Abstract
After thyroid surgery, a change in voice from baseline is considered to be the most common complication. The presence or absence of recurrent laryngeal nerve (RLN) dysfunction does not solely predict functional voice outcome after thyroidectomy, as other mechanisms can affect vocal fold function. Nonetheless, when reading the pertinent literature, it becomes obvious that the true incidence of temporary and permanent vocal fold paralysis (VFP) after thyroid surgery is still unknown. The majority of previous studies that have examined the incidence of VFP have lacked adequate assessment of postoperative vocal fold function. The reason for this variance in practice is due to the lack of consensus from the surgical professional societies and the difference in the professional background and training of today’s thyroid surgeons. Such statistics about the true risk of RLN injury with subsequent temporary or permanent VFP rates are important in obtaining informed patient consent before proceeding with thyroidectomy. Pre- and postoperative assessment of vocal fold function for patients undergoing thyroid surgery may help to detect an existing preoperative RLN palsy or an early iatrogenic RLN injury. Knowing this information may help to develop an appropriate surgical plan preoperatively and intervene supportively in a patient who may have vocal fold motion impairment postoperatively. Herein, we discuss the technical considerations for voice assessment during thyroid surgery and the rationale for routine pre- and postoperative laryngeal assessment of the larynx.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vocal fold paralysis
- Recurrent laryngeal nerve
- Voice assessment
- Fiberoptic laryngoscopy
- Thyroidectomy
- Laryngeal exam
Introduction
Thyroidectomy is considered the mainstay of treatment for nearly all thyroid cancers, including certain benign pathologies when indicated or elected by patients [1]. In the modern era, these procedures are being undertaken by a variety of surgeons with different training backgrounds and philosophies, that range from general surgeons and otolaryngologists to highly specialized endocrine surgeons and head and neck endocrine surgeons in high-volume academic centers. Yet, in the United States, the vast majority of thyroid surgeries are performed by low-volume surgeons who perform less than 5–10 thyroid cases a year [2]. This fact is at odds with the known relationship between volume and outcome for thyroid surgery.
Thyroidectomy is reportedly associated with a 25–84 % risk of postoperative voice alteration [3–7]. Iatrogenic recurrent laryngeal nerve (RLN) injury may in part be responsible for some of this alteration. Mechanisms of iatrogenic RLN injury may include mechanical (i.e., compression, crush, stretch, and laceration), thermal, or vascular (i.e., ischemic injury) factors [8]. Nonetheless, the presence or absence of RLN dysfunction does not solely predict functional voice outcome after thyroidectomy. Other mechanisms can affect vocal fold function, including injury to the external branch of the superior laryngeal nerve (EBSLN), postoperative inflammation, laryngeal edema, surgical trauma to the cricothyroid muscle or cricoarytenoid joint, endotracheal intubation-related trauma, and laryngotracheal fixation [9–11]. Vocal manifestations from these various pathologies can range from a seemingly normal voice or transient voice fatigue to profound and permanent dysphonia with a substantially adverse impact on the patient’s quality of life [7].
Assessment of vocal fold function is important in both the pre- and postoperative evaluation of patients undergoing thyroid surgery. This will detect an existing preoperative RLN palsy or an early iatrogenic RLN injury [12]. Although most postoperative voice changes resolve spontaneously within 3–6 months of thyroid surgery, patients can develop maladaptive compensatory mechanisms during postoperative recovery [13–15]. Such vocal behaviors can persist after resolution of the underlying vocal pathology and are most appropriately evaluated and treated by experienced speech-language pathologists. Early identification of voice dysfunction and referral to a speech-language pathologist for vocal rehabilitation could be beneficial to these patients so that vocal function can be optimized. Therefore, postoperative voice assessment should be initiated early and include comprehensive voice-specific functional and physical evaluations.
