Abstract
This chapter describes preoperative work-up, operative planning, and the technique of a peroral endoscopic myotomy for achalasia, as well as troubleshooting difficult situations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
This chapter describes preoperative work-up, operative planning, and the technique of a peroral endoscopic myotomy for achalasia, as well as troubleshooting difficult situations.
10.1 Clinical History
A 56-year-old woman presented in clinic with a 5-year history of chest pain, heartburn, and dysphagia. She was initially diagnosed with gastroesophageal reflux disease and put on a proton-pump inhibitor. Her symptoms did not resolve with anti-acid medication, and a subsequent esophagogastroduodenoscopy (EGD) was negative for esophagitis.
As her dysphagia progressed from solids to liquids, a complete work-up for esophageal motility disorder was performed:
-
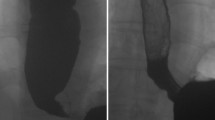
Repeat EGD: dilated and tortuous esophagus without mucosal-based lesions, suspicious for achalasia (Fig. 10.1)
-
Timed barium esophagram: smooth tapering of the distal esophagus and a persistent contrast column of 10.2 cm at 5 min, indicative of bolus retention (Fig. 10.2)
-
High-resolution impedance manometry (HRIM): elevated mean 4-s integrated relaxation pressure (IRP) of 32.4 mmHg, 10 failed swallows, and panesophageal pressurization consistent with type II achalasia according to the Chicago Classification (Fig. 10.3)
She was presented with three treatment options: pneumatic dilation, laparoscopic Heller myotomy, and peroral endoscopic myotomy (POEM). She chose to undergo POEM.
10.2 Operation
10.2.1 Patient Preparation and Operative Setup
Prior to surgery, the patient was kept on a clear liquid diet for 48 h and completed a 5-day course of oral nystatin for Candida prophylaxis.
The patient was positioned supine with the right arm abducted and the left arm tucked at the side, with the abdomen prepped in case needle decompression was required for the presence of capnoperitoneum (Fig. 10.4). The POEM was performed under general anesthesia with endotracheal intubation and skeletal muscle paralysis. Special care was taken at the time of anesthesia induction and endotracheal intubation to prevent aspiration.
10.2.2 Operative Procedure
Step 1
Initial endoscopy
Initial endoscopy was performed using a single-channel, high-definition gastroscope with CO2 insufflation. The air insufflation was confirmed to be turned off. The esophagus and stomach were aspirated of any retained fluid and food, the stomach was desufflated, and the esophageal body was examined for Candida or stasis esophagitis. The endoscope was then fitted with an oblique transparent cap (longer end of bevel posterior) and the distance from the squamo-columnar junction to the incisors was measured on the scope shaft (Fig. 10.5).
Step 2
Mucosotomy and entry into the submucosal space
A submucosal bleb was created in the esophageal wall 12 cm proximal to the esophagogastric junction (EGJ) at the 1 o’clock position, using a sclerotherapy needle containing a solution of 0.9 % saline, 10 mL of indigo carmine (0.2 mg/mL), and dilute epinephrine (5 μg/mL) (Fig. 10.6). An endoscopic cautery knife was used to create a 2-cm longitudinal mucosotomy over the submucosal bleb (Fig. 10.7). The submucosal areolar tissue was cleared to expose the circular muscle layer. The endoscope was then bluntly maneuvered into the submucosal space, utilizing the oblique scope cap.
Step 3
Creation of the submucosal tunnel
Creation of the anterior submucosal tunnel required a combination of electrocautery (Fig. 10.8) and hydrodissection using a solution of saline and indigo carmine without epinephrine (Fig. 10.9). The orientation was checked periodically by evaluating the meniscus of injected fluid within the tunnel. The tunnel was extended 3 cm distal to the EGJ. Narrowing of the submucosal tunnel and the appearance of palisading vessels and aberrant muscle bundles (Fig. 10.10), as well as markings of the shaft of the endoscope, signified transition to the EGJ. The patient’s systolic blood pressure was kept under 120 mmHg to avoid bleeding during progression of the submucosal tunnel. The epinephrine-containing solution was used again in the distal portion of the tunnel. After completion of the submucosal tunnel (Fig. 10.11), the scope was withdrawn from the tunnel and advanced through the esophageal body to the gastric lumen. Blanching of the gastric cardia mucosa, seen upon retroflexion, was recognized as a sign of extension of the submucosal tunnel onto the stomach (Fig. 10.12).
Step 4
Myotomy
A selective anterior myotomy of the inner circular muscle layer was started at 6 cm above the EGJ, using electrocautery to divide individual fibers and extended to the end of the submucosal tunnel (Fig. 10.13). Special attention was taken to protect the mucosa during myotomy progression (Fig. 10.14); splaying of longitudinal muscle fibers rarely occurred. The scope was withdrawn from the tunnel and advanced into the gastric lumen to observe patency of the EGJ.
Step 5
Mucosotomy closure
Finally, the scope was advanced into the tunnel, which was irrigated with a solution of bacitracin. The scope was withdrawn into the true esophageal lumen and the mucosotomy was closed with seven endoscopic clips (Figs. 10.15 and 10.16). A Veress needle was used to relieve capnoperitoneum. The stomach was intubated one last time, aspirated, and desufflated before withdrawal of the endoscope.
