Abstract
This chapter describes a method of engineering support of preoperative planning of surgical procedures with the use of engineering tools, such as state-of-the-art software for medical image processing, or a finite element method. The procedure of pre-operative planning consists in matching individual cases of incision sites and directions, visualization and selection of areas for resection as well as planning the technique of implant positioning and fixation. Also, the final visualization of the result of the planned medical procedure can be performed. This paper presents procedural propositions in surgery planning in the cases of corrections of the head shape in patients with craniosynostosis, corrections of the chest deformity such as pigeon chest and stabilization of the lumbar spine. 3D models created on the basis of computer tomography (CT) or magnetic resonance imaging (MRI) enabled it to conduct a biomechanical analysis as well as an objective quantitative and qualitative virtual evaluation of the surgical procedure. Preoperative planning support gives the physician an opportunity to prepare for the operation in a better way, which results in the selection of the best possible variant of an operative technique, reduction of time of the surgical procedure and minimization of the risk of intraoperative complications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Preoperative Planning
- Frontal Bone
- Spongy Bone
- Computer Tomography Image
- Surface Replacement Arthroplasty
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Engineering support in medicine can be observed on a daily basis in a form of measuring apparatuses, hospital equipment or new materials used for the manufacturing of surgical tools, implants or prosthetic appliances. However, apart from technical facilities a new methodology has been being developed aiming at the support of surgical procedures with the use of engineering software. Such procedures are used in some medical centres, mainly in the field of neurosurgery, orthopaedic surgery and cardiosurgery. At the planning stage an engineer may indicate elements which should be taken into consideration during an operation in order to achieve the desired treatment effects. It is nevertheless the doctor who makes the final decision on the operative technique and methods of surgical procedure. The possibility of a 3D visualization of the surgical procedure and prediction of the course of the operation as well as evaluation of the results undoubtedly provides a perfect assistance to the physician. Virtual training before a real-life procedure in the operating theatre enables the doctor to prepare for the operation in a precise way. It is essential in the case of young surgeons who are only beginning to develop their skills and technique. It is also vital that surgical procedures be planned individually for each patient. While performing the simulation it is possible to take into account certain ontogenetic features which could not be fully determined in a standard way, such as thickness of the bones in the sites of planned incisions or drilling.
Medical imaging technology enables it to export images of diagnostic examinations, e.g. CT or MRI, to the computer. Thanks to that a 3D model can be generated and subsequently modified. Nowadays, new systems are being created which support the doctors in the scope of the selection of a surgical technique or a proper implant. The system VIRTOPS (Virtual Operation Planning in Orthopaedic Surgery) may be one of the examples of the above-described software. It is used to plan operations of bone tumours with endoprosthetic reconstruction of the hip based on multimodal image information [17]. The chief objective of the programme is to match a proper endoprosthesis to an individual case as well as to provide a very thorough visualization of the tumour located in the bone. 3D images or films developed during the planning stage of the operation may serve as medical documentation as well as be used for the patient’s preoperative information. CT and MRI images are imported to VIRTOPS system. On the basis of the generated models virtual operation planning is carried out (Fig. 1).
Left: The marked points on the hip joint border and the approximated plane are shown. Right: Resulting position of the artificial hip joint in correspondence to the mirrored, healthy hip part [16]
Another programme which is used for preoperative planning of surgical procedures is SQ PELVIS. It enables virtual planning of operations of pelvis injuries on the models created on the basis of DICOM images [5]. The segmentation of tissues on the grounds of the Hounsfield scale plays an essential role in the planning process. Having generated a satisfactory model one may position implants and match them to the individual needs of the examined patient (Fig. 2).
Virtual planning of pelvis stabilization with the use of SQ PELVIS system. Left: Virtual reduction and fixation of the fractured bone. Right: The direction and length of the screws [5]
Another approach aims to support the surgeon by providing them with templates which facilitate technical aspects of carrying out the operation, for instance, a navigation system (Fig. 3) which was used in the work of Gras et al. [13] to plan the position of the stabilizing screws in pelvic ring injuries.
