Abstract
Autonomic symptoms are clinical manifestations of a wide range of epileptic seizures resulting from the recruitment or dysfunction of specific areas of the brain, best known as the central autonomic network. Although their prevalence, autonomic signs occurring during a seizure are often misdiagnosed.
In this chapter we described the autonomic manifestations reported during seizures according to their presentation during epileptic discharges, focusing on the role of the central autonomic network (CAN) in determining clinical manifestations. The primary cause of autonomic seizures such as temporal lobe epilepsy (TLE) and self-limited epilepsy with autonomic seizures (SeLEAS), will be illustrated and some developmental and epileptic encephalopathies (DEE) with complex autonomic dysfunction will be considered. In the end, the primary or secondary involvement of the autonomic nervous system, in the form of central or obstructive apnea or both, cardiac arrhythmia, autonomic dysregulation, and hypoxia, in determining sudden unexpected death in epilepsy (SUDEP) will be discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Epilepsy
- Childhood
- Ictal autonomic manifestations
- Temporal lobe epilepsy
- Self-limited epilepsy with autonomic seizures
- Central autonomic network
- Sudden unexpected death in epilepsy
- Developmental and epileptic encephalopathies
11.1 Introduction
Epileptic seizures are characterized by recurrent, paroxysmal, and unprovoked episodes of cerebral cortical dysfunction, due to abnormal excessive or synchronous neuronal activity in the brain [1]. During seizures involuntary movements, sensory phenomena, altered levels of consciousness, behavior abnormalities, impairments in cognitive function, and abnormal autonomic phenomena may occur. Many different autonomic symptoms appear during epileptic seizures, some of which are rarely considered life-threatening. In 2007, an international working group of expert researchers defined autonomic seizure as “an epileptic seizure characterized by altered autonomic function of any type at seizure onset or in which manifestations consistent with altered autonomic function are prominent (qualitatively dominant or clinically important) even if not present at seizure onset”. The same researchers suggested the following terminology to define autonomic status epilepticus: “an autonomic seizure which lasts more than 30 min, or a series of such seizures over a 30-min period without full recovery between seizures” [2]. The latter condition is typically observed in epilepsy previously named Panayiotopoulos syndrome (PS). Other focal seizures, especially in childhood, may manifest only as autonomic symptoms or signs [3]. The International League Against Epilepsy (ILAE) recently contributed to the classification of autonomic symptoms present in both focal and generalized seizures. The most recent edition of the ILAE’s classification (2017) presents a three-level model, beginning with seizure type and progressing to epilepsy diagnosis (focal epilepsy, generalized epilepsy, combined generalized and focal epilepsy, and unknown epilepsy group). The last level is that of epileptic syndrome: a specific syndrome diagnosis can be made based on clinical seizure types, neurologic manifestations, and electroencephalographic (EEG) patterns, often supported by specific etiological findings (structural, genetic, metabolic, immunological, and infectious) [4]. The syndromes often have age-dependent presentations and a range of specific comorbidities (Fig. 11.1). In clinical practice, epileptic syndrome identification is important for appropriate antiepileptic drug selection, prognosis, and parent counseling.
Framework for classification of the epilepsies according to the ILAE 2017. (From Scheffer et al. 2017 [5] with permission)
The expanded ILAE 2017 operational classification encourages the identification of seizure type. Focal seizures with retained or impaired awareness may optionally be characterized by one of the motor-onset or non-motor-onset symptoms listed in Fig. 11.2. In this operational classification, non-motor focal seizures may manifest as autonomic dysfunction, behavior arrest, cognitive, emotional, or sensory dysfunction. According to this classification, “focal autonomic seizures can present with gastrointestinal sensations, a sense of heat or cold, flushing, piloerection (goosebumps), palpitations, sexual arousal, respiratory changes, or other autonomic effects” [5].
Scheme of the new operational classification of seizure types promoted by ILAE 2017 (from Fisher et al. 2017 [4] with permission).2 The degree of impaired awareness is often not specified.3 Unclassifiable due to lack of information or inability to classify the episode into a category
Based on the 2017 seizure classification, an ILAE Task Force composed of members with pediatric expertise, recently published an update on the taxonomy of syndromes. They suggested to use terms directly describing the seizure semiology and classified epileptic pediatric syndromes into three categories: (1) self-limited focal epilepsies; (2) generalized epilepsies; (3) developmental and/or epileptic encephalopathies [6]. In the context of self-limited focal epilepsies of childhood (SeLFE), the authors described syndromes with specific clinical, seizure semiology, and electroencephalographic (EEG) features. Based on their long-term prognosis two subgroups were identified. In the first subgroup, Panayiotopoulos syndrome, or early-onset benign occipital epilepsy now renamed self-limited epilepsy with autonomic seizures (SeLEAS), was included in addition to benign epilepsy of childhood with centrotemporal spikes or benign Rolandic epilepsy, now renamed self-limited epilepsy with centrotemporal spikes. The second subgroup included two syndromes: idiopathic childhood occipital epilepsy—Gastaut type, now renamed childhood occipital visual epilepsy, and idiopathic photosensitive occipital lobe epilepsy, now renamed photosensitive occipital lobe epilepsy. Clinically significant autonomic symptoms and signs can also accompany seizures of focal, generalized, and/or unknown onset. SeLEAS, known as Panayiotopoulos syndrome, is a model of autonomic epilepsy specific to childhood (see below). Furthermore, ictal autonomic manifestations are frequently underreported either because they are unrecognized, given their predominantly nocturnal onset, or forgiven. In a recent prospective survey, only 11% of documented autonomic features were recalled by the patient [7]. The clinical range and significance of autonomic dysfunction during seizures are not fully understood and, in many cases, seizures are classified by the earliest prominent motor or nonmotor onset feature [8]. As reported elsewhere in this book, the central autonomic network (CAN) is often involved during the propagation of both focal and generalized seizures. A wide variety of clinical events are thought to be mediated by cortical discharges recruiting CAN pathways [9]. In addition, as already mentioned and reported in several studies, autonomic symptoms and signs are frequently childhood-related because of a susceptibility to autonomic seizures due to a lower seizure threshold of subcortical components, related to a supposed immaturity of CAN [2, 10]. Assessment of autonomic functions involved in seizures results in two outcomes: first, a better localization and management of epilepsies; second, the correct framing of some autonomic disorders co-occurring in sudden unexpected death in epilepsy (SUDEP) could facilitate the use of measures that would help to reduce mortality of people with epilepsy. This chapter will focus on autonomic signs and symptoms in epileptic seizures and the most common forms of epilepsy associated with autonomic phenomena will be considered (SeLEAS or Panayiotopoulos syndrome and Temporal lobe epilepsy). In addition, the clinical aspects underlying SUDEP will be described.
11.2 Autonomic Seizures: The Role of Central Autonomic Network
Clinical features of seizures in epilepsy result from the recruitment or dysfunction of specific areas of the brain. These areas may have a functional relationship to anatomically close areas, but seizures can also propagate to distant areas of the brain. In other words, a network dysfunction, due to poor integration of neurons, facilitates the aberrant generation and propagation of neuronal discharges. Autonomic changes are frequent manifestations of epileptic seizures [11, 12]. During seizures, autonomic symptoms may be the only ones or predominant clinical features, as in simple autonomic seizures, or accompany both focal and generalized seizures. In all these cases, autonomic seizures are characterized by recurrent stereotypical symptoms affecting the cardiovascular, neuroendocrine, respiratory, genitourinary, sexual, gastrointestinal systems, and/or cutaneous and pupillary symptoms. Direct activation of the CAN by epileptic discharges, rather than the motor or behavioral effects of the seizures themselves may cause autonomic symptoms and signs [11]. The role of the CAN and possible dysfunction of this area is assessed by functional neuroimaging, particularly functional magnetic resonance imaging [13]. The CAN is an integral component of an internal regulation system that includes the insular cortex, orbitofrontal cortex, anterior cingulate cortex, amygdala, hypothalamus, periaqueductal grey matter, parabrachial complex nucleus, the nucleus of the solitary tract, ventrolateral reticular formation of the medulla, and medullary raphe. The CAN is characterized by reciprocal interconnections and receives converging visceral and somatosensory information, through which the brain controls visceromotor, neuroendocrine, pain, and behavioral responses essential for survival [14]. From a functional and methodological point of view, this network is a structure divided into three main components in relation to distinctive regions of the central nervous system:
-
(a)
The spinal cord contains neuronal bodies and Projections causing the elementary segmental reflex control of the autonomic nervous system functions (Fig. 11.3).
-
(b)
At the brainstem level, the nucleus of the solitary tract, the ventrolateral medulla, and the parabrachial nucleus of the dorsolateral pons are involved in cardiovascular, respiratory, gastrointestinal, and genitourinary autonomic systems regulation. The periaqueductal grey in the midbrain region integrates autonomic control with pain Modulation and behavioral responses to stress and sleep (Fig. 11.3).
-
(c)
Finally, at the forebrain level, the hypothalamus integrates autonomic, endocrine, and sleep functions, while the anterior limbic circuit (anterior cingulate cortex, amygdala, and insular cortices) integrates bodily sensation and pain with the emotional autonomic response [14] (Fig. 11.3).
Principal components of the Central Autonomic Network (CAN) from the cerebral neocortex to the spinal cord. The lower segments of the CAN are regulated by the higher centers. There exist reciprocal connections between the structures. The CAN which exerts a modulating influence on the peripheral autonomic system is directly influenced by the limbic system and the epileptic foci. The real organization of CAN is much more complex than presented here
These regions control the peripheral autonomic function through both direct and indirect connections with centers in the lower brainstem [13, 15].
