol) are not yet widespread in the US).
Communication is essential in care transitions such as hospital admissions and discharges. Examples include:
-
Hospital ADT alerts to PCMHs (Private communication: Tim Pletcher, CEO, Michigan Health Information Network) within a region to facilitate early care coordination for unexpected admissions
-
Electronic messages to patients shortly after a hospital discharge to ask if they have questions about instructions or medications and to assure their connection/follow up to their PCMH [18].
-
The Michigan Health Information Network (MiHIN) uses ADT feeds from hospitals to provide alerts to physicians across the state [39].
13 Health Information Technology in PHM and The PCMH
PCMH certification criteria emphasizes health IT measures related to access and electronic communication, patient tracking and registry functions, care management, patient self-management support, electronic prescribing, test tracking, referral tracking and performance reporting. NCQA Level 3 PCMH recognition is a requisite by payers for financial incentives (NCQA 2014). Recommended health information technology functionalities for achieving PHM [43] have been articulated.
14 Medical Home Technologies and PHM
-
Electronic health records, necessary but not sufficient
EHR systems are indispensable to providing the scope of care [19, 32] required for PCMH certification, but current systems lack complete functionalities needed for PHM. Limitations include: inability to generate population-based reports easily; problems in presenting usable alerts and reminders; inability to capture data on preventive care; and non- interoperability between different EHR systems [2]. In addition, longitudinal care plans are not used [12] and while systems may be able to alert providers about gaps in care, they do not link to relevant clinical patient data [29].
-
Automation of clerical functions, essential
It has been calculated that a “manual” PCMH requires 4.25 FTE staff members per FTE physician, 1.57 staffers more than the average primary care doctor uses in a non-PCMH practice. Most of this difference represents the hiring of nurse care managers [35]. At Prevea Health [37], a multispecialty group in Green Bay, Wisconsin, automation enables managers to cover two to three times as many patients as possible with manual methods, with time savings in completion of routine tasks such as chart preparation and patient follow-up communications. Prior to deployment of the solution, managers spent an average of 188 min per high-risk patient (47 min searching the EHR for information, 2.5 patients per day). After implementation, they could process an average of 6.5 patients per day [40]. In addition to making the scope of PCMH care feasible, automated functions can make teams efficient and cost-effective [4].
-
Electronic communication, efficiency and outcomes
EHR system-based secure messaging and telephone calls enhance patient access and in-person visits. Patients are contacted in advance of visits to clarify concerns and expectations. Providers reviewed electronic records, including care gap alerts before each visit. A pilot study in the Seattle Group Health HMO found 6 % fewer in-person visits, 80 % more secure message threads and 5 % more telephone encounters with providers than without these tools [41]. Patient communication through email, secure messaging and access through practice portals are key components to improving PCMH outcomes.
-
Cognitive computing, great potential
“Cognitive computing” or harnessing the power of supercomputers to support care has great potential that is being explored and tested. One potential is as a pre-processor of current medical knowledge and literature to provide clinicians with answers and syntheses based on evidence to difficult questions. Another is to provide clinical decision support based not only on discrete data, but also unstructured information that forms about 80 % of the information stored in EHRs [1, 9, 22] to support diagnosis and management of individual patients with the potential to incorporate and integrate data from many other sources, such as geographical and income data, that have a bearing on population health, as well as the treatment of individual patients [46]. As an example, the Carilion Clinic Healthcare System in Roanoke, Va has used IBM Watson technology’s [11, 20] predictive modeling power to process structured and natural language data from the EHR. From 3 years’ data, Watson identified 8,500 patients at-risk for congestive heart failure, a leading source of the healthcare system’s costs.
15 PHM Technologies Beyond the Medical Home
-
Patient Registries and Analytics
PCMH level analytics are a key enabler to help care teams manage patients effectively and efficiently [21]. By applying analytical algorithms to EHR and claims data, teams can identify and track cohorts of patients by risk, adherence and appropriate medication use. Multimodal (secure messaging, phone) automated messaging can remind patients of appointments, prescriptions and other follow ups.
One major goal of care is to reduce exacerbations of high-risk conditions that lead to ED visits or hospitalizations. Analytics can produce registry-based summaries about patient care gaps in groups, and prioritize cases re: proactive care manager interventions for high-risk patients. Depending on the PCMH’s stage of technology adoption, they may conduct such programs for medium-risk and low-risk patients. Across the entire population, they endeavor to engage patients in managing their own health [21]. For example, different intervention programs might be aimed at those with Type 1 diabetes mellitus (DM), Type 2 DM, Type 2 DM plus hypertension, or poorly controlled Type 2 DM, with different educational materials and self-care recommendations sent to patients in each cohort.
