Abstract
Models of care for aging patients with human immunodeficiency virus (HIV) are evolving.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Human Immunodeficiency Virus
- Human Immunodeficiency Virus Patient
- Comprehensive Geriatric Assessment
- Human Immunodeficiency Virus Care
- Human Immunodeficiency Virus Clinic
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Key Points-
Models of care for aging patients with human immunodeficiency virus (HIV) are evolving.
-
The one size fits all approach is inconsistent with current care needs.
-
Interdisciplinary team-based models are needed.
-
Models of care based on the proven Comprehensive Geriatric Care approach are increasingly employed.
The success of highly active antiretroviral therapy (HAART) has significantly changed the pattern of HIV infection in developed countries, with the ‘graying’ of the HIV-infected population testament to its success.
Management of older patients is complicated by the likelihood of comorbidities requiring treatment, resultant problems with drug toxicity and interactions on polypharmacy, and changes in pharmacokinetics (potential for drug accumulation and toxicity) as hepatic and renal function often decline with age. This has provided new challenges relating to the care of older patients, particularly with regard to the management of comorbidities and antiretroviral (ARV) toxicity. This is being addressed through the refinement of existing antiretroviral therapy (ART), the development of new agents, and a growing focus on the need for a more holistic approach to care (involving the integration of accepted primary care principles into routine HIV care).
In the pre- and early-HAART era the provision of HIV care was standardized with outpatient visits performed in dedicated HIV clinics, with regular visits every 3–4 months. At present HIV patients require a more personalized approach to the frequency of visits and often a diversification to the type of health care providers.
The use of high efficacy and low toxicity ART is less likely to result in ARV switch compared to earlier treatment options (other than for drug simplification or patient convenience). As a result, knowledgeable and willing primary care providers will increasingly be central to the provision of routine assessments of patients with HIV on stable ART. On the other hand, patients with HIV, multimorbidity (MM), and age-related conditions will require HIV physicians to work in interdisciplinary teams with other specialists in a patient-centered model of care. This type of care has often been provided in tertiary referral level sites identified variously as ‘HIV metabolic clinics’ where the HIV-treating physician remains central to care, balancing the often competing demands of maintaining effective viral suppression while managing comorbidities, treatment side effects, and drug interactions.
Interestingly, this patient centered approach is conceptually close to the Comprehensive Geriatric Assessment (CGA) that is the standard approach to care in the geriatric context.
The term CGA is defined as a multidisciplinary diagnostic and treatment process that identifies medical, psychosocial, and functional limitations of a frail older person in order to develop a coordinated plan to maximize overall health with aging [1, 2]. The health care of an older adult extends beyond the traditional medical management of illness. It requires evaluation of multiple issues, including physical, cognitive, affective, social, financial, environmental, and spiritual components that influence an older adult’s health. CGA is based on the premise that a systematic evaluation of frail older persons by a team of health professionals may identify a variety of treatable health problems and lead to better health outcomes. So far the CGA approach has rarely been used in a structured fashion in patients with HIV as in the geriatric context, but issues regarding multimorbidity, frailty, and disability are increasingly incorporated into the clinical assessment of older patients with HIV.
CGA programs to identify the health condition of patients with HIV include:
-
age;
-
medical comorbidities (such as heart failure, renal dysfunction, bone disorders, hepatic dysfunction, or cancer);
-
psychosocial disorders (such as depression or isolation);
-
specific geriatric conditions (such as dementia, falls, functional disability, or polypharmacy);
-
previous or predicted high health care utilization; and
-
consideration of change in living situation (eg, from independent living to assisted living, nursing home, or in-home caregivers).
Conceptually, CGA involves several processes of care that are shared over several providers in the assessment team. The overall care rendered by CGA teams can be divided into six steps:
-
1.
data gathering;
-
2.
discussion among the team;
-
3.
development of a treatment plan;
-
4.
implementation of the treatment plan;
-
5.
monitoring response to the treatment plan; and
-
6.
revising the treatment plan.
Each of these steps is essential if the process is to be successful at achieving maximal health and functional benefits.
Although the amount of potentially important information may seem overwhelming, formal assessment tools and shortcuts can reduce this burden on the clinician performing the initial CGA [3]. These questionnaires can be used to gather information about general history (eg, past medical history, medications, social history, review of systems), as well as gather information specific to CGA, such as:
-
ability to perform functional tasks and need for assistance;
-
fall history;
-
sources of social support, particularly family or friends;
-
depressive symptoms;
-
vision or hearing difficulties; and
-
whether the patient has specified a durable power of attorney.
Interdisciplinary team members (eg, nurses, social workers, occupational therapists, pharmacists, psychologists, etc) can administer screening tools to both save time and help the team to focus on specific limitations that need more detailed evaluation [4].
Further, education and involvement of the patient remains vital for the success of any treatment plan to ensure it meets the varying needs of individual patients. Moreover, a trusting patient–physician relationship established in HIV care may provide an excellent starting point for the management of these complex problems.
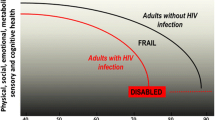
In the case of disability, the provision of care is seldom driven by HIV-related factors, while on the contrary geriatric syndromes (eg, cognitive decline, mobility, maintenance of independence, and polypharmacy), social support, and financial status are the major drivers of health care provision via home-based or supervised health setting (Fig. 9.1).
References
Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993;342:1032–6.
Devons CA. Comprehensive geriatric assessment: making the most of the aging years. Curr Opin Clin Nutr Metab Care. 2002;5:19–24.
Elsawy B, Higgins KE. The geriatric assessment. Am Fam Physician. 2011;83:48–56.
Reuben DB. Medical care for the final years of life: “When you’re 83, it’s not going to be 20 years”. JAMA. 2009;302:2686–94.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Guaraldi, G., Falutz, J. (2016). Multidimensional Geriatric Assessment in Older Patients with HIV. In: Guaraldi, G., Falutz, J., Mussi, C., Silva, A. (eds) Managing the Older Adult Patient with HIV. Adis, Cham. https://doi.org/10.1007/978-3-319-20131-3_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-20131-3_9
Published:
Publisher Name: Adis, Cham
Print ISBN: 978-3-319-20130-6
Online ISBN: 978-3-319-20131-3
eBook Packages: MedicineMedicine (R0)