Abstract
PCOS patients are typically characterized by chronic anovulation, hyperandrogenism, polycystic ovaries and these aspects are frequent in a high percentage of women during the repruductive life. PCOS frequently show overweight and/or obesity and are characterized by a higher production of androgens and reduced sensitivity to insulin. In fact it is of great importance to note that up to 60% of all PCOS patients are with modest up to exagerated overweight and that most of these patients show a modest up to an exagerated hyperinsulinism in response to the standard oral glucose tollerance test (OGTT). This reduced insulin sensitivity can be modified by a specific attention to life style, including not only a diet but also certain degree of physical activity. However, a specific effect on hyperinsulinemia can be achieved using glucose sensitizer drugs, such as metformin, so that to reduce the negative modulation exerted by hyperinsulinemia on the reproductive axis as well as on neuroendocrine control of reproduction with relevant effects also on adrenal function and neurosteroid production. Also specific integrative compounds have been proposed in recent years to counteract insulin resistance: myo-inositol (MYO) and d-chiro-inositol (DCI). These 2 compounds are tightly linked one to the other since MYO is transformed by an epimerase in DCI, having each tissue its own conversion rate, likely due to the specific needs for the two different molecules. In general both these compounds works as specific modulators of the intra cellular second messanger activated by the insulin linkage with its own membrane receptor. It remains clear that only the combination of life-style (diet & physical exercise) with one of the above mentioned treatments is able to solve the metabolic/endocrine impairment of overweight/obese PCOS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
According to the Rotterdam criteria, elaborated by the European Society of Human Reproduction and Embryology (ESHRE) and by the American Society for Reproductive Medicine (ASRM), polycystic ovary syndrome (PCOS) is defined by at least two of the three following criteria:
-
1.
Clinical signs of hyperandrogenism or biochemical hyperandrogenemia
-
2.
Oligo-/amenorrhea and chronic anovulation
-
3.
Ultrasonographic evidence of at least one polycystic ovary and exclusion of other relevant diseases (i.e., hyperprolactinemia, thyroid diseases, androgen secretion tumors, and adrenal dysfunction hyperplasia) [1]
This evolution was relevant because it permitted the inclusion of women with PCOS who were excluded by previous NIH criteria [2]: those with polycystic ovaries affected by hyperandrogenism and ovulatory cycles or chronic anovulation and normal androgen levels.
Recently, the Androgen Excess and PCOS Society considered PCOS as an androgen excess disorder in biosynthesis, utilization, and/or metabolism of androgen in women [3].
PCOS occurs in as many as 8–10 % of women of reproductive age [4] with onset manifesting as early as puberty [5].
The syndrome has strong association to infertility, hyperinsulinemia, insulin resistance (IR), impaired glucose tolerance, dyslipidemia, android fat distribution, and obesity. Approximately 60 % of women with PCOS are obese. IR is found in 40 % of normal weight women with PCOS and nearly all overweight women both with and without PCOS [6], but IR is not routinely assessed when diagnosing or treating PCOS. The IR can be treated by insulin sensitizers and/or with diet and exercise before and during fertility treatment and pregnancy. The IR is not currently diagnosed or treated routinely and the effect of treatment is undocumented. Treatment of IR in young women may reduce the risk of diabetes and CV complications later in life. Moreover, a detailed understanding of the importance of IR in female reproductive health and reproduction could lead to new treatment strategies and improved pregnancy and life birth rates for PCOS patients. The PCOS is a multigenic condition where the phenotype is modulated by external lifestyle factors. The risk of adults developing metabolic disease, particularly obesity, hypertension, diabetes, and CVD, is probably influenced by events during embryonic development and fetal and neonatal growth [7]. The risk of diseases during later life may be determined by events or conditions experienced by the mother even before pregnancy occurs.
The IR and hyperandrogenism are associated with altered coagulation and fibrinolysis leading to endothelial dysfunction, vascular chronic low-grade inflammation [8], and atherothrombosis [9]. In PCOS both normal and elevated concentrations of plasminogen activator inhibitor type-1 (PAI 1), an indicator of endothelial dysfunction and of a prothrombotic state, have been found [10]. Other biomarkers such as fibrinogen, coagulation factor VII, coagulation factor VIII, von Willebrand factor, tissue-type plasminogen activator, urokinase-type plasminogen activator (u-PA), and activated partial thromboplastin time have been studied in PCOS and the results are conflicting [11]. Increased high sensitivity C-reactive protein (hs-CRP) is associated with PCOS, cardiovascular disease, overweight, or lean PCOS [12] and IR [13].
In vitro fertilization (IVF) outcomes in PCOS patients have the same live birth rate as control IVF patients [14]. PCOS patients with IR, measured by homeostatic model assessment of insulin resistance (HOMA-IR), had a significantly lower maturation rate of their immature oocytes compared to those with normal IR [15].
Hyperandrogenism and hyperinsulinemia affect follicular microenvironment, resulting in reduced ovarian development of immature oocytes. Moreover, in PCOS patients, significant abnormalities are observed at the earliest stages of folliculogenesis. However, it is unclear which molecules are responsible for the abnormal regulation during early folliculogenesis. It has been reported that some growth factors and sex steroids may have a role in aberrant folliculogenesis in PCOS [16].