Sterile touch screen of the navigation system (Vector Vision, Brainlab) displaying standard images (lateral view, inlet, outlet) and an auto-pilot view. Red bar: virtually planned SI-screw; yellow line: prospective path of the navigated guide wire (trajectory), green bull’s-eye: reflecting the exact positioning of navigated instruments to achieve the planned screw position [13]
Another example can be provided by operative planning in orthognathic surgery [10]. The standard planning is done on the basis of CT scanning (Fig. 4). However, there are also special programmes, such as Mimics and 3-matic software (Materialise) [23] for planning the corrections of the facial skeleton. Similar procedures supporting treatment in orthognathic surgery were developed, among others, by: Cutting [8, 9], Yasuda [30] and Altobelli [1].
Example of computer-aided surgery (CAS) of a patient with Crouzon syndrome. Simulation and result of Le Fort II distraction before surgery and after CT planning [10]
In more advanced research new devices are being developed with the purpose of supporting the doctor during the surgical procedure, for example: a neck jig device presented in the work of Raaijmaakers et al.[25]. The Surface Replacement Arthroplasty jig was designed as a slightly more-than-hemispherical cage to fit the anterior part of the femoral head. The cage is connected to an anterior neck support. Four knifes are attached on the central arch of the cage. A drill guide cylinder is attached to the cage, thus allowing guide wire positioning as pre-operatively planned (Fig. 5).
Neck jig designed to drill a guide wire in a pre-determined position and direction, seen from medioposterior (left) and anterolateral (right) [25]
Apart from planning a procedure for an individual patient, new methods of engineering support make it possible to choose optimal parameters for the operation. An example can be provided by the application of a method of finite elements in the biomechanical analysis of the system after simulated virtual treatment. In the research of Jiang et al. [19] planning of corrective incisions (scaphocephaly) was done as well as biomechanical analysis of the obtained models was performed (Fig. 6). Thanks to that, it is possible to choose the most favourable variant of the operation. In addition to that, the research of Szarek et al. [27] analysed the level of stress in the hip joint endoprosthesis resulting from variable loads during human motor activity.
Distribution of stress (top) and displacements (bottom) in the skull vault before the surgery and in five variants of corrective incisions [19]
Analysing the influence of preoperative planning and 3D virtual visualization of the examined cases on the quality of treatment, it can be stated that the engineering support provides assistance for the vast majority of doctors in the scope of complex assessment of the phenomenon and preparation for a real-life procedure. The conducted research has proven that [18] both the planning time and labour intensity are reduced by around 30 % if 3D models are available. In addition to that, the precision (accuracy) of predicting the size of the resection area (e.g. in the case of tumours) increases by about 20 % (Fig. 7). Moreover, according to subjective feelings of the examined doctors their confidence in the established diagnosis has risen by around 20 % in the case of 3D planning.
Comparison between viewing 2D CT images and 3D displays of thoracic cavities in determining the resectability of lung cancer. Left: Planning time. Right: Accuracy of predicted resectability [18]
2 Engineering Support Procedure for Preoperative Planning
Surgical treatment within the skeletal system is always the last resort in the case when other preventive methods have failed. For instance, when the application of orthopaedic equipment has not brought the desirable effects. On the basis of several-year tests carried out in co-operation with surgeons a general scheme of engineering support procedure has been developed for pre-operative planning of surgical operations (Fig. 8).
In the first phase the attending physician gives a diagnosis of the disease. Usually, within the framework of a regular diagnosis a CT or MRI examination is done, thanks to which 2D images of individual cross sections are obtained. On the grounds of the Hounsfield scale, in the programme Mimics® Materialise [31] it is possible to segment the tissues of interest (e.g. bones, cartilages) and then generate a 3D model. In the next stage, on the basis of the constructed geometrical model it is possible to carry out detailed morphological measurements in order to determine the type of the defect and degree of the disease progression.
On these grounds the patient is qualified for the surgical procedure by the doctor. Additionally, the programme 3-matic® Materialise [32] makes it possible to do the analysis of bone thickness, which is very helpful in the selection of surgical tools for the operation. Mimics programme enables all sorts of modifications of the obtained model as well as simulations of the planned operation. In consultation with the doctor, bone incisions and displacements are simulated with the purpose of obtaining the desirable treatment effects. After the correction has been planned, it is advisable to conduct the morphometric analysis once again in order to check the values of indexes which were used in the preoperative evaluation.
