Key Points
-
Older adults are at high risk for deconditioning as a result of bed rest during hospitalization.
-
Deconditioning results in loss of function and discharge to higher levels of care, such as a nursing home, even after short or elective hospital stays.
-
Older adults can participate in walking, resistance exercises, and early rehabilitation programs without increasing adverse events during acute hospitalization.
-
Geriatric acute hospital units using comprehensive geriatric assessment, multidisciplinary teams, and interventions targeted to preserving function and mobility have the strongest evidence for reducing decline.
-
Older adults for whom exercise may present significant risk or for whom exercise is not possible may benefit from passive range of motion and changes in position.
-
System-wide interventions, such as changing the default activity order to out of bed, are recommended by experts yet require more study.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hospital
- Older adult
- Elder
- Deconditioning
- Immobility
- Bed rest
- Exercise
- Geriatric assessment
- Geriatric unit
- ACE unit
- Geriatric consult team
- Physical therapy
- Walking in hospital
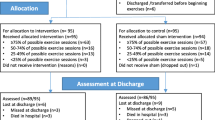
Lavern is an 82-year-old woman hospitalized after a few days’ illness at home with fever, cough, and probable pneumonia. She is admitted to the general medical ward and treated with IV fluids, antibiotics, acetaminophen, and oxygen by nasal cannula. After 24 h, she is able to sit up in bed, talk a little, and eat 25–50 % of her meals. Without her oxygen, she maintains adequate saturation and her oxygen is discontinued. She has a 5 cm red area on her sacrum, new since admission, which the nurse rates as a stage 1 pressure ulcer.
Prior to admission, Lavern was living on her own, with help from her family for groceries and transportation. She did not engage in specific exercise but was able to walk 100 feet to get her mail every day without an assistive device.
The standard protocol for this unit is for all previously ambulatory patients to undergo brief functional assessment and walk 2 to 3 times daily with a trained escort or family member. Lavern’s daughter requests that her mother remain in bed, use a bedpan or commode, and be allowed to rest to speed her recovery and avoid falls.
FormalPara Case Part 2The physician, nurse, and physical therapist caring for Lavern meet briefly with Lavern and her daughter. They ask Lavern about her goals on leaving the hospital and about her daughter’s concerns. Lavern strongly wishes to return home rather than go to a short-term rehabilitation facility or nursing home. Lavern’s daughter is afraid that exercise right now may cause her mother to relapse and also risks a fall; she sees how shaky her mother is just sitting up in bed. The clinical team presents the risks of immobility in older hospitalized adults and strategies to prevent these consequences. Lavern slowly walks four feet to the bathroom with the physical therapist. Although fatigued, she is game to try again later.
FormalPara Case Part 3By the fourth day of hospitalization, Lavern is able to walk 20 feet with an assistive device and can get to the bathroom in her room on her own. The red area on her sacrum has reduced in size. She is discharged home with physical therapy services for home rehabilitation.
Introduction
Since the time of Hippocrates, clinicians have observed that prolonged immobility results in loss of muscle strength and function. These losses are particularly likely to occur in older adults, who also constitute a disproportionate number of hospital admissions. Many clinicians have trained in care systems in which it is assumed without question that most older adults admitted for elective or emergent reasons will require a subsequent rehabilitation or nursing home stay to regain their baseline function. Yet studies show that interventions can break this cycle of immobility, loss of strength, loss of function, and discharge to higher care settings.
Barriers to implementation of these interventions include: fear of harming the older adult, myth that exercise will interfere with healing, nursing and rehabilitation resources targeted to keeping the patient in bed or wheelchair, and staff lacking training. All of these are amenable to education. This chapter will discuss the consequences of immobility and interventions that are effective for older hospitalized adults.