Prevalence of Recurrent Laryngeal Nerve Paralysis
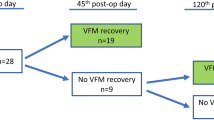
When reading the pertinent literature, it becomes obvious that the true incidence of temporary and permanent vocal fold paralysis (VFP) after thyroid surgery is still unknown. The majority of previous studies that have examined the incidence of VFP have lacked adequate postoperative vocal fold motion assessment. In fact, most studies have not incorporated direct visualization of the vocal folds as part of their postoperative assessment [5, 16, 17]. Also, there is considerable variation in the reported incidence of VFP due to the different methodology used to diagnose RLN injury, with each method having significantly different sensitivities and specificities. This is clearly demonstrated in the meta-analysis performed by Jeannon et al. [7], as a wide variation in the reported VFP rates following thyroid surgery can be appreciated. The incidence of temporary VFP ranges from 1.4 to 38. 4 % with an average value of 9.8 %, while the incidence of permanent VFP varies 10-fold, according to the method of laryngeal exam and ranges from 0 to 18.6 % with an average value of 2.3 % (Fig. 3.1).
Meta-analysis performed by Jeannon et al. [7] on 25,000 patients. (a) The overall incidence of temporary VFP and (b) permanent VFP amongst studies included in the analysis
Such statistics about the true risk of RLN injury with subsequent temporary or permanent VFP rates are important in obtaining informed patient consent before proceeding with thyroidectomy. Nondisclosure can cause potential unfavorable effects on the patient–physician relationship and health outcomes [18]. Moreover, the low rates of VFP quoted to patients preoperatively by surgeons are often derived from reported series of patients treated at high-volume academic centers with favorable and publishable results. This information for counseling should be based on knowing one’s personal outcomes and can only be accurately obtained through reasonable volume. Ultimately, uniform and standardized criteria for vocal fold evaluation before and after surgery are needed in order to allow comparison of results among different centers.
Laryngeal Examination of the Larynx Versus Subjective Voice Assessment
The reason for including laryngeal exam of the larynx in all patients undergoing thyroidectomy, both pre- and postoperatively, is basically due to the fact that VFP may occur without any voice alterations [5]. This discrepancy between glottic function and voice may be due to the variability in the remaining function of the vocal fold, position of the paralyzed cord, or compensation of the contralateral vocal fold [19].
It is common to notice improvement in voice symptoms in a patient with a stable VFP. This may be due to the resumption of normal vocal fold function or, just as likely, the evolution of a more favorable medial position with ongoing stable VFP [20, 21]. Without laryngeal exam, such improvement could be falsely interpreted as a resolution of the VFP. The correlate is also true that change in voice may derive from many sources and does not necessarily imply VFP. It is only the laryngeal exam that can accurately identify VFP.
Voice Alteration with Normal Vocal Fold Mobility
After thyroidectomy, both subjective and objective voice changes may occur in patients while maintaining intact vocal fold mobility. Subjective changes may consist of voice fatigue and difficulty with high pitch. Objective findings include decrease in the voice fundamental frequency, vocal range, maximum sound pressure, vocal jitter, and phonation time [13–15]. Subjective and objective voice changes usually occur transiently in up to 80–85 % of patients after thyroidectomy with normal vocal fold function [5, 22].
The mechanisms for voice alteration despite normal vocal fold mobility include the following [9–11, 23, 24]:
-
Cricothyroid muscle dysfunction: this may occur due to direct injury during thyroidectomy, transient myositis, or the effect of seroma formation.
-
Injury to the EBSLN during thyroidectomy.
-
Postoperative soft tissue changes affecting the larynx, including edema, strap muscle retraction, and denervation, and laryngotracheal scarring.
-
Strap muscle division during thyroidectomy.
-
Intubation-related vocal fold changes: these include short-term edema, vocal fold laceration, arytenoid dislocation, or more long-term vocal fold granuloma formation.
-
Upper respiratory tract infection: typically a viral laryngitis unrelated to surgery.
What is important to note is that patients do not usually communicate subtle voice changes, and this may pose difficulty for unmindful surgeons to pick up. To overcome this issue, various Voice Handicap Index (VHI) questionnaires have been used and are reliable in identifying voice dysfunction after thyroidectomy. Typically, patients with a change in VHI score greater than 25 from their preoperative baseline are referred to speech-language pathology and laryngology for further assessment [25]. Despite these techniques, we believe all patients need a laryngeal exam if we are to appreciate an accurate quality outcome measure of thyroidectomy.
Asymptomatic Vocal Fold Paralysis
An asymptomatic normal voice is reported to occur in 20 % of patients with VFP, falsely suggesting resolution or absence of RLN injury [26]. Various mechanisms have been suggested to explain this occurrence and include [20, 21, 26]:
-
RLN sustaining partial neural function (i.e., paresis).
