Abstract
Acute cholecystitis (AC) is one of the most common causes of emergency admissions to a general surgery service. Although early laparoscopic cholecystectomy (LC) is considered the appropriate treatment for patients with AC, the procedure can be associated with significant morbidity and mortality in high-risk patients [1–3]. High-risk surgical patients, such as the elderly and those with cardiopulmonary comorbidities have pathological changes in their organ systems resulting in increased morbidity and mortality such as myocardial infarction, congestive cardiac failure, stroke, pneumonia or atelectasis [4]. Additionally, the exposure of such high-risk patients to the pneumoperitoneum of a LC can further lead to cardiopulmonary and renal dysfunction [4]. Due to these observations, less invasive or “damage control” techniques have emerged for AC. These techniques attempt to foster temporary and sometimes permanent disease management of AC. The following discussion addresses some of these techniques.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Laparoscopic Cholecystectomy
- Cystic Duct
- Acute Cholecystitis
- Early Laparoscopic Cholecystectomy
- Bile Peritonitis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Acute cholecystitis (AC) is one of the most common causes of emergency admissions to a general surgery service. Although early laparoscopic cholecystectomy (LC) is considered the appropriate treatment for patients with AC, the procedure can be associated with significant morbidity and mortality in high-risk patients [1–3]. High-risk surgical patients, such as the elderly and those with cardiopulmonary comorbidities have pathological changes in their organ systems resulting in increased morbidity and mortality such as myocardial infarction, congestive cardiac failure, stroke, pneumonia or atelectasis [4]. Additionally, the exposure of such high-risk patients to the pneumoperitoneum of a LC can further lead to cardiopulmonary and renal dysfunction [4]. Due to these observations, less invasive or “damage control” techniques have emerged for AC. These techniques attempt to foster temporary and sometimes permanent disease management of AC. The following discussion addresses some of these techniques.
Gallbladder Drainage
Percutaneous transhepatic gallbladder drainage (PTGBD) (also known as a percutaneous cholecystostomy tube placement) is considered a safe alternative to early cholecystectomy in high-risk patients with AC. While PTGBD has been performed since the 1970s [5] and remains the most widely established technique, there are several alternatives that have been explored in the past two decades. Percutaneous transhepatic gallbladder aspiration (PTGBA) is an alternative method where the gallbladder is puncture-aspirated without placing a drainage catheter. Next, endoscopic transpapillary gallbladder drainage (ENGBD) and endoscopic transpapillary gallbladder stenting (ENGBS) are endoscopic alternatives via the traditional transpapillary route. Finally, with recent improvements in endoscopic ultrasound (EUS), EUS-guided gallbladder drainage has been described via the antrum of the stomach or the bulb of the duodenum [6]. Advantages and disadvantages of each technique are listed in Table 12.1. While PTGBD remains the standard of care, these alternatives continue to be explored and should be considered in select patient populations.
Percutaneous Transhepatic Gallbladder Drainage
PTGBD is the most common method for nonoperative gallbladder drainage. The procedure is an interventional radiologic procedure designed to decompress the acutely inflamed gallbladder. Its use has been described in both high-risk surgical patients unresponsive to medical therapy and as first line treatment to delay cholecystectomy [7–9].
Various methods have been described for PTGBD, but the most common is ultrasound-guided transhepatic gallbladder puncture. This procedure is accomplished with minimal anesthesia and generally an 18-gauge needle for drainage. Gallbladder puncture is performed under direct ultrasound guidance to avoid injury to adjacent structures. A 6- to 10-Fr pigtail catheter is then placed in the gallbladder, using a guidewire under fluoroscopy (Seldinger technique) (Fig. 12.1) [6]. Technical and clinical response rates to PTGBD have been reported between 56 and 94 % [9–11], with consistently higher success being documented in more recent studies. The primary advantage of PTGBD in high-risk surgical patients is the avoidance of general anesthesia and those associated cardiovascular risks. That being said, up to 16 % of patients experience complications, including bile peritonitis, bleeding, catheter dislodgement and pneumothorax. In addition, PTGBD may be inappropriate for patients with massive ascites or coagulopathy, and patient discomfort from the catheter has been postulated to decrease quality of life [7, 8, 12, 13].