Next, the model is prepared to be introduced into computing environment. Discretization of the model, i.e. the creation of the volumetric mesh and its optimization is done in the 3-matic programme. Then, the model is exported to Ansys Workbench® environment [33] in order to carry out biomechanical analyses. The primary objective of FEM analysis is to check whether during bone modelling or implanting no fracture or damage to the structure occurs. It is particularly important while planning endoscopic surgical procedures due to the fact that any unforeseen fracture of the bones makes it necessary to stop the microinvasive surgical treatment and complete the operation with the use of classic methods. A numerical simulation provides thus an individual risk assessment of the surgical procedure and may be a decisive factor while selecting a variant of the operation.
Finally, by comparing the results of the performed analyses it is possible to make the most advantageous and the safest choice of the operative variant. It must be emphasized that preoperative planning is an absorbing and time-consuming process, and therefore, not suitable for all kinds of operations. Its application is justified and brings many notable benefits in the case of particularly complicated surgical procedures.
In the further part this paper presents examples of procedures of engineering support for preoperative planning in the cases of surgical corrections of head shape in infants, corrections of chest deformities as well as spine stabilization.
2.1 Application of Engineering Support in Preoperative Planning of Head Shape Correction in Infants with Craniosynostosis
Craniosynostosis is a condition in which one or more of the fibrous sutures in an infant skull prematurely fuse by turning into bone (ossification), thereby changing the growth pattern of the skull [2, 20, 21, 29]. One of the most common cases of craniosynostosis is trigonocephaly, i.e. premature fusion of the metopic suture leading to a deformity of a triangular shaped forehead. Planning of the endoscopic correction of trigonocephaly in a two-month boy was done. CT images of the head were imported to Mimics environment in order to generate a 3D model of the skull. The primary task was to decide on the basis of a morphological analysis whether to qualify the patient for the classic surgical procedure or microinvasive one. The bone incisions and displacements were planned as well as possible variants of correction were developed.
In the first place, the analysis of bone thickness was performed in order to initially determine a type of the operation [22]. Maximum and minimum thickness was measured in the sites of fusion of the metopic suture subject to resection. Thickness in those points was respectively: max 7.01 mm, 4.46 mm and min 2.02 mm (Fig. 9). Thickness points of the whole skull were also determined. Average thickness of bones equalled 2.0 mm with a standard deviation of 1.2 mm.
Subsequently, points necessary for setting indexes determining an incorrect shape of the head were marked on the model [28]. These are the following points: euryon, metopion, sphenion c, lateralis orbitae, medialis orbitae, nasion (Fig. 10).
One set the values of indexes determining an incorrect shape of the skull in trigonocephaly. Those values were next compared to the standard values of children with a regular skull shape at the age of 0–2 months old in order to determine the way the correction should be performed. The results have been presented in Table 1. The measurements showed that the frontal angle was too acute but other indexes were within regular limits. No hypertelorism was detected, therefore the correction was going to be made only on the frontal bone without any interference in the orbital cavities. In this way it was determined that it was possible to carry out a microinvasive procedure. The main decisive factors at that stage of planning were as follows: the patient’s age, bone thickness (within 5 mm in the sites of potential incisions) as well as a correct distance between orbital cavities and a lack of deformities within facial skeleton. The doctor made a decision that the correction of the skull shape was going to consist in the cutting of the fused metopic suture and parting of the bones in order to obtain an optimum shape of the head.
The virtual correction was performed in two stages. In the first one the frontal bone was separated from the rest of the skull alongside frontoparietal sutures. The lower limit was provided by the nasal bone and frontozygomatic sutures. The incisions of the frontal bone were planned in Mimics environment in the way guaranteeing an optimum forehead shape (Fig. 11). Dislocations, in fact rotations, of the fragments of the bones were done manually taking into consideration the doctor’s suggestions and actual conditions of the operation. Point nasion (n) on the nasal bone was defined to be a fixed point according to which the bones were parted to make the head shape round.
Having obtained an optimal visual effect of the correction, one measured displacement of several bone points which in the further planning phase were introduced into Ansys environment as boundary conditions. In the end, the average displacement of the bones from their initial position equalled 11 mm. The value of the frontal bone angle was checked once again in order to evaluate if it was now close to standard. After the procedure the angle was increased up to 132.7º, which produced a satisfactory effect of the correction (Fig. 12).
Numerical simulations were carried out in Ansys environment. However, before that discreet models of individual bones had been prepared in 3-matic programme compatible with Mimics software.
