Abstract
This chapter reviews the strategies to achieve hemodynamic optimization in the perioperative period, addressing the role of dynamic parameters (SVV, PPV, SPV) and minimally invasive or noninvasive cardiac output monitors to guide intraoperative fluid goal-directed therapy in high-risk surgical patients.
Prof. Biagio Allaria, former Director of the Critical Patient Department of the National Institute for the Study and Treatment of Tumors, Milan. Currently consultant in Clinical Risk Management at the same Institute.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
In order to address the issue of perioperative fluid management in an informed manner, it is important to remember the proportion of body water since this information is vital if action is required to maintain the balance in various regions of the body.
Total body water (TBW) in adults is approximately 60 % of body weight. Water is held by all tissues but is particularly abundant in muscles and relatively scarce in body fat. A young adult with healthy muscles therefore has a higher TBW than an elderly overweight person with small muscles and a large amount of fat.
This distinction has important practical consequences: for example, medicines with a high distribution level that dissolve in body water will have higher dose-dependent plasma levels in overweight patients compared to young adults.
But this knowledge is also useful in assessing the need for infusions to maintain a circulating mass volume within the limits of normal.
Since water is distributed in two large areas, the intracellular compartment (60–65 % of TBW) and the extracellular compartment (35–40 % of TBW), and, in turn, the extracellular area is divided into interstitial (25–30 %) and intravascular (10 %) regions, it is clear that in a man weighing 70 kg with TBW of 42 l, intravascular water is only 4,200 ml, while interstitial water is much greater, at about 12–14 l. Interstitial water is in close contact with intravascular fluids by means of continual exchange.
When a patient loses a circulating mass (which is made up of about 55 % water), there is a rapid rebalance of the liquid component thanks to the interstitium which has a water content that is three times that of the circulation. This therefore reflects a loss of blood content for which there is no hemodynamic alert and which is due exclusively to a reduction in hematocrit. But this miniscule observation is of great significance in the operating room: the patient has lost a blood mass which is replaced by a similar quantity of plasma from the interstitia.
This is, however, a form of compensation that cannot continue in the long term in the event of persistent blood loss.
Until such compensation is sufficient, arterial pressure, heart rate, CVP, and cardiac output are normal, possible fluid challenge is negative, and dynamic monitoring parameters such as SPV, PPV, and SVV are within the limits of normal. The patient has no need of a circulating mass since this has remained normal due to fluids from the interstitia.
In addition to this compensation mechanism, there is the switching of the blood mass from “less noble” compartments such as the splanchnic compartment to those that would be more affected by a decrease in flow, like the heart, brain, and lungs. Again this is a compensation mechanism that, as with the previous one, is not without limits.
Water recovered from the interstitia is also rapidly replaced from the absorption of H2O and Na which is activated in the kidneys.
If the blood loss continues, however, venous return (VR) can be maintained as normal thanks to a fall in CVP. In fact, venous return is calculated using the formula
where MCFP is the mean circulatory filling pressure.
By observing the formula, we can see clearly that if MCFP decreases due to blood loss, venous return remains normal as CVP also falls.
A reduction in CVP is therefore a warning sign, even if arterial pressure and heart rate remain normal. If blood loss continues and therefore the circulating mass, the venous return is reduced and along with it the stroke volume, but cardiac output remains normal thanks to an increase in heart rate. We therefore have three signs of a loss of circulating mass: decreased Htc, decreased CVP, and increased heart rate.
These are wonderful multiple compensation mechanisms that make it possible to overcome any oversight by the anesthetist for a certain amount of time, although he/she must also learn to recognize them early: reduced Htc, reduced daily diuresis (due to tubular reabsorption of H2O and Na), reduced CVP, and increased heart rate are all signs of a hypovolemic process that is compensated for but at risk of leading to hemodynamic deterioration which is not desirable.
If not equipped, cardiac output decreases along with pulse and EtCO2 (which are closely linked to output).
However, unless this is a substantial acute hemorrhage, this point is not reached quickly. In fact, the body can rely not only on interstitial fluids but also intracellular fluids (which make up the majority of TBW), which amount to 24 l in patients weighing 70 kg. The passage of water from cells to the interstitium when needed is immediate and follows osmotic logic.
The extracellular compartments (interstitium and circulation) have osmotic forces that are in balance with the intracellular compartment, which is made up of concentrations of cations and anions that ensure electroneutrality in various sectors. The most important cation in the extracellular compartment is Na+ followed by cations with less importance such as K+, Mg+, and Ca++. Electroneutrality is guaranteed by the presence of anions Cl− and HCO3 − and proteins (especially albumin).
In the intracellular compartment, the most important cation is K+, and the anion PO4 − ensures electroneutrality. Osmolarity is determined by the number of particles dissolved in a solution and is therefore fundamentally determined by Na+ in the plasma and interstitium and K+ in the cells.
These concepts, as far as expected, are very important since they regulate the distribution of water in the body. This can pass freely and rapidly from compartments with low osmolarity to others with greater osmolarity by maintaining identical osmolarity in various compartments.
Why is the intracellular water content much higher than the extracellular content?
This is simply because there is a K salt content in cells that is greater than the Na salt content in extracellular compartments. A change in osmolarity in one area triggers an immediate movement of water to restabilize the balance. This game of water movement applies to the balance between intracellular and extracellular interstitial spaces since the cell membrane is not permeable for ions, and therefore water movement is considerably linked to osmotic forces. In the relationship between capillaries and the interstitium, the mechanism is different since the capillary endothelium is permeable to ions which are therefore no longer part of the osmotic force that can lead to the movement of water. The passage of water is regulated by Starling’s law, and the forces at play are mainly the hydrostatic pressure and oncotic pressure of the capillary and interstitium.
Therefore, when a patient experiences rapid blood loss, the lost volume is quickly replaced by fluids from the interstitium. This results in the maintenance of the hemodynamic balance, and the phenomenon is revealed only due to a reduction in Htc, which is nevertheless moderate since autotransfusion of whole blood from the splanchnic reservoir also occurs at the same time.
The tolerance of fluid overloading is just as amazing as the negative effect of blood loss is marvelously “muted.” When there is an inappropriate overloading of crystalloids, a kidney response suddenly enters into play, and when the possibility of a diuretic renal response is overcome, the increased hydrostatic pressure in the capillary along with a reduction in oncotic pressure due to dilution thereof pushes excess fluid into the interstitial space, thus maintaining a normal hemodynamic pattern.