Percutaneous transhepatic gallbladder drainage (PTGBD) technique. Figures from Tsuyuguchi et al. [27]
There are no randomized controlled trials that directly compare the outcomes of PTGBD to LC [10] although the morbidity [1, 2, 10, 14], mortality [2, 10, 14] among high-risk surgical patients undergoing LC is well documented. Success rates for PTGBD are fairly high, and the mortality related to the procedure (0.36 %) is fairly low, but the overall mortality rate following PTGBD (15.4 %) appears equal to or higher than that for emergency LC (4.5 %) [10]. However, the limitations of the literature preclude absolute conclusions to be made regarding the comparative advantages of this procedure.
There are two randomized controlled trials comparing PTGBD with conservative management. In 2002, Hatzidakis et al. found no difference in resolution of symptoms or overall mortality when comparing PTGBD to nonoperative management in high-risk surgical patients. These authors concluded that the nonoperative treatment should be attempted first, and PTGBD should be reserved for those unresponsive to initial medical management [8]. In a later study, Akyürek et al. compared PTGBD with early LC to medical management with delayed LC in high-risk surgical patients [7]. While the conversion to open cholecystectomy and complication rates were similar in both groups, the study did show a shorter hospital stay and lower overall cost in the group treated with PTGBD and early LC. Thus the authors advocate for percutaneous drainage in high-risk surgical patients over medical management [7].
As previously stated, there is no randomized controlled trial comparing PTGBD to emergency LC in high-risk patients. With the advances in surgical laparoscopic training, intensive care management and perioperative anesthesia, the outcomes of PTGBD and LC may be more similar than one thinks. To this end, the CHOCOLATE trial is an ongoing randomized controlled trial comparing morbidity and mortality between LC and PTGBD in high-risk surgical patients [15].
Percutaneous Transhepatic Gallbladder Aspiration
Percutaneous transhepatic gallbladder aspiration is a method to aspirate the gallbladder with a small-gauge needle under ultrasonographic guidance (Fig. 12.2) [6]. It is an easy, low-cost, bedside-applicable procedure, without the patient discomfort seen with an indwelling catheter (PTGBD).
Percutaneous transhepatic gallbladder aspiration (PTGBA) technique. Figures from Tsuyuguchi et al. [27]
Fundamentally, PTGBA should not work in the setting of infection by the principle of all infections needing continuous drainage. However, infection is not the inciting factor in AC, with obstruction of the cystic duct causing increased intraluminal pressure, leading to venous congestion, compromised blood supply and impaired lymphatic drainage. The mucosa becomes ischemic and releases inflammatory mediators causing trauma, edema, ulcers and possible wall necrosis. Secondary bacterial infection can then occur from the initial obstruction and activation of the inflammatory cascade. Secondary infections complicate up to 50 % of clinical courses, as 40–50 % of cases have been shown to have positive bile cultures [16].
This idea corresponds to Chopra et al., who documented a lower clinical response rate to PTGBA in patients with positive bile cultures [17]. Since infection may not always be present, continuous drainage could be considered excessive treatment in some patients. One time aspiration of bile from the obstructed gallbladder removes the irritant luminal contents and reduces the intraluminal pressure, thereby providing relief prior to the onset of infection. Further studies have concomitantly used antibiotic irrigation during aspiration to counteract any infection that may be present; however, the effectiveness of this technique is unclear due to limited data [18]. In comparing PTGBA to PTGBD, Chopra et al. argues that PTGBA should be the procedure of initial choice as the technical (97–100 % [17, 18]) and clinical (71–77 % [17, 18]) response rates are remarkably high, thus PTGBD should be saved as a salvage procedure for those failing to respond to a single PTGBA. Using this method, 77 % of patients in this study avoided PTGBD [17]. Tsutsui et al. advocate for repetitive PTGBA in patients that fail to initially improve, arguing that the vast majority of patients will respond within two PTGBAs, avoiding placement of an indwelling catheter [18].
