Abstract
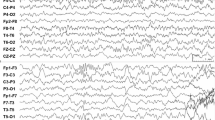
An 8-year-old boy presents with recurrent spells that occur during sleep. They are most commonly noted shortly after he falls asleep. His parents observe unilateral facial twitching and drooling, and hear him make “gurgling” sounds. He appears to be awake during the spell, but is unable to speak. The spell occurs for approximately 1 or 2 min. Afterwards, he takes a couple of minutes to recover but is able to recall the event. He reports a sensation of numbness that will affect his lips and tongue that are present on the same side as the facial twitching. Because of disruptive nature of the spells, the family is seeking medical attention for diagnosis and treatment. The patient is otherwise healthy and engaged in activities at home and at school. His development has been normal. The neurologic and general examinations are also normal. Laboratory studies are unremarkable, and a sleep-deprived electroencephalogram (EEG) is ordered (Fig. 6.1).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Case Presentation
An 8-year-old boy presents with recurrent spells that occur during sleep. They are most commonly noted shortly after he falls asleep. His parents observe unilateral facial twitching and drooling, and hear him make “gurgling” sounds. He appears to be awake during the spell, but is unable to speak. The spell occurs for approximately 1 or 2 min. Afterwards, he takes a couple of minutes to recover but is able to recall the event. He reports a sensation of numbness that will affect his lips and tongue that are present on the same side as the facial twitching. Because of the disruptive nature of the spells, the family is seeking medical attention for diagnosis and treatment. The patient is otherwise healthy and engaged in activities at home and at school. His development has been normal. The neurologic and general examinations are also normal. Laboratory studies are unremarkable, and a sleep-deprived electroencephalogram (EEG) is ordered (Fig. 6.1).
Clinical Questions
-
1.
How does this EEG support a particular clinical diagnosis?
-
2.
What is the prognostic significance of centrotemporal spikes?
-
3.
What are pediatric focal epilepsy syndromes, and what characteristics do they share?
-
4.
Do patients with benign epilepsy with centrotemporal spikes (BECTS) require medication?
-
5.
What is the anticipated clinical course and prognosis in BECTS?
Diagnostic Discussion
-
1.
Spikes and sharp waves followed by aftergoing slow waves emanating from the centrotemporal region, typically with a negative maximum at the C3 + T7 and/or C4 + T8 electrodes, and with frontal positivity, are classically seen in BECTS. BECTS is the most common of the pediatric focal epilepsy syndromes. The interictal epileptiform activity can occur either unilaterally (approximately 60 % of cases) or bilaterally (approximately 40 % of cases). Spikes can occur during wakefulness, but are more prominent during non-REM sleep when they can occur very frequently, seemingly out of proportion to the clinical seizure history.
-
2.
The frequency of the centrotemporal spikes does not correlate well with the frequency or the duration of seizures in a patient with BECTS. Indeed, interictal spikes on EEG may persist long after resolution of the clinical seizures and, hence, do not aid in deciding when to discontinue an antiepileptic drug (AED). Furthermore, many children with centrotemporal spikes never develop clinical seizures.
-
3.
BECTS, as noted above, is the most common of the three focal epilepsy syndromes recognized by the International League Against Epilepsy (ILAE). It accounts for 10–20 % of the new-onset pediatric epilepsies. The other two common focal epilepsies are early-onset childhood occipital epilepsy (Panayiotopoulos type) and late-onset childhood occipital epilepsy (Gastaut type). These three syndromes share several features. A genetic predisposition has been noted; however, various genetic and environmental factors influence the clinical phenotype. There is also a developmental age-specific onset of symptoms, with BECTS seizure onset peaking at 7–10 years of age. Lastly, the clinical course is marked by relatively mild seizures, amenable to AED treatment, which spontaneously remit (see below).
-
4.
Not all patients with BECTS require treatment with an AED. When brief focal seizures (see below) occur infrequently, the parents and physician may opt not to treat with an AED and to incur the risk of chronic AED therapy. Levetiracetam, oxcarbazepine, and other non-sedating ASDs have been used for those patients requiring treatment.
-
5.
Despite the focal EEG abnormalities, brain MRI scans do not demonstrate any significant abnormality. Children typically demonstrate normal development. However, some manifest mild neuropsychological abnormalities and academic difficulties. Focal seizures may evolve to include convulsive seizures. Clinical remission may occur 2 to 4 years after onset, though typically before 16 years of age. It is very unusual (<1 %) for BECTS to evolve to a more severe epilepsy with drug-resistant seizures.
Clinical Pearls
-
1.
BECTS is the most common pediatric localization-related epilepsy syndrome, typically presenting in an age-dependent fashion with sleep-activated focal seizures.
-
2.
While there is a genetic predisposition, other genetic and environmental factors likely play a role in determining whether or not seizures will occur.
-
3.
The typical findings of frequent interictal centrotemporal epileptiform abnormalities present during sleep on EEG support the diagnosis of “rolandic” epilepsy.
-
4.
The prognosis is excellent. There are in general terms seizures that occur that are relatively mild composed of focal seizures without convulsions. Additionally, the seizures are amenable to AED treatment (if needed), and spontaneously resolve in adolescence.
Bibliography
Fernandez IS, Loddenkemper T. Pediatric focal epilepsy syndromes. J Clin Neurophysiol. 2012;29:425–40.
Holmes GL. Rolandic epilepsy: clinical and electroencephalographic features. Epilepsy Res Suppl. 1992;6:29–43.
Nordli D. Focal and multifocal seizures. In: Swaiman K, Ashwal K, Ferriero D, editors. Pediatric neurology: principles and practice. Philadelphia, PA: Mosby Elsevier; 2006. p. 1037–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Hammond, D.N. (2014). Benign Childhood Epilepsy with Centrotemporal Spikes. In: Tatum, W., Sirven, J., Cascino, G. (eds) Epilepsy Case Studies. Springer, Cham. https://doi.org/10.1007/978-3-319-01366-4_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-01366-4_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01365-7
Online ISBN: 978-3-319-01366-4
eBook Packages: MedicineMedicine (R0)