Abstract
Mitochondrial disorders are among the most common inborn errors of metabolism. Based on genetic etiology, they can be divided into several subgroups, which require different approaches for reproductive counseling, addressing differences in recurrence risks and reproductive options. The majority are caused by mutations in nuclear genes, which are currently being rapidly resolved by whole-exome sequencing (WES) and which segregate in a Mendelian way. Prenatal diagnosis (PND) or preimplantation genetic diagnosis (PGD) is available for these families to prevent the birth of another severely affected child. In at least 15 % of cases, mitochondrial diseases are caused by mitochondrial DNA (mtDNA) mutations. Such mtDNA mutations can (1) be the result of a nuclear gene defect (multiple mtDNA deletions), (2) occur de novo (point mutations or large single mtDNA rearrangements), or (3) be maternally inherited (generally point mutations). For the maternally inherited heteroplasmic mtDNA mutations, the mitochondrial bottleneck is an important phenomenon defining the mtDNA mutation load in the offspring, with an often high (or unpredictable) recurrence risk and consequently complex counseling. PND to enable testing for mtDNA mutations is technically possible, but for many carriers of mtDNA point mutations, this approach is not applicable given the limitations in predicting phenotype. A total of 44 cases of PND performed in 35 mtDNA mutation carriers (m.3243A>G, m.9176T>C, m.8993T>G/C, m.8344A>G, m.13513G>A, m.11777C>A, m.10191T>C, m.10158T>C, m.3688G>A) have been described in literature. One additional unpublished case is presented here (m.3303C>T). For mtDNA point mutations which are most likely de novo in the affected child, the recurrence risk has been shown to be very low, and PND can be offered for reassurance. We have performed PND in four such cases, and six additional prenatal diagnoses were reported in literature. PND is also the most suitable option for female carriers with a low mutation load, demonstrating extreme skew such as mutations at nucleotide 8993. A fairly new option for preventing the transmission of mtDNA diseases is preimplantation genetic diagnosis (PGD). Embryos with mutant load below a mutation-specific or, if not possible, general expression threshold are transferred. A systematic review showed ≥95 % probability of being unaffected at (muscle) mutant level of 18 % or less, irrespective of the mutation. A total of 14 PGD cycles in six female carriers of heteroplasmic mtDNA mutations (m.3243A>G, m.8993T>G, m.8344A>G) have been completed at our center to date. All carriers produced oocytes below the threshold, and blastomere mutation load was representative for the whole embryo when two blastomeres were analyzed. A total of 12 PGD cycles in nine mtDNA mutation carriers (m.3243A>G, m.8993T>G) have been reported elsewhere. A total of six children were born after PGD and one pregnancy is ongoing. So, PGD is currently the best reproductive option for most maternally transmitted heteroplasmic mtDNA point mutations. Oocyte donation is a safe option to prevent the transmission of mtDNA disease to a future child for couples who reject PGD. Nuclear genome transfer techniques are currently investigated in research settings and might offer additional reproductive options in specific cases of mtDNA disease in the future.
Authors’ Contributions: SCEHS collected and analyzed the data, studied the literature, and developed the chapter; JCFMD provided the data and helped with study design; IFMdC was the lead clinician and referred patients for PND/PGD; CEMdD-S and HJMS supervised the writing and review of the chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Mitochondrial disease
- mtDNA
- Reproductive counseling
- Recurrence risk
- Reproductive options
- Prenatal diagnosis (PND)
- Preimplantation genetic diagnosis (PGD)
Introduction
Mitochondrial diseases are perhaps the most common of all inborn errors of metabolism [1]. They are highly variable in phenotype, ranging from severe and lethal infant/childhood manifestations to relatively mild symptoms with onset at adult age. Generally, no treatment is available. The (recurrence) risk is dependent on the nature of the underlying primary genetic defect, and so are the available reproductive options. The primary genetic defect can be located either in nuclear or mitochondrial DNA, and this feature will have direct consequences for the recurrence risk. In case of a nuclear gene defect, the disease segregates in autosomal dominant or recessive fashion with recurrence risks of 50 % or 25 %, respectively. De novo nuclear mutations with a lower recurrence risk are rare. For mtDNA defects, the recurrence risk in the family is much more difficult to predict. Age- or drug-induced mtDNA defects (i.e., multiple deletions and mtDNA depletion) occur somatically with no transmission risk at all. However, multiple mtDNA deletions and mtDNA depletion can also be secondary to a primary defect in nuclear genes involved in mtDNA maintenance. In such a case, the recurrence risk is comparable to other nuclear gene mutations. At least 15 % of mitochondrial diseases result from primary mitochondrial DNA (mtDNA) mutations [1, 2] including point mutations and large rearrangements. The recurrence risk of these mtDNA defects can vary between high/unpredictable and very low (in fact even zero for actual de novo mutations) depending on the nature of the underlying defect.
Two characteristics of mtDNA mutations which are key to understanding the complexity of mtDNA disease transmission include mitochondrial heteroplasmy and the genetic bottleneck. The majority of pathogenic mtDNA mutations resulting in severe disease are heteroplasmic, which means a mixture of mutant and wild-type mitochondria within a cell/tissue/individual. Heteroplasmy levels can vary between and within tissues of a carrier. Heteroplasmic mtDNA mutations are characterized by a threshold effect, meaning that there are no symptoms unless the mutant load (proportion of mutant mtDNA) exceeds a certain level. This threshold varies both within tissues and between different mutations and can depend on environmental factors, like the physical condition of the carrier.