For the examined models simplifications were adopted in three basic categories: geometry, material and boundary conditions. Skull geometry, which was generated on the basis of CT images, was imported from Mimics programme without skin, blood vessels and other structures. Also, one did not take into consideration joints between the anatomical elements of the skull, such as cartilages, sutures, etc. Preparatory proceedings were similar for all of the below-mentioned cases. The generated bone models with adequate incisions were digitalized. In order to optimize the model, Laplace’s method of approximating integrals was used several times (an inbuilt function of the software) with a coefficient equal to 0.4 ÷ 0.7. Next, they were divided into tetrahedral finite elements of Solid 72 type, whose maximum length of edges did not exceed 3 mm. Then, a volumetric mesh was generated in order to finally export the model to *.cdb format. Such actions caused the loss of geometrical details which were deemed irrelevant.
Material properties of the skull were adopted as isotropic in the process of modelling. It is evident that in the modelling of long bones or adult bones the bone should be treated as anisotropic material. However, both in this work and other research works [3, 6, 7] such simplification was accepted. The value of Young’s modulus was adopted at the level of 380 MPa and Poisson’s ratio equal to 0.22, which had been determined in earlier research [14]. These values are close to the results obtained by other researchers.
The last category of the simplification premises includes the boundary conditions of the model. After the introduction of the model into Ansys environment, the skull bones were fixed in the sites where there are natural joints: fusion of bones and cartilages. It should be pointed out that these joints are elastic joints (sutures), while in the static analysis a rigid fixation is necessary, which can on the other hand cause the occurrence of local concentration of stress. Further displacements were subsequently set. They had been measured during the correction planning done in cooperation with the doctor. The values of displacements were also averaged with a view to avoiding additional calculation errors.
The analysis determined the total deformation, reduced strain and stresses with the use of von Mises hypothesis. An abridged list of simplification assumptions has been presented in Table 2.
Three variants of incisions were prepared for the analysis (Fig. 13) being 30, 50 and 70 mm long respectively. Simulation was performed in order to ensure that no damage to the bones occurs during the medical procedure due to the deformation done by a certain value.
After the model geometry had been introduced, a rigid fixation was placed in the site of the frontal bone (in the vicinity of nasion point)— (Fig. 14 ). Moreover, the displacements in axes x and z were completely restricted in the sites of the frontoparietal suture. Also, the dislocation of these sites in y axis was partially limited (a maximum value of 6 mm was determined on the basis of the simulation results in Mimics software). It was calculated that displacement of upper parts of the incised halves of the frontal bone necessary to obtain an optimum shape of the skull equals 11 mm in the direction of y axis.
The results of numerical analysis have been presented in Table 3. The distribution of displacements has been taken into consideration as well as the maps of stresses occurring in the frontal bone in different incision variants. The case subject to examination is an example of one of the simplest methods of treatment in the context of incision technique. It results mainly from the fact that this is a microinvasive procedure, therefore the possibilities to use different incisions are small due to the limitations connected with the operative field and the applied surgical tools. Further part of this work presents an example of a classic surgical procedure of trigonocephaly correction.
Analysing the results of the simulation it was stated that the distribution of bones displacement is very similar in all three variants. Considerable differences may be noticed in maximum values of stresses occurring at the time of bone modelling. In the first variant they are the smallest and equal max 43 MPa, in the second variant 54 MPa. In both cases the stresses do not exceed permissible values, therefore it can be assumed that no bone damage will occur during the surgical procedure. In the third variant, maximum stresses equal 62.5 MPa. This variant was rejected due to the fact that too deep incision is always more risky as to the fracture of the bone in the vicinity of nasion point. At the same time, the visual effect does not differ much from the result obtained in variant 2. Variant 1 was also rejected as in this case the incision could prove too small to enable further correct growth of the skull. Finally, on the grounds of the quantitative and qualitative assessment variant 2 of the correction was adopted as optimal.
2.2 Application of Engineering Support in Preoperative Planning of Pigeon Chest Correction
The most common chest deformities (considered developmental anomalies) in children include funnel chest (pectus excavatum) and pigeon chest (pectus carinatum). Funnel chest usually requires surgical treatment in order to restore correct breathing parameters [15]. Whereas, in the case of pigeon chest an early discovery of the defect makes it possible to undertake a non-invasive treatment, for instance by means of orthoses. Pigeon chest is a deformity of the anterior wall of the chest characterized by a strong deformation of the sternum and parasternal fragments of the ribs. The authors of this work present in cooperation with thoracic surgeons preoperative planning of the correction procedure of pigeon chest in a 13-year-old boy.