A number of growth factors, including vascular endothelial growth factor (VEGF), basic fibroblast growth factor (BFGF), insulin-like growth factor I (IGF 1), and epidermal growth factor (EGF), localize within growing follicles and regulate important aspects of folliculogenesis [17].
The hepatocyte growth factor (HGF) and c-Met-mediated epithelial mesenchymal mechanisms are important for follicle development [18]. HGF was reported as a growth factor that controls several key functions, including the regulation of growth and differentiation of ovarian follicles. It has been reported that the HGF/c-Met signalling modulates every major component of folliculogenesis, including steroidogenesis, the growth of theca and granulosa cells, and apoptosis of granulosa cells [19]. Nevertheless, it is currently unknown whether the HGF/c-Met signalling is involved in the development of immature oocytes in PCOS.
In one study [20], the levels of HGF in serum and in follicular fluid and the mRNA expression of c- Met in granulosa cells were slightly higher in patients with PCOS than in normal patients taken as control, and the same study showed that the increase in serum HGF levels after hCG treatment was similar in the PCOS patient and in control group with no PCOS assessment. Higher levels of HGF in serum and in follicular fluid and the increased c-Met expression in granulosa cells were important for the maturation and fertilization of oocytes, and the increased c-Met expression in granulosa cells might be a marker for the fertilization of oocytes [20].
In relation to PCOS and pregnancy, several studies indicate that women with PCOS have increased risk of adverse obstetric outcomes [21], with an increased risk of preeclampsia, pregnancy-induced hypertension, gestational diabetes, and preterm birth. Whether an increased risk of pregnancy complications has been related to PCOS, an increased BMI or fertility treatment is not fully understood.
Despite the diagnostic criteria, PCOS is still an unclear disease in terms of pathogenesis; both genetic and environmental factors may contribute to the onset of PCOS features [22]. On such genetic predisposition, environmental factors may play a key role, such as peculiar lifestyle, type of food, living condition, and also the impact during the intrauterine growth [23].
2 The Impact of Obesity on the Features of PCOS Patients
Although the pathogenesis of PCOS is complex and fully understood, insulin resistance and obesity are proposed to be key metabolic defects in its etiology [24].
Obesity and abdominal obesity are common in PCOS with 10–50 % of women with PCOS having a BMI above the acceptable range of 19–25 kg/m2 [25]. Both these enhance the features of insulin resistance and are associated with reproductive dysfunction including menstrual irregularity, increased serum androgens and luteinizing hormone (LH), infertility, and complications during pregnancy and childbirth [26, 27].
There is considerable evidence that a key etiologic feature of PCOS is the presence of insulin resistance, which is present in the majority of women with PCOS, although its severity varies between lean and obese women [28].
Insulin resistance is defined as the inability of insulin to exert its physiological effect. It is manifested peripherally (at the tissues level) or centrally (at the liver level) through a reduction in the ability of insulin to lower plasma glucose. This can be demonstrated as impaired insulin-stimulated glucose uptake and suppression of lipolysis at the muscles or adipose tissue, hepatic glucose overproduction, and suppression of glycogen synthesis. The mechanism implicated in the etiology of insulin resistance includes elevated levels of plasma free fatty acid, cytokines such as tumor necrosis factor alpha and interleukin 6, leptin, resistin, and the peroxisome proliferator-activated receptor gamma (PPAR gamma) [29].
The gold standard for detecting insulin resistance is the euglycemic clamp technique, where a constant infusion of insulin is maintained and glucose infusion is adjusted to maintain euglycemia [30].
At steady state, the insulin-mediated glucose disposal rate can be calculated by the amount of infused glucose representing that taken up by tissues. Using the euglycemic clamp technique, both lean and obese women with PCOS had significantly lower rates of insulin-mediated glucose uptake than weight-matched controls of comparable age, thus indicating greater insulin resistance [31]. Obesity and PCOS had additive and deleterious effects on insulin sensitivity. Other studies of insulin resistance in PCOS support the additive role of obesity on the level of insulin resistance seen [32].
The impact of insulin in the presence of obesity in PCOS is particularly notable in high rates of glucose intolerance and diabetes seen in obese women with PCOS [33]. Glucose abnormalities may be detected by measurement of the fasting glucose; however, this method may be less sensitive in obese women with PCOS. A significant number of women with PCOS demonstrating glucose intolerance on a 2 h glucose challenge will have normal fasting glucose level according to the American Diabetes Association (ADA) criteria [33, 34].
Evidence exists that an android body fat distribution (i.e., a central distribution of body fat) induces higher risk of cardiovascular disease and diabetes than does a gluteofemoral fat distribution [34, 35]. In particular, visceral adipose tissue exhibits functional differences in comparison to subcutaneous adipose tissue when studied in vitro [36]. Production of adipocyte-associated cytokines, such as adiponectin and leptin, as well as inflammatory markers such as IL6, varies between the two adipocyte compartments [37]. Under conditions of visceral fat accumulation, these compartmental differences may contribute to the association between visceral fat and insulin resistance [38].
Women with PCOS tend to accumulate fat in a central distribution as demonstrated by increased waist-to-hip ratio [39]. In PCOS, this increase in visceral fat is associated with a worse metabolic profile, with higher fasting insulin levels, dyslipidemia, and higher serum androgen concentrations [40]. Central fat mass correlates with serum levels of inflammatory markers such as C-reactive protein, independently of age and total fat mass as reported in a recent study on PCOS and BMI-matched controls [41]. Modest alterations, therefore, in the visceral fat compartment may produce a significant impact on metabolic parameters.