These compensation mechanisms (and we have only described some of them) are initially capable of covering up our carelessness.
We have described only some of the forms of compensation activated by the body in the event of volemic imbalance.
In reality we have described those that can most easily be discovered (decreased Htc, decreased CVP, decreased diuresis, increased heart rate). But there are other more complex mechanisms that require greater acuity and control to demonstrate. I am referring to the renin-angiotensin-aldosterone system (RAAS) and the action of ADH.
At this point it is essential to refer to effective circulating volume (ECV): this is the volume of blood distributed in the arterial system intended for perfusion of the tissues. It is not a measurable parameter and is regulated by baroreceptors in three areas:
-
1.
The carotid sinuses that regulate sympathetic activity and, to a lesser extent, the release of ADH. One of the main functions of this apparatus is the maintenance of cerebral perfusion.
-
2.
The juxtaglomerular apparatus that regulates the activity of the RAAS and therefore glomerular perfusion and glomerular filtration.
-
3.
The atria and ventricles that release natriuretic peptides in response to increases in pressure.
If cardiac output decreases, the regulation systems enter into play to restore it. For example, in a patient with cardiac insufficiency, upon reduction of output the carotid sensors stimulate sympathetic activity, and those of the juxtaglomerular apparatus activate the RAAS. These responses promote an increase in heart rate and sodium retention and therefore an increase in circulating blood volume that causes greater distension of the cardiac chambers and, according to Starling’s law, an increase in cardiac output, which is also promoted by the increased heart rate.
The response of these regulation systems is therefore initially favorable, but, if cardiac insufficiency and the Na-sparing mechanism continue, the blood volume increases later on even if the heart is no longer able to empty the venous return: this leads to blocked circulation, edemas, dyspnea, and pulmonary edemas.
In the case of advanced-phase cardiac sufficiency, the blood volume increases, while the ECV decreases.
It is confirmation of the fact that volemia and ECV are two values that are not necessarily correlated.
We have highlighted the concept of ECV and described the example of chronic cardiac insufficiency to draw attention to the fact that volemic overloading may coexist even if ECV is reduced.
The aim of this article is to attract the attention of anesthetists to apparently normal situations which in reality are the result of compensation mechanisms, but providing advice for better diagnosis and management.
6.1 Fluid Dynamics in the Capillary
6.1.1 The Importance of the Glycocalyx
The mechanism that regulates fluid movement in the capillaries was described by Starling in 1896 and is still largely applicable. Fluids are maintained within the capillaries thanks to oncotic pressure from plasma components. Oncotic pressure counters hydrostatic pressure which pushes fluids into the capillaries and therefore the interstitium. In the interstitium both hydrostatic and oncotic pressure are lower than in the endocapillary plasma. The net result is a constant moderate passage of fluids from capillaries to the interstitium where any excess fluid is immediately removed from the lymph nodes and rechanneled towards the heart. The endothelial barrier is permeable for water and small molecules such as sodium, potassium, chlorine, and glucose, which pass freely via specialized pathways.
The macromolecules can be transported via larger pores or vesicles. The movement of fluid across the capillaries can be distinguished as two types: Type 1 (physiological) occurs continuously and, as mentioned above, is removed from the lymph nodes and Type 2 (pathological) is seen when the barrier is damaged or does not function properly: this results in the formation of edemas.
If it is true that the physiological basis that regulations of fluid movement across the capillaries are still the old Starling’s law, we must, however, include much more recent information that currently provides us with particularly useful data on the perioperative management of fluids.
The new information essentially relates to demonstrating the presence of the glycocalyx system at the endothelial level.
The endothelium is made up of a wafer-thin barrier formed of a single layer of cells (endothelial cells). In the part facing the lumen, the endothelium is covered by a thin, fragile membrane, the glycocalyx, which is the first barrier regulating the transport of macromolecules and cells.
This barrier, which is made up of glycoproteins and proteoglycans and contains glycosaminoglycans, traps red blood cells and protein-rich plasma. We must therefore today consider the intravascular fluid volume as having two distinct parts: that which is noncirculating and is trapped in the glycocalyx system and that which is circulating.
The endothelial wall is therefore made up of endothelial cells and the glycocalyx and is 0.4–1.2 μm in thickness; it is in continuous dynamic balance with the circulating plasma.
To function normally, this barrier requires a normal level of albumin. In hypoalbuminemic states, which are very common in our patients, the barrier does not work properly, and, even with a reduction in oncotic pressure, large quantities of fluid pass from the capillary to the interstitium, and when the lymph nodes are no longer able to empty them, edemas occur.
When we administer iso-oncotic colloids to our patients, we increase capillary hydrostatic pressure, but oncotic pressure remains constant: this situation encourages a more moderate passage of fluids towards the interstitium. When, however, we administer crystalloids, hydrostatic pressure increases, as in the case of colloids, but oncotic pressure falls: this leads to the passage of more fluids from the capillary to the interstitium.
The endothelium and the glycocalyx systems are not only a barrier between intravascular liquids and the interstitium, but play an important role in hemostasis, platelet aggregation, leukocyte adhesion, and permeability of the barrier. In perioperative phases, therefore, it is mandatory to protect the barrier from events that may damage it.
Negative factors are processes of ischemia/reperfusion, hypoxemia/reoxygenation, proinflammatory cytokine, and BNP. In particular we must draw readers’ attention to BNP since it is of great significance in anesthesiological practice.
In the case of fluid overloading, whether iatrogenic (excessive administration) or resulting from pathological states (chronic cardiac insufficiency), distention of the cardiac chambers leads to increased BNP release, which has a harmful effect on the glycocalyx system [1].
Fluid overloading therefore does not only increase the hydrostatic pressure of the capillary but damages the barrier, transforming Type 1 transcapillary fluid movement into Type 2 movement and thus promoting the formation of edemas.
There are few protective factors of the endothelial/glycocalyx complex, but one of these is a widely used anesthetic, sevoflurane, which enables better tolerance of possible fluid overloading [2]. The other two protective factors are hydrocortisone and antithrombin [3].