The incidence of adverse events for PTGBA is lower (0–4 %) than in PTGBD, and no serious adverse events have been reported [19]. Instances may exist when PTFBD is favorable to gallbladder aspiration. These situations include patients with thick bile or pus that is difficult to aspirate or patients with a large amount of bile that requires continuous drainage for infection source control. In such patients, PTGBD has a greater chance of success because of the larger caliber of the catheter and the potential for repeated irrigation. Also, because it does not provide continuous drainage, PTGBA is inappropriate in patients in whom the indication for gallbladder drainage is to provide relief from a distal biliary obstruction, such as in biliary malignancies [17].
Despite its potential advantages, PTGBA has not been widely adopted as a standard treatment modality because AC is commonly thought to require continuous drainage and the data supportive of PTGBA is limited to case series and retrospective reviews.
Endoscopic Transpapillary Gallbladder Drainage and Stenting (ENGBD and ENGBS)
ENGBD involves placement of a nasobiliary drainage tube and generally does not require biliary sphincterotomy. After successful bile duct cannulation, a guidewire is advanced into the cystic duct and subsequently into the gallbladder. A 5–8.5Fr pigtail nasobiliary drainage tube catheter is then placed into the gallbladder (Fig. 12.3) [6]. It has been reported in patients with specific comorbidities, including end-stage liver disease or coagulopathy where transhepatic techniques are contraindicated.
Endoscopic transpapillary gallbladder drainage (ENGBD) technique. Figures from Itoi et al. [28]
In ENGBS, the procedure is identical to ENGBD, but a 6–10-Fr diameter double-pigtail stent is placed instead of a nasobiliary drainage tube (Fig. 12.4) [6]. When larger diameter stents are placed (i.e., 10F), a sphincterotomy is performed to prevent post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis [19]. Also, unlike ENGBD, stents cannot be irrigated to prevent occlusion by blood or debris, which is a potential cause for concern over time [19].
Endoscopic transpapillary gallbladder stenting (ENGBS) technique. Figures from Tsuyuguchi et al. [6]
While supportive data are limited, a meta-analysis of ENGBD and ENGBS by Itoi et al. demonstrated a technical success rate of 81 % and 96 % and a clinical response rate of 75 % and 88 % respectively [19]. These early results are comparable to the success rates of the more established approaches of PTGBD and PTGBA [19]. This meta-analysis also found the incidence of adverse events to be similar to that of PTGBD (0–16 %). It is important to note that LC can be performed following resolution of the acute inflammation and sepsis. The tube or stent can then be removed preoperatively or intraoperatively when the time comes [19].
Both ENGBD and ENGBS require difficult endoscopic techniques and only case series have been conducted at a limited number of institutions [6]. Both methods have not yet been established as a standard of care. Therefore, while results are promising, these are newer options for a specific patient population, and should currently only be performed in high-volume institutes by skilled endoscopists [6].
Endoscopic Ultrasound-Guided Transmural Gallbladder Drainage (EUS-GBD)
Although endoscopic ultrasound (EUS)-guided drainage procedures have been safely used with peripancreatic fluids, including those from pancreatic pseudocysts and pancreatic, subphrenic and splenic abscess, little is known regarding EUS-guided transmural gallbladder drainage (GBD) for high-risk patients with AC [20].
The endoscopic approach describes the initial puncture being made at the prepyloric antrum of the stomach or the bulb of the duodenum with a 19-gauge needle to access the gallbladder body or neck and avoid visible vessels. From there, bile is aspirated and sent for culture. A guidewire is passed through the needle and coiled into the gallbladder. After removal of the needle, the tract is dilated using a 6–7Fr bougie. A 5Fr nasobiliary drainage tube or stent is subsequently placed [3] (Fig. 12.5) [6].
Endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) technique. Figures from Tsuyuguchi et al. [6]
Endoscopic ultrasound-guided transmural gallbladder drainage is particularly useful in patients with large amounts of perihepatic ascites who, therefore, cannot undergo PTGBD. In addition, it is useful and safe for patients with coagulopathy and for those taking antiplatelet or antithrombotic medication. As previously mentioned, the EUS-GBD puncture site is at the prepyloric antrum or duodenal bulb, both of which are less vascularized than the direct puncture through the liver compared to PTGBD. Furthermore, there is less discomfort with EUS-GBD than with PTGBD, primarily because the PTGBD puncture site is in the subcostal area of the right flank, an area very sensitive to pain [3].