The predominant underlying risk factor for development of metabolic syndrome is abdominal obesity and likely represents a consequence of insulin resistance. Patients with PCOS has been reported to have an increased risk of metabolic syndrome (MS), which refers to a clustering within the same individual of hyperinsulinemia, mild to severe glucose intolerance, dyslipidemia, and hypertension, and an increased risk for cardiovascular disease and diabetes [42]. The prevalence of metabolic syndrome in PCOS ranges from 33.4 to 47.3 % in published trials [43]. In 2006, the International Diabetes Federation defined the features of the MS and defined central obesity as present when the waist circumference is above 80 cm; in European women, this was considered as a necessary prerequisite risk factor for the diagnosis of MS [44].
The risk factors for MS are as follows:
-
Waist circumference >88 cm
-
Elevated triglycerides >150 mg/dL (>1.7 mmol/l)
-
Reduced HDL cholesterol <50 mg/dL (<1.29 mmol/l)
-
Elevated blood pressure untreated >130 mmHg systolic or >85 mmHg diastolic
-
Fasting plasma glucose >100 mg/dL (over 5.6 mmol/l) or previous diagnosis of type 2 diabetes mellitus
Women with PCOS have lower HDL levels, higher LDL to HDL ratio, and higher triglyceride levels than healthy eumenorrheic women. All these are inductors of subclinical atherosclerosis as demonstrated by the increased thickness of the carotid intima media and by the higher endothelial dysfunction observed in PCOS patients [9], probably related to the insulin resistance and/or to the higher free testosterone plasma level [45].
The impact of metabolic syndrome on the presence of cardiovascular morbidity in PCOS has not been studied; as metabolic syndrome is recognized as a significant risk factor for cardiovascular disease in the general population, obese women with PCOS with metabolic syndrome would appear to be at increased risk as well [46]. Such risk has also been demonstrated to be higher in postmenopausal women, previously demonstrated to be PCOS during fertile life [47].
3 Endocrine Profile of PCOS Patients
PCOS is characterized by increased ovarian and adrenal androgens, increased luteinizing hormone (LH) levels, high estrogen levels (mainly estrone) due to extraglandular conversion from androgens, lower levels of sex hormone binding protein (SHBG), and higher levels of insulin, the latter often present in overweight or obesity. Hyperandrogenism is a key feature of the syndrome, although it is not constant [48]. It is mainly of ovarian origin with an adrenal contribution, since a certain percentage of PCOS women might show a mild steroidogenetic defect in adrenal glands (such as for 21-hydroxylase) or just a higher adrenal hyperactivation due to stress [49].
Androstenedione and testosterone are the markers of androgen secretion from the ovary, whereas dehydroepiandrosterone sulfate (DHEAS) is the best markers of adrenal secretion. The great part of testosterone is derived from peripheral conversion of androstenedione and from direct ovarian production. Dysregulation of cytochrome p450c17, the androgen-forming enzyme in both the adrenal glands and the ovaries, is the central pathogenic mechanism underlying hyperandrogenism in PCOS patients [50].
Hyperandrogenism correlates positively with insulin resistance, and obesity worsens insulin resistance. Additionally, obesity is associated with lower concentrations of SHBG that is the major binding protein for testosterone. Normally, less than 3 % of testosterone circulates as unbound in the serum. The presence of hyperandrogenism reduces the hepatic synthesis of SHBG and leads to a relative excess of free circulating androgens. In PCOS, hirsutism usually occurs with decreased SHBG levels and obesity [51].
Moreover, estrone plasma levels, a weak estrogen with biological activity 100 times less than estradiol, are increased as the result of peripheral conversion of androstenedione by aromatase activity. Excess of estrone leads to a hyperestrogenic state, and this might predispose patient to endometrial proliferation and to a higher risk for endometrial cancer [52].
Compared to normal women, women with PCOS had an accelerated LH pulse pattern. However, when obese women with PCOS were studied in comparison to lean PCOS women, an attenuated pattern of LH secretion was noted in the obese women. Twenty four hours mean LH concentrations have also been noted to be lower with increasing BMI in obese women [53].
Overall obesity appears to exert a significant, although modest, impact on hyperandrogenism in PCOS, mediated primarily via impact on free hormone concentration. There is also evidence of attenuation of LH secretion with obesity resulting in a lower LH to FSH ratio. Hirsutism is reported more frequently in obese women with PCOS, consistent with the impact of higher free androgen concentration.
A great percentage of PCOS patients are overweight to severely obese, and any excess of weight can induce a reduction of peripheral tissue sensitivity to insulin, thus inducing the compensatory hyperinsulinism. Hyperinsulinemia might be central in the pathogenesis of the syndrome because it can induce higher ovarian androgen production and anovulation [54], sustained also by the abnormal LH secretion, with a higher frequency of menstrual abnormalities than in normoinsulinemic PCOS patients [55]. Insulin resistance and compensatory hyperinsulinemia are metabolic disturbances easily observable in at least 45–65 % of PCOS patients and frequently appear to be related to excessive serine phosphorylation of the insulin receptor [56].
