Abstract
Heart failure (HF) is the leading cardiovascular (CV) complication in patients with chronic kidney disease (CKD) and its prevalence increases with declining kidney function [1]. In the Atherosclerosis Risk in Communities (ARIC) Study [2], a large, population-based study of U.S. adults, the incidence of HF was three-fold higher in individuals with an estimated glomerular filtration rate (GFR) <60 mL/min/1.73 m2, compared with the reference group with an estimated GFR ≥90 mL/min/1.73 m2. According to the 2009 U.S. Renal Data System (USRDS) Annual Report Data [3], the prevalence of HF in the elderly U.S. population (>65 years-old) was 7.4 % in non-CKD individuals, whereas in patients with CKD stages 4 and 5 this percentage raised to 42 %. In dialysis patients, the prevalence of HF ranges from 30 to 40 % [4–7]. In a study by Harnett et al. [7], almost one-third of end-stage renal disease (ESRD) patients had HF at initiation of dialysis and more than half of these manifested recurrence of HF later on, whereas among patients without previous HF, 25 % subsequently developed HF during dialysis. However, the Dialysis Outcomes and Practice Patterns Study (DOPPS) showed considerable geographic variability in the prevalence of HF in hemodialysis populations – namely, 46 % in the U.S., but only 25 % in Europe and as low as 6 % in Japan [8]; to some extent, such differences may be explained by the fact that the U.S. patients were older and had more diabetes, coronary artery disease and other vascular diseases than their European and Japanese counterparts.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Heart Failure
- Chronic Kidney Disease
- Heart Failure Patient
- Brain Natriuretic Peptide
- Chronic Kidney Disease Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Heart failure (HF) is the leading cardiovascular (CV) complication in patients with chronic kidney disease (CKD) and its prevalence increases with declining kidney function [1]. In the Atherosclerosis Risk in Communities (ARIC) Study [2], a large, population-based study of U.S. adults, the incidence of HF was three-fold higher in individuals with an estimated glomerular filtration rate (GFR) <60 mL/min/1.73 m2, compared with the reference group with an estimated GFR ≥90 mL/min/1.73 m2. According to the 2009 U.S. Renal Data System (USRDS) Annual Report Data [3], the prevalence of HF in the elderly U.S. population (>65 years-old) was 7.4 % in non-CKD individuals, whereas in patients with CKD stages 4 and 5 this percentage raised to 42 %. In dialysis patients, the prevalence of HF ranges from 30 to 40 % [4–7]. In a study by Harnett et al. [7], almost one-third of end-stage renal disease (ESRD) patients had HF at initiation of dialysis and more than half of these manifested recurrence of HF later on, whereas among patients without previous HF, 25 % subsequently developed HF during dialysis. However, the Dialysis Outcomes and Practice Patterns Study (DOPPS) showed considerable geographic variability in the prevalence of HF in hemodialysis populations – namely, 46 % in the U.S., but only 25 % in Europe and as low as 6 % in Japan [8]; to some extent, such differences may be explained by the fact that the U.S. patients were older and had more diabetes, coronary artery disease and other vascular diseases than their European and Japanese counterparts.
The presence of HF at the start of dialysis is a strong and independent predictor of short-term [9] and long-term mortality, in both hemodialysis [7] and peritoneal dialysis patients [10]. The median survival of dialysis patients with baseline HF has been estimated to be 36 months, in contrast with 62 months for those without baseline HF [7]. Over 80 % of ESRD patients recently diagnosed with HF are expected to die within only 3 years from the time of this diagnosis [11].
Finally, it must be noted that the relationship between CKD and HF is reciprocal, i.e. renal impairment is very common among patients with HF, as well. In recent cohort studies and randomized controlled trials, CKD was detected in 35–70 % of HF patients [12]. For example, in a study by de Silva et al. [13] of 1,216 patients with chronic stable HF, only 7 % had an estimated GFR ≥90 mL/min/1.73 m2. The presence of CKD is associated with an increased hospitalization rate for worsening HF and all-cause and CV mortality; the hazard ratio for all-cause mortality in HF patients with CKD is about 1.3–2.9 compared to those without CKD [12]. Patients with HF have a 1 % increase in mortality for each 1-mL/min decrease in GFR [14]. Moreover, it was shown that GFR is the most powerful predictor of mortality in patients with HF, ahead of functional status and ejection fraction (EF) [15].
The treatment of HF in patients with CKD is unclear, as there is very little strong evidence to support any recommendations. Guidelines for the management of HF in the general population may not apply entirely to those with CKD, since such patients (particularly those with severe renal impairment) were quite often excluded from most of the RCTs that served as a rationale for these guidelines. The paucity of specific evidence and recommendations may explain why CKD patients with HF are less likely to receive certain therapies that are commonly used in the general HF population. Wang and Sanderson [16] pointed out that the main objectives of HF therapy in CKD (as well as in non-CKD) patients are the following: (1) to decrease the preload and afterload and to reduce left ventricular hypertrophy (LVH); (2) to treat myocardial ischemia; and (3) to inhibit neurohumoral hyperactivity, especially the sympathetic nervous system and the renin-angiotensin-aldosterone system (RAAS).