Transmission of mtDNA occurs only from females to their offspring and is subject to a so-called genetic bottleneck. During oogenesis, the number of mtDNA molecules to be transmitted is reduced, and the resulting few mtDNAs become the founders for the offspring. In case the transmitting woman carries a heteroplasmic mtDNA mutation, this results in considerable variation in mtDNA mutant load among her individual oocytes [3] and subsequently among offspring. The exact mechanism of the mitochondrial bottleneck is incompletely known, and some controversy exists concerning the content and “size” of the segregational unit [4–9]. This size has been hypothesized to depend on the type of mtDNA mutation [10–13] and to be individual dependent for certain mutations [10], possibly due to individual differences in initial mitochondrial copy number or genetic background. Another important question is whether the bottleneck really is mutation-specific or that only the degree of skewing is mutation-specific, resulting in apparent differences in bottleneck size. Irrespective of the mechanism, the smaller the lowest amount of the remaining mtDNA (segregational unit), the more rapid a (complete) shift of the mtDNA genotype can occur.
Primary Nuclear Defects
Counseling and Recurrence Risk
About 85 % of mitochondrial diseases is caused by mutations in nuclear genes, which are currently being rapidly resolved by whole-exome sequencing (WES) and which segregate in a Mendelian way with recurrence risks of 25 % or 50 %. In general, they do not affect the mtDNA, although part of the mtDNA defects, like multiple mtDNA deletions or mtDNA depletion, can be due to defects in nuclear genes involved in mtDNA maintenance. Comparable mtDNA defects can also occur somatically due to a nongenetic cause like aging (e.g., multiple mtDNA deletions) or mitotoxic drugs (e.g., nucleoside reverse transcriptase inhibitors can induce mtDNA depletion) with no recurrence risk at all; it is essential to define the cause of these mtDNA defects for proper estimation of the recurrence risk. De novo nuclear mutations with a low recurrence risk are rare.
Reproductive Testing Options
Nuclear gene defects resulting in mitochondrial disease are less complex with regard to reproductive options than primary mtDNA defects. Prenatal diagnosis (PND) and preimplantation genetic diagnosis (PGD) can reliably be offered, provided that the mutation is identified. The latter is the main problem in this category of mitochondrial diseases. Up to now, only in a minority of mitochondrial patients where mtDNA defects have been excluded, the genetic defect has been identified. New sequencing techniques (next-generation sequencing) and unbiased approaches (whole-exome sequencing) are promising in increasing this number, resulting in reproductive options for more at risk couples. In cases where the genetic defect is not known but the mtDNA has been excluded and an enzyme deficiency is detectable in fibroblasts, PND based on biochemical analysis might be an option [14–17]. However, there are some limitations and pitfalls including sensitivity issues, the absence of the enzymatic defect in fibroblasts in 50 % of patients, and limited knowledge on complex assembly and activity during embryonic development [18].
In patient populations where consanguinity is more common, one should be aware that an increased risk of more than one genetic condition may be present. Thus, when offering reproductive options for a mitochondrial defect, there is still a realistic risk that the resulting child is affected by one or more other genetic abnormalities. Currently, consanguineous couples are empirically counseled regarding genetic risks if no genetic diseases have occurred in their families. In specific ethnic groups, carrier screening is offered for genetic diseases that are frequent in those populations. With the upcoming DNA sequencing techniques, preconception screening will become available on a broader basis.
Familial Primary mtDNA Mutations
Counseling and Recurrence Risk
The most common heteroplasmic mtDNA point mutation is the m.3243A>G mutation in the mitochondrial MT-TL1 gene, causing MELAS syndrome (mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes), among others. This disorder is characterized by highly variable age at onset, symptom severity, and organ involvement. Correlation between the level of mutant mtDNA in blood and clinical features is poor due to the decrease in mutation load in blood cells with time [19–21]. However, mutation levels in muscle [22] and urine [23–26] seem to be of higher prognostic value. Mutant load in oocytes and embryos of m.3243A>G carriers shows large variation [10, 27] approximating a Gaussian distribution [27], indicating that the level of mutant mtDNA in oocytes and embryos for this mutation is largely determined by random genetic drift [10, 13, 27]. Existing data also point out that although in general a higher mutant load in the mother provides a higher risk of affected offspring, the recurrence risk for an individual m.3243A>G carrier remains very difficult to predict [27, 28].
mtDNA Point Mutations Demonstrating Skewing
Specific mtDNA mutations such as the nt8993 mutations do not show random transmission as with the m.3243A>G mutation, but rather demonstrate skewing. Due to the skewing to the extremes, there is an overrepresentation of oocytes and subsequent embryos with 0 % and 100 % mutation load [12, 27, 29–31]. Accordingly, with these mutations, it is possible for a mother with a high mutant load to have a child with a low mutant load and vice versa [29]. In general, the individual recurrence risk can be better characterized as low (the majority of oocytes not showing the mutation) when the mother’s mutant load is low. The proportion of children with a high mutant load increases as the mother’s mutant load increases. Other characteristics of the nt8993 mutations are the rather good correlation between mutation load and phenotype [29] and a quite uniform distribution of the mutation in all tissues [32].
Reproductive Testing Options
Prenatal Diagnosis
In general, PND for mtDNA mutations has several limitations. A key problem is the often unreliable correlation between mutation load and disease severity, making it difficult to predict the clinical disease burden for the child and the likelihood of a couple having severely affected offspring [33]. Secondly, mutation load in chorionic villi or amniocytes may not be representative for the mutation load in various fetal tissues. Limited available data suggest that the mutation load of extra-embryonic tissues such as chorionic villi can be considered representative for the mutant load in the fetus [29, 33–35]. However, these data predominantly concern the mutations at nucleotide 8993, which are skewing mutations (as discussed above). Other reports on mtDNA polymorphic variants [36] and on the m.3243A>G mutation [10, 37] indicate that mtDNA mutations may segregate in the placenta, questioning the reliability of (a single) CVS sample analysis for mitochondrial disorders carried out in a PND framework. This is further supported by intra-placental mutation load variations up to 55 % which were reported by Monnot et al. [ESHG2013, Paris]. Finally, the segregation of mtDNA mutations throughout embryofetal development and the distribution of mutation load between different fetal tissues are not fully clarified, although based on existing data from both skewing and non-skewing mutations, these issues do not seem to be a restriction [10, 29–31, 34, 35, 38–47]. Indeed, the data show that the m.3243A>G mutation segregates quite stable throughout the prenatal period, and this is remarkably distinct from postnatal segregation.
