Abstract
Epileptic encephalopathy with continuous spike and waves during slow-wave sleep (CSWS) is a spectrum of epileptic conditions best defined by the association of cognitive or behavioral impairment acquired during childhood and not related to another factor than the presence of abundant interictal epileptiform discharges (IEDs) during sleep, which tend to diffuse over the whole scalp. It is part of the childhood focal epileptic syndromes. Some cases are genetic, related to GRIN2A mutation that impairs the glutamate NMDA receptor functions, and overlap with benign epilepsy with central temporal spikes. Others are related to a structural brain lesion that may affect either the cortex or the thalami. Most cases are of unknown etiology. Landau-Kleffner syndrome (LKS) is a particular presentation where acquired aphasia is the core symptom. Clinical, neurophysiological, and cerebral glucose metabolism data support the hypothesis that IEDs play a prominent role in the cognitive deficits by interfering with the neuronal networks at the site of the epileptic foci but also at distant connected areas. Therefore, the treatment should aim to suppress CSWS. This may be achieved using conventional antiepileptic drugs, but corticosteroids seem to have more pronounced and sustained efficacy. Outcome for epilepsy is usually good, CSWS being an age-dependent EEG pattern, whereas outcome for cognition, language, and behavior is variable. Rehabilitation represents an important part of the treatment, and visual forms of language should be encouraged in children with LKS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
31.1 Introduction
Cognitive deficits are highly prevalent in epileptic children. In a community-based sample of children (<16 years) prospectively identified at the time of initial diagnosis of epilepsy, abnormal global cognitive function ranging from borderline dysfunction to severe mental retardation was found in 26.4% of the patients, independent factors contributing to cognitive deficits being age at onset <5 years, symptomatic etiology, current antiepileptic drug (AED) treatment, and epileptic encephalopathies [1]. Epileptic encephalopathies are conditions in which the epileptic activity itself may contribute to progressive cognitive dysfunction [2, 3]. Thus, in epileptic encephalopathies, uncontrolled epileptic activity is expected to result in worsening of cognitive function over time, as illustrated in a longitudinal study of a cohort of children with epilepsy onset before the age of 3 years [4]. On the other hand, early effective intervention is expected to improve developmental outcome. Various electro-clinical epilepsy syndromes ranging from neonatal to childhood onset are recognized as epileptic encephalopathies, i.e., early epileptic encephalopathy with suppression bursts, West syndrome, Dravet syndrome, Lennox-Gastaut syndrome, and epileptic encephalopathy with continuous spike and waves during slow-wave sleep (CSWS). These syndromes have multiple causes, and the cognitive difficulties of these patients are often multifactorial. So it may be very difficult to individualize the relative contribution of the underlying etiology, the epileptic activity, and the possible negative effects of AED in the cognitive deficits. In some epileptic encephalopathies like Dravet syndrome, it is the occurrence of repeated and prolonged convulsive seizures that is suspected to negatively impact cognitive outcome [5]. In epileptic encephalopathy with CSWS, the situation is completely different, as some patients do not present any clinical seizure at all. Here it is more the interictal epileptiform discharges (IED) that are believed to play a negative role on cognition, and this issue will be discussed in details in this chapter.
Epileptic encephalopathy with CSWS is now viewed as a hat for different conditions that were historically described according to various clinical and EEG criteria. The first one is Landau and Kleffner syndrome (LKS), reported in 1957 in children with normal early language development who became aphasic after the onset of epileptic seizures and had bilateral temporal IED on EEG [6]. The language disturbance was further characterized as auditory verbal agnosia, i.e., the inability to decode phonemes despite intact peripheral hearing mechanisms, leading to a severe expressive and receptive verbal deficit [7]. Observations of less severe forms of language regression without clinical seizures were further reported [8,9,10,11]. Longitudinal follow-up of these children showed that the seizures as well as the EEG abnormalities remit at adolescence [8]. The second one is electrical status epilepticus during slow sleep (ESES), reported by Tassinari et al. in 1971 in children with refractory seizures and global cognitive regression who presented a particular EEG pattern characterized by diffuse spike-waves occurring during at least 85% of slow sleep and persisting on three or more records over a period of at least 1 month [12]. The evolution of the epilepsy showed remission at adolescence even if most patients had persistent and sometimes severe neuropsychological sequels. The third one is atypical benign epilepsy with central temporal spikes (BECTS) described by Aicardi and Chevrie who reported children suffering from an epileptic syndrome resembling BECTS but with atypical features like frequent brief seizures (atypical absences, focal myoclonia), cognitive impairment, and CSWS [13]. Subsequently, observations of children with CSWS presenting other types of cognitive deterioration than aphasia or dementia were reported. These included autism and more selective cognitive impairments like frontal lobe dysfunction, apraxia and hemineglect, pseudo-bulbar palsy, visual agnosia, and learning arrest [14, 15].