The development of the linear echoendoscope has led to transmural entry and drainage of pancreatic fluid, and this is now regarded as the method of choice. More recently, the transmural approach has been reported to be successful in internal bile drainage of the gallbladder [3, 20]. The EUS-guided transmural approach to the gallbladder for bile aspiration raises concerns regarding the development of bile peritonitis. Theoretically, the gallbladder does not have adhesions to the gastrointestinal tract, raising the possibility of bile leakage during the procedure causing bile peritonitis. However, this has rarely been reported [21], suggesting that the inflamed gallbladder wall may have adhered to adjacent structures, preventing leakage through the puncture site.
The transmural approach has several potential advantages in comparison to the transpapillary approach, including the avoidance of cannulation-related pancreatitis and it is not limited by the configuration of the cystic duct. It also has several potential advantages compared with the percutaneous approach, including the avoidance of complications such as hematoma and pneumothorax and the ability to perform the transmural approach in patients with perihepatic ascites [20]. All this being said, there are disadvantages to EUS-GBD including bile peritonitis [21], pneumoperitoneum [22], stent migration into the gallbladder or intraabdominal space, puncture-induced hemorrhage, stent occlusion and inadvertent tube removal [6].
With regards to bile peritonitis, Jang et al. [22] address the issue by discussing the higher likelihood of bile peritonitis with a plastic stent than a metal stent. The authors argue that the insertion of a plastic stent requires a fistula tract of diameter larger than, or at least equal to, the diameter of the inserted stent. Because of expandability, a metal stent can seal the gap between the stent and fistula of the gallbladder wall better than a plastic stent, thus preventing bile leakage. While one report of bile peritonitis has occurred with a plastic stent [21], few studies [20–23] with small sample sizes have examined this issue making it difficult to say definitively if metal stents are overall safer in preventing bile leakage during this procedure.
Additionally, it is important to note that the pneumoperitoneum reported in these studies is self-limiting, resolving almost immediately following the procedure [3]. The pneumoperitoneum typically occurs during dilation; the use of carbon dioxide for insufflation during the procedure may lead to the rapid resolution of the pneumoperitoneum and relief of pain [3].
All this being said, EUS-GBD is not a well-established technique. Therefore, it should be performed in high-volume institutes by skilled endoscopists and further prospective evaluations are needed [6].
Intraoperative Damage Control
Acute cholecystitis can make LC difficult with the increased potential for morbidity. If the surgeon deems intraoperatively that a LC cannot be performed safely, several intraoperative damage control techniques should be considered. Some authors have advocated conversion to an open cholecystectomy if the “critical view” cannot be obtained during the dissection of Calot’s triangle [24]. This approach has multiple drawbacks. The increased operative time for the open procedure and the more painful incision can harbor its own degree of morbidity. Also, sometimes an open approach does not always provide a better view of the anatomy [24] and an open damage control procedure may be needed. Finally, due to the rarity of the open procedure nowadays, some surgeons may have difficulty with this technique due to a lack of experience.
If dissection is deemed impossible during laparoscopic cholecystectomy, raising concerns of doing more harm than good with further dissection, a laparoscopic cholecystostomy tube should be considered. This procedure involves placing a purse string suture on the dome of the gallbladder. This is utilized to secure a 14–16 French Malekot tube in the gallbladder for drainage following the suctioning of as much bile and stones as possible.
In less complicated cases, there are various maneuvers to consider to facilitate the dissection of the gallbladder. The actual maneuver often depends on the situation creating the difficulty in the operation. In some cases, the difficulty is due to a thick rind around the gallbladder. Incising the rind and dissecting it away from the gallbladder will occasionally leave a soft gallbladder whose cholecystectomy can proceed in a standard fashion.