6.1.2 The Distribution of Crystalloids and Colloids
The use of a glycosylated solution to expand the circulating volume is destined to be unsuccessful. In fact, glucose is rapidly metabolized by the liver, and therefore administering a glycosylated solution is equal to administering free water.
Water passes through all barriers freely and rapidly, and therefore 1,000 ml of an infused glycosylated solution on 7 % (the equivalent of 70 ml) remains in the circulation, adding to the other 4 l of intravascular water. The remaining water is distributed by balancing itself with other compartments where water totals 24 l and/or is eliminated via diuresis.
The use of 1,000 ml of a 0.9 % saline solution remains confined in the extracellular space (interstitium + circulation) since sodium cannot enter the larger intracellular space. Therefore a greater proportion of the solution compared to the glycosylated solution remains in the bloodstream (approx. 20 % or 200 ml out of 1,000 ml, compared with 7 % or 70 ml out of 1,000 ml for the glycosylated solution).
Colloids – hydroxyethylamides, gelatin, or albumin solutions – remain longer in the bloodstream compared with crystalloids since the dimensions of their molecules do not facilitate transcapillary movement.
This passage nevertheless occurs. It has been shown that a colloid administered in normal volemic situations, whether 6 % hydroxyethylamide or a 5 % albumin solution, enters into the interstitia in a few minutes at a rate of 68 %. If, however, these plasma expanders are administered to a hypovolemic patient, leading to normovolemic hemodilution, the amount of fluid remaining in the circulation in this period is roughly 90 % [4].
This observation is important for clinical practice. If we administer a plasma expander to a patient who needs it, and who is hypovolemic, we have greater persistence in the circulation and less passage into the interstitia. If, however, we administer it to a patient who does not require it, it rapidly enters the interstitia: this mechanism protects the circulation from an excessive rise in hydrostatic pressure but also has negative consequences that trigger pruritus and edema.
Recently a comparison has been made between 0.9 % saline, gelatin, and 6 % hydroxyethylamide in healthy young subjects. After 1 h of infusions, 68 %, 21 %, and 16 % of infused liquids, respectively, left the circulation [5].
The difference between the two colloids used was therefore moderate, but their molecular weight varied greatly: 30 KDa for gelatin and 130 KDa for hydroxyethylamide.
In the same study the response of the RAAS was assessed for the three infusions: all reduced it by depriving the response of renin and aldosterone and by promoting the elimination of H2O and Na. This observation confirms that it had already been demonstrated in the past that the elimination of H2O and Na in acute hypervolemia depends essentially on suppression of the RAAS. Even BNP increases iatrogenic hypervolemia, but its diuretic effect in this situation is weaker. As mentioned above, however, the harmful effect of BNP on the glycocalyx is very important.
It is usually thought that the amount of crystalloids to be infused in the case of acute hypovolemia is three to four times that of colloids, which are, however, equal in terms of estimated blood loss.
A systematic review of the issue seems to result in the recommendation of a 2:1 ratio [6].
What is certain is that the administration of colloids enables greater linear recovery of cardiac filling and therefore CO in all patients, whether or not they have sepsis, for saline solutions.
We must not, however, ignore the study recently published in the New England Journal of Medicine which examines the use of hydroxyethylamide in septic patients in whom the use of this drug compared with saline solutions would be greatly burdened by adverse events and mortality [7].
In cases of multiple trauma, however, the use of hydroxyethylamide seems to enable faster clearance of lactate and a lower incidence of renal damage compared with the use of saline solutions [8].
In concluding this short section, it appears possible to say that, in the presence of a perioperative hypovolemic state, it would be preferable to use colloids rather than crystalloids, which would be used exclusively to rebalance the physiological losses (perspiration and diuresis), which are abundantly and rapidly compensated for by fluid movements from extravascular compartments, whether intracellular or extracellular.
6.2 Perioperative Management of Fluids: Comparison of Liberal, Restrictive, and Goal-Directed Strategies
The goal of maintaining good organ perfusion is still too often pursued in operating rooms with high levels of crystalloid administration. This approach is supported by the conviction that surgery patients who have fasted for at least 12 h are often prepared for intestinal surgery with enema and have lost fluids through perspiration and diuresis or as a result of hypovolemia. The belief that during surgery an irrelevant quantity of body fluids escapes towards a “third space,” which has never been determined, is just as widespread.
This so-called third space has been discussed since the 1960s [9] when research with techniques based on the use of a tracer in patients undergoing major abdominal surgery demonstrated that in these patients a loss of water from the extracellular compartment is confirmed even without blood loss.
It is believed that an amount of fluid is discharged into a compartment that is then called a “third space” and that it is identified in the gastrointestinal apparatus and tissues that have been damaged during surgery. Based on this assumption, which is fantastical and minimally supported by research, the liberal use of crystalloids has become the standard, not only to compensate for diuresis and perspiration, but also for the amount of fluids discharged into the “third space” and reduced from the intravascular amount. As a result of this perioperative fluid management strategy, a consistent increase in weight (of up to 10 kg!) in patients in the immediate postoperative period has become very common in recent years.
A systematic review of the studies in which the behavior of perioperative extracellular volume has been controlled has very recently discredited the theory of the “third space” [10], and therefore currently in the perioperative phase, it is justified to compensate with crystalloids only during diuresis and perspiration.
Perspiration, among other things, is considered less important than in the past, and forty years ago it was shown by Lamke et al. [11] that it can amount to 0.5–1 ml/kg/h during major abdominal surgery.
Therefore, during a classical intervention of this kind, such as hemicolectomy in a patient weighing 70 kg (lasting 3 h), fluid loss via perspiration fluctuates between 100 and 200 ml. If diuresis occurs during the same period at a rate of 150 ml/h, it can immediately be understood that in a patient like the one described above, replacement with 500 ml crystalloids is justified. Higher doses can lead to episodes of hypervolemia which, even if transitory, cause the release of BNP, which, as we have seen, damages the glycocalyx system leading to the transcapillary passage of fluids into the interstitia with a resulting increase in weight, as described above.
In becoming aware of this reality, there is naturally a comparison with a different perioperative fluid management strategy that has been labeled “restrictive.” This strategy has been rapidly embraced in thoracic surgery, in which the advantage in terms of oxygenation and the prevention of respiratory complications is immediately clear.
In abdominal surgery, where the advantages are not particularly evident or resounding, the “restrictive” strategy of fluid therapy has not had such an immediate success.