Prevalence and Consequences of Immobility in the Acute Hospital
In the USA, just under half of all adults admitted to the hospital are 65 years or older. Although individuals 65 years and older were 13 % of the US population in 2008, they generated 35 % of all hospital discharges [1]. These numbers become more pronounced with older cohorts. For example, in 2008, adults 85 and older comprised 1.8 % of the population and 8.0 % of all discharges [1]. The proportion of individuals transferred to long-term care after hospitalization also rises greatly with older cohorts, with 44 % of those 85 years and older going to rehabilitation or nursing home sites of care rather than home after hospitalization [1]. Some of these transitions are due to shortening of hospital length of stays; in 2008, the average length of stay for older adults was 5.5 days, which is longer than the average length of stay for younger adults but shorter than hospital stays in the past [1]. However, functional loss, from immobility during hospitalization, also plays a role.
Immobility during hospitalization adversely affects many organ systems (Table 9.1), with a net result of overall functional loss. For older adults, deconditioning and functional loss begin by day 2 of hospitalization; thus prevention protocols must start at or soon after hospital admission [2, 3]. Studies reveal that declines from baseline function in mobility and self-care are common, whereas early orders for out-of-bed status, physical therapy, or bedside exercises are infrequent [4]. Although bed rest is usually ordered for older hospitalized patients, chart reviews find no medical reason for bed rest in a majority of instances [5].
For those with preexisting functional or cognitive impairments, hospitalization presents additional challenges to maintaining independence and returning home. Older adults using assistive devices such as canes or walkers are more likely to have functional decline during hospitalization than those who do not. It is possible that the need for a device, not readily available on medical or surgical floors, presents a significant barrier to mobility. In addition, nursing staff with less experience with assistive devices may be hesitant to attempt transfers or walking with these patients and may delay orders for out-of-bed status until a physical therapist is available to work with the patient.
Older adults with dementia are more likely to experience substantial loss in instrumental of activities of daily living (IADL) and activities of daily living (ADL) during hospitalization. Regaining lost abilities is related to the severity of cognitive impairment. In addition, dementia is a major independent risk factor for acquiring delirium, or acute confusional state, during hospital admission. Delirium presents a critical obstacle to treating the index illness as well as maintaining mobility and function [6].
Studies of hospitalized older adults find that those who lose IADL and ADL function during a short hospitalization may not recover lost function even after 3 to 6 months of rehabilitation [4]. For some, continued functional decline is likely due to underlying medical conditions. For others, recovery is dependent upon rehabilitation efforts, which vary greatly. For individuals who are unable to tolerate 3 h/day of formal therapy, the home or skilled nursing facility are the usual sites for posthospital rehabilitation rather than a rehabilitation hospital. In the home or skilled nursing facility, older adults usually participate in a single exercise session from a few times weekly to daily. Particularly in institutional settings, staff may perform IADLs and ADLs for the older adult, to save time and reduce fall risk, which perpetuates continued decline in function (see Chap. 8).
Assessing Function in Hospitalized Older Adults
Fortunately, studies demonstrate that interventions can minimize hospital-associated functional decline [7]. A variety of approaches have shown benefit; most of these approaches start with an assessment of the older adult’s preadmission function and risks for functional loss. Independent risk factors for hospital functional loss and nursing home placement include increasing age, low preadmission cognitive status, and low baseline IADL status; thus these factors should be part of an intake assessment for older adults.
Although several instruments are available to assess physical performance in hospitalized older adults, none is considered ideal for all individuals or settings. Because it does not require extensive training, equipment, or time, the Elderly Mobility Scale is particularly useful for measuring physical function in hospitalized ill older adults (Table 9.2) [8]. The scale has been examined in different settings and has good validity and reliability evidence. Key advantages of this scale are its simplicity and brevity: it requires 5–10 min to administer. Another instrument used in hospitals is the Hierarchical Assessment of Balance and Mobility (HABAM) scale, which rates balance (6 possible levels), transfers (8 levels), and mobility (14 levels) [9]. With this additional specificity, the HABAM instrument requires more time and training to use.