The ILAE considered that there is insufficient evidence for mechanistic differences between LKS, ESES, and other conditions with CSWS to warrant considering them separate syndromes and proposed the term of “epileptic encephalopathy with CSWS including LKS” for this particular childhood epileptic syndrome [2].
31.2 Definition and Limits of Epileptic Encephalopathy with CSWS
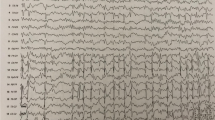
There is now a large consensus to consider epileptic encephalopathy with CSWS as a spectrum of epileptic conditions defined by [1] an onset in childhood (3–10 years), [2] the occurrence of cognitive or behavioral impairments that appear or worsen after the epilepsy onset, and [3] the presence of abundant IEDs during sleep, which tend to be more frequent, with increased amplitude and diffusion over the whole scalp during non-rapid eye movement (NREM) sleep than during the awake state. LKS is a particular presentation where acquired aphasia is the core symptom. Seizures are not a mandatory feature. When they occur, seizures have variable semiology (focal seizures without consciousness impairment, secondary generalized tonic-clonic seizures, focal negative myoclonia, atypical absences), but, unlike in Lennox-Gastaut syndrome, tonic seizures and rapid rhythms during sleep are not encountered [16, 17].
But what is less consensual are the frontiers with classical (BECTS) and particularly the minimal EEG and clinical criteria needed to pose the diagnosis of epileptic encephalopathy with CSWS, because these two conditions overlap. Observations of classical BECTS cases evolving to an epileptic encephalopathy with CSWS, sometimes precipitated by the use of some antiepileptic drugs (AED) [17, 18], and of CSWS and BECTS cases coexisting within the same family [19] further outline this overlap. It should be too simplistic to state that it is the presence of CSWS and of cognitive deficits that will distinguish BECTS from epileptic encephalopathy with CSWS. Indeed, if a pattern of CSWS was found in the course of the disease in all LKS patients reported in some series [8, 20,21,22,23], it was found only in a minority of patients in another series [24]. More recently, three LKS patients with initial normal sleep EEG were reported, the diagnosis being made after several weeks or months based on the demonstration of IEDs during sleep, including CSWS in two of them [25]. Also, some data suggest that it is not only the IED percentage but also their increased amplitude and diffusion during sleep that is detrimental to normal brain function (see below) [26, 27]. This evidences that the EEG criteria of CSWS criteria as proposed by the Tassinari’s group [12] are too restrictive to define the syndrome.
Also, the minimal cognitive impairment needed to make a diagnosis of epileptic encephalopathy with CSWS is a subject of controversy. Indeed, numerous studies have reported an unexpected high rate of cognitive difficulties in the language, the attentional, and the memory domains in children with classical BECTS, which were associated with IED severity at the acute phase of the disease and resolved with the normalization of the EEG [28,29,30].
In conclusion, it is widely accepted that BECTS and epileptic encephalopathy with CSWS are edges of a spectrum where the most frequent and diffused IEDs during sleep seem to result in the more severe behavioral and cognitive deficits [31,32,33]. The nosological limits between these two conditions are thus somewhat arbitrary.
31.3 Etiology
Epileptic encephalopathy with CSWS is part of the childhood focal epileptic syndromes. According to the terminology revised in 2010 [3], the underlying etiology allows classifying patients within one of the following three subgroups: structural/metabolic, genetic, and unknown. The subgroup of unknown etiology is the most important, representing more than half of the patients. Patients with structural brain lesions identified on magnetic resonance imaging (MRI) are in the structural/metabolic subgroup and represent about 20% of the cases. Lesions are usually antenatal cortical malformations (polymicrogyria) or ante/perinatal cortical destructive lesions, but may also be purely subcortical, the association between thalamic perinatal injury and CSWS being well recognized [34, 35]. These cases have usually preexisting signs of cerebral palsy. In the genetic subgroup are patients with preexisting psychomotor delay related to chromosomal anomalies (15q deletion for instance) or genetic syndromes like Rett syndrome [36]. More recently, inherited and de novo mutations in GRIN2A gene, encoding a subunit of the glutamate NMDA receptor, were found in 9–20% of probands within the BECTS-LKS spectrum and normal MRI [37,38,39]. GRIN2A encodes for the N-methyl-d-aspartate (NMDA) glutamate receptor a2 subunit, GluN2A. As some mutations result in a gain of function, this could theoretically lead to an etiological treatment using NMDA receptor blockers.
31.4 Pathophysiology of Cognitive Regression
Epileptic encephalopathy with CSWS is one of the best illustrations of the concept of epileptic encephalopathy. Indeed, clinical improvement is evident and sometimes impressive when treatment results in EEG normalization, even in lesion-related cases [26, 34, 35, 40, 41].