-
A more medial position of the paralyzed vocal fold.
-
Compensation of the contralateral vocal fold.
This issue highlights the significance of preoperative laryngeal assessment in patients being evaluated for additional surgery that risks injury to the RLN. Respiratory morbidity and swallowing safety may be further compromised if the contralateral nerve is operated on.
Preoperative Laryngeal Exam
Because of the relatively low overall rate of preoperative VFP in patients undergoing thyroid surgery, some have abandoned preoperative laryngeal assessment, while others have reserved it for specific cases (i.e., previous neck surgery, voice symptoms). We believe that it is very wise to routinely examine vocal fold function in all patients undergoing thyroid surgery. The rationale for this routine assessment is summarized below [12, 20, 27, 28]:
-
Preoperative VFP is commonly encountered and has been reported to occur in 1.9–3.5 % of cases with benign thyroid pathology.
-
VFP can be present in the absence of voice changes. The sensitivity of voice change in predicting VFP is only 30–70 % [12, 20].
-
It provides a baseline for postoperative laryngeal assessment.
-
VFP can suggest invasive malignancy (i.e., Stage 4 disease) preoperatively. This will prompt for more appropriate airway and lymph node imaging preoperatively and more specific patient counseling.
-
Preoperative knowledge of vocal fold functioning helps to plan the management of an invaded RLN found at surgery.
-
It is important to assess preoperative vocal fold function before assuming responsibility for any VFP found postoperatively.
-
For accurate quality assessment, postoperative vocal fold function assessment implicitly requires preoperative examination as well.
Unfortunately, guidelines from professional bodies in the United States are lacking on this topic, and no consensus is available. The current American Thyroid Association (ATA) guidelines and the American Association of Clinical Endocrinology (AACE) guidelines make no reference on this issue. Only the guidelines from the American Academy of Otolaryngology—Head and Neck Surgery recommend laryngeal examination for patients with preoperative voice changes, for those undergoing reoperative surgery, or for patients scheduled to undergo thyroidectomy for cancer [29]. On the other hand, the British Thyroid Association (BTA) recommends laryngeal examination for patients with preoperative voice changes and for those scheduled to undergo thyroidectomy for cancer. The British Association of Endocrine and Thyroid Surgeons (BAETS) recommends that all patients should undergo pre- and postoperative laryngeal examination. Similarly, the guidelines of the German Association of Endocrine Surgeons recommend pre- and postoperative laryngoscopy in all patients undergoing thyroid surgery.
Postoperative Laryngeal Exam
Routine postoperative laryngeal exam is required in all patients undergoing thyroid surgery. This will allow surgeons to detect early iatrogenic injuries and obtain accurate information regarding their surgical outcomes. The earlier the vocal folds are assessed, the higher the incidence of abnormalities observed. Dionigi et al. [16] determined that the VFP rate was 6.4 % on the day of surgery, 6.7 % on day 1, 4.8 % on day 2, 2.5 % on day 14, and 0.8 % at 6 weeks postoperatively. This study demonstrates that the ideal time period during which to evaluate vocal fold function is the early postoperative period, as such timing will allow for the most cases of VFP to be identified.
The rationale for the routine postoperative assessment of vocal fold function is summarized below [20]:
-
It is the only accurate postoperative outcome functional measure of RLN integrity. Voice abnormalities may occur in the absence of VFP; hence, for the functional and psychological recovery of the patient’s symptoms in these cases, it will confirm that no injury took place to the RLN.
-
Allows interpretation of surgical technique and, if utilized, intraoperative electromyography responses.
-
Implications for respiratory and swallowing safety after thyroidectomy. Occasionally, a patient will not have airway symptoms in the immediate postoperative period (because the airway may be sufficient despite a paralyzed vocal fold) and the patient may present at a follow-up visit complaining of shortness of breath or stridor on exertion.
The current ATA management guidelines make no reference on this issue. The BTA guidelines recommend postoperative laryngeal exam only when there has been a voice disturbance beyond 2 weeks. Only the BAETS and the American Academy of Otolaryngology—Head and Neck Surgery have recommended that laryngoscopy should be performed postoperatively for all patients undergoing thyroid surgery.
