Abstract
Epilepsy affecting 1 % of the world’s population and is the most common serious disorder of the brain, greatly impacting on the quality of life of affected individuals, particularly those whose seizures are not fully controlled. Epilepsy has a multifactorial origin and a multifaceted expression. It is caused by clusters of nerve cells in the brain which sometimes signal abnormally, causing seizures. Anything that disturbs the normal pattern of neuronal activity—from illness to brain damage to abnormal brain development—can lead to seizures. Epilepsy may develop because of an abnormality in brain wiring, an imbalance of nerve signaling chemicals called neurotransmitters, changes in important features of brain cells called membrane receptors and channels, or some combination of these and other factors.
Depending on the brain area affected and its physiological role, these disturbances of neuronal activity that occur during seizures may cause strange sensations, emotions, and behaviors. They also sometimes cause convulsions, abnormal movements, and loss of consciousness. In some people, seizures happen only occasionally. Other people may experience hundreds of seizures a day. There are many different forms of epilepsy, and symptoms vary greatly from one person to another. About three-quarters of the individuals diagnosed with the epilepsies can control their seizures with medicine or surgery. However, about 30 % will continue to experience seizures even with the best available treatment. In some cases, people experience a type of seizure that last so long that they can damage the brain and may be life-threatening. Having a single seizure as the result of a high fever (called febrile seizure) or head injury does not necessarily mean that a person has epilepsy. Only when a person has had two or more seizures is he or she considered to have epilepsy. A measurement of electrical activity in the brain and brain scans such as magnetic resonance imaging or computed tomography are common diagnostic tests for epilepsy.
Research efforts need to be stepped up to better understand pathophysiologic mechanisms and to develop more effective therapies. Current understanding is on the mechanisms underlying seizure expression and thus allow us only symptomatic treatment (and still some seizures are or become with time drug resistant). To develop a cure of epilepsy we have to understand epileptogenesis, the long process which makes brain neurons vulnerable to hyperexcitability and abnormal synchronization. Equally important is to raise awareness on the nature of epilepsy through public education so that the lives of people with epilepsy are not adversely affected by stigma, prejudice, and discrimination, neither face unjust restrictions in their human rights, employment, marriage, and daily activities such as driving.
In this chapter we introduce the historical and current efforts to define and categorize epilepsy and we briefly describe the variety of its causes and our current ideas on the mechanisms underlying the expression of its main types.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
2.1 Introduction
This chapter aims to present a concise view of the major clinical and neuroscience aspects of epilepsy for an academic but not necessarily medical audience. More comprehensive accounts can be found in recent excellent reviews and books covering both clinical [1–5] and pathophysiological aspects [6, 7].
One can find descriptions of seizures since the beginning of recorded history, but they were usually attributed to demonic possessions or other supernatural influence [8, 9]. Babylonians astutely described many of the seizure types we recognize today as tonic clonic seizures, absences, drop attacks, simple and complex partial seizures and even focal motor (Jacksonian) or gelastic attacks. A writing from China’s seventh to second century BC describes symptoms resembling both partial and generalized convulsions. All three Indian medical systems recognize epilepsy and a compendium of the sixth century BC mentions loss of consciousness during particular seizures. The Babylonians and the other advanced Asiatic civilizations, although apparently kin observers, were not motivated to search for underlying mechanisms, being content with associating each seizure type with the invasion of the body by a particular evil spirit. The concept of pathophysiology had to wait till diseases were dissociated from the supernatural. Greeks imported all this medical tradition by coining the verb ΕΠΙΛΑΜΒΑΝΕΙΝ (to seize someone) from which the word epilepsy, while however questioning the nature of its causes and finally recognized epilepsy as a disorder of the body rather than a sacred disease. This was boldly asserted by Hippocrates in the fifth century BC—“AΛΛΑ ΓΑΡ ΑΙΤΙΟΣ Ο ΕΓΚΕΦΑΛΟΣ ΤΟΥΤΟΥ ΤΟΥ ΠΑΘΕΟΣ … ΟΤΩ ΔΕ ΤΡOΠΩ ΚΑΙ ΕΞ ΟΙΗΣ ΠΡΟΦAΣΙΟΣ ΓIΝΕΤΑΙ, ΕΓΩ ΦΡAΣΩ ΣAΦΑ” (Hippocrates Corpus 90, On the sacred disease §§ 1–6, 21). Hippocrates was absolutely right on his first statement that “the cause of epilepsy is in the brain”. But the second, that “he will proceed to explain clearly the mechanism and cause of seizures” is far from being true even today. Of historical interest to medicine is also his proposal to search for abnormal humors in the head of the epileptic goats—which seems to be the first ever proposal to experiment with animal models of any disease.
The idea of the brain as a cause of epilepsy was well accepted in specific circles even up to the second century AD when we see Galen and Aretaeus treating and theorizing about epilepsy in the Latin era. Unfortunately it had little influence on the public’s view of supernatural causes, which remained up to the middle ages (at least, given the still lingering progress of our society to abolish the stigma of epilepsy). The main holdup to progress in this field appears to have been the prohibition of anatomical studies, which ended with the European Renaissance of the fourteenth to seventeenth centuries, with Thomas Willis writing of convulsive disorders and the advance of pathology in the nineteenth century. Two fundamental developments, the concepts of animal electricity (from Galvani to Todd) and of functional localization in the brain (i.e. motor cortex) lead to the study of “epileptiform” or “partial” and “generalized” seizures. About this time Caton discovered EEG in animals and 52 years later Berger discovered human EEG. This led to confirmation of Todd’s hypothesis that seizures are the result of electrical discharges by Lennox in 1935. In the beginning of the twentieth century the road to basic mechanisms of epilepsy is paved by the introduction of the neuron doctrine (Cajal), the role of synapses (Sherrington) and their transmitters (Levy, Dale). In the second half of the twentieth century research is accelerated by enormous methodological progress in both directions: reductionistic i.e. discovery of ionic channels (Hodgkin and Huxley) and molecular genetics and integrating i.e. structural and functional brain imaging, video-telemetry, MEG, computer assisted analysis and multimodal data fusion. Every advance seems to add to the enormous complexity of the nervous system and the probability that multiple elusive genetic–molecular–metabolic mechanisms contribute to the wide range of epilepsies. We seem to know enough at the micro- and macroscopic level but not much at the mesoscopic one. This is probably why we know ictogenesis well enough to have relatively efficient drugs to suppress seizures, but we know almost nothing about epileptogenesis and how to prevent it.
Epilepsy, a chronic condition that is characterized by recurrent seizures, affects people of any gender, age and geographic region. Approximately 1 % of the general population in western societies suffers from some sort of epilepsy while up to 10 % will have at least one seizure during their lifetimes [10].
The incidence and prevalence of epilepsy in the EU is estimated to be respectively 3.3–7.8 per 1000 and 44/100.000 [11]. The total number of people affected with epilepsy in EU is estimated to 2,64 million. The financial burden for EU expressed in disability adjusted life years is 245,475 and in cost-of-illness 5221 € per person and 13,800 in total [12]. However, besides the calculated financial burden, there is also an enormous and uncalculated cost to the patients and their families. Even today, epilepsy still remains a stigmatizing disease with many social consequences. The term itself, which means that the control over one’s behavior is lost and remains unchanged over three millennia [8], shows the awe experienced by both the patient and the bystanders to a seizure. Epilepsy can alter patients’ everyday life causing impairments in quality of life [13] and psychological distress to caregivers. One of the most stressful aspects of the disease is the unpredictability of seizure occurrence [14]. A large number of epilepsy patients fail to remain seizure free despite adequate treatment; there is no such thing as “cured” epilepsy since seizure threshold remains reduced compared to that of an unaffected person [15].
Moreover, epileptic seizures can be lethal. Common causes of death include accidents while Sudden Unexpected Death in Epilepsy Patients (SUDEP) is often attributed to ictal cardiac arrhythmias [16].
Epilepsy is a chronic condition of multifactorial causes (from genetics to brain trauma and from inflammation to tumor) and with a multifaceted expression (from a mere brief loss of consciousness to focal or generalized convulsions) depending on which brain area has developed a tendency for neuronal hyperexcitability and hypersynchronization and what is the physiological role of this area.
In newly diagnosed patients with epilepsy, the initial treatment option is usually choosing one of the available antiepileptic drugs (i.e. monotherapy) based on seizure type, age, co-morbidities and other factors. Should this fail to control seizures, an alternative drug can be selected or be additionally prescribed.
Antiepileptic drugs accomplish seizure reduction by suppressing neuronal intrinsic or synaptic excitation (usually mediated by the neurotransmitter glutamate) and promoting synaptic inhibition (usually mediated by the neurotransmitter gamma-amino-butyric acid or GABA). Mechanisms of action include blockage of voltage-gated Na+ (e.g. carbamazepine) and Ca2+ channels, enhancement of GABA-mediated inhibition (e.g. benzodiazepines) and interference with glutamatergic excitation (e.g. felbamate). Some antiepileptics have multiple target systems (e.g. divalproate influences Na+, Ca2+ and GABA), while some others’ mechanism of action remains unknown (such as that of gabapentin) [17]. Unfortunately all available drugs treat ictogenesis (the expression of seizures) rather than epileptogenesis (the long term development of conditions leading to seizures). In that sense all treatment is symptomatic rather than causal, i.e. we do not yet have a cure for epilepsy. This symptomatic treatment is usually effective in about 70 % of the cases.