Structures responsible for the sympathetic response include the noradrenergic neurons of the locus coeruleus and the ventrolateral medulla oblongata. The parabrachial region, nucleus ambiguous, the nucleus of the vagus nerve, corpus amygdaloideum, and periaqueductal grey matter influence parasympathetic mechanisms. Other areas play a role in both modalities [16].
The area postrema, also known as the chemoreceptor trigger zone, is one of the regions linked to vomiting. The motor elements of vomiting are controlled by the dorsal vagal nucleus, the nucleus of the solitary tract, the parvocellular reticular formation, and the ventral respiratory groups [14]. Extensive functional neuroimaging studies show that the autonomic symptoms, especially in self-limiting forms of epilepsy are related to the lower seizure threshold caused by the hyperexcitability of specific autonomic circuits connected with motor or sensory responses. Otherwise, primary epileptogenic activity may spread to higher-order brain areas when reaching the symptomatogenic threshold resulting in focal seizures that could evolve into generalized seizures [17]. In general, the autonomic disturbances present in different epileptic seizures can be classified according to their presentation during a seizure so that ictal and post-ictal forms can be distinguished. The autonomic signs have an early ictal onset when the cortex early involved in the central autonomic network. Conversely, the autonomic symptoms occur in the post-event or later in the ictal period [18].
11.3 Autonomic Changes in the Ictal Phase
11.3.1 Cardiovascular Symptoms
Since the first description of the relationship between the brain and heart in people with epilepsy more than a century ago, several studies have shown that seizures, both generalized and focal, induce autonomic dysfunction of the cardiovascular system [19, 20]. Cardiovascular alterations, specifically seizure-related cardiac arrhythmias, play an important role in determining the excess of mortality in patients with epilepsy and they have been implicated as potential pathomechanisms of SUDEP. Ictal sinus tachycardia can be observed in 82% of patients with epilepsy, as reported in a previous review. The authors reported that the average percentage of seizures associated with significant heart rate changes is similar for generalized (64%), including generalized tonic–clonic seizures, and focal onset seizures (71%) [21]. Focal seizures evolving to bilateral tonic–clonic seizures show a higher ictal heart rate as compared to focal seizures with impaired awareness [22]. Since the earliest observations in the rat, some authors demonstrated that cardiac regulation involved the right insula for sympathetic control and the left insula for parasympathetic control [23, 24]. These findings are still debated [25]. In a study using intracranial electrodes, the EEG signal precedes other seizure manifestations, but ictal tachycardia was reported to be an early sign, especially in right mesial temporal onset seizures [26]. In childhood epilepsy, available studies on ictal tachycardia are limited but no significant differences seem to be in the frequencies of ictal tachycardia in adults versus children [10]. Some authors reported ictal tachycardia in TLE seizures in 98% and confirmed right hemispheric lateralization of sympathetic cardiac control [27]. A recent study suggested that epilepsy duration is an independent risk factor for ECG changes and that cardiac alterations may be a time-dependent phenomenon [28]. Ictal Bradycardia occurs less commonly during seizures than tachycardia and is observed in <5% of seizures [29]. In a cohort of 49 children, similar results were reported (3.7% of seizures had ictal bradycardia) [30]. Occasionally the bradycardia may be severe enough to cause sinus arrest and asystole. Cardiac asystole is infrequent. In a previous study, in a large cohort, cardiac asystole occurred in 7 out of 2003 patients (0.34%), undergoing long-term video EEG/ECG monitoring [31]. This is in line with the reported 0.27–0.4% of patients suffering ictal asystole during prolonged video EEG telemetry [32]. In two different systematic reviews, it was reported that all patients examined, 103 cases in the first and 157 in the second, who presented with ictal asystole suffered from focal epilepsy [33, 34]. Prolonged cerebral hypoperfusion induced by asystole may result in the onset of syncope. Ictal asystole with subsequent syncope predominantly happens in people with temporal lobe epilepsy [33, 35]. In a cortical stimulation study, Oppenheimer et al. confirmed that bradycardia appears during stimulation of the left insular cortex. This result suggested that seizures occurring in the left hemisphere are more frequently associated with ictal bradycardia [23]. In the 20 s after the end of the electroencephalographic discharge, such as the postictal period, ictal asystole can occur. In the aforementioned review, 13 patients presented with postictal asystole, among them 85% presented focal seizures evolving into bilateral tonic-clonic seizures (TCSs) [33]. During the ictal and peri-ictal periods, other cardiac arrhythmias, including atrial flutter/atrial fibrillation and postictal ventricular fibrillation, were identified [2, 33, 36, 37]. Postictal ventricular fibrillation is preceded mainly by focal to bilateral seizures. In these conditions, increasing sympathetic activity, peri-ictal QTc prolongation and other predisposing cardiac conditions may be contributing factors anti-seizure medications (ASMs), such as sodium channel blockers, including carbamazepine, lacosamide, lamotrigine, and phenytoin, may play an important role in determining variation in heart rate frequency, firstly bradycardia, particularly at high dosages [22, 38]. However, Lamberts et al., suggested that concomitant heart disease more than epileptic features may lead to cardiovascular symptoms [39].
11.3.2 Respiratory Manifestations
Automatic mechanisms of respiration are controlled by the central respiratory oscillators located in the lower brain stem, under the control of forebrain cortical areas (hippocampal formation; anterior cingulate gyrus; insula; basal forebrain; and the motor area). Focal seizures localized in these cortical areas could affect respiration and early experimental stimulation studies, show that the activation of these areas results in irregular breathing patterns, end-expiratory apnoea, and hyperpnoea [40]. Due to anatomical location, temporal lobe epilepsy is commonly associated with apnoea and oxygen desaturations [41, 42]. Hyperventilation is a common underdiagnosed sign of seizures because monitoring of respiratory activity is not always performed during electroencephalographic recording. In a polygraphic video-EEG recordings study, on 57 pre-surgery patients, authors reported that central apnoea with oxygen desaturation and increased CO2 levels occur in around one-third of seizures [43]. The authors also observed that ictal oxygen desaturations of <90%, <80%, and <70% were shown in 33.2%, 10.2%, and 3.6% of all seizures. In this study, the degree of desaturation was significantly correlated with temporal lobe seizure onset, right hemispheric seizure lateralization, duration, and contralateral spread [43]. In a study based on cardiorespiratory monitoring and video EEG monitoring, ictal central apnoea preceded EEG seizure onset in 54.3% of cases and it was the only clinical manifestation in 16.5% of seizures [41]. The onset of central ictal apnoea (IA) depends on the quickness of the seizure spreading from one temporal lobe to the contralateral. Patients with TLE with contralateral diffusion are at the highest risk of seizure-related respiratory dysfunctions [44]. Other respiratory-related autonomic phenomena during seizures include stridor, postictal nose wiping, peri-ictal coughing, and other respiratory manifestations (i.e., laryngospasm, nocturnal choking, and laryngeal constriction) [3]. Unilateral postictal nose-wiping was reported as a symptom of localizing and lateralizing in focal epilepsy. Indeed, it occurs in 40–50% of patients with temporal lobe epilepsy and it is highly predictive (92%) of seizure onset ipsilateral to the used hand [45, 46]. Nose wiping happens during seizures originating in the non-dominant temporal lobe and can be interpreted as a purposeful reaction to rhinorrhoea. The use of the hand ipsilateral to the hemisphere of seizure onset is due to a contralateral postictal weakness or neglect [45]. Furthermore, a depth electrode study has demonstrated that the involvement of the amygdala is crucial for the induction of postictal nose wiping [47]. Ictal coughing is a rare autonomic symptom, reported only in 0.16% of a large cohort of patients, without clear localization or lateralization [48]; conversely, post ictal coughing has been reported in 25% of patients [49]. The simultaneous presence of hypersalivation and retching could be a response to excessive autonomic stimulation and subsequent increased respiratory secretions and, in the absence of additional autonomic symptoms, suggest direct activation of CAN. Usually, the origin of these phenomena is in the mesial portion of the temporal lobe, unclear is the lateralization [47, 50]. Most anecdotal observations deal with symptoms such as laryngospasm, referred to seizures originating from the frontal operculum [51] and choking sensation due to frontal lobe seizures, which are often misdiagnosed with OSAS [52].
11.3.3 Gastrointestinal Symptoms
In adulthood, gastrointestinal auras are the most common symptoms of focal epilepsy [11, 53]. In the most recent systematic review, the authors suggest that, in 83% of cases, the gastrointestinal aura originates from the temporal lobe, specifically the mesial temporal lobe. In previous studies, authors reported that abdominal feelings are associated with focal seizures originating from the non-dominant temporal lobe, but this data has not been confirmed [54, 55].
11.3.3.1 Ictal Vomiting in Adults
Ictal vomiting and ictal retching are rarely reported during focal seizures in adulthood (approximately 2% in temporal lobe epilepsies) [56]. While many studies suggest that ictal nausea, and vomiting, are linked to seizure onset in the non-dominant hemisphere, indicating a functional hemispheric asymmetry for gastrointestinal motility control [57, 58], this assumption is still debated and several authors described an involvement of left (dominant) temporal lobe [59,60,61]. According to the study by Tarnutzer [62], the evaluation of ictal video EEG, shows no significant differences between left and right temporal lobe localization and suggests that ictal vomiting has no lateralization value. In conclusion, ictal vomiting has been obtained by stimulating the left temporal mesial structures (amygdala, hippocampus, and insula cortex), particularly the insular cortex. However, studies conducted with intracranial electrical stimulation of the insular cortex have not been able to elicit vomiting [63, 64].
