Abstract
Recent clinical trials have demonstrated that aromatase inhibitors (AIs) are slightly more effective than tamoxifen at reducing breast cancer recurrences. However, breast cancer patients receiving AIs have a higher incidence of musculoskeletal symptoms, particularly joint pain and stiffness. Musculoskeletal pain and stiffness can lead to noncompliance and increased utilization of health care resources. There is a suggestion that the syndrome is the result of estrogen deprivation and may share components with autoimmune diseases such as Sjögren’s syndrome. Several factors may increase the likelihood of developing AI arthralgia, such as prior chemotherapy, prior hormone replacement therapy, and increased weight; there are inconsistencies with regard to the data on genetic predispositions to this syndrome. While several studies have been done to evaluate interventions to treat or prevent AI arthralgia, no clear treatment has emerged as being particularly beneficial. Much of the research has been limited by small sample size, difficulty blinding patients to placebo, inconsistent definitions of the syndrome, multiple patient reported outcomes, lack of objective outcome measures and heterogeneous patient populations. We are at the early stages of research in characterizing, understanding etiology, preventing and treating AI arthralgias; however much work is being done in this area which, hopefully, will ultimately improve the lives of women with breast cancer.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Overview
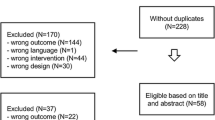
Due to early detection and improved treatments, there has been a 30 % reduction in breast cancer (BC) mortality over the past two decades (DeSantis et al. 2014). The increase in BC survival is largely due to the benefits of hormonal therapy in women with hormone receptor (HR) positive breast cancer. Recent clinical trials have demonstrated that aromatase inhibitors (AIs) are more effective than tamoxifen at reducing BC recurrences (Baum et al. 2002; Goss et al. 2003, 2005; Howell et al. 2005; Thurlimann et al. 2005; Coombes et al. 2004). However, BC patients receiving AIs have a higher incidence of musculoskeletal symptoms, particularly joint pain and stiffness. Musculoskeletal pain and stiffness leads to noncompliance and increased utilization of health care resources (Henry et al. 2012.; Scudds and Mc 1998; Kewman et al. 1991; Carey et al. 1995). In a prospective study of 1,976 patients, a 10 % increase in arthralgia was associated with a 20 % increase risk of non-compliance to AI therapy (Hadji et al. 2014). Since women with HR-positive BC benefit from long-term hormonal therapy for 5–10 years, it is important to try to minimize side effects, to enhance patient adherence and to improve quality of life (QOL). Therefore, safe and effective treatments that alleviate these symptoms are needed. There is no standard definition, consistent terminology or agreed upon outcome measures for this condition. Some refer to it as AI Arthralgia (AIA) or AI Musculoskeletal Syndrome (AIMSS) (Niravath 2013) (Fig. 7.1).
Possible management algorithm from Niravath (2013)
In large adjuvant trials involving AIs, the incidence of musculoskeletal disorders was reported in 19–35 % of patients on AI’s and 12–29 % of patients on tamoxifen (Baum et al. 2002; Goss et al. 2003). However, prospective cohort studies assessing symptoms with patient reported outcome measures suggest that 40–50 % of women have either new onset or worsening AI-related arthralgias (Crew et al. 2007; Henry et al. 2008, 2012). In a small prospective study of patients initiating AI therapy, the median time to development of AI arthralgias was 7 weeks, and by 12 weeks 55 % of patients had at least one complaint, and the incidence increased steadily over time (Shi et al. 2013). Other prospective cohort studies have found a similar incidence (Laroche et al. 2014).
Several studies have suggested an association between the development of AI arthralgias and improved disease free survival outcomes; however other studies have not shown this association. For example, a retrospective analysis of the ATAC data shows that women who developed arthralgia had a breast cancer recurrence HR of 0.65 (P = 0.001) when compared with women with no arthralgia (Cuzick et al. 2008). Similarly, analysis of the TEAM trial showed improvements in disease-free survival in patients who had arthralgia while on endocrine therapy (Hadji et al. 2012). This is in contrast to the Intergroup Exemestane study that did not find this association (Mieog et al. 2012). Measurement error is a real problem with these studies, as they primarily rely on CTCAE reporting, and not patient reported outcomes.