It should be noted that complete normalization of the sleep EEG is not always mandatory to obtain clinical improvement. Indeed, besides the percentage of spike-wave complexes during NREM sleep, the diffusion of the epileptic activity over the whole scalp is also important to consider, as children with diffuse CSWS may show spectacular clinical improvement under treatment even if a focus of spikes persists during a high percentage of sleep time [26, 41].
The initial hypothesis of a “functional ablation” of eloquent cortical areas by the “persistent convulsive discharge” to explain the neuropsychological impairment, as proposed more than half a century ago by Landau and Kleffner [6], remains the most largely accepted hypothesis. However, some observations are not fully explained by this theory. Firstly, the temporal association between CSWS on EEG and neurological regression is not always strict [7, 22, 25]. This suggests that other factors, e.g., autoimmune factors as suggested by the response to corticosteroids (see below in the treatment section), could impact language and cognition in some patients. Secondly, if some authors found strict association between the pattern of neuropsychological impairment and the location of interictal focus, others did not. Indeed, patients showing clinical frontal dysfunction but a parietal epileptic focus have been reported [15]. This discrepancy can be explained regarding the pathophysiological model that emerged from positron emission tomography with [18F]-fluorodeoxyglucose (FDG-PET) data obtained at the awake state in children at the active phase of the disease as well as at remission. Those studies demonstrated that the acute phase of CSWS is characterized by a metabolic pattern associating regional increase(s) and decrease(s) in glucose metabolism in distinct brain areas, with heterogeneous location of the abnormalities across patients [15, 27]. Combination of magnetoencephalography (MEG) and FDG-PET demonstrated that focal hypermetabolism was related to the onset or the propagation sites of spike-wave discharges, whereas hypometabolic areas were not involved in the epileptic network as such [42]. At the group level, hypometabolism occurred in regions that belong to the default network (prefrontal and posterior cingulate cortices, parahippocampal gyrus, and precuneus) [43]. The pathophysiological model proposed to explain these findings is based on the “surrounding and remote inhibition theory,” which suggests the existence of epilepsy-induced inhibition of neurons that surround or are remote from the hypermetabolic epileptic focus and connected with it via cortico-cortical or polysynaptic pathways [44, 45]. The validity of this model in epileptic encephalopathy with CSWS is supported by [1] the evidence of altered effective connectivity between hyper- and hypometabolic areas, suggesting that the level of metabolic activity in hypometabolic areas is related to the epilepsy-induced metabolic changes in the hypermetabolic ones [15, 27, 43], and [2] the complete or almost complete parallel regression of hypermetabolic and hypometabolic abnormalities at recovery from CSWS [27].
Interestingly, patients investigated by FDG-PET during sleep showed regional metabolism alterations that were similar to the wake state [46]. Furthermore, EEG combined with functional magnetic resonance imaging (EEG-fMRI) investigations demonstrated similar types of findings but directly linked to CSWS activity, i.e., IED-related increases in perfusion at the site of the epileptic focus that were associated with decreases in perfusion in distinct connected brain areas, including nodes of the default mode network [47, 48]. Thus, patients with CSWS show during sleep profound metabolic and EEG disturbances that could alter the physiological roles of sleep. One of the physiological functions of sleep is to promote memory consolidation (see [49] for review). One study showed impaired consolidation of a declarative memory task during sleep in two children with epileptic encephalopathy with CSWS and normalization of overnight memory performance after successful treatment of CSWS with hydrocortisone in one of them, suggesting that CSWS could impair the mechanisms of sleep-related brain plasticity [50]. An epilepsy-related disruption of synaptic homeostasis processes that take place during sleep is suggested in CSWS children by a study showing the absence of the expected decrease in the slope of slow waves during sleep [51].
To sum up, behavioral and functional neuroimaging data suggest sustained epilepsy-related perturbations of neurophysiological processes through the sleep-wake cycle at the acute phase of CSWS. They also incite to attribute the neurological regression not only to neuronal impairment at the epileptic focus site but also to epilepsy-induced inhibition of distant connected brain areas.
31.5 Treatment
In the absence of any published controlled study on the use of AED in epileptic encephalopathy with CSWS, treatment relies upon expert-based consensus guidelines and uncontrolled published series. The evaluation of a drug effect is probably more difficult in this epileptic syndrome than in others because [1] clinical and EEG fluctuations with time without any change of treatment are frequently observed and [2] the goals of the treatment are not only to abolish the seizures with minimal side effects but also to obtain neuropsychological improvement by decreasing IEDs during sleep.