Advantages of PND include its relatively low cost and lower physical burden compared to IVF procedures and the fact that no oocyte donor needs to be available. Disadvantages of PND are risk of miscarriage as a result of the invasive nature of the procedure and the decision the couple has to make with regard to terminating the pregnancy if results are unfavorable. The latter is obviously even more difficult when no firm predictions can be offered concerning the clinical outcome of the fetus. It has been reported that for most mtDNA point mutations, a fetus with mutation load below ~30 % or above approximately 90 % could be cautiously predicted to have a low or high probability, respectively, of being (severely) affected [33]. However, such guidelines were not based on a systematic analysis and may not be applicable for all mtDNA mutations. A systematic meta-analysis showed 95 % or higher chance of being unaffected at (muscle) mutation level of ≤18 %, irrespective of the mutation [47]. If possible, mutation-specific thresholds should be calculated as has been done with the m.3243A>G mutation (15 %) and the skewing m8993T>G mutations (30 %) (See below). A large range of mutation loads will fall within a “gray zone” with difficult or impossible interpretation, which is also the case for the m.3243A>G mutation. In 13 proven m.3243A>G carriers, a total of 19 (of which 2 occurred in the same twin pregnancy) prenatal diagnoses have been reported [10, 45, 48, 49]. Another four prenatal diagnosis cases were performed in three women without any detectable m.3243A>G mutation in leukocytes in two, and leukocytes and urine in one of them, but with considerable risk of being carriers [45, 49]. The m.3243A>G mutation was not detected in chorionic villi or amniocytes when the mutation was absent in maternal leukocytes [45, 49]. This was the case in four females (five prenatal diagnoses), one of them having 3 % mutant load in urinary tract cells. PND might indeed be an option for carriers with very low mutation load of the m.3243A>G mutation, although leukocytes seem not to be the best source to determine this—urine or muscle seems more appropriate [19–26]. Moreover, analysis of both chorionic villi and amniocytes in a carrier with 21 % mutant load in leukocytes failed to show the mutation in two fetuses [45]. One of these fetuses was part of a twin pregnancy where mutation loads of 60 % and 63 % were detected in chorionic villi and amniocytes, respectively of the other fetus. The pregnancy was (selectively) reduced for the fetus with the mtDNA mutation. Another example of an m.3243A>G carrier (mutant loads of 1% in blood and 18% in urine) without detectable mutation in chorionic villi was reported by Nesbitt et al. [49]. In two pregnancies of another carrier (with 80 % mutant load in urinary tract cells), mutation loads between 23 % and 35 % were detected; both pregnancies were continued [45]. The PND cases reported by Monnot et al. and Nesbitt et al. included four pregnancy terminations with mutation loads ranging from 59 % to 77 %, whereas, for example, a pregnancy with 79 % mutant load was continued [10, 49]. Chou et al. [48] were confronted with a carrier when she was already 8 weeks pregnant. This case illustrated the limited value of PND for this particular mutation: both of her children harbored similar (high) levels of mutant mtDNA, and the first child was severely affected and died at age 3½, whereas the second child was healthy at age 4.
For the (skewing) nt8993 mutations, PND is more feasible for carriers of a low mutation load, due to the high likelihood of unaffected offspring and a better correlation between mutation load and clinical phenotype. Seventeen cases of PND undertaken in 14 carriers with variable mutation loads of these mutations have been reported [30, 35, 38, 41, 42, 49, 50]. Prenatal diagnosis of another mtDNA mutation, m.9176T>C, in the ATPase6 gene has been reported in a family after a thorough work-up and counseling [51]. Limited data remain available about this mutation, especially concerning the genotype/phenotype correlation. The fetus appeared to have a mutation load of 87 % (CVS)–88 % (amniocentesis), just below the assumed threshold of expression (90 %). The couple decided to continue the pregnancy. A healthy child was born, not showing any abnormalities at the age of 13. Seven cases of PND in 7 carriers of other mtDNA mutations, namely m.8344A>G, m.13513G>A, m.11777C>A (n=2), m.10191T>C, m.10158T>C and m.3688G>A, respectively, were reported [49]. In four of them the pregnancy was continued (two without mutation in chorionic villi, one with 3% mutant load, one with 54% mutant load),data on pregnancy continuation or termination were not available in the remaining three.
Recently, we performed PND for an unaffected carrier of the m.3303C>T mtDNA mutation (unpublished data). The patient’s previous child, who had a nearly homoplasmic mtDNA mutation present in the blood and muscle, died at only age 5 months. Based on limited data from the literature and own experience, the expression threshold for this mutation was considered to be very high (90–95 %), and it was assumed that fetal mutant load between 0 % and 50 % would likely predict a subsequent child to be unaffected. In amniocytes, a mutant load of ~38 % was detected. The couple decided to continue the pregnancy, which is ongoing and thus far uneventful.
