Abstract
The hall of periodontal surgical procedures has been constantly amplified since the mid-1950s by the development of techniques, biomaterials and the knowledge retrieved by basic/clinical research acquired, in order to combine the advantages of function’s reestablishment with improvement of aesthetics. A single search of the National Centre for Biotechnology Information, US National Library of Medicine database (PubMed) using the terms “periodontal surgery” (http://www.ncbi.nlm.nih.gov/pubmed/?term=periodontal+surgery) provides access to more than 14,000 publications. Such a huge amount of references regards to all types of study designs; all of them presented together and without ranking the quality of information. As a result, the decision-making process may be jeopardized when low-quality data are erroneously used to guide a treatment plan.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Evidence-based Decision-making Process
- Periodontal Surgery
- Medicine Database
- Single Search
- Gingival Recession
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1.1 Defining the Concepts: Evidence-Based Dentistry and Its Application to Periodontology and Periodontal Plastic Surgery
The hall of periodontal surgical procedures has been constantly amplified since the mid-1950s by the development of techniques, biomaterials and the knowledge retrieved by basic/clinical research acquired, in order to combine the advantages of function’s reestablishment with improvement of aesthetics. A single search of the National Centre for Biotechnology Information, US National Library of Medicine database (PubMed) using the terms “periodontal surgery” (http://www.ncbi.nlm.nih.gov/pubmed/?term=periodontal+surgery) provides access to more than 14,000 publications. Such a huge amount of references regards to all types of study designs; all of them presented together and without ranking the quality of information. As a result, the decision-making process may be jeopardized when low-quality data are erroneously used to guide a treatment plan.
Since the middle 1990s, periodontology has been moving its “eyes” to “evidence-based approaches: the search of treatment options sustained by the highest quality findings of the evidence available, the patient’s oral and medical condition and history, with the dentist’s clinical expertise and the patient’s treatment needs and preferences [1–4] (Fig. 1.1). Nowadays, evidence-based periodontology represents the most confident source of information for clinical decision-making (i.e. the selection of a treatment option instead of another) and for the search of alternative/novel therapies alike [3–10]. The employment of these criteria can identify and assess the entire base of evidence in a comprehensive manner, in order to respond a focused and relevant clinical question. For most of the diseases and conditions, more than a single procedure is available for use. Consequently, clinician may choose the best option for each patient individually, based on the expected results, potential complications/adverse effects, acceptance of the selected treatment by the patient and costs. Overall, the selection of “gold standard” procedures is the main focus of patients and professionals.
One of the most important characteristics of evidence-based decision-making regards to the translation of the results of research to conventional clinical practice. Apparently, this does not seem to represent a difficult task; however, it is dependent of a critical appraisal of what different (many times a bunch of) studies have identified as clinically relevant for use and the meticulous handling of these information.
An “evidence-based periodontology” now concentrates its efforts in asking about the known and unknown information of interest, finding and appraising the best sources of evidence and examining and adjusting such outcomes for clinical practice in order to provide the best treatment options to patients’ needs [10]. The main tools used to achieve such purpose (systematic reviews [SR] and meta-analysis studies) have been growing in popularity because they may provide standardized, precise, consistent and qualified data combination of several quality-assured individual studies [1]. For instance, clinicians may search for the evidence in case reports, case series and randomized clinical trials and arbitrarily give the same “weight” (relevance) to them all (Fig. 1.2). The purpose of an evidence-based decision-making is to truly provide the directions to be followed when considering different options of treatment by allowing the clinicians to draw trustworthy conclusions based on the “scientific truth” and the ways to apply it in their practices [1, 3].
Level of validity and confidence of outcomes according to study type [1]
Based on that, “evidence-based periodontal plastic surgery” was defined as “the systematic assessment of clinically relevant scientific evidence designed to explore the aesthetic and functional effects of treatment of defects of the gingiva, alveolar mucosa and bone, based on clinician’s knowledge and patient-centred outcomes, such as perception of aesthetic conditions, functional limitations, discomfort, root sensitivity, level of sociability after surgery and preferences” [8–11]. Consequently, the primary argument to creating a background to judge and improve the quality of treatment with periodontal and peri-implant plastic surgery procedures should be the identification of the appropriate base of evidence for each respective therapy.