Surgery can be employed in selected cases of drug-resistant epilepsy or in the presence of structural lesions such as a brain tumor or hippocampal sclerosis. In certain cases of uncontrolled seizures vagal nerve stimulation might also be considered [18].
Undoubtedly epilepsy and its multiple often long term neurobiological, cognitive, psychological and social consequences require tailor-made and multitargeted treatment.
2.2 Definitions
Epilepsy is defined as a neurological condition which is characterized by a predisposition to generate recurrent epileptic seizures; it is not a single disease entity but points toward multiple underlying neurological defects and structural or functional changes in the brain. This is fundamentally considered to be independent of readily identified, transient factors that can induce seizures in the normal brain. The current definition of epilepsy requires at least two unprovoked seizures occurring 24 h apart [15].
The word seizure may refer to many sudden and severe events often including psychogenic seizures, dissociative seizures, conversion seizures many of which can often resemble epileptic seizures without being due to epilepsy [15].
Epileptic seizures are defined as events (behavioral expressions) of a paroxysmal nature often accompanied by transient alteration in consciousness level and with signs and symptoms due to abnormal, excessive or synchronized neuronal discharges of the brain which can be widespread or localized [19].
Non epileptic seizures on the other hand are not caused by abnormal neuronal discharges. They can be divided in two large groups; the organic non epileptic seizures (i.e. atypical syncope and parasomnias) and the psychogenic non epileptic seizures—NEPS (i.e. conversion symptoms and dissociative states). Typically, during a NEPS paroxysmal event sustained forceful eye closure can be present while eye closure in any form is uncommon during epileptic seizures [20].
There are currently several definitions employed to define the actual lesion or zone which is responsible for or correlated to the origin of epileptic seizures, mostly in terms of presurgical evaluation. The (actual and the larger ‘potential’) Epileptogenic Zone is described as the total cortical area which is necessary and sufficient to generate the seizures. The Epileptogenic Lesion refers to an abnormal structural brain area which is presumed to be causal of epileptic seizures in the symptomatic epilepsies and can be usually indentified by MRI. The Irritative Zone is the cortical area which is capable of generating interictal discharges while the Ictal Onset Zone is the cortical area from which ictal discharges arise. Both the Irritative Zone and the Ictal Onset Zone can be identified by scalp or intracranial EEG recordings. The Functional Deficit Zone is the cortical area with focal nonepileptic dysfunction which is responsible for functional deficits identified by neurological medical examination. The Symptomatogenic Zone refers to the cortical area which when activated by a seizure is responsible for producing the first clinical ictal signs and symptoms [21, 22].
Diagnostics of epilepsy still rely on clinical features. EEG, video and brain imagining such as MRI and CT are used for differential diagnostic purposes once a suspicion on a possible epileptic syndrome is made. Clinical manifestations depend on several factors such as the type of epilepsy or the particular epilepsy syndrome, the patient’s age, the area of the brain that generates seizures, and whether ictal discharges remain localized or propagate to other brain areas.
Every person can suffer an epileptic seizure given the right trigger and circumstances [15]. Acute symptomatic seizures occur at the time of a systemic insult or in close temporal association with a documented brain insult. Such precipitating events include metabolic disturbances, trauma, fever, infection, intoxication and substance withdrawal [23]. Alcohol withdrawal may precipitate seizures. Alcohol decreases CNS excitability by facilitating GABA action and acting as an NMDA receptor antagonist. Chronic alcohol abuse results in a down regulation of GABA and an up regulation of NMDA receptors and glutamate production. When withdrawal occurs, this increased potential for excitation can result in seizures [24]. Metabolic disturbances and trauma can further contribute to seizures in patients with alcohol abuse.
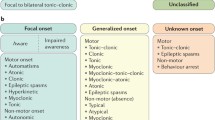
There has been a long discussion on classification of the epilepsies which has mainly been triggered by the recent technological advances both in imaging and genetics. Diagnosing a specific electroclinical syndrome is not always possible while the underlying cause might be of equal if not more value. Terminologies such as idiopathic, symptomatic, cryptogenic and also partial, complex and simple are not anymore used. A more descriptive approach has been recommended taking into account the underlying aetiology while retaining electrophysical syndromes when this is possible [25–28]. In parallel there is a growing appreciation of the fact that classification schemes should be based on current pathophysiological explanations but also serve to best distinguish conditions demanding different treatment and often these two goals may be conflicting, while mutually dependent.
2.3 Classification
Epilepsy is not a single disease entity but it is rather consisted of a range of underlying neurological disorders. The International League against Epilepsy—ILAE [25] in response to concerns about the existing classification systems, proposed a multiaxial diagnostic scheme which is summarized in Table 2.1. This diagnostic scheme aimed in categorizing individuals according to a standardized terminology that could be used by the vast majority of physicians in any relevant specialty while it would be flexible enough to include the dynamic aspects of the disease.
Yet, a syndromic diagnosis is not always possible while presumed seizures types and syndromes might alter as new information becomes available. Furthermore, a classification system is used for a variety of purposes; epidemiological investigations, basic research, clinical aspects (e.g. screening patients before surgery) and clinical trials. Thus a classification system should be able to address several different needs of diverse areas. Therefore, in the light of new basic and clinical science advances and led by the need to further simplify terminology used, a new classification has arisen concerning mainly seizures classification but also introducing a simplification of terminology used on epilepsies (Tables 2.2 and 2.3) [26].
2.4 Etiology
The possible identification of specific brain abnormalities associated with epilepsy has crucial implications in the treatment and prognosis of the disease. A broad category of brain abnormalities stems from a strongly genetic/developmental component, while other cases mainly originate from acquired insults (such as infection, trauma and hypoxia). While still classified together with other acquired pathologies, hippocampal sclerosis is considered to originate from a combination of genetic risk factors and initiating insults (such as febrile seizures) [29].
Lesions such as tumors and severe trauma are in no way transient and reversible. Seizures occurring in patients with a potential cause of epilepsy (such as a highly epileptogenic oligodendroglioma) are not classified as acute symptomatic seizures [30]. Moreover, if the lesion generates an enduring predisposition for unprovoked seizures, with a risk comparable to those who have had two unprovoked seizures, then the person should be considered to have epilepsy despite having only one seizure [15].
Although there is an apparent variance in the power of potential seizure triggers, a recognized epilepsy syndrome comes to blur the lines. Seizures in reflex epilepsies are triggered by sensory, motor or cognitive stimuli, such as bright lights, eating and music. The pathophysiology of this syndrome involves the activation of hyperexcitable diffuse cortical pathways, with different triggering points according to the precipitating stimulus (f. ex. occipital triggering and propagation through cortico-cortical pathways in photosensitivity [31].
2.4.1 Febrile Seizures
Febrile seizures (FS) encountered in children are a well-known example of provoked seizures. Factors involved in their pathogenesis include genetic susceptibility (reflected in a positive family history), inflammatory mechanisms (with a particular significance of IL-1β) [32], mutations in the GABA-A receptors and participation of sodium channels [33]. FS are benign and not to be confused with the distinct epileptic syndrome of Generalizes Epilepsy with FS (GEFS+).
2.4.2 Developmental Brain Abnormalities
Abnormalities in neuronal cell migration and dysplasias of the neural ectoderm occur in embryonic life and result in malformations of cortical development (such as hemimesencephaly, heterotopias and lissencephaly) and epileptogenic neurocutaneous syndromes (Tuberous Sclerosis Complex and Sturge-Weber syndrome), respectively. A strong genetic component is involved in Tuberous Sclerosis (autosomal dominant inheritance) as well as in vascular malformations such as cavernomas. Such lesions mainly result in intractable seizures that require surgical intervention.
A variety of aggressors can disrupt the normal migration of neurons from the periventricular germinal matrix to their final destination and disrupt cortical lamination, thus resulting in a failure of normal circuit formation. These include infectious agents (such as rubella and the TORCH complex), toxins (e.g. alcohol) [34], while genetic factors may also play a role. Histologically, a scattering of large anomalous neurons is observed, associated with thickening and white matter “balloon cells” (focal cortical dysplasia), a blurring of the cortical/white matter border (hemimegalencephaly), while heterotopic gray matter islands in the white matter are observed in heterotopias. Lissencephaly and pachygyria are notable for disrupted gyri architecture [35].
In Tuberous Sclerosis, blurred cortical lamination results from masses of astrocytic cells and calcifications, while in Sturge-Weber cortical atrophy is the result of overlying angiomas. This finding is also present in vascular malformations. Other epileptogenic factors include the presence of hemosiderin from recurrent hemorrhages, especially in cavernomas [36].
2.4.3 Acquired Lesions
Epilepsies resulting from non-developmental abnormalities include post-traumatic epilepsy (PTE), seizures originating after hypoxic brain injury (as in stroke and perinatal insults) and tumor-associated epilepsy (TAE). Hippocampal sclerosis (HS) and medial temporal lobe epilepsy (MTLE), classified as a distinctive constellation, will also be mentioned here.
Although infectious and immunologic aetiologies are important in acquired epilepsy, with the former playing an important role in the developing world (mainly in the form of tuberculomas and cystic brain lesions due to neurocysticercosis) and the latter in surgical constellations such as Rasmussen’s Syndrome [35], a systematic review is beyond the scope of this chapter.