Etiology
Estrogen deficiency after menopause has been linked to an increase in several chronic inflammatory conditions, including osteoporosis and osteoarthritis (OA) (Riggs and Melton 1992; Sherwin 1996). Estrogen can influence chondrocyte formation on multiple levels by interacting with cellular growth factors, adhesion molecules, and cytokines (Ushiyama et al. 1995; Rosner et al. 1982; Dayani et al. 1988). A dose-dependent change in matrix protein turnover occurs when cultured chondrocytes are exposed to estradiol (Richmond et al. 2000; Dayani et al. 1988; Blanchard et al. 1991; Rosner et al. 1982). Production of interleukin-6 (IL-6) and type II collagen in articular chondrocytes is also affected by estradiol, suggesting it may affect cartilage metabolism (Guerne et al. 1990; Claassen et al. 2006; Richette et al. 2003). Additional support that estrogen deprivation results in this syndrome comes from studies showing that hormone replacement with conjugated equine estrogens result in decreased joint pain, pain severity and joint swelling in postmenopausal women (Chlebowski et al. 2013).
In addition, there may be an autoimmune component to the syndrome. Animal models, where aromatase is knocked out, manifest symptoms similar to Sjögren’s syndrome. In a study of patients referred to a rheumatologist, 50 % met the criteria for sicca syndrome (Laroche et al. 2007). Several small studies have also evaluated the influence AI therapy on inflammatory serum markers but results evaluating CRP, IL-6, and TNFα have been inconsistent (Dougherty et al. 2005; Azria et al. 2007; Harputluoglu et al. 2008). Even in studies showing AI-related changes to inflammatory markers, these changes were not correlated with the development of AI arthralgia (Azria et al. 2007).
Studies assessing AI-induced arthralgias have shown a correlation between PROs and objective findings. Morales et al. demonstrated that the subjective symptoms of AI-induced arthralgias in the hands are associated with physiologic changes to joints and functional impairments (Morales et al. 2008). Women taking AIs are more likely to have an increase in tenosynovial changes as seen on MRI, a decrease in grip strength as measured by a sphygmomanometer, as well as increased pain and stiffness as measured by self-administered questionnaires (Morales et al. 2008). In a study conducted by Dizdar et al., women taking AIs had increased tendon thickness and higher rates of effusions in hand joints/tendons on musculoskeletal sonography, compared to women who never received AIs (Dizdar et al. 2009; Lintermans et al. 2011). AI use is also associated with a greater incidence of carpal tunnel syndrome of moderate intensity and short duration (Sestak et al. 2009). With regard to pain sensitivity, the syndrome does not appear to result in impairment of descending pain inhibitory pathways as measured by pressure pain testing or conditioned pain modulation testing (Henry et al. 2014).
Risk Factors
The risk factors for developing AI-associated arthralgia are unclear. In some studies high BMI, prior chemotherapy, and a history of hormone replacement therapy are major risk factors for developing joint symptoms (Sestak et al. 2008). Other studies show prior taxane chemotherapy, symptoms at the time of treatment initiation and time from menopause are also associated with severity of AI arthralgias (Shi et al. 2013; Crew et al. 2007; Mao et al. 2011). One prospective cohort study found that additional risk factors for the development of pain included higher levels of anxiety and impaired quality of life at the time of initiation of therapy (Laroche et al. 2014).
The question of genetic susceptibility to toxicity has been addressed as well. In a prospective cohort study of 343 post-menopausal women starting AI therapy, single nucleotide polymorphisms (SNPs) in genes encoding for the metabolism of estrogens (CYP17A1) and vitamin D (VDR, CYP27B1) were associated with self-reported arthralgia (Garcia-Giralt et al. 2013). In addition, patients who had SNP’s for multiple genes had the highest risk for AI arthralgia. A cross-sectional study in 390 patients also found that repeats in the CYP19A1 gene were associated with AI arthralgias (Mao et al. 2011). A better understanding of genomic and clinical risk factors can help identify patients who can be targeted for specific interventions to prevent this syndrome. An ongoing ECOG prospective cohort study in 1,000 women evaluating genomic predictors of AI arthralgias and early AI discontinuation should further clarify this issue.