Altogether, PND is not a favorable choice for female carriers of mtDNA mutations with a high or unpredictable recurrence risk and a poor correlation between mutation load and phenotype; this is mainly because of difficulties in predicting the fetal phenotype when a certain mutation load is detected in chorionic villi or amniocytes. Still, when a carrier is already pregnant, PND can be offered with the understanding that a considerable chance exists that no interpretable result can be obtained.
Preimplantation Genetic Diagnosis
Another and fairly new option to prevent transmission of mtDNA mutations is preimplantation genetic diagnosis (PGD) [10, 27, 31, 52–55]. In PGD, embryos obtained after in vitro fertilization (IVF) are analyzed at the blastomere stage (day 3), and only those with amounts of mutant mtDNA below the predicted threshold of (severe) expression are transferred in the uterus. Our threshold for the m.3243A>G mutation (MELAS) is 15 % [22, 56] and 30 % for the skewing mutation m.8993T>G (Leigh) [29]. These guidelines are based on correlations between muscle mutation load and clinical manifestations, assuming that muscle mutation load correlates with the embryonic mutation load. This determination also embraces an arbitrary safety margin to correct for potential errors in determining heteroplasmy levels and for the limited number of data available.
Such thresholds, the preference of individual patients, and input from the clinician all appear to influence the decision on how many embryos to be transferred in the setting of mtDNA disease screening. In the Netherlands, the threshold is determined before a cycle will be started, and the couple agrees that the single best embryo below this threshold will be transferred. In other countries like France, the couple has a more decisive role in choosing the embryo for transfer, even if the embryo manifests a mutation load above the threshold of expression [10, 54, 55]. For most mtDNA mutations, insufficient data are available to establish a mutation-specific threshold level. A systematic meta-analysis showed 95 % or higher chance of being unaffected at (muscle) mutant level of 18 % or less, irrespective of the mutation [56]. This offers a solution for the difficulties in establishing a transfer threshold for mtDNA mutations and implicates that PGD can be offered for any heteroplasmic mutation. Obviously, this meta-analysis is a guideline, and careful counseling is necessary, stressing the limitations of applying these findings on individual cases when data are scarce.
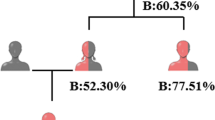
Prerequisites for PGD in mtDNA mutation carriers are the availability of oocytes with mutation load below the threshold for transfer and a comparable mutation load in all blastomeres of an embryo. We performed 14 PGD cycles in six mtDNA mutation carriers so far: four m.3243A>G carriers (a total of 9 cycles), one m.8993T>G carrier (4 IVF cycles), and one m.8344A>G carrier (1 cycle). The m.8993T>G carrier achieved two pregnancies, one resulting in a healthy son and the other pregnancy is ongoing [27]. The PGD results from this series are summarized in Fig. 17.1. Here, all carriers did indeed produce oocytes with a mutation load below the threshold, and the blastomere mutation load was generally representative for the whole embryo (although single outliers occasionally occur).
PGD cycles of the respective carrier females, performed in our center. Each cluster of bars represents an embryo with its tested blastomeres. The red dotted line represents the threshold level for transfer. For the Leigh carrier, the embryos in which the mutation was not detected are depicted as X. For these embryos, the numbers of analyzed blastomeres are not visible in the figure. ET embryo transfer, FR frozen, Bl blood, U urine, M muscle, H hair
Few additional reports of PGD performed for mtDNA disorders in other centers exist; a total of 12 cycles have been performed in nine mtDNA mutation carriers which resulted in the birth of five children [10, 31, 52, 54, 55]. In general, the mutation loads we observed for m.8993T>G among single blastomeres were concordant with previous reports [31, 52, 57]. Of note, interblastomere differences of 11 % have been noted [57] and fully descriptive data were not provided [52]; in our series, blastomeres/embryos with no mutation were overrepresented (25/28 embryos), making it difficult to draw a general conclusion. Interblastomere variation for the m.3243A>G mutation was generally larger and occurred more often than previously reported for this mutation [10, 54], although Monnot et al. did not perform single blastomere analysis for all embryos [10].
Vanderwoestyne et al. also reported large interblastomere variation of 24 % in an m.3243A>G embryo [53]. As interblastomere variation seems to occur more frequently in certain individuals, this itself might be a phenomenon subject to genetic factors [27] although insufficient data exist for such individual risk stratifications. All data taken together, nicely plotted in a figure by Steffann et al. [55], a generally homogeneous distribution of wild-type and mutant mtDNAs can be seen in individual human blastomeres regardless of the mutation, differing remarkably from data on artificially generated heteroplasmic macaque embryos [55, 58]. Based on human data which shows that single blastomeres can diverge, it is advisable to analyze two blastomeres instead of just one. The adverse risk of removing two cells from the embryo at biopsy is a negative influence on live birth delivery [59], illustrating the difficult balance between a safe and correct diagnosis on the one hand and optimizing the chance of pregnancy on the other.
Trophectoderm biopsy performed at the blastocyst stage provides a larger number of cells for analysis and appears to obviate the negative impact on live birth delivery. This approach would also enable more precise selection of a single embryo based on both mutation load and genetic sex. Male offspring with an mtDNA mutation will not encounter the risk of transmitting the mutation to their offspring. So far, only one blastocyst PGD for an mtDNA mutation (m.3243A>G) has been performed in humans although results were promising with regard to the applicability of blastocyst trophectoderm biopsy and PGD for mtDNA mutation carriers [54] (which had been supported by murine data [60]).