1.2 Evidence-Based Decision-Making: “Why Should I Base My Treatment Plan on Evidence-Based Clinical Approaches?”
The implication of truly basing a treatment plan on evidence-based clinical approaches for health promotion relies in the use of a structured sequence of criteria in the retrieval and extraction of the best source of information available for a condition or disease [10]. These steps regularly followed by high-quality systematic reviews (SRs) and overviews (i.e. reviews of SRs) undoubtedly search to convert the information of efficacy research to clinical effectiveness; that is the translation of the results achieved at university research to conventional daily practice.
It is important to consider that SRs are planned to recognize, appraise and combine information from clinical trials to provide evidence-based responses and alternatives to clinical research problems [1, 3–11]. Queries linked to development of the clinical decision-making process, estimation of the value of treatment modalities and assessment of disparities in daily practice motivate clinicians to “read” an SR. Thus, these issues can provide important scientific basis of information for clinicians since they identify current knowledge (i.e. what is known and unknown) [1, 3–11].
On the other hand, some obstacles related to the best ways of interpreting the findings of these review studies may be transposed. Most of the clinicians are not trained on how to critically manage the group of findings of an SR neither to identify the central points that could not have been adequately reported in the publication. Consequently, a noticeable difficulty in interpreting their outcomes strengthens the condition that an SR has to report as maximum as possible (and in a transparent manner) the main criteria employed in the preparation of its research protocol. As such, it will provide the clinicians and experts that will read it the capacity to understand and distinguish what has been reported [1]. Based on that, the translation of research findings to clinical practice (by the critical assessment of the evidence available) will be able to guide the decision-making process.
1.3 Systematic Reviews: “Why Are They Useful?” and “Should They Limit My Practice?”
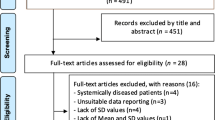
In general, systematic reviews base their result in five stages (Fig. 1.3) [1, 3, 8]:
-
1.
Definition of a clear question (i.e. establishment of a focused question based on the PICO/PECO criteria)
-
2.
Definition of inclusion and exclusion criteria
-
3.
Search for the information of relevance
-
4.
Extraction and critical assessment of the information
-
5.
Systematic/logical data pooling
-
6.
Reporting of conclusions based on the summary of the evidence
-
7.
Reporting of what is known and unknown
A systematic review of interventions (for instance, one designed to evaluate treatment of gingival recessions) applies the PICO criteria to formulate the focused question, where P represents “patient population” (e.g. patients with gingival recessions), I “intervention” (e.g. the type of intervention(s) and conditions related to the prognosis of the treatment of the recessions), C “comparison” (e.g. the “gold standard” procedure and the main treatment alternatives for soft-tissue root coverage) and O “outcomes” (i.e. the results of treatment in terms of patients’ satisfaction, recession depth reduction, functional improvements) [1, 3, 8].
The main resources and advantages of an SR relate to the precise assessment of an increased amount of data (when compared to individual studies) and its inherent greater statistical power, as well as by its robustness. Preferably, a randomized clinical trial is the type of study used to prepare an SR; however, other “lower” quality studies, such as (nonrandomized) controlled clinical trials and case series may be used as well when enough evidence is unavailable. The inclusion of such studies may decrease the real effect of treatment or even does not give support to the assumptions of interest (i.e. they may not allow the achievement of a convincing answer to the raised focused question).
Apart from the potential advantages and disadvantages of SRs, it is important to highlight that the lack of evidence (or information) of a procedure in a predetermined moment in time does not mean that the clinical evidence on the efficacy/effectiveness of such a procedure does not exist. In other words, clinical expertise may guide decision-making as well, when not enough information is available.
1.4 Clinical Remarks: “Can an Evidence-Based Decision-Making Process Be Really Relevant and Clinically Viable for Private Daily Practice?”