11.3.3.2 Ictal Vomiting in Childhood
Autonomic symptoms, mostly vomiting, are the hallmark of SeLEAS. Unlike adults, in whom ictal vomiting is rare and appears later, in childhood, it occurs as the only symptom mimicking other clinical disorders, such as sleep disorders, episodic syndromes that may be associated with migraine, gastroesophageal reflux disease, encephalitis, syncope, or metabolic disease. In these clinical disorders emesis is the predominant clinical feature at the onset of the seizure [65].
11.3.4 Cutaneous Manifestations
During focal seizures, flushing, pallor, sweating, and pilomotor erection, often associated with sensations of warmth and cold may arise. Among them, although skin flushing is part of the symptoms of seizures in Panayiotopoulos Syndrome, it is less frequently reported than pallor. In a retrospective review of medical charts seizures and videotaping, authors detected skin flushing in 19 children out of 100 who underwent surgical treatment and showed it has no lateralizing or localized value [66]. In the same study by Fogarasi et al., ictal pallor was reported in about 10% of children with focal seizures both temporal and extratemporal epilepsy mainly in TLE. Ictal pallor has a high predictive value in localizing seizure onset from the left temporal lobe, especially in younger patients [66]. It is due to vasoconstriction in the skin circulation and usually, it is underdiagnosed because of the difficulty in recognizing this symptom in video monitoring. Ictal piloerection is a rare manifestation that occurs in 0.4–1.2% of patients, mainly in people with temporal lobe epilepsy. Ictal piloerection may be distributed unilaterally or bilaterally. Unilateral piloerection is most frequently associated with the ipsilateral seizure onset zone, while bilateral ictal piloerection has no hemispheric predominance [67]. The location of the symptomatogenic zone remains unclear, but probably the insula and amygdala play an important role. The etiology of ictal piloerection includes malignant brain tumors, autoimmune encephalitis, especially limbic encephalitis, and hippocampal sclerosis [68, 69]. Finally, another cutaneous manifestation described is sweating. In a young man, ipsilateral facial sweating secondary to anti-Ma2 autoimmune encephalitis is associated with testicular neoplasia [70].
11.3.5 Sexual and Genital Manifestations
Sexual and genital manifestations can occur mainly during or after focal seizures. According to Leutmezer [71] can be subdivided into (a) sexual auras, (b) sexual automatisms, (c) genital auras, and (d) genital automatisms. The authors use the term “sexual” to refer to symptoms/signs with erotic content, while “genital” refers to symptoms/signs interesting the genitals without erotic components.
According to the last seizure classification, sexual auras can be classified: focal emotional seizures and sexual automatisms as focal emotional or focal hyperkinetic seizures; genital auras as focal sensory seizures; and genital automatisms as focal seizures with automatisms [4]. Sexual auras consist of erotic and pleasurable thoughts, orgasms, and penile erection that may occur before a seizure with temporal onset (more frequently non-dominant lobe temporal) without absolute lateralizing location. Sexual auras happen especially in female subjects. The area involved is the right amygdala which confirms its key role in human sexuality [72]. Genital auras are reported in a few cases in the literature and consist of disagreeable feelings or genital pain, sometimes associated with ictal orgasm. The cortical areas involved are the postcentral gyrus, interhemispheric fissure, and perisylvian region [73]. Sexual automatisms consist of hypermotor movements of the pelvis and truncal, combined with masturbatory activity. These manifestations typically occur in frontal lobe seizures [74]. Genital automatisms, such as repetitive manipulation of the genitals, occur most frequently in temporal lobe epilepsy, usually ipsilateral to the side of the hand used in manipulation [75, 76]. Unlike sexual auras, prevalent in women, genital automatisms usually occur in males [77]. This finding confirms the different organization of sexual functions between the two sexes within the limbic network [78].
The ictal urinary urge is a rare symptom, and his pathophysiological mechanism is not entirely clear. In previous studies, evaluating scalp video-EEG monitoring or functional imaging, demonstrated a localization in the non-dominant hemisphere, specifically, the temporal lobe [11, 79, 80]. It is not clear why ictal urinary urgency is commoner in right hemisphere epilepsy, but it confirms the presumed asymmetry of central autonomic influences on the bladder.
11.3.6 Miscellaneous
Other vegetative symptoms reported in temporal lobe epilepsies include spitting, ictal hypersalivation, and peri-ictal water drinking. Spitting is a rare symptom (appearing in up to 2%) present both in seizures arising in the nondominant temporal lobe and the dominant one [53, 81,82,83]. The symptomatogenic zone was recognized in areas controlling emotional behavior but this area could not be considered a lateralizing sign of a nondominant temporal lobe [83]. Ictal hypersalivation is a common feature in self-limited focal epilepsies of childhood particularly in self-limited epilepsy with centrotemporal spikes and in early-onset benign occipital epilepsy [84, 85]. As demonstrated in a previous study, increased salivation is a rare manifestation in patients with intractable epilepsy. In a small series of 10 adults, the authors show that this uncommon sign is a localizing feature for mesial temporal seizures, mainly those that originate in the non-dominant hemisphere [86]. Peri-ictal water drinking is a rare and under-recognized sign because it is a usual habitual action. In patients with temporal lobe epilepsy, it seems to be due to the involvement of the non-dominant hemisphere. This data reflects the asymmetrical control of neural networks concerned with fluid balance, thirst, and water-seeking. The peri-ictal water drinking could be due to the propagation of epileptiform discharges from mesial temporal structures to the hypothalamus that cause thirst and consequently water-seeking [87, 88].
11.4 Lobe Temporal Epilepsy
Temporal lobe epilepsy (TLE) is one of the most common forms of focal epilepsy in adolescence and adulthood [89], representing about 40% of all epilepsies in adult people (usually with a positive family history) [90] and the 60–75% of all patients with drug-resistant epilepsy [91] among which approximately two-thirds require surgical management [92]. TLE includes a heterogeneous group of disorders that share the localization of the epileptogenic zone in the temporal lobe, either in the lateral or in the mesial portion. Mesial TLE is probably the best-known electro-clinical pattern of all epilepsies [93] since TLE commonly arises from the mesial temporal lobe (hippocampus, amygdala, and parahippocampal gyrus) and is observed in about 80% of people with TLE [93, 94]. A wide variety of clinical events is associated with the involvement of medial temporal lobe networks. Focal seizure symptomatology is usually preceded by an epileptic aura that appears before the loss of awareness and may also represent the only clinical feature. Aura is usually composed of subjective symptoms without objective signs, which reflects the initial seizure discharge in the brain. Often it is misunderstood so that the diagnosis of epilepsy is made long after the onset of these symptoms.
Several old stimulation and observational studies demonstrated the correlation between specific cortical areas and autonomic function [95, 96] even if there is no clear topographic pattern of the autonomic effects. It is well known that the insular cortex, anterior cingulum, supplementary sensorimotor area, posterior orbitofrontal cortex, or amygdala are involved in alterations in heart and respiratory rate, mydriasis, piloerection, genitourinary symptoms [97, 98]. In addition, in drug-resistant TLE, the occurrence of recurrent and uncontrolled seizures that repeatedly activate CAN structures can result in epilepsy-related autonomic dysfunction. So that the autonomic dysfunction observed in TLE becomes more prominent with the progression of the disease as well as the increased seizure frequency [99]. In the focal aware seizures may be recognized alterations in heart and respiratory rate, abdominal discomfort, and/or rising epigastric sensation and ictus emeticus. The latter identifies the triad symptomatology consisting of nausea, retching, and vomiting, which, rather rare in temporal epilepsy, is instead typical of Panayiotopoulos syndrome. Other autonomic symptoms such as pallor, flushing, mydriasis, piloerection, sweating, and genitourinary symptoms may be present but they are ignored because less frequently reported by patients or by witnesses.
The symptomatogenic zone involved in the abdominal aura (the most reported type of autonomic aura) is the anterior insular cortex, frontal operculum, mesial temporal structures, and supplementary motor area [100]. Regarding focal aware seizures, in addition to the autonomic symptoms described, cognitive (e.g., deja vu, jamais vu), emotional state (e.g., fear) or sensory (e.g., olfactory, gustatory, visual, auditory) symptoms may also be present. Sensory auras, primarily olfactory, referred to as “uncinate fits” are typically described as unpleasant odors often associated with gustatory phenomena [101]. Although olfactory aura is historically reported as a typical TLE aura, it is a rare phenomenon occurring in only 5% of patients [102] and it is related to involvement in cortical areas such as the amygdala, olfactory bulb, insular cortex, and orbitofrontal cortex [98, 100]. The visual auras are usually caused by a dysregulation affecting the posterior regions of the temporal lobe. Visual auras include both simple and complex manifestations: the first one is due to the activation of the contralateral primary visual cortex and contiguous visual association areas; the second one involves the temporo-occipital junction or the basal temporal cortex [103]. Another feature of temporal lobe epilepsy is the presence of auditory phenomena. These auditory hallucinations, described as sounds or in the complex forms of hearing voices or songs, in the former case, can be attributed to activation of Heschel’s gyrus, while in the latter, they are attributed to activation of the temporal associative cortex. In mesial temporal lobe epilepsy, fear is one of the most common affective symptoms. Several pieces of evidence suggest the amygdala is the symptomaticogenic area of fear, but some studies reported other regions (mesial frontal regions, occipital, and parietal lobes) as the origin of this affective symptom [104,105,106,107]. Although autonomic symptoms are typical features in temporal lobe seizures, some of them may be also reported in frontal lobe epilepsy. Epigastric sensations are one of the reported symptoms of basal frontal epilepsy as gustatory, cardiac, and respiratory manifestations that are described in patients with frontal, insular, and opercular lobe epilepsy. Cold shivering and piloerection, infrequent symptoms of focal seizures, although most often associated with a left temporal lobe focus can also occur with a right temporal, as well as a frontal or parietal lobe focus [9]. Frontal lobe localization may also be suggested by urinary incontinence during focal epilepsy with secondary generalization [108]. Differential diagnosis between frontal or temporal lobe epilepsy could be challenging when ictal tachycardia is present. A recent study investigated the differences between TLE and FLE patients with ultra-short-term heart rate variability (HRV) analysis and found different HRV profiles in the pre-ictal, ictal, and postictal intervals in the two groups: the temporal lobe epilepsy patients exhibited elevated sympathetic or vagal activity during the pre-ictal and postictal condition, while the FLE patients showed a marked increment and decrement in sympathetic tone during the ictal period [109].