However, recently added follow-up data of the boy born after blastocyst PGD reported clinical symptoms and m.3243A>G mutant loads of 47 % and 46 % in blood and 52 % and 42 % in urine, respectively, at ages 6 weeks and 18 months [61]. The blastocyst mutation load had been only 12 % [54]. This contradicts the original report where no abnormal phenotype was reported and follow-up mutation load was 15 % in buccal mucosa at age 1 month; at ages of 5 and 12 months, the mutation load was measured by a commercial lab and found to be <10 % in blood and undetectable in buccal mucosa and urine [54]. While technical differences do exist between methods used to determine the mutation load, this cannot explain such a large difference. It is unclear what has happened, and the authors of both papers should work collaboratively to clarify this.
Data on the five children born so far after blastomere PGD at the 8-cell stage are much more reassuring [10, 27, 31, 52, 55]. Besides the balance between safety of embryo biopsy (the number of cells to remove for analysis) and subsequent reproductive outcome, the number of embryos available for analysis also brings some conflicting considerations. From the perspective of a cytogenetics laboratory, the more embryos available for study the better, since a larger sample improves the chances of having at least one embryo suitable for transfer (and thus improves the chances of delivering a healthy baby). However, there is a limit to the hormonal (over)stimulation that can be applied during IVF. and some clinically affected carriers will be found a priori to be poor candidates for PGD/IVF treatment (based on inacceptable health risks). For mtDNA mutation carriers approved to undergo IVF, it is important to realize that PGD for these indications represents a substantial risk reduction but not an absolute risk exclusion. This should be carefully discussed during patient counseling and the informed consent process. A 0 % mutation load only occurs seldomly (except for skewing mtDNA mutations). Furthermore, current data are suggestive, but not definitive, to guarantee that mutation load in the embryo stage will remain constant throughout life without passing the threshold level for symptoms at some later point. Nevertheless, we feel that for heteroplasmic mtDNA mutation carriers who want to have unaffected offspring who are biologically their own (and therefore not use donor oocytes), PGD represents the best therapeutic option at present. However, it should be acknowledged that PGD is not permitted in all jurisdictions.
PND Versus PGD: Specific Considerations with Respect to Skewing (8993) mtDNA Point Mutations
Although our considerations might be applicable to skewing mutations in general, only for the 8993 mutations do sufficient data currently exist. The characteristics of the nt8993 mutations make PND a feasible option for female carriers, particularly when mutation load is low. PGD is still an alternative in this group of mutation carriers with medium to high mutant load. The chance of producing embryos without the mutation is generally higher than for non-skewing mutations. In cases of high maternal mutation load, the majority of embryos is expected to have high mutation load although PGD will enable selection of those embryos with no or low mutation load. In contrast, PND would lead to the detection of multiple severely affected fetuses and recurrent pregnancy terminations.
If the maternal mtDNA mutation load is low, the majority of embryos would be expected to be without the mutation [27]. Due to the linear relationship between the mother’s and her offspring’s mutation load [29], for carriers with intermediate mutation load, the situation will be somewhere in the middle. In the choice between the two reproductive options and pregnancy risks, the burden of PGD treatment will need to be carefully considered.
Oocyte Donation
Perhaps the safest and most reliable method to prevent transmission of mtDNA disease is the use of donor oocytes accompanied by IVF using the partner’s sperm. However, the supply of suitable donors may be limited in some locations, and oocyte donation is not lawfully allowed in every country. Maternal relatives such as sisters will generally not be suitable as oocyte donors, as they are at risk of carrying the mutation in their oocytes as well. The latter cannot be excluded based on the absence of the mutation in blood or other tissues. An important personal reason for couples to reject oocyte donation is the fact that the resulting child would not be genetically related to the mother.
Nuclear Transfer
Nuclear transfer (maternal spindle transfer and pronuclear transfer) entails the transfer of the nuclear genome from an oocyte or zygote with mutated mtDNA in the cytoplasm (donor) to an enucleated acceptor oocyte or zygote of a healthy donor (acceptor) with presumably normal, mutation-free mtDNA. This technique is currently under investigation only in a research setting [62–67]. Although promising, the safety and efficacy of nuclear transfer which has been noted in primate models has yet to be shown compatible with humans, so this approach requires further study; important ethical issues also require resolution. Whether this technique will be able to completely exclude the risk of transmitting an mtDNA mutation or attain merely a reduction of this risk to offspring is still unclear, since nuclear transfer cannot avoid the co-transfer of small amounts (<1 % in spindle transfer) of mtDNA from the affected to the donor oocyte/zygote. Nuclear transfer techniques would offer a reproductive option for homoplasmic mtDNA mutation carriers and for heteroplasmic carriers with high mutation load, who might produce no or very few oocytes/embryos with mutation load below the threshold.
De Novo mtDNA Point Mutations
Counseling and Recurrence Risk
Besides being maternally inherited, mtDNA point mutation can also occur de novo in the affected individual, and this distinction makes a big difference for recurrence risk. If a de novo mutation is discovered in a child, this mutation is not expected to be present in his/her siblings. Due to the potential intra- and inter-tissue variability of mtDNA mutations, it can never be completely known for sure that the mother of the affected child does not carry any given mutation (i.e., a mutation load beneath the detection level, or the presence of a mtDNA mutation in any non-tested tissue, particularly the oocytes, would be impossible to exclude). However, proper analysis of multiple maternal tissues largely diminishes the residual risk of the mother having the mutation. Accordingly, for such de novo mtDNA point mutations, the recurrence risk is low, and the mutation is not expected to appear in a subsequent pregnancy. De novo mtDNA mutations are not rare events [1] Sallevelt et al in preparation, yet many such couples may be counseled incorrectly and given a high recurrence risk (erroneously), based on the high mutation load in the child instead of absence of the mutation in the mother.