The rationale for RAAS blockade therapy in CKD patients with HF is supported by many pathophysiological considerations. Excess angiotensin II can accumulate in the heart and promote myocyte hypertrophy, interstitial fibrosis, microvascular disease, as well as cardiac conduction disturbances, QT prolongation, and arrhythmias [17]. Additionally, high serum aldosterone, resulting from activation of renin-angiotensin system or other pathways, can induce myocardial fibrosis, possibly by release of transforming growth factor β [18, 19].
Angiotensin-Converting Enzyme Inhibitors
A subject of many studies, the mechanisms of angiotensin-converting enzyme inhibitors (ACEIs) in HF are complex and still not completely understood. By blocking the conversion of angiotensin I to angiotensin II, these drugs promote vasodilation (by reducing the vasoconstrictive effect of angiotensin II) and renal sodium excretion (by decreasing aldosterone release). They inhibit the cardiac RAAS, which is involved in LV hypertrophy and dysfunction. They also block the degradation of bradykinins, thereby stimulating the synthesis of prostaglandins and nitric oxide, which seem to prevent LVH, as well. Other significant effects of ACEIs include the reduction of sympathetic activity, improvement of endothelial function, decrease of proinflammatory cytokines and prothrombotic factors, and stimulation of fibrinolytic factors. All these mechanisms contribute to the improvement of pulmonary, right ventricular and skeletal muscle function, and the increase of arterial compliance [20].
ACEIs have been evaluated in more than 7,000 patients with systolic HF, in over 30 placebo-controlled clinical trials. Analyses of these studies showed that these drugs can alleviate symptoms, improve functional status, and reduce the risk of death and hospitalization. These benefits were seen in patients with various severity and causes of HF. U.S. and European guidelines recommend prescription of ACEIs to all patients with HF due to systolic dysfunction (LVEF ≤40 %), irrespective of symptoms, unless contraindicated or not tolerated. Treatment should be initiated at low doses and gradually increased thereafter. The most common adverse effects of ACEIs are hypotension, acute kidney injury, hyperkalemia, and cough. During ACEI therapy, serum creatinine and potassium should be assessed periodically, especially in patients with diabetes and/or CKD [21, 22].
The use of ACEIs in patients with CKD and HF seems reasonable, given the well-established simultaneous cardio- and renoprotective effects of these drugs [23]. However, there is little evidence that treatment with ACEIs reduces CV morbidity and mortality in this particular population [18]. Furthermore, clinicians are often concerned about the possibly increased risk of adverse reactions from ACEI use in HF patients with impaired kidney function [23].
Experimental studies in animal models of uremia showed that ACEIs are able to prevent LVH and cardiomyocyte loss [24, 25], whereas administration of a bradykinin receptor inhibitor completely antagonize these effects [25], suggesting that the beneficial effects of ACE inhibitors on the CV system may be mediated through bradykinin.
Several observational studies have suggested a favorable impact of ACEIs on survival in patients with CKD and HF. McAlister et al. [14] analyzed data from a prospective cohort of 754 patients with HF and found significant reductions in 1-year mortality with ACEIs and beta-blockers treatments in patients with eGFR <60 mL/min, as well as in those with eGFR ≥60 mL/min. A retrospective cohort study of 20,902 hospitalized elderly patients with a LV ejection fraction (LVEF) <40 % [26] showed that, after adjustment for multiple confounders, the prescription of an ACEI on hospital discharge was associated with a significant reduction in mortality; notably, this reduction was greater in patients with serum creatinine >3 mg/dL (n = 1,582) than in the rest of the cohort (37 % versus 16 %). Using propensity scores and multivariable-adjusted Cox regression analyses, Ahmed et al. [27] estimated the effect of ACEIs on 2-year outcomes in 1,707 patients with CKD, taken from the 6,800 patients with systolic HF (LVEF ≤45 %) in the Digitalis Investigation Group trial. In this study, CKD was defined as serum creatinine ≥1.5 mg/dL for men and ≥1.3 mg/dL for women. Patients taking ACEIs had significantly lower rates of mortality (hazard ratio = 0.58) and all-cause hospitalizations (hazard ratio = 0.69), compared to those not taking ACEIs.
Moreover, benefits of ACEIs in patients with CKD and HF have been demonstrated by several post hoc analyses of RCTs conducted in the general HF population. The Survival And Ventricular Enlargement (SAVE) study was a randomized trial of captopril versus placebo in 2,231 patients with acute myocardial infarction and LVEF ≤40 %. Patients with serum creatinine <2.5 mg/dL were excluded. A secondary analysis of this trial showed that captopril was equally efficacious in subjects with CKD (defined as eGFR <60 mL/min/1.73 m2) and those without CKD. The relative risk reduction in CV events and mortality due to captopril was actually higher in subjects with CKD (31 % versus 20 %); however, the interaction between study drug and CKD was not statistically significant [28]. In the Studies of Left Ventricular Dysfunction (SOLVD) Treatment trial, 2,569 ambulatory chronic HF patients with LVEF ≤35 % and serum creatinine ≤2.5 mg/dl were randomized to receive either placebo or enalapril. Of the 2,502 patients with baseline serum creatinine data, 1,036 had CKD (eGFR <60 ml/min/1.73 m2). The median follow-up was 35 months. Compared to placebo, enalapril significantly decreased all-cause mortality in non-CKD, but not in CKD patients (hazard ratio 0.82 versus 0.88). However, enalapril did reduce CV hospitalization in both patients with and without CKD (hazard ratio 0.77 versus 0.80). Among patients in the enalapril group, serum creatinine elevation was significantly higher in those without CKD (0.09 versus 0.04 mg/dL) during first year of follow-up, but there were no differences in changes in serum potassium (mean increase, 0.2 mEq/L, in both) [29].