Electronic registries link patient data about individuals to temporal clinical data from multiple sources (PCMH, laboratory, pharmacy, etc.) and allows for aggregation to generate knowledge about populations. In addition to helping practices identify patients at risk and to guide care and education, registries can, with appropriate analytical tools, provide practices and health care organizations with data and predictive insights for health risk stratification, identification of gaps in care, quality reporting and financial/performance evaluation. Importantly, aggregated data from multiple registries can also facilitate regional collaboration [21].
Areas where health IT has improved the efficiency of PCMH processes center on care coordination and communication tasks within a given “medical neighborhood” of a primary care based practice. Published examples of registry-enabled medical neighborhoods include the Jackson Health Network in Michigan [17] and the Northeast Georgia Physicians [38].
-
Remote patient monitoring
This modality has been used most frequently with high-risk patients, such as those with congestive heart failure or for post-surgical home recovery, but has also been used successfully to support patients with day-to-day management of chronic disease (diabetes and hypertension, [48]). PCMH care teams may use this kind of data—which must be screened for relevance—to provide automated or live feedback to patients on their health management. In addition to tele-monitoring systems, today numerous mobile apps allow patients to self-monitor their conditions using smartphones. Increasingly, these mobile apps are being used in conjunction with portable devices such as glucometers, but integration of these patient-generated data into physicians’ EHR systems is still low due to interoperability obstacles [47], as well as physicians’ concerns over certification of these patient data for safety, accuracy and effectiveness.
-
Remote consultations
No longer relegated to dedicated tele-health applications, clinician/patient remote visits are increasingly taking advantage of the availability of high-bandwidth video, well as consumer available apps on any Smart phone, such as “FaceTime” to do a “home” visit or consultation [45]. Increasingly, this form of consultation is being accepted by payers in geographic areas with low availability of specialty services, or for home visits for patients who are homebound.
16 Conclusion
The PCMH is recognized as an engine of healthcare reform. It is a building block of Accountable Care Organizations, the core of clinically integrated networks, and arguably the care delivery model that has the greatest potential to organize medical neighborhoods. PCMHs are gaining traction among primary care physicians as they cope with rising demands for services and a fast-changing reimbursement system. Information technology is an essential enabler for this transformative care delivery model as well as to achieve the Triple Aim goals in population health management. As detailed in this chapter, population health cannot be managed at an affordable cost unless providers have the needed information technology tools to apply automation to routine tasks. Moreover, the PCMH needs analytics that permit it to stratify patients by health risk, identify their care gaps, and enable care managers to intervene quickly with high-risk patients. Analytics are also essential to performance evaluation and cost management.
In conclusion, due to current lack of interoperability among EHRs and EHR systems, health IT has a long way to go before it can provide all of the support that PCMHs will need for population health management and care coordination. But, without health IT, a PCMH would have very limited capabilities. So the two trends are expected to continue evolving together.
References
Agency for Healthcare Research and Quality (AHRQ). Clinical Decision Support (CDS) initiative overview. 2014. http://healthit.ahrq.gov/ahrq-funded-projects/clinical-decision-support-cds-initiative. Accessed 19 Apr 2015.
Agency for Healthcare Research and Quality (AHRQ). Practice-based population health: information technology to support transformation to proactive primary care. 2010. http://pcmh.ahrq.gov/sites/default/files/attachments/Information%20Technology%20to%20Support%20Transformation%20to%20Proactive%20Primary%20Care.pdf.
American Academy of Family Physicians (AAFP) AAoPA, American College of Physicians (ACP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home. 2007; http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Accessed 19 Apr 2015
Berner ES, Burkhardt JH, Panjamapirom A, Ray MN. Cost implications of human and automated follow-Up in ambulatory care. Am J Manage Care. 2014;20(11 Spec No. 17):SP531–40.
Centers for Disease Control and Prevention (CDC). Chronic diseases, the power to prevent, the call to control: at a glance. 2009. http://www.cdc.gov/chronicdisease/resources/publications/aag/chronic.htm.
Centers for Medicare and Medicaid Services (CMS). EHR incentive program. 2014. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/August2014_SummaryReport.pdf.
Centers for Medicare and Medicaid (CMS). Multi-payer primary care practice demonstration fact sheet. 2012. http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads/mapcpdemo_Factsheet.pdf. Accessed 19 Apr 2015.
Crimm A. and Liss D. Patient-centered medical home evaluations: let’s keep them all in context. Health affairs blog. 2014. http://healthaffairs.org/blog/2014/05/21/patient-centered-medical-home-evaluations-lets-keep-them-all-in-context/.
DataMark Inc. Unstructured Data in Electronic Health Record (EHR) systems: challenges and Solutions. white paper. http://www.datamark.net/uploads/files/unstructured_ehr_data_white_paper.pdf (Oct 2013).
Duncan I. Healthcare risk adjustment and predictive modeling. Winsted: ACTEX Publications; 2011.