Even in 2003 it was necessary to conduct a multicenter study, published by Brandstrup et al. in Ann. Surg. [12], to draw attention to the risks of liberal fluid management in the perioperative phase. The authors compared two groups of patients who underwent colorectal surgery: one group was treated liberally with crystalloids, receiving on average 5.4 l of fluids, and the other group, which underwent a restrictive strategy, received 2.7 l.
The postoperative complications were much more common in patients treated with high doses of crystalloids (51 % vs. 33 %), including liver infections, failure of intestinal sutures, and cardiovascular and respiratory damage.
The much-feared renal damage, however, as a result of fluid restriction, was not found. It is sufficient to notice that patients undergoing the restrictive strategy received more colloids, as a percentage, and those with the liberal strategy more crystalloids, which confirms the comparison between the two different theories: one (the restrictive) that used crystalloids mainly to compensate for diuresis and perspiration and/or as a vehicle for drugs, and colloids to compensate for blood loss, and one that uses crystalloids much more liberally, even to treat any type of hypotension if confirmed during the perioperative phase.
It should be pointed out that hypotension during anesthesia is mostly due to vasodilation and could be treated by reducing anesthesia and/or using vasoconstrictors, which, among other things, are much more effective in such cases.
The liberal use of crystalloids, as we have seen, is also based on the old concept of underlying hypovolemia in surgery patients as a result of fasting and, in the case of intestinal surgery, of enema preparations. This concept has been discredited. In 2008 Jacob et al. published a study in Acta Anesth. Scand. which demonstrated the absolute normality of the circulating volume in surgical patients after nocturnal fasting [13].
The considerations made up to now point towards a constantly restrictive use of fluids in major surgery. In reality things are not as simple as this. Alongside a study that is favorable to this type of strategy, there are others that do not show differences in outcome between liberal and restrictive strategies.
Among other things, it is not easy to compare the various strategies used by different working groups, since a universally accepted restrictive strategy has not yet been codified.
Colorectal surgical interventions with miniscule administration of fluids (800 ml) have been reported, and others, such as the multicenter study by Brandstrup mentioned above, in which the average fluid administration was 2,700 ml.
We therefore have before us studies that demonstrate that liberal fluid administration can be harmful, but it seems we can confirm that a valid restrictive strategy for all patients cannot currently be defined with certainty.
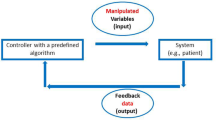
Faced with this uncertainty it is even more beneficial to agree on a personalized perioperative fluid management strategy, the so-called goal-directed fluid therapy (GDT), in order to avoid both hypovolemia leading to organ damage due to hypoperfusion and hypervolemia with cardiac overloading, O2 desaturation, and damage to the glycocalyx system.
GDT has been stressed for more than 20 years, but in order to carry it out in the 1980s, a Swan-Ganz catheter was required, and DO2I was recommended at above-normal doses (600 ml/m2/min) to ensure perfusion of the organs even in critical moments.
This position was barely acceptable for patients at high risk since such invasive monitoring was not fully justified in large numbers of surgical patients.
Due to this difficulty, GDT did not acquire the consensus that it would conceptually have deserved, but the idea reemerged gradually after several years that other less invasive methods were available for cardiovascular monitoring that, above all, enabled monitoring of the stroke volume and the use of “dynamic” parameters such as SPV, PPV, and SVV.
The instruments currently available for the personalized management of fluid therapy in the perioperative phase are numerous and can be divided up into:
-
1.
Instruments that measure stroke volume (and other parameters) by using esophageal echo Doppler or thoracic impedance graphs.
These instruments measure stroke volume directly by assessing aortic flow in various ways. The advantage of esophageal echo Doppler lies in the widespread documentation that exists on the validity of its use intraoperatively. The disadvantage is the inability to use it in awake patients and therefore in preoperative and postoperative phases.
Thoracic impedance graphs have the great advantage of being easy to activate even by the nursing staff by applying two self-adhesive sensors to the skin of the neck and throat.
This monitoring technique is therefore not at all invasive and can monitor stroke volume without calibration in addition to other useful parameters in the evaluation of circulatory filling and the contractility of the left ventricle such as the preejection period (PEP), peak aortic flow, and flow acceleration. It is the only monitoring system that is not at all invasive that provides information on extravascular lung water (EVLW). The disadvantage is the low level of experience in intraoperative monitoring, while there is generally a good consensus regarding its reliability and sensitivity in measuring stroke volume in other situations
-
2.
Instruments that monitor stroke volume and other useful parameters with invasive methods. One of these is the widely known system based on transpulmonary thermodilution (PiCCO), which requires a catheter with sensors in the superior vena cava and another in the femoral or axillary artery.
This monitoring system, after directly measuring cardiac output with the transpulmonary thermodilution method, uses the stroke volume obtained as a calibration factor for continual monitoring of the same parameter with the pulse profile analysis method. PiCCO is also able to provide information on the contractility of the left ventricle and EVLW. Since it requires sensors in the central veins and arteries, it cannot be considered a noninvasive monitoring method but can nevertheless be used in preoperative and postoperative phases other than in intensive therapy in conscious patients.
Another minimally invasive system is based on lithium dilution (LiDCO): after measuring cardiac output method cited above, it uses this value as calibration to carry out continuous monitoring of stroke volume by analyzing the pulse profile.
As with PiCCO, the cost of the sensors makes this a monitoring method for selected patients. Both methods, along with the continuous assessment of stroke volume, enable the monitoring of dynamic parameters such as SPV, PPV, and SVV. LiDCO can also be used in all perioperative phases.
The FloTrac/Vigileo system also calculates stroke volume using the pulse profile method but unlike the other systems does not require preliminary calibration, thanks to an IT program activated by inputting biometric data.
All the monitoring systems described above are so far able to monitor the so-called dynamic parameters (SPV, PPV, SVV), except for thoracic impedance graphs, which, since they do not need an arterial catheter, cannot monitor SPV and PPV but nevertheless monitor SVV, which has a similar meaning.
All the monitoring methods described above make it possible to use GDT through an early understanding above all of hypovolemic states which have not yet given clear signals of their presence and through the observation of the correction of these states.