In the first place, the evaluation of the malformation degree was carried out with the use of the Haller index (Fig. 15) defined as a relationship of the chest width in the transverse plane to the distance between the sternum and spine. That was done in order to decide if a surgical procedure was necessary. The Haller index equals 2.5 for a normally formed chest, whereas in the examined patient it amounted to 1.71, which confirmed the increased anterior and posterior dimension.
In the next stage, a geometrical model of the chest was started to be developed. On the basis of the patient’s CT images using Mimics software a three-dimensional model of individual structures of the chest was developed. The process of building a geometrical model consisted in generating and editing masks of individual elements. The creation of a mask in Mimics environment consists in segmentation by means of partition of homogeneous areas as to grey shades in a previously defined search area. In the process of segmentation of the pigeon chest model the following items were distinguished (Fig. 16):
-
22 Bone ribs,
-
11 Thoracic vertebrae,
-
10 Intervertebral discs,
-
14 Cartilage ribs
-
Sternum.
The algorithm of creating the above-mentioned elements was very similar in each case except for intervertebral discs and cartilage ribs which required more correction with the use of masks editing tools due to a heterogeneous grey shade.
Next, one began planning of the correction treatment of the defect by means of Ravitch’s method. It consisted in resection of the elements of the cartilage ribs and sternum as well as their adequate rotation and repositioning. Displacement and rotation of the fragments of the bones were set manually taking into consideration the doctor’s suggestions and actual circumstances of the surgical procedure. A correct position of the sternum was obtained by repositioning it in the direction towards the spine by about 30 mm (Fig. 17). At the same time, by removing the fragments of the cartilage ribs and by moving them one decreased the inclination angle of the sternum to the median plane from 24.26° to 13.05.
After obtaining an optimum visual effect of the correction, the dislocations of several bone points were measured. In the further phase of planning they were introduced into Ansys environment as boundary conditions. All elements of the chest were digitalized by tetrahedral elements Solid72 in 3-matic programme. The volumetric mesh was created and optimized (Fig. 18).
The numerical analysis of the pigeon chest model was performed with the use of Ansys Workbench environment. The boundary conditions of the analysis have been presented in Table 4.
With a view to carrying out simplification of the numerical model one omitted the impact of internal organs as well as pressure inside the thorax. The total number of finite elements amounted to 299 974, which were connected in 550 482 nodes. Contacts between individual elements were done automatically in the first stage, then their surfaces were corrected manually. The surfaces were linked by means of a ‘Bonded’ type connection, which does not allow the elements to dislocate in relation to each other. The total number of all connections amounted to 70. The model was fixed by means of taking away the degree of freedom in the nodes on the upper surface of the first thoracic vertebra and the lower surface of 11-th vertebra.
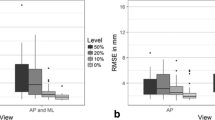
During the numerical analysis, reduced strain and stresses were determined with the use of von Mises hypothesis. The results of the numerical analysis have been shown in Fig. 19.
On the basis of the performed numerical calculations the index of the model stiffness was determined. It was defined according to the below formula (1) which equalled 2.86 for the analyzed case.
where F is the measured force and d is the measured displacement
While analyzing the findings of the simulation it was stated that the distribution of maximum stresses in the sternum (6.92 MPa), cartilage ribs (8.39 MPa) and bone ribs (36.73 MPa) did not indicate any possibility of damage occurring during the procedure of the pigeon chest correction by Ravitch’s method as they were all lower than 87.0 MPa, which was adopted as a permissible value. The obtained maximum values of main deformations 0.0012 in bone elements of the chest were also below the values suggesting the bone destruction [24].
2.3 Preoperative Planning of the Lumbar Spine Stabilization
This part presents a process of preoperative planning of a neurosurgical procedure conducted on the basis of CT images of the patient suffering from lumbar spine with degeneration process and spondylolisthesis.
In the presented case preoperative planning concerned the lumbar spine degeneration and mild form of bulging of L4/L5 intervertebral disc.
CT images processing was done with the use of Mimics software. The spine structures, which were important due to mechanical aspects, were segmented on the basis of masks assigned to them. The development of the masks consisted in matching the upper and lower threshold of the grey shade level corresponding to individual structures. The vertebrae segmentation was performed using masks covering the areas in which given vertebrae were located. The effect of the performed operations has been presented in Fig. 20.