Treatment
The use of a non-steroidal anti-inflammatory agent, or simply switching to an alternative AI, are common clinical approaches for patients experiencing significant arthralgias. Interestingly, approximately a third of patients will experience some improvement in symptoms by simply switching to another AI (Henry et al. 2012). There are, however, currently no proven treatments for AI-related arthralgias. Researchers have investigated interventions that have been studied in patients with chronic pain conditions, osteoarthritis and rheumatologic arthritis. Patients are often not willing to take medications to treat side effects, that have the potential for additional side effects, so many have gravitated to natural products, mind-body interventions and exercise. Many prospective trials are collecting blood and DNA to perform analysis that will be critical in elucidating the mechanism of this side effect as well as genetic susceptibility (Table 7.1).
Vitamin D
Vitamin D deficiency and insufficiency may contribute to musculoskeletal symptoms. In a prospective study, 60 women who were beginning adjuvant AI therapy had baseline vitamin D (25OHD) levels measured. At the conclusion of 16 weeks of letrozole, 52 % of women with baseline 25OHD levels >66 ng/ml reported no disability from joint pain, whereas only 19 % of those with levels <66 ng/ml had no disabling joint pain (Khan et al. 2010). In a subsequent randomized VITAL trial (Vitamin D for Arthralgias From Letrozole), 160 postmenopausal women with a serum vitamin D level of <40 ng/mL were randomized to receive 30,000 IU of oral vitamin D3 weekly for 24 weeks; the other was given a placebo. About 61 % of controls and 38 % of those on vitamin D reported an increase in pain (P = .008) (Khan et al. 2012).
Glucosamine Chondroitin
Glucosamine and chondroitin are popular dietary supplements frequently used with the goal of treating arthritic pain. In a non-randomized phase II trial of glucosamine and chondroitin to treat moderate-to-severe aromatase inhibitor induced joint pain, approximately 50 % of participants self-reported a ≥20 % improvement in pain, stiffness and function. The intervention was well-tolerated with minimal toxicities and no changes in estradiol levels were observed (Greenlee et al. 2013). Nonetheless, a placebo effect may be largely responsible for this finding.
Omega-3
Omega-3-fatty acids have anti-inflammatory effects and can be effective in decreasing arthralgias from rheumatologic conditions. A placebo-controlled trial of 3.3 g of Omega-3-fatty acids was conducted among 249 women on AIs with severe (≥5 of 10) pain and or stiffness. Interestingly a 60 % improvement was observed in the group randomized to Omega-3. However, a similar reduction was seen in the placebo arm. At 24 weeks, both groups had about a 2-point improvement from baseline on a 10 point scale (Hershman et al. 2014). This study demonstrates the difficulty in relying on patient-reported outcomes and the strength of the placebo effect. It also raises questions about the results of other trials where the intervention could not be truly blinded.
Duloxetine
Duloxetine is a selective serotonin and norepinephrine reuptake inhibitor used for treating pain. A single-arm, open-label phase 2 study of duloxetine was studied in women with breast cancer who developed new or worsening pain after treatment with an AI. Twenty-one of twenty-nine evaluable patients (72.4 %) achieved at least a 30 % decrease in average pain. The mean percentage reduction in average pain severity was 60.9 % (Henry et al. 2011). Based on the results of this study, a randomized placebo-controlled trial is being conducted in SWOG.
Testosterone
A double blind placebo-controlled, randomized pilot study of a transdermal testosterone preparation supported that this approach was helpful for alleviating aromatase inhibitor-induced arthralgias (Birrell and Tilley 2009). This trial involved 90 patients with baseline AI arthralgia pain and/or stiffness be greater than 50 on a 0–100 point pain scale. Patients were randomized into one of three study arms to receive a low testosterone dose versus an intermediate testosterone dose versus a placebo. After 3 months, the pain scores decreased more in the intermediate dose testosterone arm compared to the placebo arm (P = 0.04). Likewise, stiffness scores decreased more in the intermediate dose testosterone arm, compared to the placebo arm (P = 0.06). While serum testosterone concentrations increased in the groups getting testosterone, there was no suggestion that estrogen concentrations were any higher with testosterone, compared to the placebo arm. Based on these promising findings a phase III randomized placebo-controlled trial, using intradermal testosterone pellets, is being conducted in women with AI arthralgias, through the Alliance cooperative group.