Sometimes the gallbladder can be too thick-walled to grasp and simple aspiration does little to improve the retraction. In this instance, creating a hole, at least 1–2 cm high on the gallbladder away from the primary structures can allow decompression. This hole may also be used to milk a large stone out of the gallbladder and enhance retraction. In situations where the gallbladder is unable to be grasped because the entire gallbladder lumen has been replaced with stones, a similar hole in the gallbladder can be made and the stones retrieved with a large stone grasper through the subxiphoid 10 mm port. In the authors’ experience, sometimes up to 200 stones of varying sizes can be present in the gallbladder that requires many passes with the large stone grasper for full stone removal (Fig. 12.6). Remarkably in some cases, after removal of a large stone or multiple smaller stones, the dissection in Calot’s triangle can become fairly routine as the capability for retraction improves. After creating a hole in the gallbladder for stone retrieval, the retracting surgeon can close the hole by grasping both sides of the hole with a endoscopic grasper to close the defect. If the gallbladder wall is extremely thick, the assistant can actually grasp the wall of the cholecystostomy to intensify the pull of the retraction.
In instances where the dissection in Calot’s triangle is fraught with too much bleeding and suboptimal visualization, dissection in other areas of the gallbladder can create more mobility to facilitate the dissection. In this case, full division of the medial and lateral peritoneal surfaces the entire length of the gallbladder may be invaluable. This maneuver allows full mobilization of the gallbladder and with effective traction may allow careful dissection inferiorly towards Calot’s triangle.
A commonly taught dictum is that the gallbladder should be dissected “from the top down” when the inflammation is too intense in Calot’s triangle. However, the better strategy is to dissect “from the middle down.” This strategy allows the top of the gallbladder to stay fixed on the liver bed to give counter traction and prevent the situation where a floppy gallbladder is difficult to grasp. Dissecting from the middle down is performed by slowly dissecting each side of the gallbladder safely above the critical structures with increased depth behind the gallbladder until a window exists behind the gallbladder anterior to the liver bed. For this maneuver to be done properly, the gallbladder is not to be entered on the side of the liver bed and the dissection must not be performed too deeply to create a liver injury. After this window is created, the surgeon can then cautiously dissect toward the neck of the gallbladder and the cystic duct. This maneuver can allow the gallbladder to be stretched and allow lengthening of the fundus and cystic duct to ensure proper visualization of the critical structures. After the cystic duct is visualized, the operation can proceed in the conventional manner.
In other cases, the gallbladder can only be isolated at the level of the infundibulum or cystic duct-gallbladder junction. The skilled laparoscopic surgeon can suture the structure closed. However, this maneuver may not always be possible as sometimes the tissues are too friable. The surgeon can then attempt to divide the gallbladder at the level of the infundibulum. Since this area is generally too large for the standard 5 or 10 mm surgical endoclips, the surgeon needs to use an Endo GIA Universal Stapler (Covidien, Dublin, Ireland) or an Endoloop (Ethicon Endo-Surgery, Blue Ash, Ohio). In these cases, we would recommend placement of a Jackson Pratt drain (10Fr) to capture and identify any potential biliary leak. When bile is noted in the drain effluent, a low threshold should be given to investigate for a biliary leak by a hepatobiliary iminodiacetic acid (HIDA) scan or imaging study. Early detection of a biliary leak generally decreases the patient morbidity as the gastroenterology service can then perform an endoscopic retrograde cholangiopancreatography (ERCP) with biliary ductal decompression and stenting. In some cases the cystic duct stump breakdown is due to a retained stone. In this scenario, the ERCP can also be accompanied by stone retrieval.
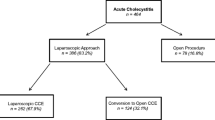
A final laparoscopic option is a laparoscopic partial (or “subtotal”) cholecystectomy (LPC) and employs the principles of damage control surgery [24, 25]. The indication for a LPC is that safe standard surgery is not possible laparoscopically and the patient will not receive better treatment for the disease process with open surgery. In some cases, the patient is a poor candidate for open surgery or the anticipated extra time or blood loss needed for the successful laparoscopic surgery is detrimental (Fig. 12.7). Factors warranting LPC can include severe congestion, edema and adhesions at Calot’s triangle, tenacious fibrosis at Calot’s triangle or severe bleeding upon performing any aspect of the operative dissection. Situations where bleeding during LC can become prominent include intense inflammation in Calot’s triangle, dense adherence of the gallbladder or posterior rind to the liver bed, and an operative field complicated by portal hypertension. A LPC is sometimes chosen preemptively to avoid a major injury such as right hepatic artery or bile duct injury while trying to dissect in a bleeding field with poor visualization of the important structures in a LC.