Valproate (VPA) is classically proposed as first choice drug, either in monotherapy or in association with a benzodiazepine (usually clobazam), but this relies on relatively old series including few patients [36, 52]. Data concerning the effect of benzodiazepines on the EEG are more convincing. De Negri et al. reported a remission of CSWS in 9 out of 15 patients with a 1-month intrarectal diazepam treatment [53]; among these nine patients, seven showed an improvement in their neuropsychological evaluation after 6 months. A more recent study reported a reduction of about 35% of the interictal epileptiform activity 24 h after the administration of high-dose diazepam [54]. Among the other old drugs, there is a consensus stating that carbamazepine, phenobarbital, and diphantoin are usually inefficacious and may even worsen the EEG and clinical condition of children with CSWS. On the contrary, ethosuximide and sulthiame are old drugs that may be helpful in reducing CSWS [52, 55].
Concerning the new AED, studies suggest that levetiracetam in add-on treatment is effective in about half of the patients [26, 31, 56, 57].
Corticosteroids are probably more efficacious and result in more long-lasting effects than classical AED. In a series of 30 patients, high-dose diazepam was efficacious in 37%, all the children showing temporary response only, whereas response to steroids was obtained in 65% [31]. The larger series on the effects of corticosteroids in epileptic encephalopathy with CSWS published so far included 44 patients [41]. Most of them were treated with hydrocortisone starting at 5 mg/kg/d with a maintenance dose of 2 mg/kg/d until the end of a full-year treatment. More than 75% of the patients responded to this regimen within the first 3 months, with normalization of the EEG in about half of them. As relapse occurred in 14 patients, 20 patients (45.4%) were long-term responders. Positive response to steroids was associated with higher IQ and shorter CSWS duration. Patients with LKS were all long-term responders in this series. The prolonged use of hydrocortisone resulted in the usual complications including cushingoid appearance in all patients, but life-threatening side effects were not observed. Seven patients discontinued prematurely the treatment because of side effects. Thus, efficacy of corticosteroids must be balanced by its side effects, and this study supports the fact that they should be introduced relatively early in children showing severe regression [41]. The mechanisms of action of corticosteroids are poorly understood. An immunosuppressive effect is possible, but a direct action on epilepsy through the modulation of various neurotransmitter systems, as hypothesized in West syndrome, seems more likely [58].
Among the other therapeutic modalities, the benefits of intravenous immunoglobulins were not confirmed in a recent series [59]. Data on the use of vagus nerve stimulation and ketogenic diet are too scarce to draw conclusions [52].
Resective surgery in patients with cortical lesions was found to be effective on both seizures and cognition; in particular when CSWS is associated with hemiplegia, hemispherotomy may show spectacular cognitive improvement because CSWS is likely to be a secondary generalization of the epileptic activity from the damaged hemisphere [40, 60, 61].
Concerning palliative surgical procedures, callosotomy and multiple subpial transections may be considered. Callosotomy was found useful in one series [40]. Multiple subpial transections have to be considered in refractory cases of LKS. This technique has indeed shown benefits only in patients with a pure verbal auditive agnosia and not in other phenotypes of CSWS epilepsy [62, 63]. Good candidates are patients with severe persisting aphasia in whom a unilateral perisylvian epileptic origin is suggested on the basis of the noninvasive presurgical evaluation [64]. MEG is particularly useful in this perspective [65]. Improvement of language after surgery was reported in the majority of patients, but was most likely to be seen years, rather than months, after surgery, which raises the question of the natural evolution to recovery [62].
31.6 Long-Term Outcome
Long-term outcome for seizures is good in epileptic encephalopathy with CSWS, persisting seizures at adulthood occurring in a minority of patients, even in those with lesion-related epilepsy [34, 35, 66].
Therefore, the main concern in epileptic encephalopathy with CSWS is the cognitive outcome. Long-term studies show persistent cognitive deficits in most patients [67,68,69]. Excluding the underlying etiology, available literature supports that the main variables impacting long-term cognitive outcome are the duration of CSWS or of regression and the type and severity of cognitive regression at the acute phase of the disease.
Authors have related either duration of CSWS or duration of regression with long-term outcome, but these two time periods could not be identical. Indeed, sleep EEG abnormalities may fluctuate from day to day in the early stage of regression, even leading to normal EEG records [25]. Therefore, the duration of regression seems more appropriate to be considered in studies designed to identify dependent factors of cognitive outcome. This has also the advantage to include patients for whom sleep EEG data at early regression are not available.
Long duration of CSWS—or regression—was found as predictive of bad cognitive outcome in a lot of studies [8, 21, 31, 67,68,69,70,71]. In some studies, this factor reached statistical significance. In a series of 18 LKS patients followed at a mean length of 67 months, long duration of CSWS was associated with outcome, no child with CSWS lasting longer than 36 months having normal outcome [21]. In a series of 30 patients with epileptic encephalopathies with CSWS of various etiologies, including lesion-related cases, followed at a mean of 6.6 years, the duration of CSWS correlated significantly with residual intellectual deficit [31]. Long duration of CSWS was statistically associated with bad cognitive outcome in a recent series of ten patients with different types of cognitive regression and normal MRI followed at long term [67].