Reproductive Testing Options
Given the low recurrence risk of apparently de novo mtDNA mutations, PND is feasible as reassurance Sallevelt et al in preparation. In four apparently de novo mtDNA disease cases based on the absence of the mutation in multiple maternal tissues, we have performed PND in a subsequent pregnancy. The mutation was not detected. In 9 of >100 reported cases describing apparently de novo mtDNA mutations, PND was performed in (a) subsequent pregnanc(y)(ies) with normal findings in the majority [35, 68–71], but recurrence in one family [49]. The latter might be the result of gonadal mosaicism, or of failed detection of very low mutation load in the mother’s lymphocytes and/or urinary epithelial cells due to the used sequencing method. This is currently being investigated further. PGD is, considering the burden of the treatment, not a favorable alternative in case of such a low recurrence risk.
mtDNA Rearrangements
Counseling and Recurrence Risk
Large, single mtDNA deletions are generally reported to occur sporadically, therefore having a low recurrence risk [72–74]. Indeed, the available data indicate that a clinically unaffected mother of an affected child has a negligible risk of another affected child [73]. Even for clinically affected mothers with an mtDNA deletion themselves, the risk of having clinically affected offspring is estimated to be low (1:24) [73]. mtDNA duplications are, like mtDNA point mutations, either maternally inherited or de novo and the same counseling aspects apply.
Reproductive Testing Options
PND seems the reproductive testing option of choice for de novo mtDNA rearrangements. Given the low recurrence risk even for women who carry an mtDNA deletion themselves, PND is the most feasible option in these cases, too. mtDNA duplications are, like mtDNA point mutations, either maternally inherited or de novo. For maternally inherited mtDNA duplications, the same considerations regarding reproductive testing options apply as for maternally inherited mtDNA point mutations.
Conclusion
Mitochondrial diseases are common metabolic disorders with potentially high morbidity and mortality. Generally, no treatment is available. Couples with a child affected by a mitochondrial disorder or a positive family history and a high risk of affected offspring may request prevention of transmission to a (future) child. Recurrence risks and the applicable reproductive testing options highly depend on the genetic etiology of the mitochondrial disease. For mitochondrial diseases due to nuclear gene defects, Mendelian segregation results in recurrence risks of 25 % or 50 %. Both PND and PGD are applicable, once the causative mutation has been identified. Recurrence risks particularly for mtDNA mutations should be determined on an individual basis, for example, taking into account the nature of the mutation and the mutation load in the mother. The risk for female carriers of mtDNA point mutations (such as the m.3243A>G mutation) of having affected offspring is often difficult to calculate, but it can be high. In those cases, PND is problematic mainly due to difficulties in predicting the phenotype with a given mutation load. PGD is currently the best reproductive testing option, although it should be regarded as a risk reduction strategy, rather than a method to exclude risk fully. Conversely, PGD is not the reproductive testing option of choice for apparently de novo mtDNA point mutations which have a low recurrence risk, making PND feasible for reassurance. The same is true for (large) mtDNA deletions which occur almost exclusively de novo. PND is also applicable for skewing mtDNA mutations, particularly when the mother has a low mutation load. The development of nuclear transfer technology would complete the portfolio of reproductive choices to prevent the transmission of mtDNA disease.
References
Thorburn DR. Mitochondrial disorders: prevalence, myths and advances. J Inherit Metab Dis. 2004;27(3):349–62.
Rotig A, Munnich A. Genetic features of mitochondrial respiratory chain disorders. J Am Soc Nephrol. 2003;14(12):2995–3007.
Howell N, et al. Mitochondrial gene segregation in mammals: is the bottleneck always narrow? Hum Genet. 1992;90(1–2):117–20.
Lightowlers RN, et al. Mammalian mitochondrial genetics: heredity, heteroplasmy and disease. Trends Genet. 1997;13(11):450–5.
Cao L, et al. The mitochondrial bottleneck occurs without reduction of mtDNA content in female mouse germ cells. Nat Genet. 2007;39(3):386–90.
Cree LM, et al. A reduction of mitochondrial DNA molecules during embryogenesis explains the rapid segregation of genotypes. Nat Genet. 2008;40(2):249–54.
Khrapko K. Two ways to make an mtDNA bottleneck. Nat Genet. 2008;40(2):134–5.
Cao L, et al. New evidence confirms that the mitochondrial bottleneck is generated without reduction of mitochondrial DNA content in early primordial germ cells of mice. PLoS Genet. 2009;5(12), e1000756.
Samuels DC, et al. Reassessing evidence for a postnatal mitochondrial genetic bottleneck. Nat Genet. 2010;42(6):471–2. author reply 472–3.
Monnot S, et al. Segregation of mtDNA throughout human embryofetal development: m.3243A>G as a model system. Hum Mutat. 2011;32(1):116–25.
Degoul F, et al. A near homoplasmic T8993G mtDNA mutation in a patient with atypic Leigh syndrome not present in the mother’s tissues. J Inherit Metab Dis. 1997;20(1):49–53.
Blok RB, et al. Skewed segregation of the mtDNA nt 8993 (T–>G) mutation in human oocytes. Am J Hum Genet. 1997;60(6):1495–501.
Brown DT, et al. Random genetic drift determines the level of mutant mtDNA in human primary oocytes. Am J Hum Genet. 2001;68(2):533–6.
Wanders RJ, et al. Prenatal diagnosis of systemic disorders of the respiratory chain in cultured amniocytes and chorionic villus fibroblasts by studying the formation of lactate and pyruvate from glucose. J Inherit Metab Dis. 1992;15(1):84–91.
Ruitenbeek W, et al. Genetic counselling and prenatal diagnosis in disorders of the mitochondrial energy metabolism. J Inherit Metab Dis. 1996;19(4):581–7.
Faivre L, et al. Determination of enzyme activities for prenatal diagnosis of respiratory chain deficiency. Prenat Diagn. 2000;20(9):732–7.