10.3 Troubleshooting
POEM is a safe surgical option for the treatment of achalasia, but it requires advanced endoscopic and surgical skills. Initial endoscopy can be difficult in the context of food impaction or retention. This situation can be prevented by giving a clear liquid diet 48 h prior to surgery. In cases of severe esophageal stasis, extensive lavage and aspiration are often required before mucosotomy.
Preoperative treatment with antifungals (nystatin or fluconazole) is recommended to prevent Candida esophagitis, which has a high prevalence in patients with achalasia.
Esophageal muscle circular thickening, sigmoid esophagus, and severe esophageal dilatation can add technical difficulty to POEM. A decision to proceed with POEM in a patient with these findings should be at the discretion of the operating surgeon.
After longitudinal mucosotomy, the endoscope is bluntly maneuvered into the submucosal space. In patients with type III achalasia, Jackhammer esophagus, or esophageal spasms, this step can be technically challenging.
Additionally, bleeding can occur in the submucosal tunnel, particularly when approaching the EGJ, because of the robust blood supply in this area. Bleeding can be controlled by directly coagulating injured vessels (away from mucosa) or applying indirect pressure onto the tunnel with the endoscope positioned in the esophageal true lumen. A systolic blood pressure goal under 120 mmHg is also recommended during this step of the procedure.
Mucosal injury can occur during initial endoscopy or submucosal tunnel creation, but it usually can be repaired by clips. Depending on the extent and location of the mucosal defect, the procedure can be aborted, continued, or performed at an orientation other than the anterior position.
The current recommendation for spastic achalasia is an extended proximal myotomy ablating the entire spastic segment. In these patients, the submucosal tunnel and myotomy are started more proximally in the esophageal body.
Sparing of longitudinal muscle fibers is not always possible. Limited areas of full-thickness myotomy are acceptable in POEM.
Capnoperitoneum may require decompression with a Veress needle. Capnoperitoneum should not be considered as a complication, but rather as a normal consequence of the procedure, given that CO2 can easily dissect through tissue planes.
Finally, mucosal redundancy and infoldings can add to the difficulty of mucosotomy clip closure. Various types of clips can be used to facilitate this last step.
10.4 Postoperative Course
Postoperatively, the patient was extubated and transferred to the postanesthesia care unit for observation. She stayed overnight and was kept nil per os. She received standing intravenous (IV) antiemetics, pain medication, and IV narcotics as needed.
A routine esophagram was performed on the morning of postoperative day 1 to rule out esophageal leak. (This systematic esophagram has since then been eliminated from our practice.) She was started on clear liquids, advanced to full liquids, and discharged on the afternoon of postoperative day 1 on anti-acid medication. The full liquid diet was maintained for 2 weeks and then gradually increased to include soft foods.
She was seen at 2 weeks postoperatively and showed great improvement in her symptoms. Subsequently, she was advanced to a regular diet and scheduled for long-term physiologic follow-up studies.
At 9 months, she was complaining of minimal heartburn on anti-acid medication. The EGD showed Los Angeles grade A reflux esophagitis. The HRIM showed absent peristalsis with eight failed swallows without panesophageal pressurization, and an IRP of 11 mmHg. At 18 months after the POEM procedure, her Eckardt score had decreased to 0 from a preoperative score of 5.
Suggested Reading
Blatnik JA, Ponsky JL. Advances in the treatment of achalasia. Curr Treat Options Gastroenterol. 2014;12:49–58.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, International High Resolution Manometry Working Group. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 Suppl 1:57–65.
Eleftheriadis N, Inous H, Ikeda H, Onimaru M, Yoshida A, Hosoya T, et al. Training in peroral endoscopic myotomy (POEM) for esophageal achalasia. Ther Clin Risk Manag. 2012;8:329–42.
Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228–35.
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–71.
Inoue E, Tianle KM, Ikeda H, Hosoya T, Onimaru M, Yoshida A, et al. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519–25.
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc. 2013;77:719–25.
NOSCAR POEM White Paper Committee, Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80:1–15.
Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012;26:3267–72.
Roman S, Gyawali CP, Xiao Y, Pandolfino JE, Kahrilas PJ. The Chicago Classification of motility disorders: an update. Gastrointest Endosc Clin N Am. 2014;24:545–61.
Sharata AM, Dunst CM, Pescarus R, Shlomovitz E, Wille AJ, Reavis KM, Swanström LL. Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg. 2015;19:161–70.
Swanström LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg. 2011;213:751–6.
Teitelbaum EN, Rajeswaran S, Zhang R, Sieberg RT, Miller FH, Soper NJ, Hungness ES. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery. 2013;154:885–91; discussion 891–2.
Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilia PJ, Pandolfino JE, Hungness ES. Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg. 2014a;18:92–8; discussion 98–9.
Teitelbaum EN, Soper NJ, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, et al. Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg Endosc. 2014b;28:3359–65.
Verlaan T, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, Fockens P. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78:39–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hungness, E.S., El Khoury, R. (2015). Peroral Endoscopic Myotomy (POEM). In: Fisichella, P., Patti, M. (eds) Atlas of Esophageal Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-13015-6_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-13015-6_10
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13014-9
Online ISBN: 978-3-319-13015-6
eBook Packages: MedicineMedicine (R0)