11.5 Autonomic Seizures and Autonomic Status Epilepticus in Self-Limited Epilepsy with Autonomic Seizure
The primary cause of autonomic seizures and autonomic status epilepticus in children is SeLEAS, formerly known as Panayiotopoulos syndrome or early onset benign occipital epilepsy [6, 110, 111]. SeLEAS is characterized by the onset in early childhood of focal autonomic seizures followed by a stereotypical onset and progression that are often prolonged. The epilepsy is self-limited, with remission typically within a few years from onset [2]. The mean duration of the disease is approximately 3 years [112]. The usual age at onset is between 3 and 6 years (70% of cases), and ranges from 1 to 14 years [113], with a peak at 5 years [113, 114]. The likelihood of having seizures after the age of 12 years is exceptional [114]. Antecedent and birth history are normal. Neurological examination, development, and cognition are normal [115, 116]. Both sexes are affected equally. SeLEAS accounts for 5% of childhood epilepsies between 1 and 14 years and 13% of childhood epilepsies between 3 and 6 years [117]. A history of febrile seizures is seen in 5–17% of patients. Seizure frequency is typically low, with approximately 25% of children having a single seizure only [118], the median total number of fits is two to three, and the prognosis is invariably excellent, with remission usually occurring within 1 year from onset [114, 118]. Focal autonomic seizures, with or without impaired awareness, are mandatory for diagnosis. Awareness is usually preserved at seizure onset and may fluctuate in degree of impairment as the seizure progresses. In a typical presentation, the child, able to speak and understand, complains “I feel sick,” looks pale, and shows autonomic symptoms and signs [110]. Autonomic features at onset may vary, but most frequently include retching, pallor, flushing, nausea, malaise, or abdominal pain. Vomiting, the most common autonomic manifestation, occurs in approximately 75% of children [6]. In others, only nausea or retching occurs, and in a few, emesis may not be apparent. Other autonomic manifestations may occur concurrently or appear later during the seizure such as pupillary (mydriasis, and, less often, miosis), temperature, and cardiorespiratory (breathing, pallor, cyanosis, and heart rate) changes. Incontinence of urine and/or feces, hypersalivation, and modifications of intestinal motility were also reported. Syncope may rarely occur. Seizures frequently evolve with eye and/or head deviation, generalized hypotonia, and focal clonic (hemiclonic) or focal to bilateral tonic–clonic seizure activity. More than 70% of seizures occur from sleep; the child may wake up with similar complaints while still aware or else may be found vomiting, conscious, confused, or unresponsive [110]. Seizures are often prolonged and can last longer than 30 min [113, 119, 120]. Electroencephalography is the most useful test in autonomic seizures. Multifocal spikes with high amplitude sharp-slow wave complexes (>200 μV) at various locations and predominant in the occipital regions can be present at disease onset [121] (Fig. 11.4). In some cases, the background activity could be normal [6]. During follow-up, abnormalities might move to either centrotemporal or frontopolar regions. Generalized abnormalities may also be seen [110, 122]. If persistent focal slowing is present, a structural brain abnormality should be sought as an alternative etiology. Diffuse slowing is not seen except in the postictal period [113, 120, 123, 124]. EEG abnormalities are activated both by sleep deprivation and by sleep when abnormalities often have a wider field and may be bilaterally synchronous. If seizures are recorded, ictal onset varies, but most have posterior onset [121]. The ictal pattern shows rhythmic slow activity intermixed with small spikes and/or fast activity [125]. Neuroimaging, if performed, shows no causal lesion. Brain MRI should be considered in cases with recurrent seizures or atypical presentations. Symptomatic autonomic epilepsy caused by heterogeneous brain lesions has been observed [113, 117, 126]. Nonspecific MRI findings should not exclude a diagnosis of SeLEAS [6]. Approximately 20% of patients may evolve to other self-limited focal epilepsies (SeLFEs), most commonly self-limited epilepsy with centrotemporal spikes (SeLECTS) [118]. Rarely, SeLEAS may evolve into epileptic encephalopathy with spike-and-wave activation in sleep (EE-SWAS). SeLEAS is probably genetically determined; however, no causative gene variants have been detected so far. There is a higher prevalence of febrile seizures in first-degree relatives and case reports of siblings with other SeLFEs [127]. SeLEAS does not usually require treatment, as the course of the disease is, in most cases, mild, and the prognosis is good [16]. It is crucial to differentiate the disease from other forms of epilepsy, especially occipital and structural epilepsy, and non-epileptic disorders [121]. Autonomic seizures and autonomic status epilepticus are easy to diagnose because of the characteristic clustering of clinical seizure semiology, which is often supported by interictal EEG findings. The main problem is to recognize emetic symptoms, ictal syncope, and other autonomic manifestations as seizure events and not to dismiss them or erroneously consider them as unrelated to the seizure and a feature of encephalitis, migraine, syncope, or gastroenteritis [128]. Autonomic seizures and autonomic status epilepticus are important to differentiate between SeLEAS and symptomatic causes. In SeLEAS, neurological state and mental state are normal and brain imaging is unremarkable. Conversely, in symptomatic cases, there are often abnormal neurological or mental symptomatology, abnormal brain imaging, and EEG background abnormalities [113].
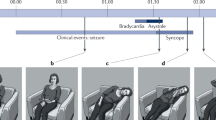
Ictal registration of a child with self-limited epilepsy with autonomic seizures (SeLEAS) (from Parisi P, et al. 2007 [121]): polygraphic recording included scalp EEG (8 channels), electrooculogram (LOC and ROC), chin electromyogram, ECG, nasal and oral airflow, thorax and abdominal movements. During sleep stage two, the seizure started (see arrow) with a run of fast spikes at 7 Hz involving principally the right occipital region (a), associated with tachycardia as the sole manifestation (minimal clinical manifestation: movement of the left arm). (b) Soon after the start and for approximately 10 min, with no clinical manifestations associated, the EEG showed the persistence of spike-and-wave at 3–4 Hz localized almost exclusively over the right occipital region, with rare spreading (see arrow) to the other EEG derivations. (c) A tonic conjugate deviation of the eyes to the left accompanied at the EEG by a rich content in high-amplitude slow waves in the theta and delta ranges predominate in the right hemisphere. (d) Ictal vomiting occurs 11 min after the onset of the seizure. (e) As repetitive vomiting stopped, the low-amplitude high frequency suddenly disappeared (see arrow) with the presence of post-ictal low-frequency components. (From Parisi P et al. Neurol Sci 2007; 28 [2]:72–9 with permission)
11.6 Autonomic Dysfunctions in Developmental and Epileptic Encephalopathies
Autonomic symptoms could be encountered in several developmental and epileptic encephalopathies (DEE) and may represent either an epileptic manifestation or, more frequently, may develop apart from the epileptic disorder strongly correlated with the burden of functional impairments [129]. Rett syndrome is a neurodevelopmental disorder that primarily affects females, characterized by consistently reported seizures and paroxysmal autonomic symptoms mostly in patients carrying the methyl-CpG-binding-protein 2 (MeCP2) or CDKL5 mutation [130, 131]. Autonomic features encompass peripheral vasomotor disturbances, breathing dysfunction during wakefulness, apnoea, and cardiac dysautonomia with susceptibility to arrhythmias [132]. Epilepsy is a core symptom of Rett syndrome, with prevalence as high as 60–90% [133]; however, the analysis of video-EEG demonstrated that the majority of clinically reported seizures did not have an autonomic correlate [134]. Dravet syndrome is an epileptic encephalopathy that develops in the first year of life presenting multiple seizure types [135]. The diagnosis is clinical, but most cases carry a mutation in the SCN1A gene encoding for neuronal sodium channels [10]. Half of the patients had temperature regulation problems; other features of autonomic dysfunction such as sweating, pupillary dilation, flushing, gastroparesis, and heart rate changes are also more commonly described in children with Dravet syndrome than controls [135, 136]. As compared to age- and sex-matched control groups of other epileptic syndromes and healthy controls, patients with Dravet syndrome displayed a relative predominance of sympathetic over parasympathetic activity when investigating the electrical characteristics of cardiac function [137]. Autonomic signs are also reported in most patients with the SCN8A mutation, mainly as the first manifestation of focal or focal to bilateral tonic/tonic-clonic seizure [138]. A stereotyped sequence of appearance has been frequently described with some signs occurring within the first seconds (flushing of the face, sometimes associated with sialorrhea, bradycardia, and hypopnea) and others such as tachycardia, polypnea, perioral cyanosis, and pallor that followed later during the seizure [138]. Tonic seizures with long-lasting apnea requiring ventilation are believed to be one of the characteristic features of patients with this mutation [139]. Likewise, a case of SCN8A-related encephalopathy with ictal asystole requiring cardiac pacemaker implantation has been described [140]. Manifestations such as breathing dysfunction, apnoea, and cardiac dysautonomia with susceptibility to arrhythmias may underlie a brainstem dysfunction and/or a channelopathy linking neural and cardiac dysfunction and may account for the higher risk of SUDEP described in patients with some DEE as compared to the general population [141]. Aspects of dysautonomic function may provide biomarkers of DEE disease severity [129] or may predict the onset of a DEE. A recent study characterizes the temporal changes in heart rate variability, a surrogate of a marker of autonomic functional state, in infants at risk of Infantile epileptic spasm syndrome (an age-dependent epileptic syndrome characterized by clusters of clinical spasms and typical electroencephalogram features) finding that certain early HRV metrics may be predictive of the clinical onset of the disease [142].