Niers L, et al. Prerequisites and strategies for prenatal diagnosis of respiratory chain deficiency in chorionic villi. J Inherit Metab Dis. 2003;26(7):647–58.
Jacobs LJ, et al. The transmission of OXPHOS disease and methods to prevent this. Hum Reprod Update. 2006;12(2):119–36.
t’Hart LM, et al. Heteroplasmy levels of a mitochondrial gene mutation associated with diabetes mellitus decrease in leucocyte DNA upon aging. Hum Mutat. 1996;7(3):193–7.
Howell N, et al. Longitudinal analysis of the segregation of mtDNA mutations in heteroplasmic individuals. J Neurol Sci. 2000;172(1):1–6.
Rahman S, et al. Decrease of 3243 A–>G mtDNA mutation from blood in MELAS syndrome: a longitudinal study. Am J Hum Genet. 2001;68(1):238–40.
Chinnery PF, et al. Molecular pathology of MELAS and MERRF. The relationship between mutation load and clinical phenotypes. Brain. 1997;120(Pt 10):1713–21.
Ma Y, et al. The study of mitochondrial A3243G mutation in different samples. Mitochondrion. 2009;9(2):139–43.
McDonnell MT, et al. Noninvasive diagnosis of the 3243A>G mitochondrial DNA mutation using urinary epithelial cells. Eur J Hum Genet. 2004;12(9):778–81.
Frederiksen AL, et al. Tissue specific distribution of the 3243A->G mtDNA mutation. J Med Genet. 2006;43(8):671–7.
Whittaker RG, et al. Urine heteroplasmy is the best predictor of clinical outcome in the m.3243A>G mtDNA mutation. Neurology. 2009;72(6):568–9.
Sallevelt SC, et al. Preimplantation genetic diagnosis in mitochondrial DNA disorders: challenge and success. J Med Genet. 2013;50(2):125–32.
Chinnery PF, et al. MELAS and MERRF. The relationship between maternal mutation load and the frequency of clinically affected offspring. Brain. 1998;121(Pt 10):1889–94.
White SL, et al. Genetic counseling and prenatal diagnosis for the mitochondrial DNA mutations at nucleotide 8993. Am J Hum Genet. 1999;65(2):474–82.
White SL, et al. Two cases of prenatal analysis for the pathogenic T to G substitution at nucleotide 8993 in mitochondrial DNA. Prenat Diagn. 1999;19(12):1165–8.
Steffann J, et al. Analysis of mtDNA variant segregation during early human embryonic development: a tool for successful NARP preimplantation diagnosis. J Med Genet. 2006;43(3):244–7.
White SL, et al. Mitochondrial DNA mutations at nucleotide 8993 show a lack of tissue- or age-related variation. J Inherit Metab Dis. 1999;22(8):899–914.
Thorburn DR, Dahl HH. Mitochondrial disorders: genetics, counseling, prenatal diagnosis and reproductive options. Am J Med Genet. 2001;106(1):102–14.
Dahl HH, Thorburn DR, White SL. Towards reliable prenatal diagnosis of mtDNA point mutations: studies of nt8993 mutations in oocytes, fetal tissues, children and adults. Hum Reprod. 2000;15 Suppl 2:246–55.
Steffann J, et al. Stability of the m.8993T->G mtDNA mutation load during human embryofetal development has implications for the feasibility of prenatal diagnosis in NARP syndrome. J Med Genet. 2007;44(10):664–9.
Marchington DR, et al. Mosaicism for mitochondrial DNA polymorphic variants in placenta has implications for the feasibility of prenatal diagnosis in mtDNA diseases. Eur J Hum Genet. 2006;14(7):816–23.
Marchington D, et al. Information for genetic management of mtDNA disease: sampling pathogenic mtDNA mutants in the human germline and in placenta. J Med Genet. 2010;47(4):257–61.
Harding AE, et al. Prenatal diagnosis of mitochondrial DNA8993 T––G disease. Am J Hum Genet. 1992;50(3):629–33.
Suomalainen A, et al. Quantification of tRNA3243(Leu) point mutation of mitochondrial DNA in MELAS patients and its effects on mitochondrial transcription. Hum Mol Genet. 1993;2(5):525–34.
Matthews PM, et al. Comparison of the relative levels of the 3243 (A–>G) mtDNA mutation in heteroplasmic adult and fetal tissues. J Med Genet. 1994;31(1):41–4.
Leshinsky-Silver E, et al. Prenatal exclusion of Leigh syndrome due to T8993C mutation in the mitochondrial DNA. Prenat Diagn. 2003;23(1):31–3.
Ferlin T, et al. Segregation of the G8993 mutant mitochondrial DNA through generations and embryonic tissues in a family at risk of Leigh syndrome. J Pediatr. 1997;131(3):447–9.
Poulton J, Marchington DR. Progress in genetic counselling and prenatal diagnosis of maternally inherited mtDNA diseases. Neuromuscul Disord. 2000;10(7):484–7.
Cardaioli E, et al. Heteroplasmy of the A3243G transition of mitochondrial tRNA(Leu(UUR)) in a MELAS case and in a 25-week-old miscarried fetus. J Neurol. 2000;247(11):885–7.
Bouchet C, et al. Prenatal diagnosis of myopathy, encephalopathy, lactic acidosis, and stroke-like syndrome: contribution to understanding mitochondrial DNA segregation during human embryofetal development. J Med Genet. 2006;43(10):788–92.
Jenuth JP, et al. Random genetic drift in the female germline explains the rapid segregation of mammalian mitochondrial DNA. Nat Genet. 1996;14(2):146–51.