Feasibility of Laryngeal Examination
Due to the difference in background and training of thyroid surgeons, some might feel it to be necessary to refer patients to specialized otolaryngology clinics for vocal fold assessment. We advise that all surgeons performing thyroidectomy to become confident with the technique of laryngoscopy and consider examining their patients routinely. Vocal fold function can be assessed by various modalities. The most commonly used methods include indirect laryngoscopy (mirror examination), videostroboscopy, and fiberoptic laryngoscopy (FOL). Significant differences in reported rates of VFP have been documented when comparing these modalities [7].
Although indirect laryngoscopy is simply performed, it has a restricted visual field and low diagnostic accuracy [30]. A significant percentage of patients cannot tolerate this method of examination due to the gag reflex. Conversely, videostroboscopy utilizes a high frequency strobe light to analyze the vibration and the mucosal wave of the vocal folds during phonation. It requires specialist equipment and therefore restricted to specialist practice and is not a feasible method of assessing voice function after thyroidectomy in routine practice. FOL offers a more detailed and wider field of vision to the larynx compared with indirect laryngoscopy (Fig. 3.2). The optical illumination and magnification can also allow the images to be portrayed on a screen for higher definition assessment. FOL should be considered the gold standard in diagnosing perioperative VFP since it is easily tolerated by patients and can be performed quickly in the office. Usually the scope is advanced above the epiglottis and with the “e” and “sniff-in” maneuver; adduction and abduction of the true vocal folds can be appreciated. On average, only 6 exams are needed for a beginner to become competent in performing FOL [31].
FOL should be performed within the first 24 h after surgery. We and others believe that early laryngeal assessment, within the first 24 h after surgery, is the optimal time frame during which to detect the majority of VFP cases, including mild impairments that begin to undergo the healing process within the first few days following surgery but still require follow-up [16].
The relative cost of the selected laryngeal examination modality should be considered. While there is no incurred cost of indirect laryngoscopy using a laryngeal mirror, there are additional health care costs in performing FOL and videostroboscopy. These modalities are justified in select cases when the larynx cannot be adequately examined using the laryngeal mirror or in the case of identified vocal fold motion impairment in order to more accurately define the abnormality [29]. Nevertheless, the surgeon assessing laryngeal function should strive to perform the most complete, cost-effective examination for the patient and document the examination accurately.
Feasibility of Transcutaneous Laryngeal Ultrasonography
Recently, transcutaneous laryngeal ultrasonography (TLUSG) has been proposed as a promising, noninvasive technique to examine the vocal folds during thyroid surgery [32–36]. Because most patients with thyroid disease are submitted to ultrasound examination during their clinical evaluation, this method of evaluating vocal fold mobility could become a real asset in the preoperative and postoperative management of patients undergoing thyroid surgery. Some advantages of TLUSG over direct laryngoscopy are its noninvasiveness, convenience, comfort, increased availability, and obviation of topical anesthetics. In addition, the use of in-office ultrasound has been shown to be cost-effective in clinical practice.
The greatest enthusiasm for this technique was historically in the pediatric population, in whom laryngoscopy is not well tolerated without anesthesia [37]. However, recent studies have had favorable findings in the adult population, demonstrating the reproducibility of TLUSG in identifying postoperative VFP with accuracy similar to direct laryngoscopy. Studies have estimated that nearly two thirds of laryngoscopies could be avoided by the use of preoperative screening TLUSG [33]. Despite these favorable findings, the vocal folds cannot be assessed by TLUSG in approximately 20–25 % of patients, thus requiring direct laryngoscopy [33–35, 38]. Moreover, the sensitivity of TLUSG in demonstrating VFP ranges from 60 to 95 % [32–34, 39, 40]. Factors such as male gender, advanced age, increased body habitus, calcification of the thyroid cartilage, sharp angulation of the thyroid cartilage, and distance from collar incision to thyroid cartilage, as well as the experience of the ultrasonographer, have all been cited to affect the accuracy of TLUSG [38, 41]. Even for some patients whose vocal folds are assessable by TLUSG, their findings can be discordant when compared with the gold standard, direct laryngoscopy. Therefore, the routine use of TLUSG as a diagnostic or screening test remains controversial.