4 Lifestyle Modification in PCOS Treatment
One of the primary goals of treatment in PCOS is the normalization of serum androgens and restoration of reproductive function; however, the presence of metabolic disturbance has become a prominent feature of the disease that may interfere with long-term health.
In non-PCOS subjects, weight loss and exercise reduce insulin resistance, plasma lipids, and blood pressure. In PCOS, therapeutic use of insulin sensitizing agents normalizes hyperinsulinemia and hyperandrogenism. However, management of lifestyle factors, where possible, is preferable to pharmacological management because of potential costs, side effects, and long-term maintenance. Metabolic abnormalities are significantly increased by obesity in PCOS, with high prevalence rates of impaired glucose tolerance and diabetes as well as dyslipidemia.
In PCOS, caloric restriction improves insulin sensitivity measured through euglycemic clamps, fasting glucose/insulin ratios, homeostasis model assessment (HOMA), OGTT stimulated insulin, and fasting insulin. Weight loss in obese women with PCOS has been demonstrated to reduce hyperlipidemia, in particular total cholesterol and triglycerides levels and plasminogen activator inhibitor-1 (PAI-1) activity, a marker of impaired fibrinolysis and atherothrombosis [57]. Weight loss also decreases ovarian cytochrome P450 c17 alpha activity and reduces basal adipocyte lipolysis.
Pasquali et al. studied obese PCOS women undergoing a hypocaloric diet with or without metformin administration [58]. A 12.3 % reduction in visceral fat was noted in those treated with diet alone versus 2.5 % reduction in subcutaneous fat. This suggests that there is a great sensitivity to reduction in the more metabolically active visceral component of adipose tissue with energy restriction.
Weight reduction in PCOS women improves insulin sensitivity as measured by euglycemic clamp studies [59]. Both insulin values of a 2 h oral glucose tolerance test [60] and fasting insulin parameters [61] have been shown to improve with weight reduction in PCOS patients.
Hyperandrogenism is one of the defining characteristics of PCOS and it is a relevant target for treatment in PCOS women. Hirsutism, a common clinical sign of PCOS, has been noted to be worsened in obese PCOS patients [62]. Serum testosterone and free androgen index are also increased in these types of patients [63]. Pasquali et al., after 3 months of treatment, did not show any change in sex steroid concentration in obese PCOS women [64].
In contrast, other studies, have demonstrated improvements in serum androgens or in SHBG levels, with decrease in free testosterone levels [65], and improvement in hirsutism [66]. Although altered gonadotropin secretion has been demonstrated in PCOS, studies evaluating weight loss have not demonstrated restoration of normal gonadotropin secretion. No improvements in LH pulsatility were found after weight loss as shown by Guzick et al. [61].
Van Dam et al. [67] studied women with PCOS after short-term dietary restriction with 24 h frequent sampling. They demonstrated an increased LH basal and pulsatile secretion, although they did demonstrate a 23 % reduction in serum testosterone. Overall these data indicate that reductions in androgens observed after weight loss may not be mediated by changes of pulsatile gonadotropin secretion but perhaps through other mechanisms such as changes in insulin sensitivity at the pituitary level.
Modest weight loss has been shown to have a significant effect in improving menstrual cycles and ovulation in PCOS [61]. There are no randomized data on the impact that modest weight reduction has on the live birth rate, either with pregnancies resulting from spontaneous ovulation or in response to fertility treatment. Lifestyle modification also reduces the long-term risk of diabetes, heart disease, and possible endometrial cancer in PCOS women.
Useful changes include the following: dietary modification with reduction in calories by limiting daily intake to 1,400 kcal with low daily intake of simple and complex sugar and increased in protein intake, low intake of sugary drinks, avoid snacking between meals, and increase intake of low glycemic index fruits and vegetables. Other important lifestyle modifications are smoking cessation, moderate alcohol/caffeine intake, and regular moderate daily exercise (at least 30 min a day at the very least).
Some studies [68] have shown that lifestyle changes (in this case, intensive exercise with a goal of over 150 min/week of activity) resulting in weight loss reduced the risk of type 2 diabetes [69]. The same studies found lifestyle changes to be superior to metformin administration. Thus, all women with PCOS should be encouraged to follow a healthy diet to engage in regular exercise. Their lifestyle changes to achieve pregnancy will improve and the risks during pregnancy will be reduced. A healthier lifestyle will also reduce their long-term risk of diabetes, hypertension, dyslipidemia, and cardiovascular diseases. It is important for all primary care providers to identify patients who may have PCOS. These patients need to undergo the appropriate screening tests and should be counselled about diet and exercise. Pharmacological intervention could be combined with this approach as appropriate, but the abovementioned studies suggest that lifestyle modification is the first-line treatment.
5 Use of Insulin Sensitizer Agents and Inositol in PCOS Treatment
The logic for use of insulin sensitizer drugs, such as metformin, to treat PCOS patients is the fact that about 45–65 % of these patients have been demonstrated to have insulin resistance and a compensatory hyperinsulinemia that negatively affect ovarian function in terms of steroidogenesis and follicular recruitment and maturation [21].
Excess insulin increases androgen concentrations blocking follicular maturation and increasing cytochrome P450 c17a activity, a key enzyme in the synthesis of both ovarian and adrenal androgens [21]. This situation typically increases 17-hydroxyprogesterone (17OHP), androstenedione, and testosterone plasma levels. The excess of intraovarian androgens negatively modulates follicular function and ovarian activity, thus inducing the typical stromal hypertrophy and maintaining ovarian atresia and anovulation [21].