The LPC technique is relatively straightforward. Optimally, as much gallbladder as possible is removed and closure of the stump or cystic duct is performed. However, in many cases where LPC is needed, adequate dissection to visualize enough cystic duct length to facilitate a secure closure is not possible [24, 25]. In LPC, a common strategy includes stapling of the gallbladder neck near the cystic duct, as previously described. Another common strategy entails leaving a portion of the gallbladder wall behind in situ on the liver bed to minimize the severe bleeding that may be encountered when trying to separate the gallbladder from the liver bed. When a portion of the gallbladder is left on the liver bed, attempts should be made to cauterize as much residual gall bladder mucosa as possible. Regardless of the individual characteristics of the technique, current reviews document that LPC is feasible in approximately 90 % of patients undergoing a difficult resection [24].
Importantly, a LPC does not eliminate all of the potential complications that could occur with a LC. In a recent meta-analysis [24], the most common complication of a LPC was postoperative bile leak, which occurred in 10.6 % of patients. Additional complications included recurrent symptoms of gallstones (2.2 %), immediate reoperation (2.7 %), and the need for postoperative ERCP (7.5 %) or postoperative percutaneous interventions (1.4 %). Further analysis revealed that fewer bile leaks, less need for ERCP, and less recurrent symptoms of gallstones seemed to occur when the cystic duct and gallbladder remnant were closed. These data support a low threshold for postoperative ERCP with biliary decompression in cases of LPC and cautious inspection of a patient’s physical examination, clinical status, and laboratory parameters prior to a potentially premature discharge.
Summary
Early cholecystectomy is the treatment of choice for acute calculous or acalculous cholecystitis. For acutely sick patients or chronically ill patients who could benefit from medical optimization, initial nonoperative treatment should be attempted. For those in whom the risk of surgery remains high despite optimization, PTGBD with or without stenting remains the standard of care for nonoperative gallbladder drainage. Patients with moderate ascites, coagulopathy or aberrant anatomy may be better served using an endoscopic approach by skilled endoscopists. Laparoscopic partial cholecystectomy should be reserved as an intraoperative damage control option along with open cholecystectomy and drainage. Overall, the treatment of AC in high-risk patients remains controversial with many therapeutic options [26]. Better studies are needed to aid the physician in management decisions.
References
Brunt LM, Quasebarth MA, Dunnegan DL, Soper NJ. Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc. 2001;15(7):700–5.
Kirshtein B, Bayme M, Bolotin A, Mizrahi S, Lantsberg L. Laparoscopic cholecystectomy for acute cholecystitis in the elderly: is it safe? Surg Laparosc Endosc Percutan Tech. 2008;18(4):334–9.
Jang JW, Lee SS, Song TJ, Hyun YS, Park do H, Seo DW, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142(4):805–11.
Gurusamy KS, Rossi M, Davidson BR. Percutaneous cholecystostomy for high-risk surgical patients with acute calculous cholecystitis. Cochrane Database Syst Rev. 2013;8, CD007088.
Elyaderani M, Gabrielle O. Percutaneous cholecystostomy and cholangiography in patients with obstructive jaundice. Radiology. 1979;130(3):601–2.
Tsuyuguchi T, Itoi T, Takada T, Strasberg SM, Pitt HA, Kim MH, et al. TG13 indications and techniques for gallbladder drainage in acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20(1):81–8.
Akyürek N, Salman B, Yüksel O, Tezcaner T, Irkorucu O, Yucel C, et al. Management of acute calculous cholecystitis in high-risk patients: percutaneous cholecystotomy followed by early laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2005;15(6):315–20.
Hatzidakis AA, Prassopoulos P, Petinarakis I, Sanidas E, Chrysos E, Chalkiadakis G, et al. Acute cholecystitis in high-risk patients: percutaneous cholecystostomy vs conservative treatment. Eur Radiol. 2002;12(7):1778–84.
Teoh WMK, Cade RJ, Banting SW, Mackay S, Hassen AS. Percutaneous cholecystostomy in the management of acute cholecystitis. ANZ J Surg. 2005;75(6):396–8.
Winbladh A, Gullstrand P, Svanvik J, Sandström P. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB. 2009;11(3):183–93.