Summary
Although the true rate of RLN injury after thyroid surgery is still unknown, we know for a fact that it is common, occurring in as many as 10 % of patients on average. Even in the absence of RLN injury, voice changes frequently occur after thyroid surgery. Only routine pre- and postoperative laryngeal assessment will allow surgeons to consistently make informed clinical decisions that will improve outcomes and assess objectively the impact of the operation of vocal fold function. We believe this to be the only reliable way that allows immediate accurate assessment of the surgical technique used. This will optimize surgical training and provide valid, accurate surgical outcome data to patients.
References
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19(11):1167–214.
Kandil E, Noureldine SI, Abbas A, Tufano RP. The impact of surgical volume on patient outcomes following thyroid surgery. Surgery. 2013;154(6):1346–52. Discussion 52–3.
de Pedro NI, Fae A, Vartanian JG, Barros AP, Correia LM, Toledo RN, et al. Voice and vocal self-assessment after thyroidectomy. Head Neck. 2006;28(12):1106–14.
Musholt TJ, Musholt PB, Garm J, Napiontek U, Keilmann A. Changes of the speaking and singing voice after thyroid or parathyroid surgery. Surgery. 2006;140(6):978–88. Discussion 88–9.
Stojadinovic A, Shaha AR, Orlikoff RF, Nissan A, Kornak MF, Singh B, et al. Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg. 2002;236(6):823–32.
Rosato L, Carlevato MT, De Toma G, Avenia N. Recurrent laryngeal nerve damage and phonetic modifications after total thyroidectomy: surgical malpractice only or predictable sequence? World J Surg. 2005;29(6):780–4.
Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract. 2009;63(4):624–9.
Hartl DM, Travagli JP, Leboulleux S, Baudin E, Brasnu DF, Schlumberger M. Clinical review: Current concepts in the management of unilateral recurrent laryngeal nerve paralysis after thyroid surgery. J Clin Endocrinol Metab. 2005;90(5):3084–8.
McIvor NP, Flint DJ, Gillibrand J, Morton RP. Thyroid surgery and voice-related outcomes. Aust N Z J Surg. 2000;70(3):179–83.
Roubeau B, Chevrie-Muller C, Lacau Saint Guily J. Electromyographic activity of strap and cricothyroid muscles in pitch change. Acta Otolaryngol. 1997;117(3):459–64.
Jones MW, Catling S, Evans E, Green DH, Green JR. Hoarseness after tracheal intubation. Anaesthesia. 1992;47(3):213–6.
Farrag TY, Samlan RA, Lin FR, Tufano RP. The utility of evaluating true vocal fold motion before thyroid surgery. Laryngoscope. 2006;116:235–8. United States.
Hong KH, Kim YK. Phonatory characteristics of patients undergoing thyroidectomy without laryngeal nerve injury. Otolaryngol Head Neck Surg. 1997;117(4):399–404.
Debruyne F, Ostyn F, Delaere P, Wellens W. Acoustic analysis of the speaking voice after thyroidectomy. J Voice. 1997;11(4):479–82.
Debruyne F, Ostyn F, Delaere P, Wellens W, Decoster W. Temporary voice changes after uncomplicated thyroidectomy. Acta Otorhinolaryngol Belg. 1997;51(3):137–40.
Dionigi G, Boni L, Rovera F, Rausei S, Castelnuovo P, Dionigi R. Postoperative laryngoscopy in thyroid surgery: proper timing to detect recurrent laryngeal nerve injury. Langenbecks Arch Surg. 2010;395(4):327–31.
Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihner E, Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008;393(5):667–73.
Abadin SS, Kaplan EL, Angelos P. Malpractice litigation after thyroid surgery: the role of recurrent laryngeal nerve injuries, 1989-2009. Surgery. 2010;148(4):718–22. Discussion 22–3.
Randolph GW. The importance of pre- and postoperative laryngeal examination for thyroid surgery. Thyroid. 2010;20(5):453–8.
Randolph GW, Kamani D. The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery. 2006;139:357–62. United States.
Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W. Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope. 2002;112(1):124–33.
Lombardi CP, Raffaelli M, D’Alatri L, Marchese MR, Rigante M, Paludetti G, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery. 2006;140(6):1026–32. Discussion 32–4.
Peppard SB, Dickens JH. Laryngeal injury following short-term intubation. Ann Otol Rhinol Laryngol. 1983;92(4 Pt 1):327–30.