11.7 Involvement of the Autonomic Nervous System in SUDEP
People with epilepsy have a 24-fold increased risk of dying suddenly compared with the general population [143] and among the causes of premature deaths in patients with epilepsy, SUDEP represents a major cause [143, 144]. SUDEP is defined as the “sudden, unexpected, witnessed or unwitnessed, nontraumatic and non-drowning death, occurring in benign circumstances, in an individual with epilepsy, with or without evidence for a seizure and excluding documented status epilepticus, in which postmortem examination does not reveal a cause of death” [145]. SUDEP is an important risk in patients with intractable epilepsy, with a variable reported incidence across the studies [146, 147]. The reported incidence does not vary between the pediatric (1.11–1.45 per 1000 person-years in children and adolescents with epilepsy) [148, 149] and adult (1.20 per 1000 person-years with epilepsy) [146] populations. However, the studies that have identified the incidence of SUDEP have not considered the different and multiple causes and types of epilepsy. The pathophysiology of SUDEP remains unknown, most cases of sudden death are unwitnessed and post-mortem examinations are often lacking [39, 150]. The potential mechanisms proposed involve prominent primary or secondary involvement of the autonomic nervous system in the form of central or obstructive apnea or both, cardiac arrhythmia, autonomic dysregulation, and hypoxia. Available data from witnessed and monitored SUDEP cases suggest that, in most cases, a convulsive seizure triggers catastrophic cardio-respiratory dysfunction that results in death [151, 152]. The autonomic system collapse, beginning with a respiratory dysfunction followed by heart failure, supports the notion that the brainstem structures that control autonomic function are involved in the mechanism of SUDEP [153]. The MORTEMUS study, which is the largest study to date describing cardiorespiratory function at the time of death in epilepsy, reported all SUDEP deaths occurring after a convulsive seizure [151]. In those cases, a seizure appeared to trigger progressive bradycardia and apnea beginning during the immediate postictal period; terminal apnea occurred before terminal asystole in all cases. It is arguable that more severe and drug-resistant disease has a greater risk of SUDEP [154, 155]. Nevertheless, SUDEP can occur early in the disease course or in individuals with a condition that is usually considered benign [156, 157] and, there are cases of non-seizure–related SUDEP, which reveal that a seizure is not necessary to trigger severe terminal cardiorespiratory dysfunction resulting in death [158]. In a cohort of three patients with refractory epilepsy, all patients died in the epilepsy monitoring unit during continuous video-EEG monitoring [158] and there was no clinical seizure and no ictal change on EEG preceding death. In all cases, there was progressive cardiorespiratory dysfunction associated with suppression of the EEG. In two cases there was tachycardia and tachypnea preceding bradypnea and bradycardia followed by terminal apnea, which was then followed by terminal asystole, a pattern that is similar to the progression of cardiorespiratory dysfunction noted in the MORTEMUS study [151]. These data suggest that catastrophic autonomic network dysfunction may occur due to initial severe brainstem dysfunction, which may be responsible for the highly abnormal cardiorespiratory patterns [159]. Interestingly, in focal and generalized epilepsies, autonomic functional changes were observed not only during the ictal period, but also during interictal and postictal periods where all aspects of the autonomic function, including parasympathetic, sympathetic, and adrenal medullary systems may be affected [9]. The magnitude of the sympathetic activation and parasympathetic suppression in each type of seizure or epilepsies may also be an important factor to be considered, as they may influence the probability risk of SUDEP [160]. HRV, which reflects the balance between sympathetic and parasympathetic activity in the autonomic nervous system, provides a physiological perspective for the examination of cardiac pathologies [161]. Patients with epilepsy often have interictal autonomic dysfunction, as is observable from the HRV abnormalities reported in both focal (particularly in temporal lobe epilepsy) and generalized epilepsy [162,163,164,165]. Children with drug-resistant epilepsy showed lower HRV values compared to children with controlled epilepsy or healthy children [166]. However, the chronically reduced parasympathetic effect may predispose drug-resistant epileptic children to a more severe stress response during seizures [166]. Patients with Dravet syndrome, which is highly associated with drug-resistant epilepsy and SUDEP, also have reduced HRV [137, 167]. In support, concurrent seizure activity in the temporal lobes significantly increased the heart rate and decreased the HRV in patients with refractory epilepsy, suggesting that there was an autonomic imbalance that tended to sympathetic dominance due to seizures [168]. There is also one case report of a man with refractory epilepsy and SUDEP in whom serial studies showed a sudden increase in parasympathetic activity, as measured by high-frequency power and the ratio between cardiac vagal index and cardiac sympathetic index during the 1 day to 30 min preceding death [169]. However, thus far, there are no clear specific HRV biomarkers for SUDEP. Surges et al. (2009) compared HRV in seven patients with SUDEP with HRV in seven control patients and found no significant differences in interictal HRV measures between the groups [170]. Although the MORTEMUS and other available SUDEP data suggest that primary cardiogenic causes of SUDEP are rare, it is still possible that abnormal HRV might contribute to SUDEP in a minority of cases. Each autonomic sign should be evaluated in the context of preceding autonomic manifestations. For example, asystole could be the first ictal expression, but could also follow IA or ictal hypotension. IA was thought to be a possible mechanism of SUDEP [171, 172]. However, several observations indicate that IA is not invariably linked to SUDEP [31, 173, 174]. Another important aspect to consider is the seizure type and the timing of the event. For instance, ictal asystole is predominantly seen in focal seizures of temporal lobe onset, whereas postictal asystole is strongly associated with TCSs, including both primary generalized TCSs and focal-to-bilateral TCSs [33]. The same holds for apnoea: ictal central apnoea is strongly linked to focal temporal lobe seizures, whereas postictal central apnoea is seen only in the context of TCSs (41 42). Eyewitness reports suggest that around 10% of witnessed SUDEP events occur in the absence of apparent seizure activity [39, 152, 175, 176], indicating that seizures are not required as proximate triggers for SUDEP. It is reasonable to assume that in some or even most of these cases, sudden death was caused by cardiac arrhythmias. Retrospective analysis of multi-day ECG data obtained during video-EEG monitoring from patients who subsequently died due to SUDEP found that SUDEP patients had greater increases in heart rate during seizures than in other refractory control epilepsy patients [177]. Heart rate alterations are the most studied and probably the most frequent ictal autonomic signs, with a prevalence of 38–100% [21]. The degree of autonomic change varies according to the seizure type. Ictal tachycardia seems to be more prominent in seizures originating from the temporal and orbitofrontal cortex and in TCSs [22, 168, 178,179,180,181,182,183]. Depth EEG recordings in people with temporal lobe epilepsy (TLE) indicate that ictal tachycardia coincides with seizure activity in the anterior hippocampus and amygdala [181]. The spread of seizure activity to subregions of the ipsilateral and contralateral hemispheres correlates with heart rate increase [168, 182, 184]. Heart rate alterations could be the earliest clinical sign of seizure onset and it might be a significant tool for seizure detection [183]. In multi-day recordings in patients admitted to epilepsy monitoring units, almost 40% of patients had ictal cardiac arrhythmias or repolarization abnormalities, including bundle branch block, atrial fibrillation, supraventricular tachycardia, asystole, and other abnormalities [36, 185]. In a prospective cohort study, patients with chronic epilepsy showed significantly higher T-wave alternation and lower HRV values compared to patients with newly diagnosed epilepsy [186]. Furthermore, cardiac repolarization abnormalities are found in epilepsy patients also in association with seizures [38, 187, 188]. Convulsive and longer seizures may increase the risk for ictal Electrocardiogram abnormalities [36]. Ventricular tachyarrhythmias may occur more frequently in patients with epilepsy (possibly related to increased risk of cardiovascular disease in this population) and could be an underestimated cause of SUDEP [39, 189, 190]. In a monitored patient without cardiac pathologies, who experienced sudden onset of ventricular tachycardia (VT) and ventricular fibrillation (VF) following a focal-to-bilateral TCS [38] a SUPED was documented. However, most of the VT/VF events occurred in patients with pre-existing or acute heart conditions [39]. However, most forms of cardiac arrhythmias can be observed in people with epilepsy, particularly in association with seizures [191]. Ictal bradycardia has been reported to occur in up to 6.4% of focal seizures and up to 13.6% of people with epilepsy undergoing video-EEG monitoring [191]. Long-term EKG recording (between 4 and 22 months) via implantable loop recorders in patients with refractory epilepsy suggest that ictal and interictal bradycardia may occur relatively commonly in this population, with 8/39 patients in both studies combined having bradycardia or asystole [155, 192]. Other ictal cardiovascular manifestations, such as blood pressure, lack precise prevalence because they are not routinely assessed during EEG recordings. The resting awake interictal heart rate (HR) and blood pressure (BP) in SUDEP cases and control epilepsy groups (refractory and controlled) are similar but there is a trend toward a higher diastolic BP and more stable (less variable) HR over time in individuals who subsequently died due to SUDEP [193]. However, increases in blood pressure can be seen across all focal seizure types and in focal-to-bilateral TCSs [194]. While these findings need to be confirmed in larger populations, they again support the possibility that patients at risk for SUDEP may have underlying autonomic dysfunction, which may increase their risk for death in