In dialysis patients, observational studies have shown that ACEIs can reduce LVH [30, 31] and improve survival and CV outcomes [32], and these benefits appeared to be independent of their blood pressure-lowering effect. However, a double-blind placebo-controlled RCT in 397 hemodialysis patients with LVH [33] failed to show any significant effect of ACEI fosinopril on a composite CV end-point. The study was, nevertheless, underpowered to estimate the impact of fosinopril on survival. Chang et al. evaluated the effects of ACEI use among hemodialysis patients that participated in the HEMO study [34]. Using proportional hazards regression and a propensity score analysis, the authors found no significant associations between ACEI use and mortality, CV hospitalization, and other CV outcomes. Surprisingly, in the proportional hazards model, ACEI use was even associated with a higher risk of HF hospitalization. A retrospective analysis of the data from the Minnesota Heart Survey [35] revealed that dialysis patients hospitalized with HF had no benefit from ACEI or ARB treatment, for either short-term (30 days) or long-term (1 year) survival, in striking contrast with all of the other HF patients.
Several concerns exist for the use of ACEIs and ARBs in patients with CKD, particularly about the risk of hyperkalemia and worsening of renal function. However, these effects are usually transient and mild.
A meta-analysis of five placebo-controlled RCTs with ACEIs in patients with HF showed that, although the rate of acute kidney injury was higher with ACEIs than with placebo, drug discontinuation was rarely necessary, and renal function returned to baseline in most cases, even without dose adjustment [23, 36]. Furthermore, a systematic review of 12 RCTs with ACEIs for renoprotection in patients with CKD showed that a mild increase in serum creatinine (up to 30 % from baseline) was quite common within the first 2 weeks of therapy; however, this increase was followed by stabilization during the next few weeks [23, 37]. In patients with both HF and CKD, a retrospective analysis of the SOLVD studies has shown that the use of ACEIs was associated with a reduction of mortality, even in those with severe renal insufficiency, and did not have an adverse effect on kidney function [38]. Therefore, ACEIs should not be contraindicated in patients with HF and CKD, and a mild and non-progressive worsening of renal function at the start of therapy should not be considered, per se, as an indication to discontinue treatment [23]. However, when the GFR falls by >30 % of the pretreatment baseline, ACEI administration should be halted. Patients should then be evaluated for conditions causing renal hypoperfusion, such as volume depletion (e.g. from diuretics), renal vasoconstriction (e.g. induced by NSAIDs), and severe bilateral renal artery stenosis or stenosis in a single kidney. Unless renovascular disease is found, ACEI therapy can be resumed after correction of the underlying cause of renal ischemia and resolution of the acute kidney injury episode [23]. Reducing the daily diuretic and/or ACEI dose may prevent future worsening of the renal function [39]. It is generally recommended to begin at 15–25 % of the goal dose and, based upon changes in blood pressure and GFR, to increase every 4–8 weeks by 25–50 % until the target dose or the highest tolerated dose is reached [40].
The risk of hyperkalemia associated with the use of ACEIs is also a source of concern. In a retrospective analysis of the SOLVD trials, in patients with HF treated with enalapril the incidence of hyperkalemia ≥5.5 mEq/L was 6 %, overall; it was higher than in the placebo group and it increased progressively with the severity of the renal dysfunction [23, 41]. Careful monitoring of serum potassium is warranted in all patients with GFR <60 mL/min undergoing ACEI therapy. Concurrent use of other potentially hyperkalemia-inducing drugs, such as NSAIDs, ARBs, and potassium-sparing diuretics, should be avoided or minimized, if possible. A low potassium diet, as well as sodium bicarbonate administration in patients with metabolic acidosis, is also indicated [42]. A potassium level over 5.5 mEq/L should prompt a reduction in the ACEI dose. If the potassium concentration remains high despite the above measures, the ACEI should be discontinued [23, 42]. In patients with severe renal impairment, ACEIs should always be used with caution, because of their potential risk for adverse events.
Angiotensin II Receptor Blockers
Experience with ARBs in HF trials is much smaller than that with ACEIs. However, several studies showed that ARBs produce hemodynamic, neurohormonal, and clinical effects similar to ACEIs. The ARBs valsartan and candesartan were associated with a reduction in hospitalizations and mortality in two HF RCTs [43, 44]. Given the existing evidence, ACEIs are currently recommended as the first choice for RAAS inhibition in HF, but ARBs are a reasonable alternative, especially for patients who cannot tolerate ACEIs because of cough or angioedema [22]. Side effects like hypotension, worsening renal function, and hyperkalemia are as common as for ACEIs. Therefore, caution is required, by starting treatment at very low doses, followed by slow, step-by-step increases. Additionally, blood pressure, renal function, and serum potassium should be closely monitored.