The use of metformin might be suggested when abnormal insulin sensitivity is diagnosed [70]. Metformin reduces hepatic glucose production from 9 to 30 % on peripheral tissues, such as muscle cells and adipocytes, and acts by increasing glucose uptake through the glucose transport system.
Metformin positively acts on hormonal PCOS abnormalities through a direct and/or indirect action on steroidogenesis [21]; the recovery of normal ovulatory function is probably due to the direct action of metformin on the ovarian tissues and to the metformin-induced normalization of the ovarian steroidogenesis with normal feedback on the pituitary gland, lowering LH secretion and restoring LH pulse secretion. Metformin improves ovarian and adrenal steroidogenesis; in fact, insulin plays specific modulatory roles on these two glands that have the same enzymatic pathways [71].
The use of insulin sensitizers do not reduce hyperandrogenism better than oral contraceptive [72], but as recently reported, the typology of PCOS to be treated is of great relevance, since only when insulin sensitivity is abnormal metformin shows a greater efficacy on all the PCOS features including hyperandrogenism [73]. Other metabolically active hormones such as leptin, resistin, adiponectin, and ghrelin are positively activated by metformin administration and thus participate in the improvement of the reproductive function at the hypothalamus-pituitary-ovarian level.
In the last years, a higher attention has been given to the role of inositol-phosphoglycan (IPG) mediators of insulin action [74], and growing evidences suggest that a deficiency of D-chiro-inositol (DCI) containing IPG might be at the basis of insulin resistance, frequent in PCOS patients. PCOS patients have high urinary clearance of DCI [75] and that metformin administration in obese PCOS patients improves the release of DCI-IPG mediator [76].
DCI is synthesized by an epimerase that converts myo-inositol into DCI and, depending on the specific needs of the two molecules, each tissue has a typical conversion rate [77]. Considering that ovaries never become insulin resistant and being MYO administration able to induce regular menses in both lean and obese hyperinsulinemic PCOS patients [74], a possible modulatory role of MYO on the insulin-mediated endocrine effects has been hypothesized [74]. Recent studies suggest that some abnormal action of insulin might be dependent from IPG mediators of insulin action and suggest that a deficiency in a specific DCI-containing IPG may underlie insulin resistance, similarly to type 2 diabetes. DCI administration has been demonstrated to reduce insulin resistance both in lean and obese patients with PCOS improving ovarian function and decreasing hyperandrogenism [78]. Such studies suggested the putative presence of a defect in the insulin signalling pathway in which DCI-PG is the mediator of insulin action, thus contributing to the pathophysiology of the insulin resistance of PCOS [75]. Besides DCI, MYO has been reported to be greatly correlated to ovarian function [79] and oocyte quality in patients undergoing IVF procedures, independently from circulating plasma levels [80]. Such data support a specific role also for MYO on gonadotropin-induced ovarian function [81] though not confirmed by others [75].
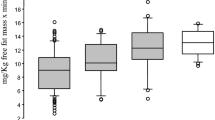
MYO administration has been demonstrated to modulate insulin sensitivity in overweight PCOS patients improving all hormonal parameters and improving insulin sensitivity [74, 81]. The daily dosage of 2 g in the morning has been reported to be effective in hyperinsulinemic obese PCOS patients with fasting insulin levels above 12 mU/ml [81]. Such insulin level seems to be a putative cutoff that suggests when MYO administration might give higher chances of success not only on hormonal parameters but also on hyperinsulinemia and insulin sensitivity [81].
In conclusion, PCOS is a complex syndrome, with hormonal and metabolic aspects, and the therapeutical approach for PCOS patients needs to consider these two aspects together. Metformin as well as inositol integrative administration might be easily used to solve the metabolic aspects of PCOS impairments. Lifestyle as well as hormonal treatments has to be considered relevant therapeutic tools to be used together with insulin sensitizer drugs.