From a theoretical point of view, an “evidence-based decision-making” could be developed based on the questioning of the importance of the disease/condition, achievement and analysis of the best information available and adjustment and application of the results of research to the treatment of my patients. Overall, these steps are able to provide the “scientific truth” to the community of researchers involved in this process, patients and clinicians as well. On the other hand, the amount of information achieved after following these steps, or even the identification of a “lack of evidence”, should not be interpreted simplistically like a “clinical guide”.
Regarding to the answer of the question whether an evidence-based decision-making process can be really relevant and clinically viable for private daily practice, it seems no longer acceptable to propose a treatment planning not focused on the best level of information available for each treated case. Conversely, it does not mean that new or alternative procedures might be used when definitive information is still scarce, so clinical expertise may fulfil the gap of knowledge until strong evidence becomes available. Independent of the existence of enough evidence to support or refute the proposal of a periodontal/peri-implant plastic surgical therapy, clinicians should follow the principles of combining the best level of information available, clinician’s expertise and patient’s preferences.
Definitions for the Strength and Direction of Recommendation Regarding the Need of Therapy and Procedures
Within all chapters of this book, summary of the reviews/critical remarks of the literature and evidence quality rating/strength of recommendation of procedures were based on the criteria defined by the US Preventive Services Task Force (USPSTF) adapted by the American Dental Association [12]:
-
Strong – Evidence strongly supports providing this intervention
-
In favour – Evidence favours providing this intervention
-
Weak – Evidence suggests implementing this intervention after alternatives have been considered
-
Expert opinion for – Evidence is lacking; the level of certainty is low. Expert opinion guides this recommendation
-
Expert opinion against – Evidence is lacking; the level of certainty is low. Expert opinion suggests not implementing this intervention
-
Against – Evidence suggests not implementing this intervention or discontinuing ineffective procedures
References
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.0.1 [updated September 2008] The Cochrane Collaboration 2008. Available from: www.cochrane-handbook.org. Accessed and downloaded 15 Nov 2008
McGuire MK, Newman MG. Evidence-based periodontal treatment. I. A strategy for clinical decisions. Int J Periodontics Restorative Dent. 1995;15:70–83.
Needleman IG. A guide to systematic reviews. J Clin Periodontol. 2002;29 Suppl 3:6–9.
Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA, Lima LA. Can subepithelial connective tissue grafts be considered the gold standard procedure in the treatment of Miller Class I and II recession-type defects? J Dent. 2008;36:659–71.
Chambrone L, Lima LA, Pustiglioni FE, Chambrone LA. Systematic review of periodontal plastic surgery in the treatment of multiple recession-type defects. J Can Dent Assoc. 2009;75:203a–f.
Chambrone L, Sukekava F, Araujo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localised recession-type defects. Cochrane Database Syst Rev. 2009;(2):CD007161.
Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. J Periodontol. 2010;81:452–78.
Chambrone L, Faggion Jr CM, Pannuti CM, Chambrone LA. Evidence-based periodontal plastic surgery: an assessment of quality of systematic reviews in the treatment of recession-type defects. J Clin Periodontol. 2010;37:1110–8.
Chambrone L, Pannuti CM, Tu Y-K, Chambrone LA. Evidence-based periodontal plastic surgery. II. An individual data meta-analysis for evaluating factors in achieving complete root coverage. J Periodontol. 2012;83:477–90.
Chambrone L, De Castro Pinto RCN, Chambrone LA. The concepts of evidence-based periodontal plastic surgery: application of the principles of evidence-based dentistry for the treatment of recession-type defect. Periodontol 2000. 2015 (in press)
Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol 2015;86(2 Suppl):S8–51.
ADA Clinical Practice Guidelines Handbook [updated November 2013]. American Dental Association– available at: http://ebd.ada.org/contentdocs/ADA_Clinical_Practice_Guidelines_Handbook_-_2013_Update.pdf. Accessed 29 Jan 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Chambrone, L. (2015). Evidence-Based Decision-Making: An Overview. In: Chambrone, L. (eds) Evidence-Based Periodontal and Peri-Implant Plastic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-13975-3_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-13975-3_1
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13974-6
Online ISBN: 978-3-319-13975-3
eBook Packages: MedicineMedicine (R0)