It should be pointed out that in young, healthy patients with all compensation mechanisms intact, up to 25 % of circulating volume can be lost before a drop in pressure and/or an increase in heart rate is observed [14]. It is true, as we have already said, that less obvious signals such as a fall in CVP, a contraction of hourly diuresis, and a fall in Htc may occur, but there is no doubt that the monitoring systems listed above are an important and easy-to-read tool in understanding these imbalances early and monitoring their correction.
Useful information on the utility or otherwise of mass administration comes from performing the so-called fluid challenge. If the patient’s hemodynamic characteristics can be placed on the steep ascending part of Starling’s curve, a volume bolus (e.g., 200 cc of a colloid infused in 5 min) causes an increase in stroke volume of at least 15 %. A response of this type favors the administration of fluids. If, however, the hemodynamic status is placed on the horizontal part of the curve, a mass bolus will not lead to a significant increase in stroke volume. A response of this type discourages the subsequent administration of fluids.
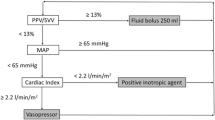
The information provided by the “dynamic parameters” is even more immediate: SPV, PPV, or SVV higher than 15 % is indicative of hypovolemia, and a response that tends to lead to normalization after a fluid bolus is indicative of the utility of fluid administration. The most tested hemodynamic parameter in recent years is PPV [15, 16].
The studies relating to this suggest that to implement GDT in the perioperative period using PPV, it must be between 10 and 15 % with the infusion of fluids if it exceeds 15 % for the purpose of reporting the value within the recommended range.
A recent study, however, in 413 patients under general anesthesia and artificial ventilation for various types of surgery at four different study centers [17], has demonstrated a gray zone for PPV between 9 and 13 %, in which it was not possible to predict whether a patient would be a responder or a nonresponder upon administration of fluids. The identification of the gray zone makes it possible to determine with certainty the nonresponders who do not respond favorably to fluid administration (PPV <9 %) and the responders who will almost certainly benefit from the administration of mass infusion (PPV >13 %). Average values are not very indicative in predicting the utility or otherwise of infusions. In this study the responders and nonresponders were identified with a 500 ml fluid challenge and by observing the percentage response of the cardiac index measured with Swan-Ganz catheters or otherwise with transpulmonary thermodilution or esophageal echo Doppler. Patients who responded to the fluid bolus with an increase in the CI of 15 % or more were considered responders.
A monitoring system that is not at all invasive which has recently drawn a consensus in particular for its ease of use is based on continuous control of the variability of the plethysmographic wave and Hb obtained using simple plethysmographic skin sensors.
The controlled parameters are the plethysmographic variability index (PVI) and SpHb. PVI has a similar meaning to the dynamic parameters listed above, and SpHb enables constant information on total hemoglobin and is very useful in monitoring hidden bleeding.
A very recent meta-analysis published in Anesthesia [18] looked at 10 studies in which PVI was used to monitor fluid infusions. If patients were under artificial ventilation and the fluid challenge was performed with colloids, PVI was a very useful parameter to monitor infusions. There are currently no convincing comparisons with other monitoring systems that measure dynamic parameters (SPV, PPV, SVV), but the method is promising and has the great advantage of not even requiring catheterization of a peripheral artery. The cost of the instrument that enables this type of monitoring is not particularly high. The PVI value at which it can reasonably be thought that the patient is hypovolemic and at which a fluid challenge and possible subsequent mass infusion is justified varies from author to author, but it can be considered that variability greater than 15 % is indicative of a hypovolemic state.
PVI has also been used to monitor fluid therapy in patients with spontaneous respiration: in this case, however, the cutoff point is much higher and is determined as 19 % by Keller [19]. The dedicated instrument also provides the continuous value of pulse symmetry, heart rate, and, as mentioned, total hemoglobin, and it can be thought that at least in high-risk patients, it can be substituted with simple pulse symmetry with the advantage of providing much more comprehensive data.
It can be said that this instrument, along with the recent mobile version of thoracic impedance graphs, can be considered extremely useful and not at all invasive in the management of fluids in the perioperative period.
6.3 The Specific Case of Fluid Therapy in Day Surgery in a Low-Risk Patient
In this type of patient, a liberal strategy of fluid administration seems much more acceptable.
In fact, in day surgery it is essential to reduce postoperative disorders such as nausea, vomiting, and postural hypotension.
These objectives are achieved with the administration of 20–30 ml/kg of crystalloids [20, 21].
In the case of laparoscopic surgery, even higher infusions (40 ml/kg) are required to achieve the results mentioned above [22].
6.4 How to Manage an Asymptomatic Patient with Chronic Anemia Perioperatively?
For over 40 years the hemostatic characteristics of patients with chronic anemia have been well known. Even today the description made by Duke and Abelman in Circulation in 1969 still applies [23].
Patients with chronic anemia have high cardiac output, enhanced left ventricular contractility, tachycardia, low peripheral vascular resistance, and reduced circulating volume.
Thanks to the high cardiac output and increase in tissue extraction of O2, tissue oxygenation is substantially ensured even in the presence of significant anemia. Hemodynamic changes depend on the extent of anemia and become particularly relevant when Hb falls below 7 g/dl.
With this kind of hemodynamic picture, it can easily be understood that patients with chronic anemia are weak. Anesthetists, by depriving the heart of its contractile force, reduce cardiac output and thus DO2 by jeopardizing tissue oxygenation. Hypotensive events are, moreover, more common and subsequently complicate oxygenation. It is therefore vital not to subsequently reduce the circulating mass in these patients and to avoid as far as possible cardiodepressant anesthetics, remembering that tachycardia is a compensation mechanism.
Precisely because tachycardia is a compensation mechanism, it is inadvisable to use beta-blockers. Furthermore, since hypovolemia is compensated for by stimulation of the RAAS, ACE inhibitors and sartanes (which are not very widespread in general anesthesia in all patients) are contraindicated.
If GDT is a useful strategy in all patients at risk, this is particularly true of those with chronic anemia, but, as currently understood, the approach to this type of patient who must undergo surgical intervention is all in the preparation.
The preparation for interventions in patients with chronic anemia rests upon two main points: diagnosis of the type of anemia and correction of it.