References
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic-ovary syndrome. Fertil Steril 81:19–25
Zawadski JK, Dunaif A (1992) Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens JR, Haseltien FP, Merriam GR (eds) Polycystic ovary syndrome. Blackwell, Boston, pp 337–384
Azziz R, Carmina E, Dewailly D, Androgen Excess Society et al (2006) Position statement: criteria for defining polycystic ovary syndrome: an androgen excess society guideline. J Clin Endocrinol Metab 91:4237–4245
Carmina E, Lobo RA (1999) Polycystic ovary syndrome: arguably the most common endocrinopathy is associated with significant morbidity in women. J Clin Endocrinol Metab 84:1897–1899
Zboroeski JV, Cauley JA, Talbott EO et al (2000) Bone mineral density, androgens, and the polycystic ovary: the complex and controversial issue of androgenic influence in female bone. J Clin Endocrinol Metab 85:3496–3506
Carmina E, Lobo RA (2004) Use of fasting blood to assess the prevalence of insulin resistance in women with polycystic ovary syndrome. Fertil Steril 82:661–665
Catalano PM, Presley L, Minium J, Hauguel-de Mouzon S (2009) Fetuses of obese mothers develop insulin resistance in utero. Diabetes Care 32:1076–1080
Kebapcilar L, Taner CE, Kepapcilar AG, Sari I (2009) High mean platelet volume, low grade systemic coagulation and fibrinolytic cavitation are associated with androgen and insulin levels in polycystic ovary syndrome. Arch Gynecol Obstet 280:187–193
Talbott EO, Guzick DS, Sutton Tyrell K, McHugh Pemu KP, Zborowski JV, Remsberg KE, Kuller LH (2000) Evidence for association between polycystic ovary syndrome and premature carotid atherosclerosis in middle-aged women. Arterioscler Thromb Vasc Biol 20:2014–2421
Oral B, Mermi B, Dilek M, Alanoglu G, Sutcu R (2009) Thrombin activatable fibrinolysis inhibitor and other hemostatic parameters in patients with polycystic ovary syndrome. Gynecol Endocrinol 25:110–116
Dahlgren E, Janson PO, Johansson S, Lapidus L, Lindstedt G, Tengborn L (1994) Hemostatic and metabolic variables in women with polycystic ovary syndrome. Fertil Steril 61:455–460
Genazzani AD, Santagni S, Ricchieri F, Campedelli A, Rattighieri E, Chierchia E, Marini G, Despini G, Prati A, Simoncini T (2014) Myo-inositol modulates insulin and luteinizing hormone secretion in normal weight patients with polycystic ovary syndrome. J Obstet Gynaecol Res. doi:10.1111/jog.12319
Repaci A, Gambineri A, Pasquali R (2011) The role of low-grade inflammation in the polycystic ovary syndrome. Mol Cell Endocrinol 335:30–41
Heijnen EM, Eijkemans MJ, Hughes EG, Laven JS, Macklon NS, Fausen BC (2006) A meta-analysis of outcomes of conventional IVF in women with polycystic ovary syndrome. Hum Reprod Update 12:13–21
Vlaisavljevic V, Kovac V, Sajko MC (2009) Impact of insulin resistance on the developmental potential of immature oocytes retrieved from human chorionic gonadotropin-primed women with polycystic ovary syndrome undergoing in vitro maturation. Fertil Steril 91:957–959
Franks S, Stark J, Hardy K (2008) Follicle dynamics and anovulation in polycystic ovary syndrome. Hum Reprod Update 14:367–378
Wang TH, Chang CL, Wu HM, Chiu YM, Chen CK, Wang HS (2006) Insulin like growth factor II, IGF- binding protein 3, and IGFBP 4 in follicular fluid are associated with oocyte maturation and embryo development. Fertil Steril 67:1846–1852
Guglielmo MC, Ricci G, Catizone A, Barbieri M, Gardieri M, Stefanini M et al (2011) The effect of hepatocyte growth factor on the initial stages of mouse follicle development. J Cell Physiol 226:520–529
Uzumcu M, Pan Z, Chu Y, Kuhn PE, Zachow R (2006) Immunolocalization of the hepatocyte growth factor system in the rat ovary and the anti apoptotic effect of HGF in rat ovarian granulose cells in vitro. Reproduction 132:291–299
Nur Sahin MD, Asli Toylu MD, Bulent Gulekli MD et al (2013) The levels of hepatocyte growth factor in serum and follicular fluid and the expression of c-Met in granulosa cells in patients with polycystic ovary syndrome. Fertil Steril 99:264–270
Palomba S, Falbo A, Russo T, Tolino A, Orio F, Zullo F (2010) Pregnancy in women with polycystic ovary syndrome: the effect of different phenotypes and features on obstetric and neonatal outcomes. Fertil Steril 94:1805–1811
Palomba S, Falbo A, Zullo F, Orio F (2009) Evidence based and potential benefits of metformin in the polycystic ovary syndrome: a comprehensive review. Endocr Rev 30:1–50
Deligeoroglou E, Kouskouti C, Christopoulos P (2009) The role of genes in the polycystic ovary syndrome: predisposition and mechanism. Gynecol Endocrinol 25:603–609
Ehrmann DA (2005) Polycystic ovary syndrome. N Engl J Med 352:1223–1236
Kiddy DS, Sharp PS, White DM et al (1990) Differences in clinical and endocrine features between obese and non obese subjects with polycystic ovary syndrome: an analysis of 263 consecutive cases. Clin Endocrinol (Oxf) 32(2):213–220
Sebire NJ, Jolly M, Harris JP (2001) Maternal obesity and pregnancy outcome: a study of 287 213 pregnancies in London. Int J Obes Relat Metab Discord 25(8):1175–1182