Prednisolone
Autoimmune diseases are often treated with low dose steroids, and as mentioned above, there is some similarities between the arthralgia syndrome from AI’s and Sjögren’s syndrome. To test this approach, patients with AI arthralgia were administered 5 mg of oral prednisolone once a day in the morning for only 1 week. Patients were then asked to answer a questionnaire about joint pain symptoms at 1 week, 1 month and 2 months after the beginning of prednisolone use. Joint pain symptoms improved in 67 % of patients immediately after prednisolone use, with 63 % still reporting analgesic effect at 1 month, and 52 % at 2 months after beginning the short-term use of prednisolone (Kubo et al. 2012).
Acupuncture
Acupuncture is a popular non-pharmacologic modality that has been shown to be a useful adjunct in a range of painful conditions, including musculoskeletal pain (Anonymous 1998). Small pilot trials for AI arthralgias have reported conflicting results. A randomized, sham-controlled, blinded trial to assess the effect of a 6-week intervention of acupuncture in 38 women with AI-associated joint symptoms reported that true acupuncture group had a 50 % decrease pain compared to no change in the sham acupuncture group (Crew et al. 2010). Other smaller studies have suggested a benefit of both standard and electroacupuncture (Oh et al. 2013; Mao et al. 2014). A larger multicenter randomized trial with a waitlist control, sham, and true acupuncture is being conducted in SWOG.
Exercise
Several studies have suggested that exercise can reduce treatment-related adverse effects. A randomized trial of 121 women with AI arthralgia reported that pain scores decreased by 24 % at 12 months among women randomized to exercise vs. no change among women randomized to usual care (mean baseline to 12-month change: −1.27 + 0.34 vs. −0.01 + 0.35, respectively; P = .013). A dose–response effect was also observed with greater exercise leading to less pain severity (Irwin et al. 2013). In addition, a small pilot study of tai chi in 12 women with self reported AI arthralgia demonstrated a reduction in pain (Galantino et al. 2013). Additional work in this area is warranted, however, these studies are limited by the inability to blind participants.
Switching
Two studies have been done suggesting switching AI’s can result in improvement of symptoms. In one study, 60 % of patients that switched remained on the alternate AI at 6 months, and 15 % had no complaints of joint symptoms (Briot et al. 2010). Another study showed that 39 % of patients were able to tolerate the second AI (Henry et al. 2012). Given the strong placebo effect, these results should be interpreted with caution with regard to the biologic effect of switching treatments. Another approach is to switch to tamoxifen, a therapy with similar long-term benefits.
Future Directions
There is enormous discrepancy between studies evaluating AI arthralgia due to lack of uniformity in both subjective and objective outcome measures and inconsistency in reporting. As a result priorities going forward might focus on uniform definitions, a better understanding of the natural history, defining mechanisms and determining effective treatment and prevention strategies. While there has been some work evaluating the syndrome, the heterogeneity in terminology and definitions can make interpreting the findings difficult. A consensus on consistent terminology and definition might help with future studies.
The original large phase III clinical trials resulting in drug approval did not capture patient reported outcomes, which was a missed opportunity for understanding this syndrome in a large number of women. Because the symptoms were often not attributed to the drug, these trials underestimated the degree to which these side effects interfere with quality of life, adherence and function. Cohort studies have used a variety of patient reported outcomes such as the Brief Pain Inventory (BPI), the Health Assessment Questionnaire (HAQ), the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and the Score for Assessment and Quantification of Chronic Rheumatic Affections of the Hands (SACRAH). Consistent outcome measures would allow for better consistency of interpreting the results of interventional trials.
There are ongoing cohort studies, as the one being done through ECOG, where 1,000 patients are being followed at initiation of AI therapy and evaluated over the course of a year. In addition DNA and serum are being collected to clarify if there are genetic determinants of risk. This study should help clarify the short-term natural history. However the 1 year follow-up will limit the understanding of delayed symptoms and poor adherence. Another shortcoming of this trial, as opposed to the missed opportunity in the early randomized trials is that there is no placebo arm with which to better understand any nocebo effect. In addition, understanding the factors that contribute to improvement of symptoms in some patients, as opposed to others, may help physicians make better therapeutic recommendations.