To accomplish these two objectives, a large amount of time is required. When the anesthetist is faced with a patient with chronic anemia, who is apparently asymptomatic and has not yet received a precise diagnosis of the cause of anemia, elective surgery must be postponed for 1–2 months. To respond to diagnostic questions, the easiest, but often the longest, way is to refer the patient to a hematologist, asking him/her to correct the anemia. However, apart from very specific situations, the most common causes of asymptomatic chronic anemia are not numerous and can easily be identified and corrected. In young women the most common cause of anemia is iron deficiency linked to menstrual discharge. More complex is sideropenic anemia in men and especially in elderly persons. In these cases, the first question to be asked is whether the patient is losing blood: hemorrhoids, gastric or colonic neoplasia, and hiatus hernia are the most common causes of iron deficiency and are corrected prior to considering planned elective surgery before it is necessary.
Let us imagine a 70-year-old male patient with moderate anemia (Hb 11 g/dl), low iron and ferritin levels, and low MCV of red blood cells, who must undergo a hip replacement. Reports show the presence of an asymptomatic colon tumor. It is clear that hemicolectomy will take precedence over the hip replacement. But, if we have underestimated the moderate anemia, how will we go about things?
In the case of anemia without obvious iron deficiency, attention should be drawn to the low levels of folic acid and B12, especially if MCV of red blood cells is higher than 100.
MCV, which is always available, is a determining factor: values higher than 100 require control of plasma levels of B12 and folate; MCV values below 80, on the other hand, require a focus on iron deficiency [24].
In patients with a documented deficiency in iron, it is essential to prescribe oral treatment for at least 1 month, which will be decided when Hb is <13 g/dl for women and <14 g/dl for men, along with MCV <80, ferritin <12 mg/dl, or transferrin saturation <15 % [25].
Since oral therapy is often poorly tolerated and the cause of treatment interrupted, it can be useful to remember that a better tolerated medicine is nowadays available in Italy (iron bisglycinate chelate), which therefore results in better patient compliance with the therapeutic plan.
The recommended dose of this medicine is 2 tablets per day (28 mg) for 1 month, possibly continuing with 1 tablet per day if longer periods are available.
It has been shown that at this dosage iron bisglycinate chelate has the same efficacy as ferrous sulfate, which is usually used, but with drastically higher gastric tolerability [26].
In the event of MCV >100 and plasma B12 levels below the limits of normal (200–900 pg/ml), it will obviously be necessary to supplement this vitamin.
If MCV is normal, a control of reticulocytes and creatinine will be useful to determine possible hemolysis or a nephrological cause of anemia. In this type of situation, a consultation with a hematologist or nephrologist is important.
A few more words may be said about anemia from chronic disease that is an exclusion diagnosis and is suspected if iron and B12 deficiency have been ruled out, if renal function is normal, if hemolysis is not suspected, and if chronic disease is present (such as COPD or rheumatoid arthritis).
In such cases the use of erythropoietin (beta epoetin and similar) is justified, since it is supported by simultaneous oral administration of iron [24].
In concluding this brief chapter on perioperative anemia, it should be specified that, following a diagnosis of anemia without identified causes in a patient who has been proposed for elective surgery, especially if the intervention might involve consistent blood loss, must consider postponing the intervention. Anemia should be seen as a significant pathological condition and not simply as a moderate change in laboratory data. Let us remember the title of the work of an expert in the field, Lawrence T. Goodenough, published 10 years ago in Arch. Int. Med.: “Anemia: not just an innocent bystander?”.
6.5 Perioperative Colloids: Angels or Demons?
There is no doubt that colloids, whether proteic (albumin) or nonproteic (hydroxyethylamide, gelatin, dextran), have a capacity for plasma expansion that is more effective and longer lasting for crystalloids. Since the most common determining factor for perioperative hemodynamic imbalance is hypovolemia, it should be deduced that colloids are the better adapted fluids to treat this complication. This is because, as we have said many times in this article, crystalloids should be used to compensate for losses due to perspiration and diuresis, while blood losses and resulting hypovolemia should be treated with colloids until the transfusion of blood and blood derivatives is no longer useful. Since, however, for many years a restrictive strategy in the use of blood has been increasingly adopted (the critical limit for Hb below which is currently justified is set by most authors as 7–8 g/dl), it is clear that the place of colloids in the perioperative phase is highly important.
But which colloids? To delve further into the topic, let us return to the excellent editorial published by Niem et al. in the Journal of Anesthesia in 2010, which concluded that “… rapidly degradable hydroxyethylamides (hydroxyethylamide 130/0.4) have an excellent hemodynamic effect, and the risk of renal damage and hemostatic imbalance, as well as allergic reactions, is minimal” [27].
Older studies too demonstrate the beneficial effect on inflammatory responses [28], postoperative nausea, and vomiting [29] and more generally on the outcomes of surgical patients [12].
Currently hydroxyethylamide 130/0.4 therefore seems to be the best colloids to recommend in the treatment of perioperative hypovolemia.
We must not, however, confuse this indication with the use of colloids in patients with septic shock.
According to Perner et al., who have recently published what is perhaps the most important study in this field in the NEJM, colloids should not be prescribed to patients with septic shock [30].
The study caused a sensation throughout the world, but also quickly established the erroneous conviction that hydroxyethylamide 130/0.4 is dangerous for all patients. This statement is nowadays untenable. Among other things, a number of authors in the same journal have sent letters to the editor in which they criticize the work of Perner. The criticisms come from prestigious centers such as the University of Berlin, the University of Munich in Bavaria, and the University of Cape Town [31]. These criticisms refer in particular to the fact that in Perner’s study colloids were used without a hemodynamic guide, and thus with the risk of plasma hyperexpansion, especially in patients in whom hemodynamic stability had already been achieved.
The hemodynamic status in Perner’s study was controlled only with CVP, which alone is certainly an unsafe parameter in the evaluation of circulatory filling. This may have contributed to colloid overloading compared to real needs, with the negative effects we have referred to repeatedly above.
Less recent information about forms of hydroxyethylamide that are now more commonly used may also have played a role in creating a certain amount of skepticism in hydroxyethylamide comparisons.
Not all forms of hydroxyethylamide are equal. There are three different types: the first is the concentration of the solution (e.g., 6 %) and the second and third are the molecular weight and molar substitution (e.g., 130/0.4).