The created geometrical models of the anatomical structures of the spine constitute the basis for further procedures aiming to check the degree of the implant matching by means of the simulation of a surgical procedure. At this stage a 3D model of stabilization executed in CAD software can be transferred to Mimics programme (in STL format). Next step is to adjust the implant in the site of the predicted stabilization. Precise positioning of the implant in the spine as well as the fact that the surgical procedure is microinvasive play an essential role during the implant insertion. The performed simulation makes it possible to verify the construction by checking compatibility of main stabilization measurements with individual anatomical features of the patient. In this case it was used an implant by Coflex company which is used in clinical practice for lumbar spine stabilization with posterior intervertebral systems (Fig. 21).
In the case of application of ready-made implants available on the market, the preoperative planning enables it to choose from the catalogued series of types the best kind and type of stabilization matching an individual patient. Geometrical models of L4 and L5 vertebrae were modified in the site of the implant positioning, exactly like during a surgical procedure. Material properties were attributed to stabilization. They were determined as follows: titanium alloy Ti-6Al-4 V, i.e. Young modulus equal to 115 GPa and Poisson’s ratio equal to 0.3 [23].
For the sake of subsequent strength analysis the model was digitalized with the use of a finite element method MES. Each element of the performed model had a mesh created by means of tetragonal elements of an average edge distance of 3 mm. Then, material properties were determined for individual elements. The programme Mimics by the firm Materialise, which was used in this research, makes it possible to define proportions and distribution of the material within the object. The programme enables it to attribute to each spatial element as many properties as defined by the designer. Cortical bone tissue is different from compact bone not only in its structure but also in mechanical properties. That is why cortical bone and spongy bone were distinguished within each vertebra. In order to segment the spongy bone tissue the functions available in Mimics software were applied. To achieve that it was necessary to make the mask areas of spongy bone on the vertebra contours in all cross sections
The masks served the purpose of providing the areas covered by defined masks with spongy bone material properties. This tool of the programme was used while defining material properties of other anatomical structures on the basis of the already created masks. The values of the determined properties have been placed in Table 5, whereas the graphic distribution of tissues has been presented in Fig. 22.
A key factor taken into consideration in the selection of a stabilization type for the lumbar spine is the impact it will exert on the stabilized section. Numerical simulations of the models of the physiological section of the human lumbar spine as well as numerical simulations of the posterior interspinal stabilization make it possible to analyse the degree of load on the spine and the influence of implantation on spinal properties. The analysis of the spinal load and of the impact of the conducted implantation on the lumbar spine properties was made in ANSYS programme. In order to achieve that, the executed models, both physiological one and stabilized one, were imported to that programme. Calculations were carried out with the set boundary conditions equal to loads occurring in a natural standing position. The load amounting to 1000 N was set on the upper surface of vertebra L3 while fixation was set on the lower surface of vertebra L5/S1 (Fig. 23).
While analyzing the obtained results of compression it was noticed that resultant values of displacements are higher for the physiological spine model than in the case of the implant model. Their maximum values equal respectively 0.45 mm for the model without implant, and 0.22 mm for the model with implant. The biggest reduction of stresses determined according to Huber-Mises hypothesis occurred in the bone tissue, at the vertebral pedicle. The values did not exceed 36 MPa for the physiological model. However, for the spine-and-implant system the highest intensity of stresses occurred in the very implant amounting to 37 MPa. In the spine-and-implant system one observed lower values of strain than in the physiological model. Maximum values of strain equalled respectively 0.016 and 0.008 (Table 6).
The conducted analyses make it possible to state that the implanted stabilization has improved the spine stability. After the implant positioning the values of resultant displacements decreased during strength simulations. It resulted from the fact that the degenerated movable segment was stabilized with the use of the implant as well as due to the material properties forming the implant. Also it is significant that after stabilization the cross-section areas of spinal nerves increase (Fig. 24), therefore it can be concluded that the patient’s pain will decrease.
The performed research shows how medical and biomechanical interpretation of numerical simulations can be used to plan neurosurgical procedure of spine stabilization. Biomechanical analyses of strength and forces can ascertain the durability and stability of the implant connection with the stabilized section of spine and also determine places that require reconstruction of bone. With finite element method, surgical prediction can be made to guide surgeons to make the decision of improving surgical treatment. Virtual planning of the treatment is helpful for the neurosurgeons, because it increases the quality of treatment and safety during the operation.