Lindsey D. “Carilion Clinic Using ”Watson“ Technology to Identify At-Ris, Patients,” Becker’s Health IT and CIO Review. 2014. http://www.beckershospitalreview.com/healthcare-information-technology/carilion-clinic-using-watson-technology-to-identify-at-risk-patients.html.
Dykes PC, Samal L, Donahue M, Greenberg JO, Hurley AC, Hassan O, O’Malley TA, Venkatesh AK, Volk LA, Bates D. A patient-centered longitudinal care plan: vision versus reality. J Am Med Inf Assoc. doi:http://dx.doi.org/10.1136/amiajnl-2013-002454 1082-1090. First published online: 1 Nov 2014.
Edwards ST, Bitton A, Hong J, Landon BE. Patient-centered medical home initiatives expanded in 2009–2013: providers, patients and payment incentives increased. Health Aff. 2014;33(10):1823–31. doi:10.1377/hlthaff.2014.0351.
Friedberg MW, Schneider EC, Rosenthal MB, Volpp KG, Werner RM. Association between participating in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014;311(8):815–25. doi:10.1001/jama.2014.353.
Grumbach K, Bodenheimer T, Grundy P. The outcomes of implementing patient-centered medical home demonstrations: a review of the evidence on quality, access and costs from recent prospective evaluation studies Aug 2009, paper prepared for PCPCC, Washington DC.
Grundy P, Hagan KR, Hansen JC, Grumbach K. The multi-stakeholder movement for primary care renewal and reform. Health Aff. 2010;29(5):791–8.
Richard H. Population health management requires automation. Group Pract J. 2011. http://www3.phytel.com/Libraries/In-the-News-PDFs/Population-Health-Management-Requires-Automation.sflb.ashx.
Hodach R, Handmaker K. Population health management technologies for accountable care. Phytel white paper. 2013. 12.
Hsiao Chun-Ju, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States. 2001–2013, NCHS Data Brief, No. 143. 2014. http://www.cdc.gov/nchs/data/databriefs/db143.htm.
IBM. Implement watson: healthcare. 2015. URL: http://www.ibm.com/smarterplanet/us/en/ibmwatson/implement-watson.html. Last Accessed 25 Mar 2015.
Institute for Health Technology Transformation (IHTT). Population health management: a roadmap for provider-based automation in a New Era of healthcare. 2012. http://ihealthtran.com/pdf/PHMReport.pdf.
Kesselheim AS, Cresswell K, Phansalkar S, Bates DW, Sheikh A. Clinical decision support systems could be modified to reduce ‘Alert Fatigue’ while still minimizing the risk of litigation. Health Aff. 2011;30(12):2310–7. doi:10.1377/hlthaff.2010.1111.
Kindig D, Stoddart G. What is population health? Am J Public Health. 2003;93:380–3.
Klein S. The veterans health administration: implementing patient-centered medical homes in the nation’s largest integrated delivery System. 2011. The Commonwealth Fund. http://www.commonwealthfund.org/~/media/Files/Publications/Case%20Study/2011/Sep/1537_Klein_veterans_hlt_admin_case%20study.pdf. Accessed 19 Apr 2015.
Margolius D, Bodenheimer T. Transforming primary care: from past practice to practice of the future. Health Aff. 2010;29(5):779–84.
Nash D. Healthcare reform’s Rx for primary care, MedPage Today, Aug. 18, 2010. Accessed at http://www.medpagetoday.com/Columns/21750.
NCQA. Patient-centered medical homes fact sheet. 2013. http://www.ncqa.org/Portals/0/Public%20Policy/2013%20PDFS/pcmh%202011%20fact%20sheet.pdf. Accessed 19 Apr 2015.
NCQA. PCMH 2011-PCMH 2014 crosswalk. (no date). http://www.ncqa.org/Programs/Recognition/Practices/PatientCenteredMedicalHomePCMH/PCMH2011PCMH2014Crosswalk.aspx. Accessed 19 Apr 2015.
Nelson R. Your EHR needs a population health management system. 2013. Kevin MD. http://www.kevinmd.com/blog/2013/02/ehr-population-health-management-system.html.
Nguyen OK, Chan CV, Makam A, Stieglitz H, Amarasingham R. Envisioning a social-health information exchange as a platform to support a patient-centered medical neighborhood: a feasibility study. J Gen Intern Med. 2015;30(1):60–7.
Nielsen M. Show me the sata: do patient-centered medical homes work? PCPCC presentation, 9 June 2014.
Nutting PA, Crabtree BJ, Miller WL, Stange KC, Stewart E, Jaen C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff. 2011;30(3):439–45.
O’Kane ME. Are medical homes an answer to health care’s cost problem? 2014. NCQA Blog. http://blog.ncqa.org/medical-homes-answer-health-cares-cost-problem/?utm_source=SilverpopMailing&utm_medium=email&utm_campaign=Recognition%20Notes%201.8.14 %20(1)%20B&utm_content.