A clearer understanding of the mechanism behind AI arthralgia may result in more targeted interventions or drug modifications that could reduce the development of this secondary effect. However, it may be that the exact mechanism that results in the drug effectiveness, i.e., the lowering of estradiol, may be the inciting factor. Careful attention will need to be paid to the fact that improvements in symptoms could affect the efficacy of the therapy if directed to the mechanism of action. As a result pure management of symptoms with interventions known to improve pain or treat other forms of arthritis have been studied.
Understanding risk factors may help risk stratify patients for treatment with tamoxifen or AI therapy, and may help target preventive interventions. Early suggestions from a biologic perspective have focused on estrogen-related pathways and polymorphisms in the aromatase pathway. It is clear that prior chemotherapy, prior hormone replacement therapy and baseline psychological state may influence the development of symptoms and adherence. These factors as well as genetic factors may help determine which patients should avoid AIs upfront and be treated with tamoxifen from the start. It will be crucial to understand if these individuals have a different prognosis.
The optimal outcome measure and timing of assessments is unclear, therefore clinical trials often vary from each other in primary outcome, duration and patient populations. The issue of placebo effect, as demonstrated by the SWOG Omega-3 study makes clinical trials challenging, and should push the field to try to better define objective as well as subjective definitions of this syndrome. Furthermore, many clinical trials cannot be truly blinded and may result in inaccurate conclusions. Interventional studies are subject to biases resulting from a very strong placebo effect and a waxing and waning symptom course.
The ultimate goal of treating or preventing AI arthralgias is to improve quality of life and increase adherence while maintaining efficacy, so these outcomes need to be considered in prevention and treatment studies.
References
Anonymous (1998) NIH consensus conference. Acupuncture. JAMA 280:1518–1524
Azria D, Lamy Y, Belkacemi G et al (2007) Letrozole-induced arthralgia: results of a multicenteric prospective trial exploring clinical parameters and plasma biomarkers. ASCO Breast Cancer Symposium
Baum M, Budzar AU, Cuzick J (2002) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet 359:2131–2139 [see comment][erratum appears in Lancet 2002 Nov 9;360(9344):1520]
Birrell S, Tilley W (2009) Testosterone undecanoate treatment reduces joint morbidities induced by anastrozole therapy in postmenopausal women with breast cancer: results of a double-blind, randomized phase II trial. San Antonio breast cancer symposium
Blanchard O, Tsagris L, Rappaport R et al (1991) Age-dependent responsiveness of rabbit and human cartilage cells to sex steroids in vitro. J Steroid Biochem Mol Biol 40:711–716
Briot K, Tubiana-Hulin M, Bastit L et al (2010) Effect of a switch of aromatase inhibitors on musculoskeletal symptoms in postmenopausal women with hormone-receptor-positive breast cancer: the ATOLL (articular tolerance of letrozole) study. Breast Cancer Res Treat 120:127–134
Carey TS, Evans A, Hadler N et al (1995) Care-seeking among individuals with chronic low back pain. Spine 20:312–317
Chlebowski RT, Cirillo DJ, Eaton CB et al (2013) Estrogen alone and joint symptoms in the women’s health initiative randomized trial. Menopause 20:600–608
Claassen H, Schluter M, Schunke M et al (2006) Influence of 17beta-estradiol and insulin on type II collagen and protein synthesis of articular chondrocytes. Bone 39:310–317
Coombes RC, Hall E, Gibson LJ et al (2004) A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 350:1081–1092
Crew KD, Greenlee H, Capodice J et al (2007) Prevalence of joint symptoms in postmenopausal women taking aromatase inhibitors for early-stage breast cancer. J Clin Oncol 25:3877–3883
Crew KD, Capodice J, Greenlee H et al (2010) Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early stage breast cancer. J Clin Oncol 28:1154–1160