The dual blockade of the RAAS for the treatment of HF, using a combination of an ACEI with an ARB, seems a reasonable approach. It was shown to reduce the LV size more than either agent alone [45]. However, the clinical benefits of this combination are uncertain. A trial in patients with HF post-myocardial infarction showed that combined therapy did not improve outcomes and resulted in more side effects, compared to each of the two drugs [46]. The addition of ARBs to chronic ACEI therapy caused a modest decrease in hospitalization in two studies, with a trend to decreased total mortality in one and no impact on mortality in another [22, 44, 45, 47]. Furthermore, the American College of Cardiology/American Heart Association guidelines suggest that this combination increases the risks of adverse effects [22].
In a study of patients with diabetic nephropathy and CKD stages 3–4, ARBs decreased the risk of developing HF [48]. In a post hoc analysis of the Telmisartan Randomized Assessment Study in ACE Intolerant Subjects With Cardiovascular Disease (TRANSCEND) and the Ongoing Telmisartan Alone and in Combination With Ramipril Global End Point Trial (ONTARGET), Tobe et al. [49] examined renal and CV outcomes in renal subgroups, defined by GFR and albuminuria. The main CV outcome was the composite of CV death, myocardial infarction, stroke, or hospitalization for HF. The authors found no CV benefit in any subgroup with either telmisartan versus placebo or with dual therapy (telmisartan plus ramipril) versus monotherapy.
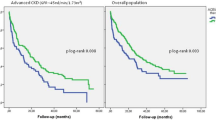
Trials of ARBs in patients with HF and CKD are very scarce. In a recent cohort study of 1,665 elderly patients with systolic HF (LVEF <45 %) and eGFR <60 mL/min/1.73 m2, followed up for 8 years, Ahmed et al. [50], using a propensity score analysis, found that treatment with ACEIs or ARBs was associated with a significant, but modest reduction in all-cause mortality (hazard ratio 0.86; 95 % confidence interval 0.74–0.996; P = 0.045) and no change in hospitalization for HF. A single RCT has been conducted so far using ARBs in ESRD patients. This multicenter Italian trial [51] included 332 hemodialysis patients with HF (NYHA II–III; LVEF ≤40 %), who were randomized to telmisartan or placebo, in addition to ACEI therapy. At 3 years, telmisartan significantly reduced all-cause mortality (35.1 % vs. 54.4 %; p < 0.001), CV death (30.3 % vs. 43.7 %; p < 0.001), and hospital admission for HF (33.9 % vs. 55.1 %; p < 0.0001). Adverse effects, mainly hypotension, occurred in 16.3 % of the telmisartan group versus 10.7 % in the placebo group.
In conclusion, considering their concurrent CV and renal benefits, we believe that ACEIs should be indicated to all CKD and ESRD patients with systolic HF, unless contraindicated or not tolerated. Alternatively, ARBs can be used, particularly in those who develop cough or angioedema from ACEIs. Dual therapy with ACEIs and ARBs can also be considered, especially in resistant cases, although the advantage over monotherapy is still uncertain and the risk of adverse effects is likely increased. Careful dose titration and clinical monitoring is required to prevent serious side effects, such as hypotension, hyperkalemia, and acute kidney injury. The role of ACEIs and ARBs in patients with CKD and HF with normal LVEF is unknown.
Aldosterone Antagonists
RAAS inhibition with ACEIs and/or ARBs may not be able to maintain adequate suppression of aldosterone production during long-term therapy, because both aldosterone and angiotensin II ultimately can escape the effects of these drugs, resulting in rebound of aldosterone levels [52, 53]. This may be a significant issue in patients with HF, since experimental studies suggest that aldosterone has deleterious effects on the structure and function of the heart, independently of and in addition to those of angiotensin II [22]. Aldosterone stimulates sodium and fluid retention and promotes myocardial remodeling and fibrosis, as well as endothelial dysfunction and atherosclerosis [54, 55]. Aldosterone antagonists (AAs), in addition to ACEIs or ARBs, can provide more complete inhibition of the RAAS, with long-term benefits. However, a higher risk of adverse effects like hyperkalemia and worsening renal function is also to be expected.
Spironolactone and eplerenone were associated with significant reductions in mortality and CV events in patients with systolic HF in the RALES (Randomized Aldactone Evaluation Study) [56] and EPHESUS (Eplerenone Post–Acute Myocardial Infarction Heart Failure Efficacy and Survival) trials [57, 58], respectively. On the other hand, many studies have reported an increased incidence of severe hyperkalemia in HF patients treated with AAs in association with ACEIs [23]. Based on these data, U.S. [22] and European [21] guidelines recommend the addition of an AA to an ACEI or an ARB in selected patients with systolic HF (NYHA class III–IV, LVEF <35 %), but without severe renal dysfunction (serum creatinine ≤2.5 mg/dL in men and ≤2.0 mg/dL in women) and with serum potassium <5.0 mEq/L. Treatment should be initiated at low doses (e.g. 12.5 or 25 mg of spironolactone or eplerenone), followed by a gradual increase (up to a target of 50 mg, if tolerated), under careful surveillance of creatinine and potassium levels. Hyperkalemia and/or worsening of the renal function require dose reduction or even withdrawal of AAs. In men, breast tenderness or enlargement may also occur with spironolactone therapy, in which case switching to eplerenone is indicated. The use of AAs should be avoided whenever adequate monitoring of potassium and creatinine levels is deemed as not feasible. Furthermore, AAs are contraindicated in association with other potassium-sparing diuretics, with potassium supplements, and with combined ACEIs and ARBs [21, 22].