2.4.3.1 Brain Injury (Traumatic, Hypoxic/Ischemic)
Post traumatic epilepsy (PTE) is the most common cause of new-onset epilepsy in young adults [37] and accounts for 20 % of structural epilepsy (5 % of all epilepsy cases) [38]. Nevertheless, only a sub-group of brain trauma patients will develop epilepsy. The latency from the time of the injury to the onset of epilepsy is extremely variable (weeks to years) [39] while scalp EEG may be unable to detect initial epileptiform activity [40]. Higher injury severity and the presence of an intracranial hematoma are important risk factors for both early (in the first week after injury) and late seizures [41]. Other risk factors for PTE include advanced patient age, multiple concussions and seizures within 24 h post-injury [42].
Histopathological consequences of penetrating injuries include the formation of an epileptogenic cortical scar, while non-penetrating trauma results in axonal shearing, edema and ischemia in the gray–white matter junction [43]. Haemoglobin breakdown products, resulting from haemorrhage, have been implicated in epileptogenesis [44].
Changes in molecular signaling involving gene induction and modifications of neurotransmitter receptors and ion channels occur early after an injury. Axonal sprouting and dendritic modifications (such as mossy fiber sprouting) happen later on. A variety of mechanisms, including blood-brain barrier disturbances, inflammatory responses and release of related cytokines have also been implied [43]. All of the above changes result in an increased excitability that lowers seizure threshold.
Neuronal damage extends past an acute hypoxic insult and into the reperfusion phase. Pathophysiological mechanisms include apoptosis, activation of inflammatory mediators [45] as well as excessive extracellular glutamate excitotoxicity and intracellular accumulation of calcium [46]. Astrocytes post-insult release signals (such as thrombospondins) that increase excitatory synapse formation [47].
Apart from mechanisms leading to increased neuronal excitation, tissue necrosis and liquefaction can result in the formation of isolated cortical foci. Animal models of cortical isolation (“undercut” models) have shown a selective loss of GABAergic interneuron [48], resulting in a limitation of inhibitory mechanisms, which also contributes to epileptogenesis. It is worth noting that cortical isolation is present in both acquired (PTE, hypoxic injury) and developmental structural epilepsies.
2.4.3.2 Hippocampal Sclerosis (HS)
HS is present in at least 30 % of all epilepsy cases, according to both surgical [49] and post-mortem [50] series. HS is mainly associated with mesial temporal lobe epilepsy (MTLE) and reported in 50–70 % of patients with TLE and MTLE [51].
Whether HS is the cause or a consequence of seizures remains a highly controversial subject. Although status epilepticus has been proved to cause neuronal death, whether brief seizures amount to a similarly deleterious effect is still debated. Studies supporting the claim that the type of precipitating injury, seizure frequency and severity influence HS abound [52]. On the other hand, it has been proposed that hippocampal abnormalities in TLE play a pathogenetic role. Further support to this claim comes from imaging studies, showing that the degree of hippocampal atrophy is not correlated with the duration and severity of seizures [53]. Also, patients with multiple or poorly controlled seizures, as well as patients in a distinct subgroup of TLE, do not always display hippocampal sclerosis and neuronal loss. Finally, it has also been suggested that the pathologic alterations observed in sclerotic hippocampi can result from an abnormal cell migration during brain development [54].
Histopathologically, two areas of the hippocampus are mainly affected in HS: Ammon’s horn and the dentate gyrus. In Ammon’s horn, there is a marked neuronal depletion and astrocytic proliferation. These astrocytes display increased expression of glutamatergic receptors and are more capable of generating action potential-like responses in vitro compared to normal astrocytes [55]. In the dentate gyrus, loss and dispersion of granule cells, growth of new fiber systems (mossy fiber sprouting), loss of inhibitory interneurons and upregulation of inhibitory neurotransmission (perhaps in an attempt to curb increased excitation) are observed. In contrast to these changes, the subiculum (which is the main output region of the hippocampus) remains intact [56]. Nevertheless, it has been reported to contribute to epileptogenesis by initiating spontaneous interictal discharges [57].
ILAE classifies HS in three distinct categories, based on the regions (CA1 or CA4) involved in neural cell loss and gliosis. These categories differ in epilepsy history and prognosis of postsurgical seizure control [54].
2.4.3.3 Tumor-Associated Epilepsy (TAE)
Epilepsy is far more common in brain tumor patients than in the general population. Compared to high-grade tumors and cerebral metastases, low-grade gliomas are linked to a higher risk of seizures. Although the longer survival rate of patients with low-grade tumors, as well as molecular differences of each tumor category, could contribute to these findings, slow growing tumors might deafferentate cortical areas and thus create highly epileptogenic foci, as opposed to high-grade tumors that could induce epilepsy mainly through rapid tissue disruption and necrosis [58]. The most common seizure types in TAE are generalized tonic-clonic and complex partial seizures.
Evidence from both animal models [59, 60] and patients with TAE [61, 62] point towards the fact that crucial changes occur in the peritumoural region and not the immediate tumor invasion zone. These include glial cell swelling and damage resulting from hypoxia, acidosis [63] and altered expression of glutamate receptors in reactive astrocytes.
Numerous studies have shown that a frontal location of the tumor (and thus close to the premotor and motor cortex) is associated with a higher probability of associated epilepsy [64, 65]. Propagation of abnormal signals and/or a disruption of electrical activity transmitted to the primary motor cortex could be a logical explanation for the higher incidence of epilepsy when a tumor is located closer to the premotor cortex. In addition, the limbic and temporal lobe, the primary somatosensory cortex (S-I) and the opercula and insula regions of the secondary somatosensory area (S-II) also have a low threshold for producing seizures [65]. Notable exceptions include medial sphenoid wing meningiomas (where incidence of seizures is low) and seizure-like phenomena associated with posterior temporal-inferior occipital lesions [66].
2.4.4 Seizure Precipitants and Modulators
2.4.4.1 Sleep Deprivation
There is a controversy regarding seizures occurring after sleep deprivation. EEG recordings after sleep deprivation in epilepsy patients have been widely used, while sleep deprivation is known to activate epileptiform discharges independently of the activating effects of sleep [67]. However, seizures occurring after sleep deprivation are not classified as provoked by ILAE [15] and epilepsy specialists [68], since recurrence is far more likely than for patients with a provoked seizure. Further confounding to this issue, sleep deprivation is causing severe stress, a known seizure promoting factor, so it is hard to say whether epilepsy aggravation upon sleep deprivation is a direct effect (Chap. 3 will elaborate on the complex relationship between sleep and epilepsy).
2.4.4.2 Stress and Epilepsy
Seizures, particularly infantile spasms, have been linked to a stress-related elevation of CRH, which is responsible for the cascade leading to the production of adrenal steroids (such as cortisol). CRH has been found to act proconvulsively on seizure-prone brain regions such as the limbic system [69], by enhancing the actions of glutamate and suppressing afterhyperpolarisation [70]. Glucocorticoids limit the production of CRH as part of a negative feedback loop. Nevertheless, they activate CRH gene expression in the amygdala (a potential proconvulsive action) while adrenal-derived neuropeptides have both pro- and anticonvulsive properties [71]. Adrenocorticotropic hormone (ACTH) is released from the pituitary in response to hypothalamic CRH and has been proved to be anticonvulsive. ACTH also suppresses CRH, while inducing steroid synthesis, and thus is superior to oral steroids in the treatment of infantile spasms [72]. Under the influence of CRH, β-endorphin is released in an attempt of stress-level reduction. It acts as an endogenous opioid (μ-receptors), inhibiting the release of GABA and increasing dopamine levels [73] hence its excitatory effect.
2.4.4.3 Epilepsy and Reproductive Hormones
While men are reported to be more susceptible to epilepsy [74], sex-specific seizure propensity differs in various epilepsy syndromes. Sex-related differences are mainly thought to be the consequence of estrogen, progestin and androgens, which are also responsible for sexual brain dimorphism and behaviour patterns [75].
Ten to seventy percent of female patients with epilepsy has a greater propensity to seize in specific phases of their menstrual cycle, a “clustering” termed catamenial epilepsy, and observed in premenstrual and preovulatory periods, where the estrogen/progesterone ratio is high. Progesterone has antiepileptic properties, mediated by the GABAergic neurosteroid allopregnanolone, while it also has receptors in the limbic system. Estrogen, on the other hand, is primarily proconvulsive, by directly affecting glutamate receptor subtypes and increasing the density of hippocampal dendritic spines and excitatory synapses in animal models. Nevertheless, it has also been reported to increase neuropeptide Y concentration, with a possible antiepileptic effect [76].
2.5 Pathophysiology of Seizures and Epilepsy
Medicine is both art and science. The Hippocratic art of healing becomes a medical science to the extent that we succeed to identify which physiological function is changed in each disease and by what mechanism. Decades of neurological and neurosurgical observations have made numerous such links between the expression of seizures (loss of motor control, consciousness etc.) and the normal function of the particular brain areas which appear to initiate epileptic discharges and/or show lesions in each patient. In the process epileptology has become the greatest school for neuroscience, i.e. the description of the motor homunculus (for motor control), correlates of consciousness etc. More recently basic research in epileptology has elucidated many mechanisms underlying the expression of seizures at the macroscopic (brain imaging) and microscopic levels, especially in the ionic channels and neurotransmitter systems involved in the expression of seizures. Knowledge at the mesoscopic level (brain circuits) is seriously lagging behind. The most crucial question of mechanisms underlying epileptogenesis is still unanswered, although strides are currently made in this direction by molecular genetics and neuroplasticity research.