Safety of Exercise in the Acute Hospital Setting
To date studies, including pooled data in meta-analyses, have shown no increase in adverse effects, such as falls, injuries, or infections, in older adults engaged in hospital exercise programs [10–12]. No increase in adverse consequences is seen even with high-intensity resistance exercises performed in bed when compared with passive range of motion [13]. In fact, some programs show decreased hospital length of stay and decreased fall risk in the active intervention groups.
Studies have typically excluded older adults with unstable medical conditions as well as those in the intensive care unit (ICU) or receiving palliative care. Some programs exclude older adults who were not ambulatory prior to admission or who have been admitted from a nursing home. Other individuals who need additional review prior to entering a standard hospital mobility program are listed in Table 9.3.
Physical impairment, whether due to deconditioning or to acquiring the motor neuropathy syndrome known as ICU-acquired weakness, is common in adults who survive an ICU stay. Although few in number, randomized controlled studies of rehabilitation in the ICU setting demonstrate the feasibility and safety of physical therapy to improve immediate and long-term function [14, 15]. In this setting, range of motion and bed mobility exercises are often initiated first. For selected patients, sitting exercise, transfers from bed to chair, resistance exercises, and ambulation are employed. Programs have successfully integrated reduced use of heavy sedation with physical and occupational therapy starting within 72 h after intubation. Study results suggest benefits such as shorter ICU stays, earlier return to walking status, and greater likelihood of regaining baseline function.
Preventing Functional Decline with Geriatric Units and Teams
Traditionally hospitals have focused on treating the acute illness or surgical procedure rather than considering the hazards of hospitalization for older adults. Thus clinicians and staff focus on the principle reason for hospitalization—the pneumonia, fracture, myocardial infarction, or cholecystectomy—rather than overall function and independence, which primarily determines quality of life for older adults. Hospital administrators place considerable attention on the most efficient, rapid method to deliver care. Protocols may emphasize prevention of injuries, such as falls, rather than avoiding discharge to higher levels of care. The easiest way to avoid a fall or injury is to not permit mobility; thus many hospital policies actually promote muscle loss, decreased mobility, and loss of function.
Hospital geriatric teams and geriatric geographic units that employ geriatric assessment and individualized patient treatment plans have been extensively studied since the 1980s. Many studies have used rigorous study designs, with more than 22 randomized controlled trials, but have variable target patient groups, assessment instruments, interventions, and outcomes. Despite this heterogeneity, several meta-analyses have found that hospital-based geriatric units and teams are associated with improved function, mortality rates, and likelihood of returning home and reduced likelihood of living in an institution [10, 12]. The number of older patients needed to treat (NNT) for the outcomes of survival and returning home ranges from 17 (home at 6 months after hospitalization) to 33 (home at 12 months after hospitalization) in comparison with usual medical care [10]. Benefits in reduced hospital costs are also seen; studies have not analyzed savings from fewer nursing home stays, which would further decrease costs.
In subgroup analyses comparing teams and geographic units, Ellis and colleagues found that the specialized geriatric units were more effective than mobile geriatric teams, which have variable outcomes [10]. Only 13 (follow-up at 6 months) or 20 (12 months) older adults need to be treated in a geographic geriatric unit to prevent one person from dying or living in an institution [10]. Also, benefits are seen whether admission to the geriatric unit is based solely on age, such as 75 years and older; particular conditions, such as delirium or falls; or perceived needs, such as functional impairment or risk for institutionalization. Thus comprehensive assessment delivered through a dedicated multidisciplinary team working in a geographically distinct unit improves an older adult’s chance to survive hospitalization and return home.
One example of a specialized geriatrics unit is the Acute Care of the Elderly or ACE unit. These programs use geriatric assessment and multidisciplinary teams to deliver acute medical care while targeting interventions to maintain function. ACE units encourage patients to participate in ADLs and promote daily exercise, such as walking in hallways. Multidisciplinary teams conduct daily rounds that focus on function as well as medical concerns. Also, the environment of an ACE unit is designed to enhance mobility: handrails in unobstructed hallways, elevated toilets for easier transfer, and exercise space integrated into the unit.