The effects of AAs on clinical outcomes in patients with HF and moderate or severe CKD are not clear, since both RALES and EPHESUS trials excluded patients with serum creatinine levels >2.5 mg/dL. A prospective RCT in 112 patients with stages 2 and 3 CKD showed a significant improvement in LV mass and arterial stiffness with spironolactone versus placebo, independently of central and peripheral blood pressure changes [59]. In Iran, Taheri et al. conducted a small double-blind RCT of spironolactone 25 mg/day versus placebo, in addition to an ACEI or an ARB, in 16 hemodialysis patients with HF (NYHA class III–IV and LVEF <45 %). After 6 months of treatment, the mean LVEF increased significantly more in the spironolactone group than in the placebo group and the mean LV mass decreased in the spironolactone group, while it increased significantly in the placebo group. The incidence of hyperkalemia was unchanged in both groups [60]. The same research team performed a study with an identical design in 18 peritoneal dialysis patients with HF. They found a significant increase in LVEF in the spironolactone group, but not in the placebo group, and a non-significant increase in serum potassium in both groups [61].
The risk of AA-induced hyperkalemia in patients with advanced CKD has rarely been assessed in prospective studies, but most experts believe that this risk is unacceptably high and may become life-threatening, therefore prohibiting the use of these drugs in patients with severe and end-stage kidney disease. However, it has been suggested that hyperkalemia may be a less serious issue in hemodialysis patients, due to the effective removal of potassium through dialysis, as well as to the ability of these patients to tolerate relatively high levels of potassium without clinical manifestations. Chua et al. recently reviewed 6 RCTs that evaluated the safety of low-dose spironolactone in hemodialysis patients (of which, about 50 % were already on ACEI or ARB therapy). The authors found that the incidence of hyperkalemia with spironolactone treatment was similar to that in control groups; however, all these studies involved small populations of compliant subjects, who were at low risk for hyperkalemia [62].
Large-scale RCTs are required to evaluate the efficacy and safety of AAs in addition to ACEIs or ARBs as a treatment strategy for HF in CKD patients. In stage 3 CKD patients with HF, AAs may be considered, but should be used with great caution, limiting the dose to 25 mg/day, or every other day, and closely monitoring the potassium levels. The AAs should be avoided in patients with CKD stage 4 and 5 [23], although potassium removal by dialysis may lessen the risk of hyperkalemia in patients on renal replacement therapy. The combined use of all three RAAS inhibitors (ACEIs, ARBs, and AAs) cannot be recommended in HF patients, with or without CKD [22].
Future Therapeutic Prospects
Direct renin inhibitors (DRIs) are a newer class of RAAS inhibitors, acting at the first regulatory step of this hormonal system. Initially used as antihypertensive agents, DRIs have more recently been tested in patients with HF. In the ALOFT (Aliskiren Observation of Heart Failure Treatment) Study, which included 302 patients with stable HF, adding the DRI aliskiren to ACEIs or ARBs appeared to be safe and effective in decreasing plasma brain natriuretic peptide (BNP) and urinary aldosterone levels [63]. Two other large trials are underway using aliskiren in HF patients. The ATMOSPHERE (Aliskiren Trial to Minimize Outcomes in Patients with Heart Failure) examines the effect of aliskiren on CV mortality and hospitalization in patients with chronic HF, whereas the ASTRONAUT (Aliskiren Trial on Acute Heart Failure Outcomes) evaluates aliskiren in patients stabilized after acute HF [64]. These studies will shed important light on the role of DRIs in the treatment of HF. However, we should mention here the Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Disease Endpoints (ALTITUDE), which compared aliskiren to placebo, in addition to ACEI or ARB therapy in patients with diabetic nephropathy and CV disease. This study was prematurely stopped, because of the lack of any prospects of showing a treatment benefit, as well as due to safety concerns, including renal dysfunction, hyperkalemia, hypotension, and an unexpected excess of strokes. As a consequence, it has been suggested that dual aliskiren and ACEI/ARB therapy should not be used in patients with hypertension and CKD (eGFR <60 mL/min/1.73 m2) [63].
BAY 94–8862 is a novel, non-steroidal, mineralocorticoid receptor antagonist with greater selectivity than spironolactone and stronger binding affinity than eplerenone. The very recent MinerAlocorticoid Receptor Antagonist Tolerability Study (ARTS) was a multicentre, randomized, double-blind, placebo-controlled, parallel-group study, aiming to evaluate the safety and tolerability of this new drug in patients with systolic HF (LVEF ≤40 %) and mild-to-moderate CKD (eGFR 30–89 mL/min/1.73 m2). This study showed that BAY 94–8862 5–10 mg/day was at least as effective as spironolactone 25 or 50 mg/day in decreasing serum levels of BNP and proBNP, as well as albuminuria, but it was associated with lower incidence of hyperkalaemia (5.3 % versus 12.7 %; P = 0.048) [65].