The type and severity of cognitive regression at the acute phase of the disease need also to be considered. Several studies showed persistence of neuropsychological dysfunctions particular to each syndrome at long term, so that patients with prolonged global intellectual regression had the worst outcome, whereas those with more specific deficits recovered best [66, 67, 72]. Concerning more specifically LKS, patients usually keep language difficulties at adulthood, but the disability is highly variable, depending on response to treatment [8, 25, 66, 73]. Persistent impairment in verbal short-term memory was demonstrated in patients after recovery from LKS using functional imaging: when compared to controls, patients showed decrease activation for an immediate serial recall word task in those posterior superior temporal gyri that were involved in the epileptic focus during the active phase of the disease [74].
In atypical BECTS, where cognitive regression may be discrete, long-term outcome may be favorable: a study followed 12 patients until ages 6 to 14 years and showed that long duration of negative motor seizure period was associated with low IQ, 4 patients having IQ less than 70 [75]. Another study found full cognitive recovery in two of the five patients with atypical BECTS [76].
31.7 Rehabilitation
Rehabilitation is a very important part of the treatment. In LKS cases with preserved nonverbal skills, learning of visual forms of language including sign language is useful as they can successfully be learned at different ages and don’t interfere with oral language recovery. Still, sign language could facilitate recovery by stimulating functionally connected core language networks [73].
References
Berg AT, Langfitt JT, Testa FM, Levy SR, DiMario F, Westerveld M, et al. Global cognitive function in children with epilepsy: a community-based study. Epilepsia. 2008;49(4):608–14.
Engel J Jr. Report of the ILAE classification core group. Epilepsia. 2006;47(9):1558–68.
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde Boas W, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia. 2010;51(4):676–85.
Berg AT, Smith SN, Frobish D, Beckerman B, Levy SR, Testa FM, et al. Longitudinal assessment of adaptive behavior in infants and young children with newly diagnosed epilepsy: influences of etiology, syndrome, and seizure control. Pediatrics. 2004;114(3):645–50.
Brunklaus A, Ellis R, Reavey E, Forbes GH, Zuberi SM. Prognostic, clinical and demographic features in SCN1A mutation-positive Dravet syndrome. Brain. 2012;135(Pt 8):2329–36.
Landau WM, Kleffner FR. Syndrome of acquired aphasia with convulsive disorder in children. Neurology. 1957;7(8):523–30.
Rapin I, Mattis S, Rowan AJ, Golden GG. Verbal auditory agnosia in children. Dev Med Child Neurol. 1977;19(2):197–207.
Paquier PF, Van Dongen HR, Loonen CB. The Landau-Kleffner syndrome or ‘acquired aphasia with convulsive disorder’. Long-term follow-up of six children and a review of the recent literature. Arch Neurol. 1992;49(4):354–9.
Soprano AM, Garcia EF, Caraballo R, Fejerman N. Acquired epileptic aphasia: neuropsychologic follow-up of 12 patients. Pediatr Neurol. 1994;11(3):230–5.
Tassinari CA, Rubboli G, Volpi L, Billard C, Bureau M. Etat de mal électrique épileptique pendant le sommeil lent (ESES ou POCS) incluant l’aphasie épileptique acquise (syndrome de Landau-Kleffner). In: Roger J, Bureau M, Dravet C, Genton P, Tassinari CA, Wolf P, editors. Les syndromes épileptiques de l’enfant et de l’adolescent. 3rd ed. Eastleigh: John Libbey; 2002. p. 265–83.
Deonna TW. Acquired epileptiform aphasia in children (Landau-Kleffner syndrome). J Clin Neurophysiol. 1991;8(3):288–98.
Patry G, Lyagoubi S, Tassinari CA. Subclinical “electrical status epilepticus” induced by sleep in children. A clinical and electroencephalographic study of six cases. Arch Neurol. 1971;24(3):242–52.
Aicardi J, Chevrie JJ. Atypical benign partial epilepsy of childhood. Dev Med Child Neurol. 1982;24(3):281–92.
Roulet Perez E, Davidoff V, Despland PA, Deonna T. Mental and behavioural deterioration of children with epilepsy and CSWS: acquired epileptic frontal syndrome. Dev Med Child Neurol. 1993;35(8):661–74.
De Tiege X, Goldman S, Laureys S, Verheulpen D, Chiron C, Wetzburger C, et al. Regional cerebral glucose metabolism in epilepsies with continuous spikes and waves during sleep. Neurology. 2004;63(5):853–7.
Galanopoulou AS, Bojko A, Lado F, Moshe SL. The spectrum of neuropsychiatric abnormalities associated with electrical status epilepticus in sleep. Brain and Development. 2000;22(5):279–95.
Tassinari CA, Rubboli G, Volpi L, Meletti S, d’Orsi G, Franca M, et al. Encephalopathy with electrical status epilepticus during slow sleep or ESES syndrome including the acquired aphasia. Clin Neurophysiol. 2000;111(Suppl 2):S94–S102.