Molar substitution (0.7, 0.6, 0.5, 0.4) gives its name to the hydroxyethylamide, hetastarch, hexastarch, pentastarch, and tetrastarch. The higher the molar substitution (e.g., 0.7) and molecular weight (e.g., 670 Kdaltons), the more the drug remains in the body, which is essentially the reason for complications reported in the past, predominantly renal damage. Even the concentration is important: 6 % solutions are iso-oncotic, and therefore with 6 % hydroxyethylamide a liter of blood is replaced by a liter of hydroxyethylamide; 10 % solutions are hyperoncotic, and the mass expansion is therefore considerably greater than the infused volume (145 %) [32].
Today the form of hydroxyethylamide most used is 6 % 130/0.4, an iso-oncotic plasma expander, with a low molecular weight and low molar substitution: these are all qualities that guarantee safety if plasma expansion is guided by the patient’s real needs.
To be thorough, we must also refer to the C2/C6 ratio. The hydroxyethylation of glucose subunits that make up the hydroxyethylamide molecular occurs mainly at the C2 and C6 levels. The hydroxyethylation of C2 inhibits amylase access to the substrate in a much more marked way than the hydroxyethylation of C6. Types of hydroxyethylamide with a high C2/C6 ratio are much more difficult for amylase to attack and therefore are harder to break down. Since we do not need the hydroxyethylamide we use to lead to rapid plasma expansion with low persistence in the body, it is obvious that hydroxyethylamides with a low C2/C6 ratio are preferable.
In concluding this chapter we must say that the latest generation of hydroxyethylamides (6 % 130/0.4) are, according to current knowledge, efficient and sufficiently safe plasma expanders that can be used in perioperative phases. In particular, compared with gelatin [33] and 5 % albumin [34], 6 % hydroxyethylamide 130/0.4 has not demonstrated a higher rate or extent of renal damage.
But even in various types of critical patient, including cases of severe sepsis, 6 % hydroxyethylamide 130/0.4 was not an independent risk factor in a study that appeared in the Brit. J. Anaesth. involving 3,147 patients [35]. Even if there were “only” 822 patients in this study with severe sepsis and they were therefore much less represented compared with Perner’s study in the NEJM in 2012, we cannot ignore it.
A few words should be said about the solutions used as vehicles for hydroxyethylamide. There are basically two that are commercially available: 0.9 % polysaline and a balanced solution that is much more similar to the biochemical composition of plasma. When large amounts of hydroxyethylamide are used, the second option is certainly preferable. With the first, in fact, the risk of hyperchloremic acidosis is real, but it is much less common since most authors use it after saline infusions of at least 3 l [32] and its clinical relevance does not appear to be reduced.
Studies in this field are not unequivocal in the information they provide. Alongside those that confirm that hyperchloremic acidosis is a benign disease that disappears on its own [36–38], there are others that maintain that it is the basis of renal and splanchnic fluid reductions [39] and interference in the passage of electrolytes via membranes [40].
Measurements have been made comparing the effects on coagulation with two types of hydroxyethylamide, one derived from potato plants in a balanced solution and one from maize in a saline solution. The authors of this study concluded that 6 % hydroxyethylamide 130/0.4 derived from potato plants in a balanced solution has less of a negative effect on hemostasis even in the presence of Ringer’s acetate alone [41].
This appears to confirm the premise of this chapter that nonproteic iso-oncotic colloids, if used correctly, behave “as angels rather than demons” in perioperative phases.
As regards the most commonly used proteic colloid (albumin), it appears that its use in perioperative phases is not justified as a plasma expander, since this role is usefully taken on by 6 % hydroxyethylamide 130/0.4.
6.6 Conclusions
Perioperative hemodynamic optimization can be achieved by following the precise rules, even if they vary from one patient to the next, by consciously responding to three questions: When to infuse? How much to infuse? How to infuse?
We answered the first and second questions by recalling the importance of early identification of clinical signs of hypovolemia, which is the most common imbalance in the operating room, and the use of instruments that are easily obtainable today for selected patients, which make it possible not only to recognize hypovolemic states early, but also to correct them accurately. Goal-directed fluid therapy is a strategy that is easy to perform today in operating rooms and is certainly able to improve the outcomes of at-risk patients.
Not using it is increasingly considered a guilty omission. The alibi we have used for years that GDT was possible only with a diagnostic means, the Swan-Ganz catheter, which by itself could constitute an additional risk in nonexpert hands, is no longer tenable. We have monitoring instruments that are increasingly easy to use and less costly, and only a lack of desire and culture is at the heart of their inadequate use.
To the third question (What to infuse?) we have clearly replied that mass filling is undertaken with nonproteic colloids, primarily hydroxyethylamide 130/0.4 when the use of blood is not justified; today blood is used much more restrictively.
Crystalloids are reserved for the filling of fluids lost with perspiration and diuresis, which are nevertheless moderate during operations.
Described in such brief terms, these concepts seem very simple, but to put them into practice, it is necessary to have a deep understanding of everything that has been stated above, including every single detail.