Pasquali R, Casimirri F, Venturoli S et al (1994) Body fat distribution has weight independent effects on clinical, hormonal and metabolic features of women with polycystic ovary syndrome. Metabolism 43(6):706–713
Dunaif A (1997) Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev 18(6):774–800
Kahn BB, Flier JS (2000) Obesity and insulin resistance. J Clin Invest 106:473–481
Monzillo LU, Hamby O (2003) Evaluation of insulin sensitivity in clinical practice and in research settings. Nutr Rev 61(12):397–412
Dunaif A, Segal KR, Futterweit W et al (1989) Profound peripheral insulin resistance, independent of obesity in polycystic ovary syndrome. Diabetes 38(9):1165–1174
Ciampelli M, Fulghesu AM, Cucinelli F et al (1999) Impact of insulin and body mass index on metabolic and endocrine variables in polycystic ovary syndrome. Metabolism 48(2):167–172
Legro RS, Kunselman AR, Dodson WC (1999) Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab 84(1):165–169
Qiao Q, Tuomilehto J (2001) Diagnostic criteria of glucose intolerance and mortality. Minerva Med 92(2):113–119
Van Pelt RE, Jankowski CM, Gozansky WS (2005) Lower body adiposity and metabolic protection in postmenopausal women. J Clin Endocrinol Metab 90(8):4573–4578
Frayn KN (2000) Visceral fat and insulin resistance- causative or correlative? Br J Nutr 83(suppl):S71–S77
Havel PJ (2004) Update on adipocyte hormones: regulation of energy balance and carbohydrate/lipid metabolism. Diabetes 83(suppl):S143–S151
Giorgino F, Laviola L, Eriksson JW (2005) Regional differences of insulin action in adipose tissues: insights from in vivo and in vitro studies. Acta Physiol Scand 183(1):13–30
Rebuffe Scrive M, Cullberg G, Lundberg PA (1989) Anthropometric variables and metabolism in polycystic ovarian disease. Horm Metab Res 21(7):391–397
Norman RJ, Masters SC, Hague W (1995) Metabolic approaches to the subclassification of polycystic ovary syndrome. Fertil Steril 63(2):329–335
Puder JJ, Varga S, Kraenzlin M (2005) Central fat excess in polycystic ovary syndrome: relation to low grade inflammation and insulin resistance. J Clin Endocrinol Metab 90(11):6014–6021
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ (2010) The metabolic syndrome. Lancet 375(9710):181–183
Ehrmann DA, Lijenquist DR, Kasza K, Azziz R, Legro RS, Ghazzi MN, PCOS/Troglitazone Study Group (2006) Prevalence and predictors of the metabolic syndrome in women with polycystic ovary syndrome (PCOS). J Clin Endocrinol Metab 91:48–53
International Diabetes Federation (2006) The International Diabetes Federation consensus worldwide definition of the metabolic syndrome. International Diabetes Federation, Brussels
Lusher TF, Richard V, Tshudi M, Yang ZH, Boulanger C (1990) Endothelial control of vascular tone in large and small coronary arteries. J Am Coll Cardiol 15:519–527
Muniyappa R, Montagnani M, Koh KK, Quon MJ (2007) Cardiovascular actions of insulin. Endocr Rev 28:463–491
Carmina E (2009) Cardiovascular risk and events in polycystic ovary syndrome. Climacteric 12(suppl 1):22–25
Hirschberg AL (2009) Polycystic ovary syndrome, obesity and reproductive implications. Womens Health 5:529–540
Genazzani AD, Petraglia F, Pianazzi F, Volpogni C, Genazzani AR (1993) The concomitant release of androstenedione with cortisol and luteinizing hormone pulsatile releases distinguishes adrenal from ovarian hyperandrogenism. Gynecol Endocrinol 7:33–41
Vrbikova J, Hainer V (2009) Obesity and polycystic ovary syndrome. Obes Facts 2:26–35
Plouffe L (2000) Disorders of excessive hair growth in the adolescent. Obstet Gynecol Clin North Am 27:79–99
Chittenden BG, Fullerton G, Maheshwari A, Bhattacharya S (2009) Polycystic ovary syndrome and the risk of gynaecological cancer: a systematic review. Reprod Biomed Online 19:398–405
Arroyo A, Laughlin GA, Morales AJ, Yen SS (1997) Inappropriate gonadotropin secretion in polycystic ovary syndrome: influence of adiposity. J Clin Endocrinol Metab 82(11):3728–3733
Barbieri RL (2000) The role of adipose tissue and hyperinsulinemia in the development of hyperandrogenism in women. In: Frisch RE (ed) Adipose tissue and reproduction. Karger, Basel, pp 42–57
Conway GS, Jacobs HS, Holly JM, Wass JA (1990) Effects of LH, insulin, insulin like growth factor I and insulin like growth factor small binding protein I in the polycystic ovary syndrome. Clin Endocrinol (Oxf) 33:593–603
Dunaif A, Givens JR, Haseltine F et al (1992) The polycystic ovary syndrome. Blackwell, Boston
Andersen P, Selieflot I, Abdel Noor M (2001) Increased insulin sensitivity and fibrinolytic capacity after dietary intervention or metformin. N Engl J Med 344(18):1343–1350
Pasquali R, Gambineri A, Biscotti D et al (2000) Effect of long term treatment with metformin added to hypocaloric diet on body composition, fat distribution and androgen and insulin levels in abdominally obese women with or without the polycystic ovary syndrome. J Clin Endocrinol Metab 85(8):2767–2774
Huber Buchholz MM, Carey DG, Norman RJ (1999) Restoration of reproductive potential by lifestyle modification in obese polycystic vary syndrome: role of insulin sensitivity and luteinizing hormone. J Clin Endocrinol Metab 84(4):1470–1474