O’Kane ME, Barr MS, Scholle SH. Patient-centered medical homes save money and improve care. 2014. NCQA presentation. http://www.ncqa.org/Portals/0/Newsroom/PCMH%20Research%20Slides_9-3-14_FINAL_v2.pdf.
Patel MS, Arron MJ, Sinsky TA, Green EH, Baker DW, Bowen JL., Day S. Estimating the staffing infrastructure for a patient-centered medical home. Am J Managed Care. 1;19:N6. 2013. Accessed at http://www.ajmc.com/publications/issue/2013/2013-1-vol19-n6/estimating-the-staffing-infrastructure-for-a-patient-centered-medical-home/1.
Patient Centered Primary Care Collaborative (PCPCC). Benefits of implementing the primary care patient-centered medical home: a review of cost & quality results. 2012. http://www.pcpcc.org/sites/default/files/media/benefits_of_implementing_the_primary_care_pcmh.pdf. Accessed 19 Apr 2015.
Phytel. Prevea health automates population health management and improves outcomes. 2013. http://www3.phytel.com/Libraries/Case-Study-PDFs/Prevea-Health-CS-041013.sflb.ashx. Accessed 19 Apr 2015.
Phytel. Case study: northeast Georgia physicians group. 2012. http://cdn2.content.compendiumblog.com/uploads/user/863cc3c6-3316-459a-a747-3323bd3b6428/4c5909e8-1708-4751-873e-4129cb2ed878/File/2eb524a34e010967789612b5ed70bd79/1392222301097.pdf.
Pletcher T. Changing the status quo to improve health services in Michigan: an interview with Dr. Tim Pletcher. Kanter J. 2015; 2:30–39. URL: http://www.kanterhealth.org/wp-content/uploads/Kanter-Journal-FINAL.pdf. Last accessed 24 Mar 2015.
Rai A, MD and Weisse JL, MS, RN. Care managers for value-based healthcare, case in point, Dorland Health Newslet. 2013;11(10). http://cdn2.content.compendiumblog.com/uploads/user/863cc3c6-3316-459a-a747-3323bd3b6428/4c5909e8-1708-4751-873e-4129cb2ed878/File/555ef563c0d60ea0c089eb2673ac8265/1391564340558.pdf.
Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M, Larson EB. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff. 2010;29(5):835–43. doi:10.1377/hlthaff.2010.0158.
Rosenberg CN, Peele P, Keyser D, McAnallen S, Holder D. Results from a patient-centered medical home pilot at UPMC health plan hold lessons for broader adoption of the model. Health Aff. 2012;31(11):2423–31. doi:10.1377/hlthaff.2011.1002.
Shaljian, M., Nielsen, M. Managing populations, maximizing technology: population health management in the medical neighborhood. Patient-centered primary care collaborative. 2013. www.pcpcc.org/resource/managing-populations-maximizing-technology#sthash.P8lGuRJK.dpuf.
Starfield B. The future of primary care: refocusing the system. N Engl J Med. 2008;359:2087–91. doi:10.1056/NEJMp0805763.
Terry K. Google testing telehealth service linked to search. Medscape Med News. 2014. http://www.medscape.com/viewarticle/833823?src=rss.
Terry K. Mobile health tech could reduce doctor visits. InformationWeek Healthcare. 2013. http://www.informationweek.com/wireless/mobile-health-tech-could-reduce-doctor-visits/d/d-id/1112162?.
Terry K Is healthcare big data ready for prime time?. InformationWeek Healthcare. 2013. http://www.informationweek.com/big-data/big-data-analytics/is-healthcare-big-data-ready-for-prime-time/d/d-id/1108628?.
Terry K. Strategy: how mobility, Apps and BYOD will transform healthcare. InformationWeek Healthcare. 2012. http://reports.informationweek.com/abstract/105/8914/Healthcare/strategy-how-mobility-apps-and-byod-will-transform-healthcare.html.
UnitedHealth Center for Health Reform & Modernization. Advancing primary care delivery: practical, proven and scalable approaches. 2014. http://www.unitedhealthgroup.com/~/media/UHG/PDF/2014/UNH-Primary-Care-Report-Advancing-Primary-Care-Delivery.ashx.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Grundy, P.H., Hodach, R.J. (2016). Health IT’s Essential Role in the Patient-Centered Medical Home and Practice-Based Population Health Management. In: Weaver, C., Ball, M., Kim, G., Kiel, J. (eds) Healthcare Information Management Systems. Health Informatics. Springer, Cham. https://doi.org/10.1007/978-3-319-20765-0_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-20765-0_15
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20764-3
Online ISBN: 978-3-319-20765-0
eBook Packages: MedicineMedicine (R0)