Saltik S, Uluduz D, Cokar O, Demirbilek V, Dervent A. A clinical and EEG study on idiopathic partial epilepsies with evolution into ESES spectrum disorders. Epilepsia. 2005;46(4):524–33.
De Tiege X, Goldman S, Verheulpen D, Aeby A, Poznanski N, Van Bogaert P. Coexistence of idiopathic rolandic epilepsy and CSWS in two families. Epilepsia. 2006;47(10):1723–7.
Dulac O, Billard C, Arthuis M. Electroclinical and developmental aspects of epilepsy in the aphasia-epilepsy syndrome. Arch Fr Pediatr. 1983;40(4):299–308.
Robinson RO, Baird G, Robinson G, Simonoff E. Landau-Kleffner syndrome: course and correlates with outcome. Dev Med Child Neurol. 2001;43(4):243–7.
Hirsch E, Marescaux C, Maquet P, Metz-Lutz MN, Kiesmann M, Salmon E, et al. Landau-Kleffner syndrome: a clinical and EEG study of five cases. Epilepsia. 1990;31(6):756–67.
Massa R, de Saint-Martin A, Hirsch E, Marescaux C, Motte J, Seegmuller C, et al. Landau-Kleffner syndrome: sleep EEG characteristics at onset. Neurophysiol Clin. 2000;111(Suppl 2):S87–93.
McVicar KA, Ballaban-Gil K, Rapin I, Moshe SL, Shinnar S. Epileptiform EEG abnormalities in children with language regression. Neurology. 2005;65(1):129–31.
Van Bogaert P, King MD, Paquier P, Wetzburger C, Labasse C, Dubru JM, et al. Acquired auditory agnosia in childhood and normal sleep electroencephalography subsequently diagnosed as Landau-Kleffner syndrome: a report of three cases. Dev Med Child Neurol. 2013;55(6):575–9.
Aeby A, Poznanski N, Verheulpen D, Wetzburger C, Van Bogaert P. Levetiracetam efficacy in epileptic syndromes with continuous spikes and waves during slow sleep: experience in 12 cases. Epilepsia. 2005;46(12):1937–42.
De Tiege X, Ligot N, Goldman S, Poznanski N, de Saint Martin A, Van Bogaert P. Metabolic evidence for remote inhibition in epilepsies with continuous spike-waves during sleep. NeuroImage. 2008;40(2):802–10.
Verrotti A, Filippini M, Matricardi S, Agostinelli MF, Gobbi G. Memory impairment and benign epilepsy with centrotemporal spike (BECTS): a growing suspicion. Brain Cogn. 2014;84(1):123–31.
Baglietto MG, Battaglia FM, Nobili L, Tortorelli S, De Negri E, Calevo MG, et al. Neuropsychological disorders related to interictal epileptic discharges during sleep in benign epilepsy of childhood with centrotemporal or Rolandic spikes. Dev Med Child Neurol. 2001;43(6):407–12.
Deonna T, Zesiger P, Davidoff V, Maeder M, Mayor C, Roulet E. Benign partial epilepsy of childhood: a longitudinal neuropsychological and EEG study of cognitive function. Dev Med Child Neurol. 2000;42(9):595–603.
Kramer U, Sagi L, Goldberg-Stern H, Zelnik N, Nissenkorn A, Ben-Zeev B. Clinical spectrum and medical treatment of children with electrical status epilepticus in sleep (ESES). Epilepsia. 2009;50(6):1517–24.
Moeller F, Moehring J, Ick I, Steinmann E, Wolff S, Jansen O, et al. EEG-fMRI in atypical benign partial epilepsy. Epilepsia. 2013;54(8):e103–8.
Stephani U, Carlsson G. The spectrum from BCECTS to LKS: the Rolandic EEG trait-impact on cognition. Epilepsia. 2006;47(Suppl 2):67–70.
Guerrini R, Genton P, Bureau M, Parmeggiani A, Salas-Puig X, Santucci M, et al. Multilobar polymicrogyria, intractable drop attack seizures, and sleep- related electrical status epilepticus. Neurology. 1998;51(2):504–12.
Guzzetta F, Battaglia D, Veredice C, Donvito V, Pane M, Lettori D, et al. Early thalamic injury associated with epilepsy and continuous spike-wave during slow sleep. Epilepsia. 2005;46(6):889–900.
Van Bogaert P, Aeby A, De Borchgrave V, De Cocq C, Deprez M, De Tiege X, et al. The epileptic syndromes with continuous spikes and waves during slow sleep: definition and management guidelines. Acta Neurol Belg. 2006;106(2):52–60.
Carvill GL, Regan BM, Yendle SC, O’Roak BJ, Lozovaya N, Bruneau N, et al. GRIN2A mutations cause epilepsy-aphasia spectrum disorders. Nat Genet. 2013;45(9):1073–6.