Cuzick J, Sestak I, Cella D et al (2008) Treatment-emergent endocrine symptoms and the risk of breast cancer recurrence: a retrospective analysis of the ATAC trial. Lancet Oncol 9:1143–1148
Dayani N, Corvol MT, Robel P et al (1988) Estrogen receptors in cultured rabbit articular chondrocytes: influence of age. J Steroid Biochem 31:351–356
DeSantis C, Ma J, Bryan L et al (2014) Breast cancer statistics, 2013. CA Cancer J Clin 64:52–62
Dizdar O, Ozcakar L, Malas FU et al (2009) Sonographic and electrodiagnostic evaluations in patients with aromatase inhibitor-related arthralgia. J Clin Oncol 27:4955–4960
Dougherty RH, Rohrer JL, Hayden D et al (2005) Effect of aromatase inhibition on lipids and inflammatory markers of cardiovascular disease in elderly men with low testosterone levels. Clin Endocrinol (Oxf) 62:228–235
Galantino ML, Callens ML, Cardena GJ et al (2013) Tai chi for well-being of breast cancer survivors with aromatase inhibitor-associated arthralgias: a feasibility study. Altern Ther Health Med 19:38–44
Garcia-Giralt N, Rodriguez-Sanz M, Prieto-Alhambra D et al (2013) Genetic determinants of aromatase inhibitor-related arthralgia: the B-ABLE cohort study. Breast Cancer Res Treat 140:385–395
Goss PE, Ingle JN, Martino S et al (2003) A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med 349:1793–1802 [see comment]
Goss PE, Ingle JN, Martino S et al (2005) Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J Natl Cancer Inst 97:1262–1271
Greenlee H, Crew KD, Shao T et al (2013) Phase II study of glucosamine with chondroitin on aromatase inhibitor-associated joint symptoms in women with breast cancer. Support Care Cancer 21:1077–1087
Guerne PA, Carson DA, Lotz M (1990) IL-6 production by human articular chondrocytes. Modulation of its synthesis by cytokines, growth factors, and hormones in vitro. J Immunol 144:499–505
Hadji P, Kieback DG, Tams J et al (2012) Correlation of treatment-emergent adverse events and clinical response to endocrine therapy in early breast cancer: a retrospective analysis of the German cohort of TEAM. Ann Oncol 23:2566–2572
Hadji P, Jackisch C, Bolten W et al (2014) COMPliance and arthralgia in clinical therapy: the COMPACT trial, assessing the incidence of arthralgia, and compliance within the first year of adjuvant anastrozole therapy. Ann Oncol 25:372–377
Harputluoglu H, Dizdar O, Malas U et al (2008) Aromatase inhibitor-associated arthralgia: prevalence, clinical and serum parameters among Turkish postmenopausal breast cancer patients. ASCO Annual Meeting. J Clin Oncol (May 20 supplement)
Henry NL, Giles JT, Ang D et al (2008) Prospective characterization of musculoskeletal symptoms in early stage breast cancer patients treated with aromatase inhibitors. Breast Cancer Res Treat 111:365–372
Henry NL, Banerjee M, Wicha M et al (2011) Pilot study of duloxetine for treatment of aromatase inhibitor-associated musculoskeletal symptoms. Cancer 117:5469–5475
Henry NL, Azzouz F, Desta Z et al (2012) Predictors of aromatase inhibitor discontinuation as a result of treatment-emergent symptoms in early-stage breast cancer. J Clin Oncol 30:936–942
Henry NL, Conlon A, Kidwell KM et al (2014) Effect of estrogen depletion on pain sensitivity in aromatase inhibitor-treated women with early-stage breast cancer. J Pain 15:468–475
Hershman D, Unger J, Crew K et al (2014) Omega-3 fatty acids for aromatase inhibitor–induced musculoskeletal symptoms in women with early-stage breast cancer (SWOG S0927)
Howell A, Cuzick J, Baum M et al (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62
Irwin M, Cartmel B, Gross C et al (2013) Effect of exercise vs. usual care on aromatase inhibitor-associated arthralgias in women with early stage breast cancer: the hormones and physical exercise (HOPE) Study. SABCS
Kewman DG, Vaishampayan N, Zald D et al (1991) Cognitive impairment in musculoskeletal pain patients. Int J Psychiatry Med 21:253–262
Khan QJ, Reddy PS, Kimler BF et al (2010) Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat 119(1):111–118
Khan Q, Kimler B, Reddy P et al (2012) Randomized trial of vitamin D3 to prevent worsening of musculoskeletal symptoms and fatigue in women with breast cancer starting adjuvant letrozole: the VITAL trial. J Clin Oncol 30(suppl; abstr 9000)