References
Bagshaw SM, Cruz DN, Aspromonte N, Daliento L, Ronco F, Sheinfeld G, Anker SD, Anand I, Bellomo R, Berl T, Bobek I, Davenport A, Haapio M, Hillege H, House A, Katz N, Maisel A, Mankad S, McCullough P, Mebazaa A, Palazzuoli A, Ponikowski P, Shaw A, Soni S, Vescovo G, Zamperetti N, Zanco P, Ronco C, Acute Dialysis Quality Initiative Consensus Group. Epidemiology of cardio-renal syndromes: workgroup statements from the 7th ADQI Consensus Conference. Nephrol Dial Transplant. 2010;25:1406–16.
Kottgen A, Russell SD, Loehr LR, Crainiceanu CM, Rosamond WD, Chang PP, Chambless LE, Coresh J. Reduced kidney function as a risk factor for incident heart failure: the atherosclerosis risk in communities (ARIC) study. J Am Soc Nephrol. 2007;18(4):1307–15.
U.S. Renal Data System (USRDS). Chronic kidney disease in the adult NHANES population. 2009 USRDS Annual Report Data. http://www.usrds.org/2009/pdf/V1_01_09.PDF.
Cheung AK, Sarnak MJ, Yan G, Berkoben M, Heyka R, Kaufman A, Lewis J, Rocco M, Toto R, Windus D, Ornt D, Levey AS, HEMO Study Group. Cardiac diseases in maintenance hemodialysis patients: results of the HEMO Study. Kidney Int. 2004;65(6):2380–9.
Stack AG, Bloembergen WE. A cross-sectional study of the prevalence and clinical correlates of congestive heart failure among incident US dialysis patients. Am J Kidney Dis. 2001;38(5):992–1000.
Wang AY, Lam CW, Yu CM, Wang M, Chan IH, Lui SF, Sanderson JE. Troponin T, left ventricular mass, and function are excellent predictors of cardiovascular congestion in peritoneal dialysis. Kidney Int. 2006;70(3):444–52.
Harnett JD, Foley RN, Kent GM, Barre PE, Murray D, Parfrey PS. Congestive heart failure in dialysis patients: prevalence, incidence, prognosis and risk factors. Kidney Int. 1995;47(3):884–90.
Goodkin DA, Young EW, Kurokawa K, Prutz KG, Levin NW. Mortality among hemodialysis patients in Europe, Japan, and the United States: case-mix effects. Am J Kidney Dis. 2004;44 Suppl 2:16–21.
Soucie JM, McClellan WM. Early death in dialysis patients: risk factors and impact on incidence and mortality rates. J Am Soc Nephrol. 1996;7:2169–75.
Wang AY, Wang M, Lam CW, Chan IH, Lui SF, Sanderson JE. Heart failure in long-term peritoneal dialysis patients: a 4-year prospective analysis. Clin J Am Soc Nephrol. 2011;6(4):805–12.
Trespalacios FC, Taylor AJ, Agodoa LY, Bakris GL, Abbott KC. Heart failure as a cause for hospitalisation in chronic dialysis patients. Am J Kidney Dis. 2003;41:1267–77.
Shiba N, Shimokawa H. Chronic kidney disease and heart failure – bidirectional close link and common therapeutic goal. J Cardiol. 2011;57(1):8–17.
de Silva R, Nikitin NP, Witte KKA, Rigby AS, Goode K, Bhandari S, Clark AL, Cleland JG. Incidence of renal dysfunction over 6 months in patients with chronic heart failure due to left ventricular systolic dysfunction: contributing factors and relationship to prognosis. Eur Heart J. 2006;27:569–81.
McAlister FA, Ezekowitz J, Tonelli M, Armstrong PW. Renal insufficiency and heart failure: prognostic and therapeutic implications from a prospective cohort study. Circulation. 2004;109(8):1004–9.
Hillege HL, Girbes ARJ, de Kam PJ, Boomsma F, de Zeeuw D, Charlesworth A, Hampton JR, van Veldhuisen DJ. Renal function, neurohormonal activation, and survival in patients with chronic heart failure. Circulation. 2000;102:203–10.
Wang AY, Sanderson JE. Treatment of heart failure in long-term dialysis patients: a reappraisal. Am J Kidney Dis. 2011;57(5):760–72.
Raizada V, Hillerson D, Amaram JS, Skipper B. Angiotensin II-mediated left ventricular abnormalities in chronic kidney disease. J Investig Med. 2012;60(5):785–91.
Ritz E. Left ventricular hypertrophy in renal disease: beyond preload and afterload. Kidney Int. 2009;75:771–3.
Steigerwalt S, Zafar A, Mesiha N, Gardin J, Provenzano R. Role of aldosterone in left ventricular hypertrophy among African-American patients with end-stage renal disease on hemodialysis. Am J Nephrol. 2007;27:159–63.
Ascenção R, Fortuna P, Reis I, Carneiro AV. Drug therapy for chronic heart failure due to left ventricular systolic dysfunction: a review. III. Angiotensin-converting enzyme inhibitors. Rev Port Cardiol. 2008;27(9):1169–87.
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Strömberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29(19):2388–442.
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119(14):e391–479.
Acquarone N, Castello C, Antonucci G, Lione S, Bellotti P. Pharmacologic therapy in patients with chronic heart failure and chronic kidney disease: a complex issue. J Cardiovasc Med (Hagerstown). 2009;10(1):13–21.