Echternach M, Maurer CA, Mencke T, Schilling M, Verse T, Richter B. Laryngeal complications after thyroidectomy: is it always the surgeon? Arch Surg. 2009;144(2):149–53. Discussion 53.
Stojadinovic A, Henry LR, Howard RS, Gurevich-Uvena J, Makashay MJ, Coppit GL, et al. Prospective trial of voice outcomes after thyroidectomy: evaluation of patient-reported and clinician-determined voice assessments in identifying postthyroidectomy dysphonia. Surgery. 2008;143(6):732–42.
Sittel C, Stennert E, Thumfart WF, Dapunt U, Eckel HE. Prognostic value of laryngeal electromyography in vocal fold paralysis. Arch Otolaryngol Head Neck Surg. 2001;127(2):155–60.
Shin JJ, Grillo HC, Mathisen D, Katlic MR, Zurakowski D, Kamani D, et al. The surgical management of goiter: Part I. Preoperative evaluation. Laryngoscope. 2011;121(1):60–7.
Fenton JE, Timon CI, McShane DP. Recurrent laryngeal nerve palsy secondary to benign thyroid disease. J Laryngol Otol. 1994;108(10):878–80.
Chandrasekhar SS, Randolph GW, Seidman MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013;148 Suppl 6:S1–37.
Bora MK, Narwani S, Agarwal S, Bapna AS. A study of routine exposure of recurrent laryngeal nerve during thyroid surgery. Indian J Otolaryngol Head Neck Surg. 2005;57(3):182–4.
Laeeq K, Pandian V, Skinner M, Masood H, Stewart CM, Weatherly R, et al. Learning curve for competency in flexible laryngoscopy. Laryngoscope. 2010;120(10):1950–3.
Wong KP, Lang BH, Ng SH, Cheung CY, Chan CT, Lo CY. A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy. Surgery. 2013;154(6):1158–64. Discussion 64–5.
Cheng SP, Lee JJ, Liu TP, Lee KS, Liu CL. Preoperative ultrasonography assessment of vocal cord movement during thyroid and parathyroid surgery. World J Surg. 2012;36(10):2509–15.
Wang CP, Chen TC, Yang TL, Chen CN, Lin CF, Lou PJ, et al. Transcutaneous ultrasound for evaluation of vocal fold movement in patients with thyroid disease. Eur J Radiol. 2012;81(3):e288–91.
Dedecjus M, Adamczewski Z, Brzezinski J, Lewinski A. Real-time, high-resolution ultrasonography of the vocal folds–a prospective pilot study in patients before and after thyroidectomy. Langenbecks Arch Surg. 2010;395(7):859–64.
Carneiro-Pla D, Miller BS, Wilhelm SM, Milas M, Gauger PG, Cohen MS, et al. Feasibility of surgeon-performed transcutaneous vocal cord ultrasonography in identifying vocal cord mobility: a multi-institutional experience. Surgery. 2014;156:1597–602.
Friedman EM. Role of ultrasound in the assessment of vocal cord function in infants and children. Ann Otol Rhinol Laryngol. 1997;106(3):199–209.
Wong KP, Lang BH, Chang YK, Wong KC, Chow FC. Assessing the validity of Transcutaneous Laryngeal Ultrasonography (TLUSG) after thyroidectomy: what factors matter? Ann Surg Oncol. 2014;22:1774–80.
Sidhu S, Stanton R, Shahidi S, Chu J, Chew S, Campbell P. Initial experience of vocal cord evaluation using grey-scale, real-time, B-mode ultrasound. ANZ J Surg. 2001;71:737–9. Australia.
Vats A, Worley GA, de Bruyn R, Porter H, Albert DM, Bailey CM. Laryngeal ultrasound to assess vocal fold paralysis in children. J Laryngol Otol. 2004;118(6):429–31.
Bozzato A, Zenk J, Gottwald F, Koch M, Iro H. Influence of thyroid cartilage ossification in laryngeal ultrasound. Laryngorhinootologie. 2007;86(4):276–81.
Conflicts of Interest Disclosures
All authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Noureldine, S.I., Tufano, R.P. (2016). Pre- and Post-Thyroidectomy Voice Assessment. In: Hanks, J., Inabnet III, W. (eds) Controversies in Thyroid Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-20523-6_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-20523-6_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20522-9
Online ISBN: 978-3-319-20523-6
eBook Packages: MedicineMedicine (R0)