Additional Hospital-Based Strategies
NICHE
Started in 1990, Nurses Improving Care of Healthsystem Elders (NICHE) is a national program to promote high-quality, evidence-based care of older adults. The project has developed and disseminated assessment tools, best practices, and educational materials for nurses. The most common NICHE strategy for improving the care of hospitalized older adults is the resource nurse model. In this strategy, assigned unit-based nurses acquire expertise in geriatrics best practices and disseminate information and skills to other nurses on the unit. Although this practical model makes sense, it is a more dilute intervention than the mobile geriatrics team and geographic geriatrics unit, and studies to date have not demonstrated consistent functional benefits.
Hospital Environments
Typically, hospital hallways have not been designed for patient ambulation but rather to move beds, equipment, and people as efficiently as possible. Similarly, rooms have not been arranged to facilitate walking to the bathroom or to a chair. IV poles, urinary catheters, and other devices tether patients in place. Bedrails, bed heights left elevated, and a multitude of equipment clutter the average room and environs. Areas suitable for safe walking can be created by adding nonglare lighting, railings, markers for distances walked, and periodic seating for rest stops. In addition, appropriate assistive devices, such as adjustable canes or walkers, can be available on units and patients trained in their use early in the hospital stay, not just on the day of discharge. Patients also need gowns that do not gap open, such as opposing johnny gowns, and nonslip footwear to facilitate mobility.
Standardized Protocols or Order Sets
Orthopedics research has found that early mobilization programs—out of bed or walking on day of surgery—significantly reduces length of stay and improves joint function after hip or knee surgery, without increasing adverse outcomes and with retained patient satisfaction [16]. Borrowing in part from these studies, hospitals have initiated walking programs for older adults.
Walking for Wellness [17] and Project Move [18] are examples of hospital-based programs that provide an overall framework for all older patients. These programs automatically provide a shared initial assessment, patient education, and mobility plans used across a hospital. Some of these programs have demonstrated reduced complications from immobility as well as sustainability as a system-wide intervention. Trained escorts, family members, nurses, and physical therapists are used in these programs. Clarity, ease of operation, and consistency of implementation are essential elements of hospital-wide projects.
Another hospital-wide strategy is to eliminate “bed rest” as a default admission order. When bed rest is ordered as an add-on order, an explanation must be given by the ordering clinician. Analogous to restraint orders, bed rest orders can be allowed for only a short duration before expiration, such as 24 h, and must be reordered to be continued. This strategy has also been used in some ICU settings, in which the computerized order entry system no longer lists bed rest as the default activity level but does list physical and occupational therapist consultation, in automatically generated admission orders.
Ongoing hospital-wide education regarding the importance of patients continuing to perform self-care activities, sitting out of bed, and early mobilization is also recommended by experts. See Tables 9.4 and 9.5 for descriptions of hospital-based exercise interventions and approaches.
Conclusion
Older adults are at particularly high risk for consequences of immobility due to hospitalization. Feared yet common outcomes are loss of physical function, mobility, and discharge to a higher level of care rather than home. Older age and prior cognitive and IADL impairments are associated with greater risk for these outcomes. Traditionally, hospitals have focused on the acute illness more than the hazards of hospitalization experienced by older patients. Yet research in the hospital setting reveals opportunities to prevent deconditioning and loss of function.
The most valuable intervention appears to be the geographic, multidisciplinary geriatrics unit, which may also reduce hospital costs. However, simple walking programs with trained escorts or family members can increase amount of time walking and out of bed greatly and are acceptable to patients and families. Similarly, order sets that default to “out-of-bed” activity status will greatly reduce the time in bed. Although many clinicians accept the cycle of hospitalization, muscle weakness, functional loss, nursing home stay, and rehospitalization as inevitable and indeed this may be true for older adults at highest risks of decline, greater adoption of hospital “best practices” such as ACE units could break this cycle for many hospitalized older adults.