Amann K, Tyralla K, Gross ML, Schwarz U, Törnig J, Haas CS, Ritz E, Mall G. Cardiomyocyte loss in experimental renal failure: prevention by ramipril. Kidney Int. 2003;63(5):1708–13.
Amann K, Gassmann P, Buzello M, Orth SR, Törnig J, Gross ML, Magener A, Mall G, Ritz E. Effects of ACE inhibition and bradykinin antagonism on cardiovascular changes in uremic rats. Kidney Int. 2000;58(1):153–61.
Frances CD, Noguchi H, Massie BM, Browner WS, McClellan M. Are we inhibited? Renal insufficiency should not preclude the use of ACE inhibitors for patients with myocardial infarction and depressed left ventricular function. Arch Intern Med. 2000;160:2645–50.
Ahmed A, Love TE, Sui X, Rich MV. Effects of angiotensin-converting enzyme inhibitors in systolic heart failure patients with chronic kidney disease: a propensity score analysis. J Card Fail. 2006;12:499–506.
Tokmakova MP, Skali H, Kenchaiah S, Braunwald E, Rouleau JL, Packer M, Chertow GM, Moyé LA, Pfeffer MA, Solomon SD. Chronic kidney disease, cardiovascular risk, and response to angiotensin-converting enzyme inhibition after myocardial infarction: the Survival And Ventricular Enlargement (SAVE) study. Circulation. 2004;110:3667–73.
Bowling CB, Sanders PW, Allman RM, Rogers WJ, Patel K, Aban IB, Rich MW, Pitt B, White M, Bakris GC, Fonarow GC, Ahmed A. Effects of enalapril in systolic heart failure patients with and without chronic kidney disease: insights from the SOLVD Treatment trial. Int J Cardiol. 2013;167(1):151–6.
London GM, Pannier B, Guerin AP, Marchais SJ, Safar ME, Cuche JL. Cardiac hypertrophy, aortic compliance, peripheral resistance, and wave reflection in end-stage renal disease. Comparative effects of ACE inhibition and calcium channel blockade. Circulation. 1994;90(6):2786–96.
Cannella G, Paoletti E, Delfino R, Peloso G, Rolla D, Molinari S. Prolonged therapy with ACE inhibitors induces a regression of left ventricular hypertrophy of dialyzed uremic patients independently from hypotensive effects. Am J Kidney Dis. 1997;30(5):659–64.
Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation. 2001;103(7):987–92.
Zannad F, Kessler M, Lehert P, Grünfeld JP, Thuilliez C, Leizorovicz A, Lechat P. Prevention of cardiovascular events in end-stage renal disease: results of a randomized trial of fosinopril and implications for future studies. Kidney Int. 2006;70(7):1318–24.
Chang TI, Shilane D, Brunelli SM, Cheung AK, Chertow GM, Winkelmayer WC. Angiotensin-converting enzyme inhibitors and cardiovascular outcomes in patients on maintenance hemodialysis. Am Heart J. 2011;162(2):324–30.
Berger AK, Duval S, Manske C, Vazquez G, Barber C, Miller L, Luepker RV. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in patients with congestive heart failure and chronic kidney disease. Am Heart J. 2007;153:1064–73.
Flather MD, Yusuf S, Køber L, Pfeffer M, Hall A, Murray G, Torp-Pedersen C, Ball S, Pogue J, Moyé L, Braunwald E. Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients. Lancet. 2000;355:1575–81.
Bakris GL, Weir MR. Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: is this a cause for concern? Arch Intern Med. 2000;160:685–93.
Khan NA, Ma I, Thompson CR, Humphries K, Salem DN, Sarnak MJ, Levin A. Kidney function and mortality among patients with left ventricular systolic dysfunction. J Am Soc Nephrol. 2006;17:244–53.
Abdo AS, Basu A, Geraci SA. Managing chronic heart failure patient in chronic kidney disease. Am J Med. 2011;124(1):26–8.
Gradman AH, Papademetriou V. Combined renin-angiotensin-aldosterone system inhibition in patients with chronic heart failure secondary to left ventricular systolic dysfunction. Am Heart J. 2009;157(6 Suppl):S17–23.
de Denus S, Tardif JC, White M, Bourassa MG, Racine N, Levesque S, Ducharme A. Quantification of the risk and predictors of hyperkalemia in patients with left ventricular dysfunction: a retrospective analysis of the Studies of Left Ventricular Dysfunction (SOLVD) trials. Am Heart J. 2006;152:705–12.
Palmer BF. Managing hyperkalemia caused by inhibitors of the rennin-angiotensin-aldosterone system. N Engl J Med. 2004;351:585–92.
Granger CB, McMurray JJ, Yusuf S, Held P, Michelson EL, Olofsson B, Ostergren J, Pfeffer MA, Swedberg K, CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet. 2003;362:772–6.
Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–75.
Wong M, Staszewsky L, Latini R, Barlera S, Volpi A, Chiang YT, Benza RL, Gottlieb SO, Kleemann TD, Rosconi F, Vandervoort PM, Cohn JN, Val-HeFT Heart Failure Trial Investigators. Valsartan benefits left ventricular structure and function in heart failure: Val-HeFT echocardiographic study. J Am Coll Cardiol. 2002;40:970–5.
Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Køber L, Maggioni AP, Solomon SD, Swedberg K, Van de Werf F, White H, Leimberger JD, Henis M, Edwards S, Zelenkofske S, Sellers MA, Califf RM, Valsartan in Acute Myocardial Infarction Trial Investigators. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003;349:1893–906.
Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J, CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362:777–81.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S, RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Tobe SW, Clase CM, Gao P, McQueen M, Grosshennig A, Wang X, Teo KK, Yusuf S, Mann JF, ONTARGET and TRANSCEND Investigators. Cardiovascular and renal outcomes with telmisartan, ramipril, or both in people at high renal risk: results from the ONTARGET and TRANSCEND studies. Circulation. 2011;123(10):1098–107.
Ahmed A, Fonarow GC, Zhang Y, Sanders PW, Allman RM, Arnett DK, Feller MA, Love TE, Aban IB, Levesque R, Ekundayo OJ, Dell’Italia LJ, Bakris GL, Rich MW. Renin-angiotensin inhibition in systolic heart failure and chronic kidney disease. Am J Med. 2012;125(4):399–410.
Cice G, Di Benedetto A, D’Isa S, D’Andrea A, Marcelli D, Gatti E, Calabrò R. Effects of telmisartan added to angiotensin-converting enzyme inhibitors on mortality and morbidity in hemodialysis patients with chronic heart failure: a double-blind, placebo-controlled trial. J Am Coll Cardiol. 2010;56(21):1701–8.
Staessen J, Lijnen P, Fagard R, Verschueren LJ, Amery A. Rise in plasma concentration of aldosterone during long-term angiotensin II suppression. J Endocrinol. 1981;91(3):457–65.
Borghi C, Boschi S, Ambrosioni E, Melandri G, Branzi A, Magnani B. Evidence of a partial escape of renin-angiotensin-aldosterone blockade in patients with acute myocardial infarction treated with ACE inhibitors. J Clin Pharmacol. 1993;33(1):40–5.
Weber KT. Aldosterone in congestive heart failure. N Engl J Med. 2001;345(23):1689–97.
Briet M, Schiffrin EL. Aldosterone: effects on the kidney and cardiovascular system. Nat Rev Nephrol. 2010;6(5):261–73.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341(10):709–17.
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M, Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348(14):1309–21.
Pitt B, White H, Nicolau J, Martinez F, Gheorghiade M, Aschermann M, van Veldhuisen DJ, Zannad F, Krum H, Mukherjee R, Vincent J, EPHESUS Investigators. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46(3):425–31.
Edwards NC, Steeds RP, Stewart PM, Ferro CJ, Townend JN. Effect of spironolactone on left ventricular mass and aortic stiffness in early-stage chronic kidney disease: a randomized controlled trial. J Am Coll Cardiol. 2009;54(6):505–12.
Taheri S, Mortazavi M, Shahidi S, Pourmoghadas A, Garakyaraghi M, Seirafian S, Eshaghian A, Ghassami M. Spironolactone in chronic hemodialysis patients improves cardiac function. Saudi J Kidney Dis Transpl. 2009;20(3):392–7.
Taheri S, Mortazavi M, Pourmoghadas A, Seyrafian S, Alipour Z, Karimi S. A prospective double-blind randomized placebo-controlled clinical trial to evaluate the safety and efficacy of spironolactone in patients with advanced congestive heart failure on continuous ambulatory peritoneal dialysis. Saudi J Kidney Dis Transpl. 2012;23(3):507–12.
Chua D, Lo A, Lo C. Spironolactone use in heart failure patients with end-stage renal disease on hemodialysis: is it safe? Clin Cardiol. 2010;33(10):604–8.
McMurray JJ, Pitt B, Latini R, Maggioni AP, Solomon SD, Keefe DL, Ford J, Verma A, Lewsey J, Aliskiren Observation of Heart Failure Treatment (ALOFT) Investigators. Effects of the oral direct renin inhibitor aliskiren in patients with symptomatic heart failure. Circ Heart Fail. 2008;1(1):17–24.
Sever PS, Gradman AH, Azizi M. Managing cardiovascular and renal risk: the potential of direct renin inhibition. J Renin Angiotensin Aldosterone Syst. 2009;10(2):65–76.
Pitt B, Kober L, Ponikowski P, Gheorghiade M, Filippatos G, Krum H, Nowack C, Kolkhof P, Kim SY, Zannad F. Safety and tolerability of the novel non-steroidal mineralocorticoid receptor antagonist BAY 94–8862 in patients with chronic heart failure and mild or moderate chronic kidney disease: a randomized, double-blind trial. Eur Heart J. 2013;34(31):2453–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Gaiţă, D., Moşteoru, S., Segall, L. (2015). How to Use Inhibitors of the Renin-Angiotensin-Aldosterone System in Patients with CKD and Heart Failure. In: Goldsmith, D., Covic, A., Spaak, J. (eds) Cardio-Renal Clinical Challenges. Springer, Cham. https://doi.org/10.1007/978-3-319-09162-4_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-09162-4_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09161-7
Online ISBN: 978-3-319-09162-4
eBook Packages: MedicineMedicine (R0)