2.5.1 Basic Neurophysiology
GABA is the major inhibitory neurotransmitter in the brain. GABAA receptors coupled to chloride are involved to the hyperpolarizing of membranes which enables the inhibition of neuronal activity. The chloride mediated hyperpolarizing current counterbalances the excitatory input’s depolarizing currents and needs to be overcome for an action potential to fire. As data of animal models suggest, the acute GABAA receptor blockade will produce epileptic activity while in addition the GABAA receptors are the targets of many anticonvulsant medications which are currently in use. Benzodiazepines and topiramate increase the rate of chloride channels opening while barbiturates increase the duration that these channels remain open thus decreasing excitability. GABAB receptors show a similar action through a different mechanism. GABAB receptors couple to potassium channels and form a current with longer duration of action compared to the GABAA receptor activation [77].
Glutamate on the other hand, is a major excitatory neurotransmitter in the brain, mediated by three main receptors: N-methyl-d-aspartic acid (NMDA), alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA)/kainite and metabotropic. Selective NMDA receptor agonists show proconvulsant action while antagonists of the AMP/kainite and NMDA receptors have antiepileptic properties [78].
Glia cells and gap junctions between neuron cells facilitate voltage spread. GABA regulates the release and reuptake of neurotransmitters and transporters located both on glia and neurons. Furthermore, glia regulates the extracellular potassium concentration, which is correlated to neuronal excitability and epilepsy [79].
Two main types of ion channels exist. The ligand-gated channels which are activated by GABA, glutamate and acetylcholine, mediate cell communication at the synapse while the voltage-gated channels mediate the action potential and the axonal conduction of electrical signals. During resting state, the latter are closed and they open with the local membrane potential changes. Abnormalities of these channels lead to a disruption of membrane’s depolarization and repolarization that is necessary for the action potential. Several studies have suggested that channelopathies can be the underlying cause of certain epileptic syndromes. Generalized Epilepsy with Febrile Seizures Plus (GEFS+) is linked to missense mutations in sodium (NaV1.1) channels, while complete loss-of-function mutations in NaV1.1 cause Severe Myoclonic Epilepsy of Infancy. Benign Neonatal Infantile Seizures is also caused by mutations in sodium (NaV1.2) channels [80]. Potassium channelopathies have been implicated in Sudden Unexplained Death in Epilepsy (SUDEP, Kv1.1) [81], while monogenic idiopathic generalized epilepsies (IGE) have been associated with mutations in GABAA receptor genes [82]. Absence epilepsies have also been linked to GABAA [83], GABAB [84] as well as voltage-gated calcium channel dysfunction [85].
Neuromodulators (such as neuropeptides and neurosteroids) are endogenous factors that influence the balance between excitation and inhibition in the brain. Neuropeptides regulate GABAergic and glutamatergic neurotransmission, as well as the monoaminergic system. Neurosteroids are locally synthesized from cholesterol and circulating steroid hormones, and mostly target membrane receptors.
Many neuropeptides have been identified as endogenous antiepileptics. However, only one is currently in use as a treatment (ACTH). Other anticonvulsant neuropeptides include neuropeptide Y, which increases neocortical GABAergic neurotransmission and hippocampal dopamine, and somatostatin (expressed, most importantly, in GABA-ergic, inhibitory hippocampal hilar interneurons) [86].
The list of proconvulsant neuropeptides includes, among others, corticotropin-releasing hormone (CRH), β-endorphin and arginine-vasopressin peptide (AVP). While the former two are implicated in stress-related mechanisms, high levels of AVP have been associated with febrile seizures, given that this peptide in lower levels also acts as an endogenous antipyretic [87].
2.5.2 Hypersynchrony, Hyperexcitation and Epileptogenesis
Current research converges on the notion that seizures erupt when two fundamental measures of neuronal activity, excitability and synchronization, surpass certain normal level and that epileptogenesis is based on an aberrant exploitation of the most fundamental property of our brain, neuronal plasticity, the very one that enables us to develop, adopt to the environment and learn.
The early Penfield and Jasper’s hypothesis on generalized seizures introduced the idea of seizures correlating to synchronous brain activity characterized by decreased inhibition and enhanced excitation leading to the transient hypersynchronous activity of electrical epileptiform discharges [88]. The hallmarks of epilepsy which refer to hypersynchrony and hyperexcitation, still remain. Yet, synchronization in epilepsy is complex and it strongly depends on how ‘synchrony’ is defined, on the signals being measured (i.e. neuronal spikes or field potentials) and the spatial scale [89].
There is a variety of possible causes of hyperexitability. They can be intrinsic to neurons, like changes of types, numbers and opening times of voltage gated ion channels for Na+ or Ca2+, which may occur post-translationally, through 2nd messengers or through modulation of gene expression. They can also be extrinsic, like changes of local ion concentrations i.e. in [K+], and in extracellular space or modulation of transmitter metabolism or uptake by glial cells. Finally they can be synaptic, like increased excitatory post synaptic potentials (usually mediated by glutamate) and/or decreased inhibitory potentials (usually mediated by GABA), alterations in expression of transmembrane gated ionotropic channels, remodeling of synapse location or configuration, changes in gap-junction synaptic function etc. Simply put, it is a matter of balance tipped in favor of excitation in specific neurons (Fig. 2.1).
(a) Simplified view of excitability changes towards an epileptiform activity. (b) Comparison of a normal neuronal discharge (upper) to an epileptiform one (lower). A = excitatory postsynaptic potential, B = sodium channel mediated action potential, C = inhibitory postsynaptic potential. Blockage of C leads to delayed and persistent expression of NMDA receptor channels mediated Ca++ spikes and paroxysmal depolarization shift (D)
Synchronization can be increased in an equally large number of different ways like: recurrent excitation of neighbouring neurons, rhythms offering a narrow time window of higher opportunity to fire, gap junctions and rebound from synchronous inhibition.
Neuronal populations synchrony caused by an excitation/inhibition imbalance along with alterations in neural communication are key elements of epileptogenesis, while glia cells, through their extracellular modulation of environment, also play a role to it.
Hyperexcitability, i.e. burst of action potentials and paroxysmal depolarization shifts coupled with hypersynchronization of neighboring neurons may lead to seizure local initiation. Activation of connected neurons with concomitant loss of surround inhibition can lead to seizure propagation to other brain areas.
Epileptogenesis is a dynamic process which progresses until the manifestation of the first clinical seizure. Changes on neuronal interconnectivity and excitability are present [5], either in relation to a genetic susceptibility to seizures [90] or to an identifiable structural brain lesion [25].
One feature that facilitates seizures in the cortex is the existence of positive feedback loops between the pyramidal neurons which enable them to excite each other. Therefore, the connection structure of the neuronal network (rather than the density of existing neurons) seems to be of high importance to epileptogenesis [91, 92].
The fact that there is a wide diversity of seizure types, apparent causes and the variety of epileptic syndromes phenomenology [93] does not make it possible for a single pathophysiologic mechanism to underlie it all.
Epileptogenesis consists of a variety of intracellular, intrinsic membrane and extracellular mechanisms with neuronal plasticity and glia offering adaptation to environmental changes [94]. Therefore, the existence of a small group of neurons being responsible for epileptic discharges which then spread throughout the rest of the brain is also unlikely.
Epileptogenesis is considered to take several years in three stages (Fig. 2.2) and mainly unexplored remains the 2nd one: the latent period. If the initial insult is not countered several modification in the brain are escalated leading to epileptogenesis and expression of the first spontaneous seizures. Things may stabilize there or worsen in which case chronic epilepsy is established. Pharmacoresistance may develop either because antiepileptic drugs cannot cope with the new hypersynchronous and complex networks which newly emerge or because their membrane targets have changed or because mechanisms develop which decrease their brain levels.
The putative mechanisms of epileptogenesis as they emerge from research in several animal models have been recently reviewed [85, 95–101]. In retrospect, probably the most influential animal model has been that of kindling induced epilepsy in rodents [102]. An example of significant relevance between animal and human studies is the observation that hippocampus is the brain area most vulnerable to epileptogenesis and specifically its anterior part (in humans—ventral in rodents a distinction based on still unresolved underlying mechanisms (see [103, 104].
Epilepsy syndromes can be broadly separated in two categories: generalized and focal epilepsies. Focal onset seizures and generalized onset seizures differ in terms of the main mechanisms involved. While in both types of seizures cellular excitability is increased, the mechanisms of synchronization differ.
2.5.3 Pathophysiology of Focal Epilepsy
Pyramidal neurons receive a large amount of excitatory input in contrast to the relatively less inhibitory one. Yet, with inhibitory synapses being on the soma and close to axon hillock, inhibition is able to counterbalance the large amount of excitation received through ‘gating it out’, an effect known as the ‘inhibition veto’ [105].
A paradoxical action of inhibitory interneurons, being active during seizure onset, suggests this as the basis of a cellular correlate to the large scale discharges that are recorded in EEG. A period of intense activation of interneurons is followed by recurrent discharges of principal excitatory cells which had been ‘silenced’ during the inhibitory activation. These fast oscillations are important markers of the seizure onset zone. Possible mechanisms of this action is firstly the extracellular increase of potassium concentration which will cause depolarization of membranes and as a result the increase of excitatory neurons discharges and secondly the intracellular increase of chloride within the principal excitatory neuron which results to the impairment of inhibition and thus an excitation/inhibition imbalance. It has been shown that the reversed chloride gradient is correlated to GABA having an excitatory effect on neurons [106].