References
Bruegger D, Schwartz L, Chappell D et al (2011) Release of atrial natriuretic peptide precedes shedding of the endothelial glycocalyx equally in patients undergoing on- and off-pump coronary artery bypass. Basic Res Cardiol 106:1111–1121
Chappel D, Heindl B, Jacob M et al (2011) Sevoflurane reduced leukocyte and platelet adhesion after ischemia-reperfusion by protecting the endothelial glycocalyx. Anesthesiology 115:483–491
Chappel dD, Jacob M, Hoffmann-Kiefer K et al (2007) Hydrocortisone preserves the vascular barrier by protecting the endothelial glycocalyx. Anesthesiology 107:776–784
Lobo DN, Macafee DA, Allison SP (2006) How perioperative fluid balance influences postoperative outcomes. Best Prac Res Clin Anaesthesiol 20:439–455
Lobo DN, Stanga Z, Aloyrius MM et al (2010) Effect of volume loading with 1 liter intravenous infusions of 0,9% saline, 4% succinylated gelatin and 6% HES on blood volume and endocrine responses. Crit Care Med 38:464–470
Hartog CS, Kohl M, Reihart K (2011) A systematic review of third generation HES 130/0,4 in resuscitation: safety not adequately addressed. Anesth Analg 112:635–645
Myburgh JA, Finfer S, Bellomo R et al (2012) HES or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911
James MF, Michell WL, Joubert IA et al (2011) Resuscitation with HES improves renal function and lactate clearance in penetrating trauma in a randomized controlled study: the FIRST trial. Br J Anaesth 107:693–702
Shires T, Williams J, Brown F (1961) Acute change in extracellular fluids associated with major surgical procedures. Ann Surg 154:803–810
Brandstrup B, Svensen C, Engquist A (2006) Hemorrhage and operation cause a contraction of extracellular space needing replacement-evidence and implication? Syst Rev Surg 139:419–432
Lamke LO, Nilsson GE, Reithner KL (1977) Water loss by evaporation from the abdominal cavity during surgery. Acta Chir Scand 143:279–284
Brandstrup B, Tonnesen H, Beier-Hegersen R et al (2003) Danish Study Group on perioperative fluid therapy. Effect of intravenous fluid restriction in postoperative complications: comparison of two perioperative fluid regimes: a randomized assessor-blinded multicenter trial. Ann Surg 238:641–648
Jacob M, Chappel D, Conzen P et al (2008) Blood volume is normal after preoperative overnight fasting. Acta Anaesthesiol Scand 52:522–529
Doherty M, Buggy J (2012) Intraoperative fluids: how much is too much? Br J Anaesth 109:69–79
Bens J, Chytra I, Altman P et al (2010) Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care 14:R118
Mayer J, Boldt J, Mengistu AM et al (2010) Goal directed intraoperative therapy based on autocalibrated arterial pressure wave form analysis reduces hospital stay in high-risk surgical patients: a controlled randomized trial. Crit Care 14:R18
Cannesson M, Uannick LM, Christopher K et al (2010) Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a gray zone approach. Anesthesiology 115:231–241
Yn JY, Ho KM (2012) Use of plethysmographic variability index derived from the Massimo pulse oximeter to predict fluid or preload responsiveness: a systematic review and meta-analysis. Anaeshtesia 67:777–783
Keller G, Cassar E, Desebbe O et al (2008) Ability of pleth variability index to detect hemodynamic changes induced by passive leg raising in spontaneously breathing volunteers. Crit Care 12:R37
Maharaj CH, Kallam SR, Malik A et al (2005) Preoperative intravenous fluid therapy decreases postoperative nausea and pain in high risk patients. Anesth Analg 100:675–682
Lambert KG, Wakim JH, Lambert NE (2009) Preoperative fluid bolus and reduction of postoperative nausea and vomiting in patients undergoing laparoscopic gynecologic surgery. AANA J 77:110–114
Holte K, Klarskov B, Christensen DS et al (2004) Liberal vs restrictive fluid administration to improve recovery after laparoscopic cholecystectomy: a randomized, double-blind study. Ann Surg 240:892–899
Duke R, Abelmann WH (1969) The hemodynamic response to chronic anemia. Circulation 39:503–515
Lawrence T, Goodnough T, Shader A et al (2005) Detection, evaluation and management of anemia in the elective surgical patients. Anasth Analg 101:1858–1861
Beris P, Munoz M, Garcia-Erce JA et al (2008) Perioperative anaemic management: consensus statement on the role of intravenous iron. Br J Anaesth 100:590–604
Ferrari R, Nicolini P, Mancia M et al (2012) Treatment of mils non chemotherapy-induced iron deficiency anemia in cancer patients: comparison between oral ferrous bisglycinate chelate and ferrous sulfate. Biomed Pharmacother 66(6):414–418, Elsevier, Masson
Niemi TT, Miyashita R, Yamakage M (2010) Colloid solutions: a clinical update. J Anesth 24:913–925
Boldt J, Schölorn T, Mayer J et al (2006) The value of an albumin based intravascular volume replacement strategy in elderly patients undergoing major abdominal surgery. Anesth Analg 103:191–199
Moretti EW, Robertson KM, El-Moalem H et al (2003) Intraoperative colloid administration reduces postoperative nausea and vomiting and improves postoperative outcomes compared with crystalloid administration. Anasth Analg 96:611–617
Perner A, Haase N, Guttormsem AB et al (2012) HES 130/0,4 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Magder S Protocols, physiology and trials of HES. Letters to Editor (2012) N Engl J Med. 367:1265–1267
Westphal M, James M, Korek S (2009) Hydroxyethyl starches. Anesthesiology 111:187–202
Boldt J, Brosch C, Röhm K et al (2008) Comparison of the effects of gelatin and a modern HES solution on renal function and inflammatory response in elderly cardiac surgery patients. Br J Anaesth 100:457–464
Boldt J, Brosch C, Röhm K et al (2008) Is albumin administration in hypoalbuminemic elderly cardiac surgery patients of benefit with regard to inflammation, endothelial activation, and long-term kidney function? Anesth Analg 107:1496–1503
Sakr Y, Payen D, Reinhart K et al (2007) Effects of HES administration on renal function in critically ill patients. Br J Anaesth 98:216–224
McFarlane C, Lee A (1994) A comparison of Plasmalyte 148 and 0,9% saline for intraoperative fluid replacement. Anesthesia 49:779–781
Scheingraber S, Rehm M, Schisch C et al (1999) Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology 90:1265–1270
Mathes DD, Morell RC, Rohr MS (1997) Dilutional acidosis: is it a real clinical entity? Anesthesiology 86:501–503
Williams EL, Hildebrand KL, Mc Cormick SA et al (1999) The effects of intravenous lactate Ringer’s Solution vs. 0,9 sodium chloride solution on serum osmolality in human volunteers. Anesth Analg 88:999–1003
Prough DS, White RT (2000) Acidosis associated with perioperative saline administration: dilution or delusion? Anesthesiology 93:1167–1169
Boldt J, Wolf M, Mengistu A (2007) A new plasma-adapted HES preparation: in vitro coagulation studies using thromboelastography and whole blood aggregometry. Anesth Analg 104:425–430
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Allaria, B. (2015). Hemodynamic Optimization in the Perioperative Period: General Guidelines and a Comparison of Personalized Strategies. In: Chiumello, D. (eds) Practical Issues Updates in Anesthesia and Intensive Care. Springer, Cham. https://doi.org/10.1007/978-3-319-18066-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-18066-3_6
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18065-6
Online ISBN: 978-3-319-18066-3
eBook Packages: MedicineMedicine (R0)