Meirelles FV, Smith LC. Mitochondrial genotype segregation in a mouse heteroplasmic lineage produced by embryonic karyoplast transplantation. Genetics. 1997;145(2):445–51.
Chou YJ, et al. Prenatal diagnosis of a fetus harboring an intermediate load of the A3243G mtDNA mutation in a maternal carrier diagnosed with MELAS syndrome. Prenat Diagn. 2004;24(5):367–70.
Nesbitt et al. A national perspective on prenatal testing for mitochondrial disease. Eur J Hum Genet. 2014;22:1255–9.
Bartley J, Senadheera D, Park P, Brar H, Abad D, Wong L-J. Prenatal diagnosis of T8993G mitochondrial DNA point mutation in amniocytes by heteroplasmy detection. Am J Hum Genet. 1996;59:A317.
Jacobs LJ, et al. Transmission and prenatal diagnosis of the T9176C mitochondrial DNA mutation. Mol Hum Reprod. 2005;11(3):223–8.
Thorburn DR, Wilton L, Stock-Myer S. Healthy baby girl born following pre-implantation genetic diagnosis for mitochondrial DNA m.8993T>G mutation. Mol Genet Metab. 2009;98:5–6.
Vandewoestyne M, et al. Poor correlation between polar bodies and blastomere mutation load in a patient with m.3243A>G tRNALeu(UUR) point mutation. Mitochondrion. 2012;12(4):477–9.
Treff NR, et al. Blastocyst preimplantation genetic diagnosis (PGD) of a mitochondrial DNA disorder. Fertil Steril. 2012;98(5):1236–40.
Steffann J, et al. Data from artificial models of mitochondrial DNA disorders are not always applicable to humans. Cell Rep. 2014;7(4):933–4.
Hellebrekers DM, et al. PGD and heteroplasmic mitochondrial DNA point mutations: a systematic review estimating the chance of healthy offspring. Hum Reprod Update. 2012;18(4):341–9.
Tajima H, et al. The development of novel quantification assay for mitochondrial DNA heteroplasmy aimed at preimplantation genetic diagnosis of Leigh encephalopathy. J Assist Reprod Genet. 2007;24(6):227–32.
Lee HS, et al. Rapid mitochondrial DNA segregation in primate preimplantation embryos precedes somatic and germline bottleneck. Cell Rep. 2012;1(5):506–15.
De Vos A, et al. Impact of cleavage-stage embryo biopsy in view of PGD on human blastocyst implantation: a prospective cohort of single embryo transfers. Hum Reprod. 2009;24(12):2988–96.
Neupane J, et al. A systematic analysis of the suitability of preimplantation genetic diagnosis for mitochondrial diseases in a heteroplasmic mitochondrial mouse model. Hum Reprod. 2014;29(4):852–9.
Mitalipov S, et al. Limitations of preimplantation genetic diagnosis for mitochondrial DNA diseases. Cell Rep. 2014;7(4):935–7.
Tachibana M, et al. Mitochondrial gene replacement in primate offspring and embryonic stem cells. Nature. 2009;461(7262):367–72.
Craven L, et al. Pronuclear transfer in human embryos to prevent transmission of mitochondrial DNA disease. Nature. 2010;465(7294):82–5.
Craven L, et al. Mitochondrial DNA disease: new options for prevention. Hum Mol Genet. 2011;20(R2):R168–74.
Tachibana M, et al. Towards germline gene therapy of inherited mitochondrial diseases. Nature. 2013;493(7434):627–31.
Paull D, et al. Nuclear genome transfer in human oocytes eliminates mitochondrial DNA variants. Nature. 2013;493(7434):632–7.
Smeets HJ. Preventing the transmission of mitochondrial DNA disorders: selecting the good guys or kicking out the bad guys. Reprod Biomed Online. 2013;27(6):599–610.
Lebon S, et al. Recurrent de novo mitochondrial DNA mutations in respiratory chain deficiency. J Med Genet. 2003;40(12):896–9.
Shanske S, et al. The G13513A mutation in the ND5 gene of mitochondrial DNA as a common cause of MELAS or Leigh syndrome: evidence from 12 cases. Arch Neurol. 2008;65(3):368–72.
Gotz A, et al. Fatal neonatal lactic acidosis caused by a novel de novo mitochondrial G7453A tRNA-Serine (UCN) mutation. Pediatr Res. 2012;72(1):90–4.
Shanske S, et al. Mutation in an mtDNA protein-coding gene: prenatal diagnosis aided by fetal muscle biopsy. J Child Neurol. 2013;28(2):264–8.
Zeviani M, Antozzi C. Mitochondrial disorders. Mol Hum Reprod. 1997;3(2):133–48.
Chinnery PF, et al. Risk of developing a mitochondrial DNA deletion disorder. Lancet. 2004;364(9434):592–6.
Chinnery PF, Hudson G. Mitochondrial genetics. Br Med Bull. 2013;106:135–59.
Acknowledgments
“Stichting Metakids”; referring neurologists and clinical geneticists; PND and PGD teams, Maastricht University Medical Centre+; Department of Obstetrics and Gynaecology, Maastricht University Medical Centre. The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure All authors are paid by the respective institutions according to his/her job contract. “Stichting Metakids” has funded research/work on mitochondrial diseases. The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sallevelt, S.C.E.H., Dreesen, J.C.F.M., de Coo, I.F.M., de Die-Smulders, C.E.M., Smeets, H.J.M. (2015). Selecting the Right Embryo in Mitochondrial Disorders. In: Sills, E. (eds) Screening the Single Euploid Embryo. Springer, Cham. https://doi.org/10.1007/978-3-319-16892-0_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-16892-0_17
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16891-3
Online ISBN: 978-3-319-16892-0
eBook Packages: MedicineMedicine (R0)