There are suggestions that the seizure onset zone is organized in microdomains which present synchronous high frequency firing in the form of ‘microseizures’ [107]. The merging of these cortical microdomains is proposed as the mechanism underlying the ictal transmission and the emergence of the macroseizure [89].
At the time that a seizure initiates, an early ictal desynchronization is noted. As the seizure progresses, this is followed by an increasing large scale synchronization [108, 109]. A possible explanation of this phenomenon is the ‘inhibition veto’ induced by the area ahead of the ictal waveform [105].
Long lasting repetitive seizures, as seen in status epilepticus, lead to a progressive and permanent modification of cortical neuronal networks thus repetitive seizures will lead to spontaneous recurrent seizures. This might also be true in the cases of acquired epileptogenesis for example after brain damage. The degeneration of GABAergic interneurons and the spouting of new glutamatergic circuits both leading to increased excitation is a consistent finding in both animal models and human tissue studies. This diminished inhibition permits the recurrent excitation and multisynaptic network activation while the remaining GABAergic inhibition prevents it from happening continually [110]. Repetitive seizures cause neuronal damage which strongly depends on the seizure severity as this is recorded by electrographic recordings. Neuronal death and synaptic regeneration appear to be important mechanisms to epileptogenesis.
Beyond the cell level though, epileptic seizures are also “multi- scale network phenomena”. Networks can be represented as a graph made of nodes and links between them. Small worlds as they have been described by Watts and Strogatz [111], have many local links and a few of long-range connections. This characteristic allows them to locally process information and at the same time coordinate this local activity by long range connections, therefore balancing ‘segregation’ and ‘integration’ which are crucial for information processing. A network’s topography (i.e. how the nodes are connected or in regard to epileptic seizures in the brain, cortex topography) will influence the dynamics that take place on the network.
Spatial scale’s impact of synchronization can be seen in the high frequency interictal discharges. Populations of neurons synchronize their action potential firing which manifests as high-frequency oscillations with spectral peaks correlating to the inter-spike frequency of individual neurons at the 200–300 Hz. Also, in chronic epilepsy, the presence of interictal high frequency oscillations (i.e. fast ripples) which have a much higher firing frequency than the maximum firing rate of the pyramidal neuron, suggests the emergence of a network phenomenon generated by out-of-phase neuronal populations [89].
Finally, synchronization reaches its maximum close to seizure termination. It has been suggested that synchronization’s enhancement or disruption promotes the seizure termination, proposing that once all of the available neural correlates are integrated within the synchronous paroxysmal activity, the seizure terminates because of the emergence of an extended ‘hypoexcitable area’. A synchronized neural bursting can be terminated either by the decreased excitatory transmission caused by the massively increased membrane conductance [112] or by the synchronized inhibition; inhibition can be synchronized by synchronized excitation due to the interconnectivity between inhibitory interneurons and their connections to the principal excitatory cells [113]. On top of that, extracellular environmental changes can further contribute to seizure termination [114].
2.5.4 Pathophysiology of Generalized Epilepsy
Generalized seizures can be classified as atonic, tonic, clonic, tonic-clonic, myoclonic, or absence seizures on the basis of clinical symptoms and EEG abnormalities. Typical absence seizures and the interactions of the thalamocortical circuitry have been used as examples to understand the pathophysiological mechanisms underlying generalized seizures.
Especially the mechanisms underlying the conspicuous EEG rhythm of 3/s generalized spike and wave discharges (GSWD) and the transient “loss of consciousness” characterizing these seizures have been investigated for over eight decades because—although relatively benign—they are thought to constitute a unique electrographic and behavioral marker of the genetic predisposition to most types of epilepsy [115–117]. Interestingly, the subject is still controversial since both its classification terms, idiopathic and primary generalized, are recently proposed to be abandoned. The question of the neuronal mechanisms underlying the generation of GSWD and the concomitant “loss of consciousness” will be more properly dealt with in the next chapter (Chap. 3), since it relates to some mechanisms of sleep [118, 119]. Regarding the second term, all seizures, even those associated with what have historically been thought of as ‘primary generalized’ epilepsies, are considered now to originate in local microcircuits and then propagate from that initial ictogenic zone [7]. The matter goes beyond semantics and is of crucial practical importance to the clinic where the pharmacology of seizures known as generalized is quite distinct from that of focal epilepsies. The long history of conceptual developments as for the mechanisms by which rhythmical GSWD appear so very synchronous all over the brain (in titles in Fig. 2.3a) can be found in [6, 115, 117, 118, 120].
According to the prototype epileptic circuit (Fig. 2.3b) there is always a focus from where generalized seizures start. This neocortical focus develops in mutual influence with the thalamocortical neurons of its sector and initiates activity in GABAergic neurons of reticular thalamic nucleus. The interaction of thalamocortical and reticular neurons sets the pace of the oscillatory neuronal activity, while seizures spread through cerebral networks and subsequent involvement of the newly recruited cortex in cortico-thalamo-cortical reverberations, resulting in a globally synchronous EEG rhythm. According to this general prototype, locally-lead (mostly frontally) GSWD and absences have been referred to as “frontal absences” and thought to represent fast secondary generalization by a frontal focus [122]. They correspond to those with apparently localized onset of the ILAE guidance [26].
To better understand the nature of focal SWDs (FSWDs) in relation to GSWD in idiopathic generalized epilepsy Koutroumanidis and colleagues [123, 124] studied video-EEG recordings of children with typical childhood absence epilepsy. In particular they studied their behavior during the different phases of sleep microstructure and the topographic relation of the FSWDs to the EEG leading areas of the absences in each child. They found significant concordance (80 %) between the interictal FSWD (in blue frame in Fig. 2.4) and the “lead-in” or pre-generalization-FSWD (indicated by blue arrows in Fig. 2.4) in waveform, topography, in onset and propagation patterns as well in their affiliation to CAP-B periods. On the contrary the first generalized spike of the sustained 3/s GSWD (indicated by red arrows in Fig. 2.4) showed limited variability and only 8.2 % concordance with the focal SWD and the focal (pre-generalisation) SWD, while appearing in proximity to CAP-A and sleep transition periods. In general, focal SWDs were frontal or occipital, while the generalized mostly fronto-temporal or temporal (Fig. 2.4 right). These studies concluded that focal “lead in” or pre-generalization SWD are not likely the determinants of GSWD. They may reflect a system of multifocal non-localizing electrically unstable cortical areas that under the facilitatory influence of exogenous or endogenous factors like sleep instability can foster a corticothalamic response strong enough to generate 3 Hz GSWD in long preset networks—of autonomous onset location—that are conditionally sustainable and potentially ictal. FSWD can be viewed as incomplete forms of the GSWD; together they define the EEG identity of idiopathic “generalized” epileptogenesis. It is worth exploring the relationship between the characteristics of the focal as well as the generalized EEG signs and the variation in behavioral deficits in different absence seizures. Such electroclinical investigation may reveal what is lost in particular absence seizures [123, 124].
Comparison of topographic features of the first SWD in a sustained 3/s GSWD (red arrows), singular interictal focal SWD (in blue frame) and “lead in” or pre-generalization focal SWD (modified from [124])
The recognition of focal onset generalized epilepsies does not take the magic away from the spectacular synchronization of GSWD and the associated behavioral changes of IGE. On the contrary it kindles interest on the brain mechanisms which have prepared (probably through long epileptogenesis) specific brain-wide circuits to be ready to respond to cortical hyperexcitability in this so well organized way. These considerations are in line with increasing acceptance of epilepsy as a network disease. Epileptic activity is increasingly considered as the dysfunction of a neuronal networks, a multi-entrance circuits rather than a single pinpoint source [125]. Gloor’s 1968 paper on corticoreticular epilepsy (see Fig. 2.3a) had a pioneering influence in this direction [126]. Brain networks are neither orderly nor random; they are very complex and non-linear; but both of the latter are quantifiable. Recent observations suggest that networks acquire larger path lengths and clustering coefficients near the beginning of the seizure and that become more small-world during seizure propagation and more random at seizure termination, when there is also increased coupling. Contradiction in data exist, but the total evidence converges to the suggestion of a refinement of the traditional idea that seizures are hypersynchronous events [127]. In parallel or perhaps in consequence to the network aspects of epilepsy there is a very interesting fermentation about the concept of “system epilepsies” [128–130] to describe some types of epilepsy that depend on the dysfunction of specific functional neural systems.
Typical absence seizures and the interactions of the thalamocortical circuitry are examples used to understand the pathophysiological mechanisms underlying generalized seizures. The thalamocortical circuitry consists of the pyramidal neurons of the neocortex, the thalamic relay nucleus and the thalamic nucleus reticularis and it generates the sleep spindles observed during NREM sleep. The thalamocortical systems thus appears as the primary hub of neural processes common to sleep and generalized epilepsy and possibly underlying their mutual relationships.