Lee MJ, Saini S, Brink JA, Hahn PF, Simeone JF, Morrison MC, et al. Treatment of critically ill patients with sepsis of unknown cause: value of percutaneous cholecystostomy. Am J Roentgenol. 1991;156(6):1163–6.
Hsieh YC, Chen CK, Su CW, Chan CC, Huo TI, Liu CJ, et al. Outcome after percutaneous cholecystostomy for acute cholecystitis: a single-center experience. J Gastrointest Surg. 2012;16(10):1860–8.
Cherng N, Witkowski ET, Sneider EB, Wiseman JT, Lewis J, Litwin DE, et al. Use of cholecystostomy tubes in the management of patients with primary diagnosis of acute cholecystitis. J Am Coll Surg. 2012;214(2):196–201.
Bingener J, Richards ML, Schwesinger WH, Strodel WE, Sirinek KR. Laparoscopic cholecystectomy for elderly patients: gold standard for golden years? Arch Surg. 2003;138(5):531–5.
Kortram K, van Ramshorst B, Bollen TL, Besselink MG, Gouma DJ, Karsten T, et al. Acute cholecystitis in high risk surgical patients: percutaneous cholecystostomy versus laparoscopic cholecystectomy (CHOCOLATE trial): study protocol for a randomized controlled trial. Trials. 2012;13:7.
Elwood DR. Cholecystitis. Surg Clin North Am. 2008;88(6):1241–52.
Chopra S, Dodd GD, Mumbower AL, Chintapalli KN, Schwesinger WH, Sirinek KR, et al. Treatment of acute cholecystitis in non-critically ill patients at high surgical risk: comparison of clinical outcomes after gallbladder aspiration and after percutaneous cholecystostomy. Am J Roentgenol. 2001;176(4):1025–31.
Tsutsui K, Uchida N, Hirabayashi S, Kamada H, Ono M, Ogawa M, et al. Usefulness of single and repetitive percutaneous transhepatic gallbladder aspiration for the treatment of acute cholecystitis. J Gastroenterol. 2007;42(7):583–8.
Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71(6):1038–45.
Lee SS, Park DH, Hwang CY, Ahn CS, Lee TY, Seo DW, et al. EUS-guided transmural cholecystostomy as rescue management for acute cholecystitis in elderly or high-risk patients: a prospective feasibility study. Gastrointest Endosc. 2007;66(5):1008–12.
Song TJ, Park do H, Eum JB, Moon SH, Lee SS, Seo DW, et al. EUS-guided cholecystoenterostomy with single-step placement of a 7F double-pigtail plastic stent in patients who are unsuitable for cholecystectomy: a pilot study (with video). Gastrointest Endosc. 2010;71(3):634–40.
Jang JW, Lee SS, Park DH, Seo DW, Lee SK, Kim MH. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011;74(1):176–81.
Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder: implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65(4):735–7.
Henneman D, Costa DW, Vrouenraets BC, Wagensveld BA, Lagarde SM. Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review. Surg Endosc. 2012;27(2):351–8.
Ji W, Li LT, Li JS. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int. 2006;5(4):584–9.
Eachempati SR, Cocanour CS, Dultz LA, Phatak UR, Albarado R, Todd SR. Acute cholecystitis in the sick patient. Curr Probl Surg. 2014;51(11):441–66.
Tsuyuguchi T, Takada T, Kawarada Y, Nimura Y, Wada K, Nagino M, et al. Techniques of biliary drainage for acute cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg. 2007;14(1):46–51.
Itoi T, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Ishii K, et al. Endoscopic transpapillary gallbladder drainage in patients with acute cholecystitis in whom percutaneous transhepatic approach is contraindicated or anatomically impossible (with video). Gastrointest Endosc. 2008;68(3):455–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Dultz, L.A., Todd, S.R., Eachempati, S.R. (2015). Damage Control Techniques in Acute Cholecystitis. In: Eachempati, S., Reed, II, R. (eds) Acute Cholecystitis. Springer, Cham. https://doi.org/10.1007/978-3-319-14824-3_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-14824-3_12
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14823-6
Online ISBN: 978-3-319-14824-3
eBook Packages: MedicineMedicine (R0)