the setting of a seizure. Blood pressure is regulated by the baroreflex, whereby significant deterioration in its sensitivity has been observed in the early postictal period following bilateral/generalized convulsive seizures [195]. This may be due to increased muscle contractions, a large amount of catecholamine released, and impaired brainstem function [195]. While most cases of SUDEP were probably caused by a cardiorespiratory failure during the early postictal period following generalized convulsive seizures, recent studies have reported that impaired baroreflex sensitivity may also cause life-threatening systemic blood pressure to decrease after generalized convulsive seizures [196]. In addition to the cardiological autonomic involvement, the respiratory one has also been underlined by scientific evidence. The MORTEMUS study provides clear evidence of respiratory dysfunction in SUDEP. In patients with SUDEP in the MORTEMUS series, convulsive seizures were followed by terminal apnea and then asystole [151]. In total, 75% of people who succumb to SUDEP are found in the prone position, (which is likely to further aggravate postictal breathing disturbances) [151, 197] and are unwitnessed, though there is often evidence of a recent seizure (e.g., tongue bite, urinary incontinence, or body positioning to suggest a recent seizure) at the time of death [197,198,199]. Ictal central apnea strongly correlates with focal epilepsy, particularly temporal lobe epilepsy. In 56 patients with focal epilepsy, approximately one-third of focal seizures with or without generalization were accompanied by desaturations below 90% [43]. In another cohort, ictal central apnea occurred in 47% of 109 patients (36.5% of 312 seizures), most notably in temporal lobe epilepsy [41]. Dlouhy et al. (2015) found that electrical stimulation of the amygdala in patients undergoing intracranial EEG monitoring resulted in central apnea [200]. It has also been observed that seizures spreading to the amygdala may cause central apnea and oxygen desaturation in patients with persistent epilepsy [200]. In pediatric patients with refractory epilepsy who underwent intracranial electroencephalography, apnea formation was found to occur simultaneously with the spread of the seizure to the amygdala area responsible for respiratory suppression [201]. This suggests that there may be a functional link between the amygdala and respiration in the brainstem which may cause respiratory loss as a result of epileptiform activity. In a study by Park et al., focal to the bilateral tonic–clonic seizures or generalized tonic–clonic seizures which caused ictal/postictal hypoxemia more than 125 s had a statistically significant association with high-risk cardiac arrhythmias (nonsustained ventricular tachycardia, bradyarrhythmia, and sinus pauses). The odds ratio for the occurrence of arrhythmia was 7.86 for desaturation durations ≥125 s versus desaturations <125 s (p = 0.005). The odds ratio increased to 13.09 for desaturation durations ≥150 s (p < 0.001) [202]. These studies show that the peri-ictal respiratory decline may be the critical initial node in the series of terminal events resulting in sudden death. Animal models have been studied to identify the basic neurobiological mechanisms of respiratory arrest with seizures. It has been well-studied that 5-hydroxytryptamine (5-HT) neurons play a critical role in maintaining respiratory drive. Provoked audiogenic seizures in DBA/2 mice which lack several 5 HT receptor proteins in the brainstem lead to death due to respiratory arrest, which can be prevented with oxygenation [203]. Notably, seizure-related death is reduced using selective serotonin reuptake inhibitors (SSRI) [204, 205]. Additionally, adenosine antagonists may also significantly reduce ictal apnea [206]. Reduced 5-HT levels and immature 5-HT neurons in the medulla have also been noted in infants who died of sudden infant death syndrome (SIDS), which suggests a possible role of 5-HT axis dysfunction as a cause of sudden unexplained death [207]. Further investigation is needed to evaluate whether SSRIs and adenosine antagonists might have a role in reducing ictal apnea in humans. Another characteristic feature of the early postictal phase was the generalized flattening of the EEG trace (postictal generalized EEG suppression, PGES). The origin and clinical importance of PGES are not yet fully understood [208], but it might be a condition for the neurovegetative breakdown in TCS-related SUDEP. Clinical and electrophysiological data obtained from children with epilepsy revealed that PGES was associated with peri-ictal tachycardia and hypoxemia [209]. However, in a clinical study examining generalized convulsive seizures retrospectively, the percentage of postictal unresponsiveness, including oropharyngeal immobility, was found to be higher in patients with PGES after seizures [210]. This suggests that postictal immobility and PGES are associated with peri-ictal respiratory disorders [211]. Electrodermal activity (EDA) measures changes in the electrical conductance of the skin due to sympathetic neuronal activity [212]. One study evaluating primarily children found that there is a surge of EDA (correlating with increased sympathetic activation) and suppression of high-frequency power of HRV (correlating with parasympathetic suppression) after tonic–clonic seizures [160]. This post-ictal autonomic dysregulation correlated to increased duration of PGES in this study. These data suggest that PGES, which may be a biomarker for SUDEP, could be associated with significant autonomic dysfunction during the critical post-ictal period when SUDEP most often occurs. Additional investigation showed that age may affect the degree of sympathetic and parasympathetic activity following seizures [213]. Adults tend to have longer durations of PGES Sarkis et al. also found that adults had longer durations of PGES and that the duration of PGES correlated with the degree of sympathetic activation as measured by EDA [213]. However, after controlling for PGES duration, pediatric patients were found to have stronger sympathetic activation as well as greater parasympathetic suppression than adults. These age-dependent findings may correlate with the variable incidence of SUDEP seen in different age groups. From the brain structural view, a volume loss of brainstem regions, a structure with a crucial role in autonomic control, has been also observed in SUDEP cases compared to controls [214] suggesting a possible link between structural and functional autonomic pathology. SUDEP victims show significant tissue loss in areas essential for cardiorespiratory recovery and enhanced volumes in areas that trigger hypotension or impede respiratory patterning [215]. In detail, substantial bilateral gray matter loss appeared in SUDEP cases in the medial and lateral cerebellum. The periaqueductal gray, left posterior and medial thalamus, left hippocampus, and bilateral posterior cingulate also showed volume loss in SUDEP [215]. In a retrospective study, posterior thalamic grey matter volume, an area mediating oxygen regulation, was reduced in cases of SUDEP and subjects at high risk, when compared to controls [216]. The T1 images of individuals with temporal lobe epilepsy (TLE) revealed a volume loss in the dorsal mesencephalon region, which plays a role in autonomic control [214]. While the 3T magnetic resonance imaging (MRI) findings of patients with focal epilepsy showed large atrophy in the autonomic nuclei of the medulla oblongata’s periaqueductal gray area instead [153]. Also, some neurotransmitters may play a role in the etiopathogenesis of SUDEP. Acetylcholine (ACh), the main stimulant of the autonomic nervous system, mediates signal transmission through cholinergic and nicotinic receptors. Accumulating evidence indicates that dysfunction of nicotinic ACh receptors, which are widely expressed in hippocampal and cortical neurons, may be significantly implicated in the pathogenesis of epilepsy [217]. It has also been reported that M1 muscarinic receptors in the medial septum region of the hippocampus integrate the inputs of vagal afferents from the brainstem into the hippocampus [218]. In this context, it is important to investigate the possible effects of M1 receptors on epilepsy and SUDEP [219]. On the other hand, deficits in serotonergic signaling might also be involved in seizure-related breathing disturbances. Animal data suggest that postictal deficits in serotonergic neurotransmission can impair the arousal reaction to postictally elevated CO2 levels and cause hypoventilation or respiratory arrest [207], which can be prevented by the administration of serotonin reuptake inhibitors [220]. Moreover, in a post-mortem study, the depletion of brainstem neurons involved in serotonin and galanin signaling was greater in SUDEP cases than in controls [221].
11.7.1 Genetic Epilepsy and SUDEP
A growing body of evidence points to a genetic susceptibility to cardiorespiratory and autonomic dysfunction in epilepsy. Animal data suggest that an ion channelopathy may cause both epilepsy and alter the autonomic control of the heart [222]. Epilepsy-related alterations in the cardiac expression of sodium (Nav1.1/1.5), potassium (Kv4.2/4.3), calcium (NCX1), and cationic (HCN2/4) channels have thus been reported in animal models [223]. It remains to be determined whether or not this mechanism is associated with impaired vegetative regulation in patients with epilepsy and especially, with the risk of SUDEP. In an analysis of the entire exome sequencing of 61 SUDEP cases, mutations known to cause long QT syndrome were found in 7% of cases and an additional 15% had candidate variants in potentially predisposing genes to malignant cardiac arrhythmias [224]. Similarly, the effect of the SCN1A mutation on heart function may partly explain the increased risk of mortality in Dravet syndrome [225,226,227]. Other genetic defects might contribute to both epilepsy and cardiac arrhythmias in some individuals, for example, SCN5A, KCNQ1, and KCNH2 [172, 228, 229]. For individuals with pathogenic variants in genes including SCN1A, SCN1B, SCN8A, SCN2A, GNB5, KCNA1, and DEPDC5, there are varying degrees of evidence to suggest an increased risk for sudden death. Why the risk for sudden death is higher is not completely clear; however, in many cases, pathogenic variants in these genes are also associated with autonomic dysfunction, which is hypothesized as a contributing factor to SUDEP [230]. Several ion channel genes whose mutations are involved in cardiac arrhythmias are also expressed in the brain (Fig. 11.5) [231]. For example, the SCN5A gene, whose mutation is associated with long QT syndrome, is also expressed in the brain and is associated with epilepsy [232].