References
Staley K (2015) Molecular mechanisms of epilepsy. Nat Neurosci 18(3):367–372. doi:10.1038/nn.3947
Engel J Jr (2013) Progress in the field of epilepsy. Curr Opin Neurol 26(2):160–162. doi:10.1097/WCO.0b013e32835ee5a3
Panayiotopoulos CP (2005) Idiopathic generalized epilepsies: a review and modern approach. Epilepsia 46(Suppl 9):1–6. doi:10.1111/j.1528-1167.2005.00330.x
Fisher RS, van Emde BW, Blume W, Elger C, Genton P, Lee P, Engel J Jr (2005) Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 46(4):470–472. doi:10.1111/j.0013-9580.2005.66104.x
Engel J Jr, Pedley TA (2005) What is epilepsy? In: Engel J (ed) Epilepsy: a comprehensive textbook. Lippincott Williams & Wilkins\Raven Press, Philadelphia, pp 1–11
Avoli M (2012) A brief history on the oscillating roles of thalamus and cortex in absence seizures. Epilepsia 53(5):779–789. doi:10.1111/j.1528-1167.2012.03421.x
Paz JT, Huguenard JR (2015) Optogenetics and epilepsy: past, present and future. Epilepsy Curr 15(1):34–38. doi:10.5698/1535-7597-15.1.34
Temkin O (1945) The falling sickness. The John Hopkins Press, Baltimore, p 380
Saraceno BA, G, Lee P (2005) Atlas: epilepsy care in the World
Thurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, Ding D, Hesdorffer DC, Hauser WA, Kazis L, Kobau R, Kroner B, Labiner D, Liow K, Logroscino G, Medina MT, Newton CR, Parko K, Paschal A, Preux PM, Sander JW, Selassie A, Theodore W, Tomson T, Wiebe S, ILAE Commission on Epidemiology (2011) Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia 52(Suppl 7):2–26. doi:10.1111/j.1528-1167.2011.03121.x
Forsgren L, Beghi E, Oun A, Sillanpaa M (2005) The epidemiology of epilepsy in Europe—a systematic review. Eur J Neurol 12(4):245–253. doi:10.1111/j.1468-1331.2004.00992.x
Effertz T, Mann K (2013) The burden and cost of disorders of the brain in Europe with the inclusion of harmful alcohol use and nicotine addiction. Eur Neuropsychopharmacol 23(7):742–748. doi:10.1016/j.euroneuro.2012.07.010
Guekht AB, Mitrokhina TV, Lebedeva AV, Dzugaeva FK, Milchakova LE, Lokshina OB, Feygina AA, Gusev EI (2007) Factors influencing on quality of life in people with epilepsy. Seizure 16(2):128–133. doi:10.1016/j.seizure.2006.10.011
Isaacs KL, Philbeck JW, Barr WB, Devinsky O, Alper K (2004) Obsessive-compulsive symptoms in patients with temporal lobe epilepsy. Epilepsy Behav 5(4):569–574. doi:10.1016/j.yebeh.2004.04.009
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel J Jr, Forsgren L, French JA, Glynn M, Hesdorffer DC, Lee BI, Mathern GW, Moshe SL, Perucca E, Scheffer IE, Tomson T, Watanabe M, Wiebe S (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55(4):475–482. doi:10.1111/epi.12550
Surges R, Thijs RD, Tan HL, Sander JW (2009) Sudden unexpected death in epilepsy: risk factors and potential pathomechanisms. Nat Rev Neurol 5(9):492–504. doi:10.1038/nrneurol.2009.118
Simonato M, Brooks-Kayal AR, Engel J Jr, Galanopoulou AS, Jensen FE, Moshe SL, O’Brien TJ, Pitkanen A, Wilcox KS, French JA (2014) The challenge and promise of anti-epileptic therapy development in animal models. Lancet Neurol 13(9):949–960. doi:10.1016/S1474-4422(14)70076-6
Morris GL, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C (2013) Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Epilepsy Curr 13(6):297–303. doi:10.5698/1535-7597-13.6.297
Krumholz A, Wiebe S, Gronseth G, Shinnar S, Levisohn P, Ting T, Hopp J, Shafer P, Morris H, Seiden L, Barkley G, French J, Quality Standards Subcommittee of the American Academy of Neurology, American Epilepsy Society (2007) Practice parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology 69(21):1996–2007
DeToledo JC, Ramsay RE (1996) Patterns of involvement of facial muscles during epileptic and nonepileptic events: review of 654 events. Neurology 47(3):621–625
Rosenow F, Luders H (2001) Presurgical evaluation of epilepsy. Brain 124(Pt 9):1683–1700
Martinkovic L, Hecimovic H, Sulc V, Marecek R, Marusic P (2014) Modern techniques of epileptic focus localization. Int Rev Neurobiol 114:245–278. doi:10.1016/B978-0-12-418693-4.00010-8
Pohlmann-Eden B, Beghi E, Camfield C, Camfield P (2006) The first seizure and its management in adults and children. BMJ 332(7537):339–342. doi:10.1136/bmj.332.7537.339
Kattimani S, Bharadwaj B (2013) Clinical management of alcohol withdrawal: a systematic review. Ind Psychiatry J 22(2):100–108. doi:10.4103/0972-6748.132914
Engel J, Jr., International League Against E (2001) A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE Task Force on Classification and Terminology. Epilepsia 42(6):796–803
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde BW, Engel J, French J, Glauser TA, Mathern GW, Moshe SL, Nordli D, Plouin P, Scheffer IE (2010) Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia 51(4):676–685. doi:10.1111/j.1528-1167.2010.02522.x
Berg AT, Cross JH (2012) Classification of epilepsies and seizures: historical perspective and future directions. Handb Clin Neurol 107:99–111. doi:10.1016/B978-0-444-52898-8.00005-7
Berg AT (2012) Introduction: changing terms and concepts for epilepsy. Epilepsia 53(Suppl 2):1–2. doi:10.1111/j.1528-1167.2012.03549.x
Thom M (2014) Review: hippocampal sclerosis in epilepsy: a neuropathology review. Neuropathol Appl Neurobiol 40(5):520–543. doi:10.1111/nan.12150
Verhaert K, Scott RC (2010) Acute symptomatic epileptic seizures. In: Panayiotopoulos CP (ed) Atlas of epilepsies. Springer, London
Italiano D, Ferlazzo E, Gasparini S, Spina E, Mondello S, Labate A, Gambardella A, Aguglia U (2014) Generalized versus partial reflex seizures: a review. Seizure 23(7):512–520. doi:10.1016/j.seizure.2014.03.014
Reid AY, Galic MA, Teskey GC, Pittman QJ (2009) Febrile seizures: current views and investigations. Can J Neurol Sci 36(6):679–686
Pavlidou E, Hagel C, Panteliadis C (2013) Febrile seizures: recent developments and unanswered questions. Childs Nerv Syst 29(11):2011–2017. doi:10.1007/s00381-013-2224-3
Dahlgren L, Wilson RD (2001) Prenatally diagnosed microcephaly: a review of etiologies. Fetal Diagn Ther 16(6):323–326
Kim JH (2001) Pathology of epilepsy. Exp Mol Pathol 345–367
Wong JH, Awad IA, Kim JH (2000) Ultrastructural pathological features of cerebrovascular malformations: a preliminary report. Neurosurgery 46(6):1454–1459
Annegers JF, Coan SP (2000) The risks of epilepsy after traumatic brain injury. Seizure 9(7):453–457. doi:10.1053/seiz.2000.0458
Agrawal A, Timothy J, Pandit L, Manju M (2006) Post-traumatic epilepsy: an overview. Clin Neurol Neurosurg 108(5):433–439. doi:10.1016/j.clineuro.2005.09.001
Raymont V, Salazar AM, Lipsky R, Goldman D, Tasick G, Grafman J (2010) Correlates of posttraumatic epilepsy 35 years following combat brain injury. Neurology 75(3):224–229. doi:10.1212/WNL.0b013e3181e8e6d0
Spencer S (2010) Intracranial electrodes. In: Engel J (ed) Epilepsy, a comprehensive textbook. Lippincott, Williams & Wilkins, Philadelphia, pp 1791–1815
Frey LC (2003) Epidemiology of posttraumatic epilepsy: a critical review. Epilepsia 44(Suppl 10):11–17
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW (2007) XIII. Antiseizure prophylaxis. J Neurotrauma 24(supplement 1):S-83–S-86. doi:10.1089/neu.2007.9983
Lamar CD, Hurley RA, Rowland JA, Taber KH (2014) Post-traumatic epilepsy: review of risks, pathophysiology, and potential biomarkers. J Neuropsychiatry Clin Neurosci 26(2):iv–113. doi:10.1176/appi.neuropsych.260201
Willmore LJ, Ueda Y (2009) Posttraumatic epilepsy: hemorrhage, free radicals and the molecular regulation of glutamate. Neurochem Res 34(4):688–697. doi:10.1007/s11064-008-9841-3
Chalak LF, Rollins N, Morriss MC, Brion LP, Heyne R, Sanchez PJ (2012) Perinatal acidosis and hypoxic-ischemic encephalopathy in preterm infants of 33 to 35 weeks’ gestation. J Pediatr 160(3):388–394. doi:10.1016/j.jpeds.2011.09.001
Szydlowska K, Tymianski M (2010) Calcium, ischemia and excitotoxicity. Cell Calcium 47(2):122–129. doi:10.1016/j.ceca.2010.01.003