Lesca G, Rudolf G, Bruneau N, Lozovaya N, Labalme A, Boutry-Kryza N, et al. GRIN2A mutations in acquired epileptic aphasia and related childhood focal epilepsies and encephalopathies with speech and language dysfunction. Nat Genet. 2013;45(9):1061–6.
Lemke JR, Lal D, Reinthaler EM, Steiner I, Nothnagel M, Alber M, et al. Mutations in GRIN2A cause idiopathic focal epilepsy with rolandic spikes. Nat Genet. 2013;45(9):1067–72.
Peltola ME, Liukkonen E, Granstrom ML, Paetau R, Kantola-Sorsa E, Valanne L, et al. The effect of surgery in encephalopathy with electrical status epilepticus during sleep. Epilepsia. 2011;52(3):602–9.
Buzatu M, Bulteau C, Altuzarra C, Dulac O, Van Bogaert P. Corticosteroids as treatment of epileptic syndromes with continuous spike-waves during slow-wave sleep. Epilepsia. 2009;50(Suppl 7):68–72.
De Tiege X, Trotta N, Op de Beeck M, Bourguignon M, Marty B, Wens V, et al. Neurophysiological activity underlying altered brain metabolism in epileptic encephalopathies with CSWS. Epilepsy Res 2013.
Ligot N, Archambaud F, Trotta N, Goldman S, Van Bogaert P, Chiron C, et al. Default mode network hypometabolism in epileptic encephalopathies with CSWS. Epilepsy Res. 2014;108(5):861–71.
Bruehl C, Witte OW. Cellular activity underlying altered brain metabolism during focal epileptic activity. Ann Neurol. 1995;38:414–20.
Schwartz TH, Bonhoeffer T. In vivo optical mapping of epileptic foci and surround inhibition in ferret cerebral cortex. Nat Med. 2001;7(9):1063–7.
Maquet P, Hirsch E, Dive D, Salmon E, Marescaux C, Franck G. Cerebral glucose utilization during sleep in Landau-Kleffner syndrome: a PET study. Epilepsia. 1990;31(6):778–83.
Siniatchkin M, Groening K, Moehring J, Moeller F, Boor R, Brodbeck V, et al. Neuronal networks in children with continuous spikes and waves during slow sleep. Brain. 2010;133(9):2798–813.
De Tiege X, Harrison S, Laufs H, Boyd SG, Clark CA, Allen P, et al. Impact of interictal epileptic activity on normal brain function in epileptic encephalopathy: an electroencephalography-functional magnetic resonance imaging study. Epilepsy Behav. 2007;11(3):460–5.
Urbain C, Galer S, Van Bogaert P, Peigneux P. Pathophysiology of sleep-dependent memory consolidation processes in children. Int J Psychophysiol 2013;89(2):273–83.
Urbain C, Di Vincenzo T, Peigneux P, Van Bogaert P. Is sleep-related consolidation impaired in focal idiopathic epilepsies of childhood? A pilot study. Epilepsy Behav. 2011;22(2):380–4.
Bolsterli BK, Schmitt B, Bast T, Critelli H, Heinzle J, Jenni OG, et al. Impaired slow wave sleep downscaling in encephalopathy with status epilepticus during sleep (ESES). Clin Neurophysiol. 2011;122(9):1779–87.
Lagae L. Rational treatment options with AEDs and ketogenic diet in Landau-Kleffner syndrome: still waiting after all these years. Epilepsia. 2009;50(Suppl 7):59–62.
De Negri M, Baglietto MG, Battaglia FM, Gaggero R, Pessagno A, Recanati L. Treatment of electrical status epilepticus by short diazepam (DZP) cycles after DZP rectal bolus test. Brain Dev. 1995;17(5):330–3.
Sanchez Fernandez I, Hadjiloizou S, Eksioglu Y, Peters JM, Takeoka M, Tas E, et al. Short-term response of sleep-potentiated spiking to high-dose diazepam in electric status epilepticus during sleep. Pediatr Neurol. 2012;46(5):312–8.
Fejerman N, Caraballo R, Cersosimo R, Ferraro SM, Galicchio S, Amartino H. Sulthiame add-on therapy in children with focal epilepsies associated with encephalopathy related to electrical status epilepticus during slow sleep (ESES). Epilepsia. 2012;53(7):1156–61.
Wang SB, Weng WC, Fan PC, Lee WT. Levetiracetam in continuous spike waves during slow-wave sleep syndrome. Pediatr Neurol. 2008;39(2):85–90.
Atkins M, Nikanorova M. A prospective study of levetiracetam efficacy in epileptic syndromes with continuous spikes-waves during slow sleep. Seizure. 2011;20(8):635–9.