Main channelopathies associated with epilepsy and arrhythmias. AV atrioventricular, CPVT catecholaminergic polymorphic ventricular tachycardia, VF ventricular fibrillation. (From Costagliola G, et al. 2021 [231] with permission)
11.7.2 Detection and Prevention of SUDEP
Seizure control is the most important potentially modifiable risk factor of SUDEP. To best participate in their care, patients should be knowledgeable about the potential risks of seizures, including SUDEP. The American Academy of Neurology and American Epilepsy Society recommend that clinicians counsel epilepsy patients regarding SUDEP. Survey studies of epilepsy patients and family members of SUDEP patients have shown that they prefer to know about the risk factors of SUDEP during the early phase of management [233, 234]. Unfortunately, some data suggest that only a small minority of neurologists counsel all of their patients about SUDEP [235]. Ictal autonomic changes and interictal autonomic dysfunction might serve as diagnostic clues, providing targets for seizure detection. Retrospective studies suggest that heart rate alterations can be prevented by improving seizure control using ASMs [236,237,238]. ASMs often serve as a double-edged sword for epileptic patients. Although ASMs are mainly designed to help epileptic patients control their seizures, some might worsen their condition leading to other health complications [239], including cardiorespiratory dysfunctions such as myocardial infarction [20, 240], arrhythmias [20], respiratory depression [239], and even cardiovascular death or SUDEP [240]. This has been particularly reported with sodium channel blockers [20], including the risk of an atrioventricular block with carbamazepine [241], sinus pause and hypotension with rapid administration of phenytoin [20, 242] or atrioventricular block or atrial fibrillation with lacosamide [243,244,245]. However, no formal relationship has been established between these drug-related adverse events and ictal arrhythmias [20]. A meta-analysis by Ryvlin reported that adjunctive ASMs might reduce the SUDEP risk by seven times when given to patients with intractable epilepsy [246]. The impact of epilepsy surgery on the risk of SUDEP is more controversial [146], however, lower mortality rates were observed in successful versus failed TLE surgery [155, 247,248,249]. In patient with drug-resistant epilepsy, pacemaker implantation is advisable to reduce the risk of falls and life-treating injuries, although some individuals might not benefit from these devices’ injuries [188, 236, 250,251,252]. Of course, ASM adherence and surgical interventions, when appropriate, may improve seizure control and reduce the risk of SUDEP. The effect of vagus nerve stimulation (VNS) on autonomic function remains uncertain. Heart changes associated with VNS are rare. Few cases of VNS-induced bradycardia have been reported. In addition, data on the alterations in the parasympathetic tone of the cardiovascular system induced by VNS are contradictory [253]. VNS was associated with a reduced SUDEP risk [254, 255]. VNS seems to reduce abnormally elevated levels of T-wave alternans, thereby stabilizing the electrical properties of the heart [256]. However, whether this intervention could help to reduce the risk of sudden cardiac death due to ventricular tachycardia and ventricular fibrillation (VT/VF) is currently unknown. Prone position and post-ictal immobility are often cited in SUDEP cases, and some data suggest that nocturnal supervision might reduce the risk of SUDEP [257]. A Cochrane Review and the American Academy of Neurology–American Epilepsy Society SUDEP guidelines concluded that only very-low-certainty (Grading of Recommendations Assessment, Development, and Evaluation) and level C (modified Grading Recommendations Assessment) evidence was available to support the preventive impact of nocturnal supervision on SUDEP risk [146, 258]. This evidence was derived from retrospective case–control studies [254, 257, 259] and is supported by the observation that the majority of SUDEP events occur at night, during sleep in non-supervised individuals [151, 175, 199]. Epilepsy monitoring unit data from the MORTEMUS study also suggests that an immediate nonspecific postictal intervention from a caregiver is likely to prevent SUDEP [151]. Nursing interventions such as stimulating and turning the patient to the lateral position and suction with or without supplemental oxygenation have been reported to shorten the duration of peri-ictal hypoxemia and seizure duration [260, 261]. However, currently, no guidelines exist on the use of supplemental oxygen with seizures, and the potential benefits must be weighed against the significant cost and risks of home oxygen. Currently, there have been efforts to utilize the autonomic response to treat/reduce seizures and eventually SUDEP risk, in drug-resistant epilepsy patients. For example, autonomic biofeedback therapy has shown some promising results in reducing seizure frequency in drug-resistant temporal lobe epileptic patients by using their galvanic skin response (a measure of sympathetic activation) [262]. This suggests that changes in autonomic network control such as blood pressure and heart rate may be monitored to not only predict and measure seizures but also be harnessed for treatment strategies against epilepsy. These autonomic responses may also be used to record and monitor nocturnal seizures which may help to deter SUDEP [263]. Over the past 10 years, there has been a growing interest in the potential applications of mobile health technologies for seizure detection, with the objective of faster caregivers’ intervention and decreased risk of seizure-related injuries [161, 179, 264]. While detection of generalized TCSs has shown promising results with utilization either alone or in combination with accelerometers, automatic video detection, surface EMG, and bed alarms [265, 266], these approaches are much less sensitive for focal seizures. While it is clear that pacemaker implantation can be very helpful in preventing ictal syncope (i.e., syncope due to ictal asystole with subsequent hypotension and cerebral hypoperfusion) and falls, it is not clear that pacemaker implantation can prevent SUDEP. Schuele et al. found that when pacemakers were implanted in patients with ictal asystole and followed for 5 years, the risk of recurrent asystole appears to be low and that asystole may be a benign event [267, 268]. In this panorama, an interesting perspective remains the development of technologies capable of early detection of autonomic alterations and providing warnings of different types of seizures, thus reducing the risk of SUDEP.
Abbreviations
- ASMs:
-
Anti-seizure medications
- CAN:
-
Central autonomic network
- DEE:
-
Developmental and epileptic encephalopathies
- EDA:
-
Electrodermal activity
- EEG:
-
Electroencephalogram
- EE-SWAS:
-
Epileptic encephalopathy with spike-and-wave activation in sleep
- HRV:
-
Heart rate variability
- IA:
-
Ictal apnoea
- ILAE:
-
International League Against Epilepsy
- PGES:
-
Postictal generalized EEG suppression
- SeLEAS:
-
Self-limited epilepsy with autonomic seizures
- SeLECTS:
-
Self-limited epilepsy with centrotemporal spikes
- SeLFE:
-
Self-limited focal epilepsies of childhood
- SUDEP:
-
Sudden unexpected death in epilepsy
- TCSs:
-
Tonic-clonic seizures
- TLE:
-
Temporal lobe epilepsy
- VNS:
-
Vagus nerve stimulation
References
Fisher RS, van Emde BW, Blume W, Elger C, Genton P, Lee P, Engel J Jr. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470–2. https://doi.org/10.1111/j.0013-9580.2005.66104.x.
Ferrie CD, Caraballo R, Covanis A, Demirbilek V, Dervent A, Fejerman N, Fusco L, Grünewald RA, Kanazawa O, Koutroumanidis M, Lada C, Livingston JH, Nicotra A, Oguni H, Martinovic Z, Nordli DR Jr, Parisi P, Scott RC, Specchio N, Verrotti A, Vigevano F, Walker MC, Watanabe K, Yoshinaga H, Panayiotopoulos CP. Autonomic status epilepticus in Panayiotopoulos syndrome and other childhood and adult epilepsies: a consensus view. Epilepsia. 2007;48(6):1165–72. https://doi.org/10.1111/j.1528-1167.2007.01087.x. Epub 2007 Apr 18.
Baumgartner C, Koren J, Britto-Arias M, Schmidt S, Pirker S. Epidemiology and pathophysiology of autonomic seizures: a systematic review. Clin Auton Res. 2019;29(2):137–50. https://doi.org/10.1007/s10286-019-00596-x. Epub 2019 Feb 25.
Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E, Jansen FE, Lagae L, Moshé SL, Peltola J, Roulet Perez E, Scheffer IE, Zuberi SM. Operational classification of seizure types by the International League Against Epilepsy: position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):522–30. https://doi.org/10.1111/epi.13670. Epub 2017 Mar 8.
Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, Hirsch E, Jain S, Mathern GW, Moshé SL, Nordli DR, Perucca E, Tomson T, Wiebe S, Zhang YH, Zuberi SM. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512–21. https://doi.org/10.1111/epi.13709. Epub 2017 Mar 8.
Specchio N, Wirrell EC, Scheffer IE, Nabbout R, Riney K, Samia P, Guerreiro M, Gwer S, Zuberi SM, Wilmshurst JM, Yozawitz E, Pressler R, Hirsch E, Wiebe S, Cross HJ, Perucca E, Moshé SL, Tinuper P, Auvin S. International League Against Epilepsy classification and definition of epilepsy syndromes with onset in childhood: position paper by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022;63(6):1398–442. https://doi.org/10.1111/epi.17241. Epub 2022 May 3.
Mielke H, Meissner S, Wagner K, Joos A, Schulze-Bonhage A. Which seizure elements do patients memorize? A comparison of history and seizure documentation. Epilepsia. 2020;61(7):1365–75. https://doi.org/10.1111/epi.16550. Epub 2020 Jun 9.
Panayiotopoulos CP. Epileptic seizures and their classification. In: A clinical guide to epileptic syndrome and their treatment. 2nd ed. London: Springer-Verlag; 2007. p. 17–56.
Devinsky O. Effects of seizures on autonomic and cardiovascular function. Epilepsy Curr. 2004;4(2):43–6. https://doi.org/10.1111/j.1535-7597.2004.42001.x.
Moseley BD. Seizure-related autonomic changes in children. J Clin Neurophysiol. 2015;32(1):5–9. https://doi.org/10.1097/WNP.0000000000000138.
Baumgartner C, Lurger S, Leutmezer F. Autonomic symptoms during epileptic seizures. Epileptic Disord. 2001;3(3):103–16.
Freeman R, Schachter SC. Autonomic epilepsy. Semin Neurol. 1995;15(2):158–66. https://doi.org/10.1055/s-2008-1041019.