3 Conclusions
Preoperative planning of medical procedures with engineering support definitely facilitates the achievement of desirable effects of treatment. Contemporary technical and technological advances, particularly in bone surgery, encourage the implementation of new innovative ideas and cutting edge technology into operative technique aiming at the application of microinvasive procedures. There are several CAD programmes which could become a perfect biomechanical tool complementing medical knowledge. Such software makes it possible to do, among other things, mechanical analyses as well as to plan surgical procedures. Preoperative planning may be supplemented by an additional procedure of reconstructing anatomical structures and performing a virtual medical operation (simulation) in the computer system. The models obtained in such a way may also serve the purpose of engineering analysis which aims at characterizing the interaction of tissues in time as well as assessing the risk of bone damage or fracture during a surgical procedure. The developed method of engineering support makes it easier for the doctors to make right decisions at each stage of treatment. This kind of support may have a significant importance for young inexperienced surgeons or medical students. However, even experienced doctors may practise each phase of the surgical procedure virtually, which considerably shortens the duration of the operation. The application of a complex planning procedure is simply indispensable in the case of complicated, multi-phase surgical procedures. Its major advantage is an individual approach to each patient. The examples of planning surgical procedures show that engineering support increases patients’ safety during the operation and improves the quality of treatment. Interdisciplinary collaboration between doctors and engineers brings desirable benefits and results in well-performed operations.
References
Altobelli DE, Kikinis R, Mulliken JB, Cline H, Lorensen W, Jolesz F (1993) Computed-assisted three-dimensional planning in craniofacial surgery. Plast Reconstr Surg 92:576–585
Barone CM, Jimenez DF (2004) Endoscopic approach to coronal craniosynostosis. Clin Plast Surg 31:415–422
Baumer TG, Powell BJ, Fenton TW, Haut RC (2009) Age dependent mechanical properties of the infant porcine parietal bone and a correlation to the human. J Biomech Eng 131(11):111–116
Bruchin R, Stock UA, Drucker JP, Zhari T, Wippermann J, Albes JM, Himtze D, Eckardt S, Konke C, Wahlers T (2005) Numerical simulation techniques to study the structural response of the human chest following median sternotomy. Ann Thorac Surg 80:623–630
Cimerman M, Kristan A (2007) Preoperative planning in pelvic and acetabular surgery: the value of advanced computerized planning modules. Injury 38(4):442–449
Coats B, Margulies SS (2006) Material properties of human infant skull and suture at highrates. J Neurotrauma 23:1222–1232
Couper ZS, Albermani FG (2005) Biomechanics of shaken baby syndrome: physical testing and numerical modeling. In: Deeks Hao (eds) Developments in mechanics of structures and materials. Taylor Francis Group, London, pp 213–218
Cutting C, Bookstein Fl, Grayson B, Fellingham L, Mccarthy JG (1986) Three dimensional computer-assisted design of craniofacial surgical procedures: optimization and interaction with cephalometric and CT-basedmodels. Plast Reconstr Surg 77:877–885
Cutting C, Grayson B, Bookstein F, Fellingham L, Mccarthy JG (1986) Computer-aided planning and evaluation of facial and orthognathic surgery. Clin Plast Surg 13:449–462
Ehmer U, Joos U, Flieger S, Wiechmann D (2012) The University Münster model surgery system for Orthognathic surgery. Part I—the idea behind. Head Face Med 8:14
Furusu K, Watanabe I, Kato Ch, Miki K, Hasegawa J (2001) Fundamental study of side impast analysis using the finite element model of the human thorax. JSAE 22:195–199
Gzik M, Wolański W, Kawlewska E, Larysz D, Kawlewski K (2011) Modeling and simulation of trigonocephaly correction with use of finite elements method. Proceedings of the III ECCOMAS thematic conference on computational vision and medical image processing: VipIMAGE, Portugal, pp 47–50