References
Healthcare Cost and Utilization Project (HCUP). Hospital utilization among oldest old; 2008. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb103.jsp. Accessed 16 Mar 2015.
Hirsch CH, Sommers L, Olsen A, et al. The natural history of functional morbidity in hospitalized older adults. J Am Geriatr Soc. 1990;38:1296–303.
Mudge AM, O’Rourke P, Denaro CP. Timing and risk factors for functional changes associated with medical hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2010;65:866–72.
Narain P, Rubenstein LZ, Wieland DG, et al. Predictors of immediate and 6-month outcomes in hospitalized elderly patients. J Am Geriatr Soc. 1998;36:775–83.
Callen BL, Mahoney JE, Grieves CB, et al. Frequency of hallway ambulation by hospitalized older adults on medical units of an academic hospital. Geriatr Nurs. 2004;25:212–7.
Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52(8):1263–70.
Siebens H, Aronow H, Edwards D, et al. A randomized controlled trial of exercise to improve outcomes of acute hospitalization in older adults. J Am Geriatr Soc. 2000;48:1545–52.
Nolan JS, Remilton LE, Green MM. The reliability and validity of the Elderly Mobility Scale in the acute hospital setting. Internet J Allied Health Sci Pract. 2008; 6(4):1–7.
Rockwood K, Rockwood MRH, Andrew MK, et al. Reliability of the hierarchical assessment of balance and mobility in frail older adults. J Am Geriatr Soc. 2008;56(7):1213–7.
Ellis G, Whitehead MA, Robinson D, et al. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553.
Kosse NM, Dutmer AL, Dasenbrock L, Bauer JM, Lamoth CJ. Effectiveness and feasibility of early physical rehabilitation programs for geriatric hospitalized patients: a systematic review. BMC Geriatr. 2013;13:107.
de Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;(1):CD005955.
Mallery LH, MacDonald EA, Hubley-Kozey CL, Earl ME, Rockwood K, MacKnight C. The feasibility of performing resistance exercise with acutely ill hospitalized older adults. BMC Geriatr. 2003;3:3.
Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300:1685–90.
Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–82.
Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil. 2014;1–11.
Tucker D, Molsberger SC, Clark A. Walking for wellness: a collaborative program to maintain mobility in hospitalized older adults. Geriatr Nurs. 2004;25(4):242–5.
Markey DW, Brown RJ. An interdisciplinary approach to addressing patient activity and mobility in the medical-surgical patient. J Nurs Care Qual. 2002;16(4):1–12.
Resources
Hospital Elder Life Program (HELP) program to reduce delirium in hospitalized older adults, which prevents functional loss. http://www.hospitalelderlifeprogram.org/. Accessed 9 Dec 2014.
Kleinpell RM, Fletcher K, Jennings BM. Reducing functional decline in hospitalized elders, in patient safety and quality: an evidence-based handbook for nurses, Chap. 11. Hughes RG, editor. Rockville: Agency for Healthcare Research and Quality; 2008. http://www.ncbi.nlm.nih.gov/books/NBK2629/. Accessed 9 Dec 2014.
Nurses Improving Care for Healthsystem Elders (NICHE) Try This® series of assessment tools, http://hartfordign.org/practice/try_this/ For reducing hospital functional decline, http://consultgerirn.org/uploads/File/trythis/try_this_31.pdf. Accessed 9 Dec 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sullivan, G.M. (2015). Exercise for Hospitalized Older Adults. In: Sullivan, G., Pomidor, A. (eds) Exercise for Aging Adults. Springer, Cham. https://doi.org/10.1007/978-3-319-16095-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-16095-5_9
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16094-8
Online ISBN: 978-3-319-16095-5
eBook Packages: MedicineMedicine (R0)