Pasquli R, Casimirri F, Colella P, Melchionda N (1989) Body fat distribution and weight loss in obese women. Am J Clin Nutr 49(19):185–187
Guzick DS, Wing R, Smith D (1994) Endocrine consequences of weight loss in obese, hyperandrogenic anovulatory women. Clin Endocrinol (Oxf) 61(4):598–604
Franks S, Kiddy D, Sharp P (1991) Obesity and polycystic ovary syndrome. Ann N Y Acad Sci 626:201–206
Holte J, Bergh T, Gennarelli G, Wide L (1994) The independent effects of polycystic ovary syndrome and obesity ion serum concentrations of gonadotropins and sex steroids in premenopausal women. Clin Endocrinol (Oxf) 41(4):473–481
Pasquali R, Fabbri R, Venturoli S et al (1986) Effects of weight loss and antiandrogenic therapy on sex hormone blood levels and insulin resistance in obese patients with polycystic ovaries. Am J Obstet Gynecol 154(1):139–144
Kiddy DS, Hamilton Fairley D, Seppala M et al (1989) Diet induced changes in sex hormone binding globulin and free testosterone in women with normal or polycystic ovaries: correlation with serum insulin and insulin like growth factor I. Clin Endocrinol (Oxf) 31(6):757–763
Kiddy DS, Hamilton Fairley D, Bush A et al (1992) Improvement in endocrine and ovarian function during dietary treatment of obese women with polycystic ovary syndrome. Clin Endocrinol (Oxf) 36(1):105–111
Van Dam EW, Roelfsema F, Veldhuis JD (2002) Increase in daily LH secretion in response to short term calorie restriction in obese women with PCOS. Am J Physiol Endocrinol Metab 282(4):E865–E872
Tang T, Glanville J, Hayden CJ (2006) Combined lifestyle modification and metformin in obese patients with polycystic ovary syndrome. A randomized placebo controlled double blind multicentre study. Hum Reprod 21:80–89
Kitabchi AE, Temprosa M, Knowler WC (2005) Role of insulin secretion and sensitivity in the evolution of type 2 diabetes in the diabetes prevention program: effects of lifestyle intervention and metformin. Diabetes 54:2404–2414
Nieuwenhuis Ruifrok AE, Kuchenbecker WK, Hoek A, Middleton P, Norman RJ (2009) Insulin sensitizing drugs or weight loss in women of reproductive age who are overweight or obese; systematic review and meta analysis. Hum Reprod Update 15:57–68
La Marca A, Morgante G, Paglia T, Ciotta L, Cianci A, De Leo V (1999) Effects of metformin on adrenal steroidogenesis in women with polycystic ovary syndrome. Fertil Steril 72:985–989
Cosma M, Swiglo BA, Flynn DN et al (2008) Insulin sensitizers for the treatment of hirsutism: a systematic review and metaanalyses of randomized controlled trials. J Clin Endocrinol Metabol 93:1135–1142
Genazzani AD, Lanzoni C, Ricchieri F, Baraldi E, Csarosa E, Jasonni VM (2007) Metformin administration is more effective when non obese patients with polycystic ovary syndrome show both hyperandrogenism and hyperinsulinemia. Gynecol Endocrinol 23:146–152
Genazzani AD, Lanzoni C, Ricchieri F, Jasonni VM (2008) Myoinositol administration positively affects hyperinsulinemia and hormonal parameters in overweight patients with polycystic ovary syndrome. Gynecol Endocrinol 24:139–144
Baillargeon JP, Diamanti Kandarakis E, Ostlund RE, Apridonidze T, Iuorno MJ, Nestler JE (2006) Altered D-chiro-inositol urinary clearance in women with polycystic ovary syndrome. Diabetes Care 29:300–305
Baillargeon JP, Iuorno MJ, Jakubowicz DJ, Apridonidze T, He N, Nestler JE (2004) Metformin therapy increases insulin stimulated release of D-chiro-inositol containing inositolphosphoglycan mediator in women with polycystic ovary syndrome. J Clin Endocrinol Metabol 89:242–249
Larner J (2002) D chiro-inositol, its functional role in insulin action and its deficit in insulin resistance. Int J Exp Diabetes Res 3:47–60
Nestler JE, Jakubowicz DJ, Reamer P, Gunn RD, Allan G (1999) Ovulatory and metabolic effects of D chiro inositol in the polycystic ovary syndrome. N Engl J Med 340:1314–1320
Gerli S, Mignosa M, Di Renzo GC (2003) Effects of inositol on ovarian function and metabolic factors in women with PCOS: a randomized double blind placebo controlled trial. Eur Rev Med Pharmacol Sci 7:151–159
Chiu TTY, Rogers MS, Law ELK, Briton Jones CM, Cheung LP, Haines CJ (2002) Follicular fluid and serum concentrations of myo-inositol in patients undergoing IVF: relationship with oocyte quality. Hum Reprod 6:1591–1596
Genazzani AD, Ricchieri F, Prati A, Santagni S, Chierchia E, Rattichieri E, Campedelli A, Simoncini T, Artini PG (2012) Differential insulin response to myoinositol administration in obese PCOS patients. Gynecol Endocrinol 28:969–973
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 International Society of Gynecological Endocrinology
About this chapter
Cite this chapter
Genazzani, A.D. et al. (2015). PCOS and Insulin Resistance (IR): From Lifestyle to Insulin Sensitizers. In: Fauser, B.C.J.M., Genazzani, A.R. (eds) Frontiers in Gynecological Endocrinology. ISGE Series. Springer, Cham. https://doi.org/10.1007/978-3-319-09662-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-09662-9_2
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09661-2
Online ISBN: 978-3-319-09662-9
eBook Packages: MedicineMedicine (R0)