Gras F, Marintschev I, Wilharm A, Klos K, Mückley T, Hofmann G (2010) O: 2D-fluoroscopic navigated percutaneous screw fixation of pelvic ring injuries—a case series. BMC Musculoskelet Disord 11:153
Gzik M, Wolański W, Tejszerska D, Gzik-Zroska B, Koźlak M, Larysz D (2009) Interdisciplinary researches supporting neurosurgical correction of children head deformation. Model Optim Phys Syst 8:49–54
Gzik-Zroska B, Wolański W, Gzik M (2013) Engineering-aided treatment of chest deformities to improve the process of breathing. Int J Numer Method Biomed Eng 29:926–937
Handels H, Ehrhardt J, Plötz W, Pöppl SJ (2001) Three-dimensional planning and simulation of hip operations and computer-assisted construction of endoprostheses in bone tumor surgery. Comput Aided Surg 6(2):65–76 (Wiley Online Library)
Handels H, Ehrhardt J, Plötz W, Pöppl SJ (2000) Virtual planning of hip operations and individual adaption of endoprostheses in orthopaedic surgery. Int J Med Inform 58–59:21–28
Hu Y, Malthaner RA (2007) The feasibility of three-dimensional displays of the thorax for preoperative planning in the surgical treatment of lung cancer. Eur J Cardiothorac Surg 31:506–511
Jiang X, You J, Wang N, Shen Z, Li J (2010) Skull mechanics study of PI procedure plan for craniosynostosis correction based on finite element method, Proceedings of 4th International Conference on Bioinformatics and Biomedical Engineering (iCBBE)
Jimenez DF, Barone CM, Cartwright CC et al (2002) Early management of craniosynostosis using endoscopic-assisted strip craniectomies and cranial orthotic molding therapy. Pediatrics 110:97–104
Larysz D, Wolański W, Gzik M, Kawlewska E (2011) Virtual planning of the surgical treatment of baby skull shape correction. Model Optim Phys Syst 10:49–52
Larysz D, Wolański W, Kawlewska E, Mandera M, Gzik M (2012) Biomechanical aspects of preoperative planning of skull correction in children with craniosynostosis. Acta Bioeng Biomech 14:19–26
Marchetti C, Bianchi A, Muyldermans L, Di Martino M, Lancellotti L, Sarti A (2011) Validation of new soft tissue software in orthognathic surgery planning. Int J Oral Maxillofac Surg 40:26–32
Nackenhorst U (1997) Numerical simulation of stress stimulated bone remodeling. Technische Mech 17(1):31–40
Raaijmaakers M, Gelaude F, de Smedt K, Clijmans T, Dille J, Mulier M (2010) A custom-made guide-wire positioning device for hip surface replacement arthroplasty: description and first results. BMC Musculoskelet Disord 11:161
Sacha E, Tejszerska D, Larysz D, Gzik M, Wolański W (2010) Computer method in craniosynostosis. Proceedings of 12th International Scientific Conference “Applied Mechanics”, Technical University of Liberec, pp 111–115
Szarek A, Stradomski G, Włodarski J (2012) The analysis of hip joint prosthesis head microstructure changes during variable stress state as a result of human motor activity. Mater Sci Forum 706–709:600–605
Tejszerska D, Wolański W, Larysz D, Gzik M, Sacha E (2011) Morphological analysis of the skull shape in craniosynostosis. Acta Bioeng Biomech 13(1):35–40
Wolański W, Larysz D, Gzik M, Kawlewska E (2013) Modeling and biomechanical analysis of craniosynostosis correction with the use of finite element method. Int J Numer Method Biomed Eng 29:916–925
Yasuda T, Hashimoto Y, Yokoi S, Toriwaki JI (1990) Computer system for craniofacial surgical planning based on CT images. IEEE Trans MedImaging 9:270–280
Materialise software & services for biomedical engineering: mimics software. http://biomedical.materialise.com/mimics. Accessed 13 March 2014
Materialise software & services for biomedical engineering: 3-matic software. http://biomedical.materialise.com/3-metic. Accessed 13 March 2014
ANSYS software. http://www.ansys.com/. Accessed 13 March 2014
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wolański, W. et al. (2015). Preoperative Planning of Surgical Treatment with the Use of 3D Visualization and Finite Element Method. In: Tavares, J., Natal Jorge, R. (eds) Developments in Medical Image Processing and Computational Vision. Lecture Notes in Computational Vision and Biomechanics, vol 19. Springer, Cham. https://doi.org/10.1007/978-3-319-13407-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-13407-9_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13406-2
Online ISBN: 978-3-319-13407-9
eBook Packages: EngineeringEngineering (R0)