Lin TN, Kim GM, Chen JJ, Cheung WM, He YY, Hsu CY (2003) Differential regulation of thrombospondin-1 and thrombospondin-2 after focal cerebral ischemia/reperfusion. Stroke 34(1):177–186
Avramescu S, Nita DA, Timofeev I (2009) Neocortical post-traumatic epileptogenesis is associated with loss of GABAergic neurons. J Neurotrauma 26(5):799–812. doi:10.1089/neu.2008.0739
Blumcke I, Coras R, Miyata H, Ozkara C (2012) Defining clinico-neuropathological subtypes of mesial temporal lobe epilepsy with hippocampal sclerosis. Brain Pathol 22(3):402–411. doi:10.1111/j.1750-3639.2012.00583.x
Novy J, Belluzzo M, Caboclo LO, Catarino CB, Yogarajah M, Martinian L, Peacock JL, Bell GS, Koepp MJ, Thom M, Sander JW, Sisodiya SM (2013) The lifelong course of chronic epilepsy: the Chalfont experience. Brain 136(Pt 10):3187–3199. doi:10.1093/brain/awt117
de Tisi J, Bell GS, Peacock JL, McEvoy AW, Harkness WF, Sander JW, Duncan JS (2011) The long-term outcome of adult epilepsy surgery, patterns of seizure remission, and relapse: a cohort study. Lancet 378(9800):1388–1395. doi:10.1016/S0140-6736(11)60890-8
von Lehe M, Lutz M, Kral T, Schramm J, Elger CE, Clusmann H (2006) Correlation of health-related quality of life after surgery for mesial temporal lobe epilepsy with two seizure outcome scales. Epilepsy Behav 9(1):73–82. doi:10.1016/j.yebeh.2006.03.014
Bower SP, Kilpatrick CJ, Vogrin SJ, Morris K, Cook MJ (2000) Degree of hippocampal atrophy is not related to a history of febrile seizures in patients with proved hippocampal sclerosis. J Neurol Neurosurg Psychiatry 69(6):733–738
Blumcke I, Thom M, Aronica E, Armstrong DD, Bartolomei F, Bernasconi A, Bernasconi N, Bien CG, Cendes F, Coras R, Cross JH, Jacques TS, Kahane P, Mathern GW, Miyata H, Moshe SL, Oz B, Ozkara C, Perucca E, Sisodiya S, Wiebe S, Spreafico R (2013) International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: a Task Force report from the ILAE Commission on Diagnostic Methods. Epilepsia 54(7):1315–1329. doi:10.1111/epi.12220
O’Connor ER, Sontheimer H, Spencer DD, de Lanerolle NC (1998) Astrocytes from human hippocampal epileptogenic foci exhibit action potential-like responses. Epilepsia 39(4):347–354
de Lanerolle NC, Lee TS, Spencer DD (2012) Histopathology of human epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
Cohen I, Navarro V, Clemenceau S, Baulac M, Miles R (2002) On the origin of interictal activity in human temporal lobe epilepsy in vitro. Science 298(5597):1418–1421. doi:10.1126/science.1076510
Riva M (2005) Brain tumoral epilepsy: a review. Neurol Sci 26(Suppl 1):S40–S42. doi:10.1007/s10072-005-0404-y
Senner V, Kohling R, Puttmann-Cyrus S, Straub H, Paulus W, Speckmann EJ (2004) A new neurophysiological/neuropathological ex vivo model localizes the origin of glioma-associated epileptogenesis in the invasion area. Acta Neuropathol 107(1):1–7. doi:10.1007/s00401-003-0771-5
Buckingham SC, Campbell SL, Haas BR, Montana V, Robel S, Ogunrinu T, Sontheimer H (2011) Glutamate release by primary brain tumors induces epileptic activity. Nat Med 17(10):1269–1274. doi:10.1038/nm.2453
Patt S, Steenbeck J, Hochstetter A, Kraft R, Huonker R, Haueisen J, Haberland N, Ebmeier K, Hliscs R, Fiehler J, Nowak H, Kalff R (2000) Source localization and possible causes of interictal epileptic activity in tumor-associated epilepsy. Neurobiol Dis 7(4):260–269. doi:10.1006/nbdi.2000.0288
Aronica E, Yankaya B, Jansen GH, Leenstra S, van Veelen CW, Gorter JA, Troost D (2001) Ionotropic and metabotropic glutamate receptor protein expression in glioneuronal tumours from patients with intractable epilepsy. Neuropathol Appl Neurobiol 27(3):223–237
Kempski O, Staub F, von Rosen F, Zimmer M, Neu A, Baethmann A (1988) Molecular mechanisms of glial swelling in vitro. Neurochem Pathol 9:109–125
Chang EF, Potts MB, Keles GE, Lamborn KR, Chang SM, Barbaro NM, Berger MS (2008) Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg 108(2):227–235. doi:10.3171/JNS/2008/108/2/0227
Hamasaki T, Yamada K, Yano S, Nakamura H, Makino K, Hide T, Hasegawa Y, Kuroda J, Hirai T, Kuratsu J (2012) Higher incidence of epilepsy in meningiomas located on the premotor cortex: a voxel-wise statistical analysis. Acta Neurochir 154(12):2241–2249. doi:10.1007/s00701-012-1511-1
Beaumont A, Whittle IR (2000) The pathogenesis of tumour associated epilepsy. Acta Neurochir 142(1):1–15
Fountain NB, Kim JS, Lee SI (1998) Sleep deprivation activates epileptiform discharges independent of the activating effects of sleep. J Clin Neurophysiol 15(1):69–75
Lawn N, Lieblich S, Lee J, Dunne J (2014) Are seizures in the setting of sleep deprivation provoked? Epilepsy Behav 33:122–125. doi:10.1016/j.yebeh.2014.02.008
Baram TZ (2007) Models for infantile spasms: an arduous journey to the Holy Grail. Ann Neurol 61(2):89–91. doi:10.1002/ana.21075
Aldenhoff JB, Gruol DL, Rivier J, Vale W, Siggins GR (1983) Corticotropin releasing factor decreases postburst hyperpolarizations and excites hippocampal neurons. Science 221(4613):875–877
Reddy DS (2009) The role of neurosteroids in the pathophysiology and treatment of catamenial epilepsy. Epilepsy Res 85(1):1–30. doi:10.1016/j.eplepsyres.2009.02.017
Jaseja H, Jaseja B, Badaya S, Tonpay P (2012) Superior therapeutic efficacy of adrenocorticotrophic hormone (ACTH) in infantile spasms: emerging evidence. Epilepsy Behav 25(2):250. doi:10.1016/j.yebeh.2012.08.003
Koneru A, Satyanarayana SR, Rizwan S (2009) Endogenous opioids: their physiological role and receptors. Global J Pharmacol 3:149–153
McHugh JC, Delanty N (2008) Epidemiology and classification of epilepsy: gender comparisons. Int Rev Neurobiol 83:11–26. doi:10.1016/S0074-7742(08)00002-0
Scharfman HE, MacLusky NJ (2014) Sex differences in the neurobiology of epilepsy: a preclinical perspective. Neurobiol Dis 72(Pt B):180–192. doi:10.1016/j.nbd.2014.07.004
Reddy DS (2014) Neurosteroids and their role in sex-specific epilepsies. Neurobiol Dis 72(Pt B):198–209. doi:10.1016/j.nbd.2014.06.010
Kaila K, Ruusuvuori E, Seja P, Voipio J, Puskarjov M (2014) GABA actions and ionic plasticity in epilepsy. Curr Opin Neurobiol 26:34–41. doi:10.1016/j.conb.2013.11.004
Ure J, Baudry M, Perassolo M (2006) Metabotropic glutamate receptors and epilepsy. J Neurol Sci 247(1):1–9. doi:10.1016/j.jns.2006.03.018
Foresti ML, Arisi GM, Shapiro LA (2011) Role of glia in epilepsy-associated neuropathology, neuroinflammation and neurogenesis. Brain Res Rev 66(1–2):115–122. doi:10.1016/j.brainresrev.2010.09.002
Catterall WA (2012) Sodium channel mutations and epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
Glasscock E, Yoo JW, Chen TT, Klassen TL, Noebels JL (2010) Kv1.1 potassium channel deficiency reveals brain-driven cardiac dysfunction as a candidate mechanism for sudden unexplained death in epilepsy. J Neurosci 30(15):5167–5175. doi:10.1523/JNEUROSCI.5591-09.2010
Cossette P, Lachance-Touchette P, Rouleau GA (2012) Mutated GABAA receptor subunits in idiopathic generalized epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
Crunelli V, Leresche N, Cope DW (2012) GABAA receptor function in typical absence seizures. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
Han HA, Cortez MA, Snead OC (2012) GABAB receptor and absence epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
Noebels JL (2012) The voltage-gated calcium channel and absence epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper’s basic mechanisms of the epilepsies, 4th edn. National Center for Biotechnology Information, Bethesda
Clynen E, Swijsen A, Raijmakers M, Hoogland G, Rigo JM (2014) Neuropeptides as targets for the development of anticonvulsant drugs. Mol Neurobiol 50(2):626–646. doi:10.1007/s12035-014-8669-x
Richmond CA (2003) The role of arginine vasopressin in thermoregulation during fever. J Neurosci Nurs 35(5):281–286
Penfield W, Jasper H (1954) Epilepsy and the functional anatomy of the human brain. Little, Brown and Company, Boston