Hrachovy R. ACTH and steroids. In: Engel JJ, Pedley T, editors. Epilepsy, a comprehensive textbook, vol. 2. Philadelphia: Lippincott-Raven; 1997. p. 1463–73.
Arts WF, Aarsen FK, Scheltens-de Boer M, Catsman-Berrevoets CE. Landau-Kleffner syndrome and CSWS syndrome: treatment with intravenous immunoglobulins. Epilepsia. 2009;50(Suppl 7):55–8.
Kallay C, Mayor-Dubois C, Maeder-Ingvar M, Seeck M, Debatisse D, Deonna T, et al. Reversible acquired epileptic frontal syndrome and CSWS suppression in a child with congenital hemiparesis treated by hemispherotomy. Eur J Paediatr Neurol. 2009;13(5):430–8.
Loddenkemper T, Cosmo G, Kotagal P, Haut J, Klaas P, Gupta A, et al. Epilepsy surgery in children with electrical status epilepticus in sleep. Neurosurgery. 2009;64(2):328–37; discussion 37.
Grote CL, Van Slyke P, Hoeppner JA. Language outcome following multiple subpial transection for Landau-Kleffner syndrome. Brain. 1999;122(Pt 3):561–6.
Irwin K, Birch V, Lees J, Polkey C, Alarcon G, Binnie C, et al. Multiple subpial transection in Landau-Kleffner syndrome. Dev Med Child Neurol. 2001;43(4):248–52.
Cross JH, Neville BG. The surgical treatment of Landau-Kleffner syndrome. Epilepsia. 2009;50(Suppl 7):63–7.
Paetau R. Magnetoencephalography in Landau-Kleffner syndrome. Epilepsia. 2009;50(Suppl 7):51–4.
Praline J, Hommet C, Barthez MA, Brault F, Perrier D, Passage GD, et al. Outcome at adulthood of the continuous spike-waves during slow sleep and Landau-Kleffner syndromes. Epilepsia. 2003;44(11):1434–40.
Seegmuller C, Deonna T, Dubois CM, Valenti-Hirsch MP, Hirsch E, Metz-Lutz MN, et al. Long-term outcome after cognitive and behavioral regression in nonlesional epilepsy with continuous spike-waves during slow-wave sleep. Epilepsia. 2012;53(6):1067–76.
Pera MC, Brazzo D, Altieri N, Balottin U, Veggiotti P. Long-term evolution of neuropsychological competences in encephalopathy with status epilepticus during sleep: a variable prognosis. Epilepsia. 2013;54(Suppl 7):77–85.
Liukkonen E, Kantola-Sorsa E, Paetau R, Gaily E, Peltola M, Granstrom ML. Long-term outcome of 32 children with encephalopathy with status epilepticus during sleep, or ESES syndrome. Epilepsia. 2010;51(10):2023–32.
Scholtes FB, Hendriks MP, Renier WO. Cognitive deterioration and electrical status epilepticus during slow sleep. Epilepsy Behav. 2005;6(2):167–73.
Veggiotti P, Termine C, Granocchio E, Bova S, Papalia G, Lanzi G. Long-term neuropsychological follow-up and nosological considerations in five patients with continuous spikes and waves during slow sleep. Epileptic Disord. 2002;4(4):243–9.
Debiais S, Tuller L, Barthez MA, Monjauze C, Khomsi A, Praline J, et al. Epilepsy and language development: the continuous spike-waves during slow sleep syndrome. Epilepsia. 2007;48(6):1104–10.
Deonna T, Prelaz-Girod AC, Mayor-Dubois C, Roulet-Perez E. Sign language in Landau-Kleffner syndrome. Epilepsia. 2009;50(Suppl 7):77–82.
Majerus S, Laureys S, Collette F, Del Fiore G, Degueldre C, Luxen A, et al. Phonological short-term memory networks following recovery from Landau and Kleffner syndrome. Hum Brain Mapp. 2003;19(3):133–44.
Fujii A, Oguni H, Hirano Y, Osawa M. Atypical benign partial epilepsy: recognition can prevent pseudocatastrophe. Pediatr Neurol. 2010;43(6):411–9.
Tovia E, Goldberg-Stern H, Ben Zeev B, Heyman E, Watemberg N, Fattal-Valevski A, et al. The prevalence of atypical presentations and comorbidities of benign childhood epilepsy with centrotemporal spikes. Epilepsia. 2011;52(8):1483–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Van Bogaert, P. (2020). The Epileptic Encephalopathy with Continuous Spike and Waves During Slow-Wave Sleep. In: Salih, M.A. (eds) Clinical Child Neurology. Springer, Cham. https://doi.org/10.1007/978-3-319-43153-6_31
Download citation
DOI: https://doi.org/10.1007/978-3-319-43153-6_31
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43152-9
Online ISBN: 978-3-319-43153-6
eBook Packages: MedicineMedicine (R0)