Kubo M, Onishi H, Kuroki S et al (2012) Short-term and low-dose prednisolone administration reduces aromatase inhibitor-induced arthralgia in patients with breast cancer. Anticancer Res 32:2331–2336
Laroche M, Borg S, Lassoued S et al (2007) Joint pain with aromatase inhibitors: abnormal frequency of Sjogren’s syndrome. J Rheumatol 34:2259–2263
Laroche F, Coste J, Medkour T et al (2014) Classification of and risk factors for estrogen deprivation pain syndromes related to aromatase inhibitor treatments in women with breast cancer: a prospective multicenter cohort study. J Pain 15:293–303
Lintermans A, Van Calster B, Van Hoydonck M et al (2011) Aromatase inhibitor-induced loss of grip strength is body mass index dependent: hypothesis-generating findings for its pathogenesis. Ann Oncol 22:1763–1769
Mao JJ, Su HI, Feng R et al (2011) Association of functional polymorphisms in CYP19A1 with aromatase inhibitor associated arthralgia in breast cancer survivors. Breast Cancer Res 13:R8
Mao JJ, Xie SX, Farrar JT et al (2014) A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur J Cancer 50:267–276
Mieog JS, Morden JP, Bliss JM et al (2012) Carpal tunnel syndrome and musculoskeletal symptoms in postmenopausal women with early breast cancer treated with exemestane or tamoxifen after 2-3 years of tamoxifen: a retrospective analysis of the intergroup exemestane study. Lancet Oncol 13:420–432
Morales L, Pans S, Verschueren K et al (2008) Prospective study to assess short-term intra-articular and tenosynovial changes in the aromatase inhibitor-associated arthralgia syndrome. J Clin Oncol 26:3147–3152
Niravath P (2013) Aromatase inhibitor-induced arthralgia: a review. Ann Oncol 24:1443–1449
Oh B, Kimble B, Costa DS et al (2013) Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer: pilot study. Acupunct Med 31:264–271
Richette P, Corvol M, Bardin T (2003) Estrogens, cartilage, and osteoarthritis. Joint Bone Spine 70:257–262
Richmond RS, Carlson CS, Register TC et al (2000) Functional estrogen receptors in adult articular cartilage: estrogen replacement therapy increases chondrocyte synthesis of proteoglycans and insulin-like growth factor binding protein 2. Arthritis Rheum 43:2081–2090
Riggs BL, Melton LJ 3rd (1992) The prevention and treatment of osteoporosis. N Engl J Med 327:620–627 [see comment][erratum appears in N Engl J Med. 1993 Jan 7;328(1):65; author reply 66; PMID: 8416278]
Rosner IA, Manni A, Malemud CJ et al (1982) Estradiol receptors in articular chondrocytes. Biochem Biophys Res Commun 106:1378–1382
Scudds RJ, Mc DRJ (1998) Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain 75:229–235
Sestak I, Cuzick J, Sapunar F et al (2008) Risk factors for joint symptoms in patients enrolled in the ATAC trial: a retrospective, exploratory analysis. Lancet Oncol 9:866–872
Sestak I, Sapunar F, Cuzick J (2009) Aromatase inhibitor-induced carpal tunnel syndrome: results from the ATAC trial. J Clin Oncol 27:4961–4965
Sherwin BB (1996) Hormones, mood, and cognitive functioning in postmenopausal women. Obstet Gynecol 87
Shi Q, Giordano SH, Lu H et al (2013) Anastrozole-associated joint pain and other symptoms in patients with breast cancer. J Pain 14:290–296
Thurlimann B, Keshaviah A, Coates AS et al (2005) A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 353:2747–2757
Ushiyama T, Inoue K, Nishioka J (1995) Expression of estrogen receptor related protein (p29) and estradiol binding in human arthritic synovium. J Rheumatol 22:421–426
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Breast Cancer Research Foundation
About this chapter
Cite this chapter
Hershman, D.L., Loprinzi, C., Schneider, B.P. (2015). Symptoms: Aromatase Inhibitor Induced Arthralgias. In: Ganz, P. (eds) Improving Outcomes for Breast Cancer Survivors. Advances in Experimental Medicine and Biology(), vol 862. Springer, Cham. https://doi.org/10.1007/978-3-319-16366-6_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-16366-6_7
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16365-9
Online ISBN: 978-3-319-16366-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)