Jiruska P, de Curtis M, Jefferys JG, Schevon CA, Schiff SJ, Schindler K (2013) Synchronization and desynchronization in epilepsy: controversies and hypotheses. J Physiol 591(Pt 4):787–797. doi:10.1113/jphysiol.2012.239590
Zara F, Bianchi A (2009) The impact of genetics on the classification of epilepsy syndromes. Epilepsia 50(Suppl 5):11–14. doi:10.1111/j.1528-1167.2009.02113.x
Lothman EW, Bertram EH 3rd, Stringer JL (1991) Functional anatomy of hippocampal seizures. Prog Neurobiol 37(1):1–82
Schevon CA, Cappell J, Emerson R, Isler J, Grieve P, Goodman R, McKhann G Jr, Weiner H, Doyle W, Kuzniecky R, Devinsky O, Gilliam F (2007) Cortical abnormalities in epilepsy revealed by local EEG synchrony. Neuroimage 35(1):140–148. doi:10.1016/j.neuroimage.2006.11.009
Benbadis SR (2001) Epileptic seizures and syndromes. Neurol Clin 19(2):251–270
Lukasiuk K, Pitkanen A (2009) Seizure induced gene expression. In: Schwartzkroin PA (ed) Encyclopedia of basic epilepsy research. Academic, Oxford, pp 1302–1309
McNamara JO, Huang YZ, Leonard AS (2006) Molecular signaling mechanisms underlying epileptogenesis. Sci STKE 356:re12. doi:10.1126/stke.3562006re12
Armijo JA, Valdizan EM, De Las CI, Cuadrado A (2002) Advances in the physiopathology of epileptogenesis: molecular aspects. Rev Neurol 34(5):409–429
Scharfman HE, Brooks-Kayal AR (2014) Is plasticity of GABAergic mechanisms relevant to epileptogenesis? Adv Exp Med Biol 813:133–150. doi:10.1007/978-94-017-8914-1_11
Kandratavicius L, Balista PA, Lopes-Aguiar C, Ruggiero RN, Umeoka EH, Garcia-Cairasco N, Bueno-Junior LS, Leite JP (2014) Animal models of epilepsy: use and limitations. Neuropsychiatr Dis Treat 10:1693–1705. doi:10.2147/NDT.S50371
Ritter LM, Golshani P, Takahashi K, Dufour S, Valiante T, Kokaia M (2014) WONOEP appraisal: optogenetic tools to suppress seizures and explore the mechanisms of epileptogenesis. Epilepsia 55(11):1693–1702. doi:10.1111/epi.12804
Coppola A, Moshe SL (2012) Animal models. Handb Clin Neurol 107:63–98. doi:10.1016/B978-0-444-52898-8.00004-5
Scharfman HE (2007) The neurobiology of epilepsy. Curr Neurol Neurosci Rep 7(4):348–354
McNamara JO (1986) Kindling model of epilepsy. Adv Neurol 44:303–318
Kostopoulos G, Moschovos C, Papatheodoropoulos C (2005) Functional differentiation along the longitudinal axis of hippocampus and its possible relevance to epileptogenesis. Epileptic Disord 7(2):167–170
Bekiari C, Grivas I, Giannakopoulou A, Michaloudi-Pavlou H, Kostopoulos GK, Papadopoulos GC (2015) Dentate gyrus variation along its septo-temporal axis: structure and function in health and disease. In: Lowes Z (ed) Dentate gyrus: structure, role in disease, and potential health implications. Nova, New York
Trevelyan AJ, Sussillo D, Watson BO, Yuste R (2006) Modular propagation of epileptiform activity: evidence for an inhibitory veto in neocortex. J Neurosci 26(48):12447–12455. doi:10.1523/JNEUROSCI.2787-06.2006
Avoli M, de Curtis M (2011) GABAergic synchronization in the limbic system and its role in the generation of epileptiform activity. Prog Neurobiol 95(2):104–132. doi:10.1016/j.pneurobio.2011.07.003
Stead M, Bower M, Brinkmann BH, Lee K, Marsh WR, Meyer FB, Litt B, Van Gompel J, Worrell GA (2010) Microseizures and the spatiotemporal scales of human partial epilepsy. Brain 133(9):2789–2797. doi:10.1093/brain/awq190
Schiff SJ, Sauer T, Kumar R, Weinstein SL (2005) Neuronal spatiotemporal pattern discrimination: the dynamical evolution of seizures. Neuroimage 28(4):1043–1055. doi:10.1016/j.neuroimage.2005.06.059
Cymerblit-Sabba A, Schiller Y (2012) Development of hypersynchrony in the cortical network during chemoconvulsant-induced epileptic seizures in vivo. J Neurophysiol 107(6):1718–1730. doi:10.1152/jn.00327.2011
Ben-Ari Y, Dudek FE (2010) Primary and secondary mechanisms of epileptogenesis in the temporal lobe: there is a before and an after. Epilepsy Curr 10(5):118–125. doi:10.1111/j.1535-7511.2010.01376.x
Watts DJ, Strogatz SH (1998) Collective dynamics of “small-world” networks. Nature 393(6684):440–442. doi:10.1038/30918
Gutkin BS, Laing CR, Colby CL, Chow CC, Ermentrout GB (2001) Turning on and off with excitation: the role of spike-timing asynchrony and synchrony in sustained neural activity. J Comput Neurosci 11(2):121–134
Pavlov I, Kaila K, Kullmann DM, Miles R (2013) Cortical inhibition, pH and cell excitability in epilepsy: what are optimal targets for antiepileptic interventions? J Physiol 591(Pt 4):765–774. doi:10.1113/jphysiol.2012.237958
de Curtis M, Manfridi A, Biella G (1998) Activity-dependent pH shifts and periodic recurrence of spontaneous interictal spikes in a model of focal epileptogenesis. J Neurosci 18(18):7543–7551
Avoli M, Gloor P, Kostopoulos G, Naquet R (1990) Generalized epilepsy: neurobiological approaches. Birkhauser, Boston
Kostopoulos G (1997) Neuronal mechanisms underlying loss of consciousness during absence seizures. In: Kostopoulos G, Rakovic D, Koruga D, Rakic L (eds) Brain and consciousness. ECPD of the UN, Belgrade, pp 185–193
Kostopoulos GK (2001) Involvement of the thalamocortical system in epileptic loss of consciousness. Epilepsia 42(Suppl 3):13–19
Kostopoulos GK (2000) Spike-and-wave discharges of absence seizures as a transformation of sleep spindles: the continuing development of a hypothesis. Clin Neurophysiol 111(Suppl 2):S27–S38
Kostopoulos GK (2009) Brain mechanisms linking epilepsy to sleep. In: Schwartzkroin PA (ed) Encyclopedia of basic epilepsy research, vol 3. Academic, Oxford, pp 1327–1336
Meeren H, van Luijtelaar G, Lopes da Silva F, Coenen A (2005) Evolving concepts on the pathophysiology of absence seizures: the cortical focus theory. Arch Neurol 62(3):371–376. doi:10.1001/archneur.62.3.371
Bertram EH (2013) Neuronal circuits in epilepsy: do they matter? Exp Neurol 244:67–74. doi:10.1016/j.expneurol.2012.01.028
Holmes MD, Brown M, Tucker DM (2004) Are “generalized” seizures truly generalized? Evidence of localized mesial frontal and frontopolar discharges in absence. Epilepsia 45(12):1568–1579. doi:10.1111/j.0013-9580.2004.23204.x
Koutroumanidis M, Tsiptsios D, Kokkinos V, Kostopoulos GK (2012) Focal and generalized EEG paroxysms in childhood absence epilepsy: topographic associations and distinctive behaviors during the first cycle of non-REM sleep. Epilepsia 53(5):840–849. doi:10.1111/j.1528-1167.2012.03424.x
Kokkinos V, Koupparis AM, Kostopoulos GK (2013) An intra-K-complex oscillation with independent and labile frequency and topography in NREM sleep. Front Hum Neurosci 7:163. doi:10.3389/fnhum.2013.00163
Spencer SS (2002) Neural networks in human epilepsy: evidence of and implications for treatment. Epilepsia 43(3):219–227
Kostopoulos GK, Gloor P (2013) Epilepsy is a network disease. In: 30th International Epilepsy Congress, Montreal
Kramer MA, Cash SS (2012) Epilepsy as a disorder of cortical network organization. Neuroscientist 18(4):360–372
Koutroumanidis M (2007) Panayiotopoulos syndrome: an important electroclinical example of benign childhood system epilepsy. Epilepsia 48(6):1044–1053. doi:10.1111/j.1528-1167.2007.01096.x
Avanzini G, Manganotti P, Meletti S, Moshe SL, Panzica F, Wolf P, Capovilla G (2012) The system epilepsies: a pathophysiological hypothesis. Epilepsia 53(5):771–778. doi:10.1111/j.1528-1167.2012.03462.x
Halasz P (2013) How sleep activates epileptic networks? Epilepsy Res Treat 2013:425697. doi:10.1155/2013/425697
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Giourou, E., Stavropoulou-Deli, A., Giannakopoulou, A., Kostopoulos, G.K., Koutroumanidis, M. (2015). Introduction to Epilepsy and Related Brain Disorders. In: Voros, N., Antonopoulos, C. (eds) Cyberphysical Systems for Epilepsy and Related Brain Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-20049-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-20049-1_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20048-4
Online ISBN: 978-3-319-20049-1
eBook Packages: EngineeringEngineering (R0)