Sklerov M, Dayan E, Browner N. Functional neuroimaging of the central autonomic network: recent developments and clinical implications. Clin Auton Res. 2019;29(6):555–66. https://doi.org/10.1007/s10286-018-0577-0. Epub 2018 Nov 23.
Benarroch EE. The central autonomic network: functional organization, dysfunction, and perspective. Mayo Clin Proc. 1993;68(10):988–1001. https://doi.org/10.1016/s0025-6196(12)62272-1.
Bennaroch EE. The autonomic nervous system: basic anatomy and physiology. Contin Lifelong Learn Neurol. 2007;13(6 (Autonomic Disorders)):13–32.
Zontek A, Paprocka J. Gastrointestinal and autonomic symptoms—how to improve the diagnostic process in Panayiotopoulos syndrome? Children (Basel). 2022;9(6):814. https://doi.org/10.3390/children9060814.
Graziosi A, Pellegrino N, Di Stefano V, Raucci U, Luchetti A, Parisi P. Misdiagnosis and pitfalls in Panayiotopoulos syndrome. Epilepsy Behav. 2019;98(Pt A):124–8. https://doi.org/10.1016/j.yebeh.2019.07.016. Epub 2019 Jul 29.
Goodman JH, Stewart M, Drislane FW. Autonomic disturbances. In: Engel J, Pedley TA, editors. Epilepsy, a comprehensive textbook, vol. 3. 2nd ed. Lippincott William & Wilkins; 2008. p. 1999–2005.
Russell AE. Cessation of the pulse during the onset of epileptic fits, with remarks on the mechanism of fits. Lancet. 1906;168:152–4. https://doi.org/10.1016/S0140-6736(01)30477-4.
Shmuely S, van der Lende M, Lamberts RJ, Sander JW, Thijs RD. The heart of epilepsy: current views and future concepts. Seizure. 2017;44:176–83. https://doi.org/10.1016/j.seizure.2016.10.001. Epub 2016 Oct 26.
Eggleston KS, Olin BD, Fisher RS. Ictal tachycardia: the head-heart connection. Seizure. 2014;23(7):496–505. https://doi.org/10.1016/j.seizure.2014.02.012. Epub 2014 Mar 6.
Surges R, Cho CA, Walker MC. Enhanced QT shortening and persistent tachycardia after generalized seizures. Neurology. 2010;74(5):421–6. https://doi.org/10.1212/WNL.0b013e3181ccc706.
Oppenheimer SM, Gelb A, Girvin JP, Hachinski VC. Cardiovascular effects of human insular cortex stimulation. Neurology. 1992;42(9):1727–32. https://doi.org/10.1212/wnl.42.9.1727.
Oppenheimer S, Cechetto D. The insular cortex and the regulation of cardiac function. Compr Physiol. 2016;6(2):1081–133. https://doi.org/10.1002/cphy.c140076.
Chouchou F, Mauguière F, Vallayer O, Catenoix H, Isnard J, Montavont A, Jung J, Pichot V, Rheims S, Mazzola L. How the insula speaks to the heart: cardiac responses to insular stimulation in humans. Hum Brain Mapp. 2019;40(9):2611–22. https://doi.org/10.1002/hbm.24548. Epub 2019 Feb 28.
Hirsch M, Altenmüller DM, Schulze-Bonhage A. Latencies from intracranial seizure onset to ictal tachycardia: a comparison to surface EEG patterns and other clinical signs. Epilepsia. 2015;56(10):1639–47. https://doi.org/10.1111/epi.13117. Epub 2015 Aug 18.
Mayer H, Benninger F, Urak L, Plattner B, Geldner J, Feucht M. EKG abnormalities in children and adolescents with symptomatic temporal lobe epilepsy. Neurology. 2004;63(2):324–8. https://doi.org/10.1212/01.wnl.0000129830.72973.56.
Chan SW, Dervan LA, Watson RS, Anderson AE, Lai YC. Epilepsy duration is an independent factor for electrocardiographic changes in pediatric epilepsy. Epilepsia Open. 2021;6(3):588–96. https://doi.org/10.1002/epi4.12519. Epub 2021 Jul 19.
Leutmezer F, Schernthaner C, Lurger S, Potzelberger K, Baumgartner C. Electrocardiographic changes at the onset of epileptic seizures. Epilepsia. 2003;44:348–54.
Moseley B, Bateman L, Millichap JJ, Wirrell E, Panayiotopoulos CP. Autonomic epileptic seizures, autonomic effects of seizures, and SUDEP. Epilepsy Behav. 2013;26(3):375–85. https://doi.org/10.1016/j.yebeh.2012.08.020. Epub 2012 Oct 23.
Lanz M, Oehl B, Brandt A, Schulze-Bonhage A. Seizure induced cardiac asystole in epilepsy patients undergoing long term video-EEG monitoring. Seizure. 2011;20(2):167–72. https://doi.org/10.1016/j.seizure.2010.11.017. Epub 2010 Dec 22.
Rocamora R, Kurthen M, Lickfett L, Von Oertzen J, Elger CE. Cardiac asystole in epilepsy: clinical and neurophysiologic features. Epilepsia. 2003;44(2):179–85. https://doi.org/10.1046/j.1528-1157.2003.15101.x.
van der Lende M, Surges R, Sander JW, Thijs RD. Cardiac arrhythmias during or after epileptic seizures. J Neurol Neurosurg Psychiatry. 2016;87(1):69–74. https://doi.org/10.1136/jnnp-2015-310559. Epub 2015 Jun 2.
Tényi D, Gyimesi C, Kupó P, Horváth R, Bóné B, Barsi P, Kovács N, Simor T, Siegler Z, Környei L, Fogarasi A, Janszky J. Ictal asystole: a systematic review. Epilepsia. 2017;58(3):356–62. https://doi.org/10.1111/epi.13644. Epub 2016 Dec 18.
Schuele SU, Bermeo AC, Alexopoulos AV, Locatelli ER, Burgess RC, Dinner DS, Foldvary-Schaefer N. Video-electrographic and clinical features in patients with ictal asystole. Neurology. 2007;69(5):434–41. https://doi.org/10.1212/01.wnl.0000266595.77885.7f.
Nei M, Ho RT, Sperling MR. EKG abnormalities during partial seizures in refractory epilepsy. Epilepsia. 2000;41:542–8.
Zijlmans M, Flanagan D, Gotman J. Heart rate changes and ECG abnormalities during epileptic seizures: prevalence and definition of an objective clinical sign. Epilepsia. 2002;43(8):847–54. https://doi.org/10.1046/j.1528-1157.2002.37801.x.
Surges R, Shmuely S, Dietze C, Ryvlin P, Thijs RD. Identifying patients with epilepsy at high risk of cardiac death: signs, risk factors and initial management of high risk of cardiac death. Epileptic Disord. 2021;23(1):17–39. https://doi.org/10.1684/epd.2021.1254.
Lamberts RJ, Blom MT, Wassenaar M, Bardai A, Leijten FS, de Haan GJ, Sander JW, Thijs RD, Tan HL. Sudden cardiac arrest in people with epilepsy in the community: circumstances and risk factors. Neurology. 2015;85(3):212–8. https://doi.org/10.1212/WNL.0000000000001755. Epub 2015 Jun 19.
Van Buren JM. Some autonomic concomitants of ictal automatism; a study of temporal lobe attacks. Brain. 1958;81(4):505–28. https://doi.org/10.1093/brain/81.4.505.
Lacuey N, Zonjy B, Hampson JP, Rani MRS, Zaremba A, Sainju RK, Gehlbach BK, Schuele S, Friedman D, Devinsky O, Nei M, Harper RM, Allen L, Diehl B, Millichap JJ, Bateman L, Granner MA, Dragon DN, Richerson GB, Lhatoo SD. The incidence and significance of periictal apnea in epileptic seizures. Epilepsia. 2018;59(3):573–82. https://doi.org/10.1111/epi.14006. Epub 2018 Jan 16.
Vilella L, Lacuey N, Hampson JP, Rani MRS, Loparo K, Sainju RK, Friedman D, Nei M, Strohl K, Allen L, Scott C, Gehlbach BK, Zonjy B, Hupp NJ, Zaremba A, Shafiabadi N, Zhao X, Reick-Mitrisin V, Schuele S, Ogren J, Harper RM, Diehl B, Bateman LM, Devinsky O, Richerson GB, Tanner A, Tatsuoka C, Lhatoo SD. Incidence, recurrence, and risk factors for peri-ictal central apnea and sudden unexpected death in epilepsy. Front Neurol. 2019;10:166. https://doi.org/10.3389/fneur.2019.00166.
Bateman LM, Li CS, Seyal M. Ictal hypoxemia in localization-related epilepsy: analysis of incidence, severity and risk factors. Brain. 2008;131(Pt 12):3239–45. https://doi.org/10.1093/brain/awn277. Epub 2008 Oct 24.
Seyal M, Bateman LM. Ictal apnea linked to contralateral spread of temporal lobe seizures: intracranial EEG recordings in refractory temporal lobe epilepsy. Epilepsia. 2009;50:2557–62.
Leutmezer F, Serles W, Lehrner J, Pataraia E, Zeiler K, Baumgartner C. Postictal nose wiping: a lateralizing sign in temporal lobe complex partial seizures. Neurology. 1998;51(4):1175–7. https://doi.org/10.1212/wnl.51.4.1175.
Hirsch LJ, Lain AH, Walczak TS. Postictal nosewiping lateralizes and localizes to the ipsilateral temporal lobe. Epilepsia. 1998;39(9):991–7. https://doi.org/10.1111/j.1528-1157.1998.tb01449.x.
Wennberg R. Electroclinical analysis of postictal noserubbing. Can J Neurol Sci. 2000;27(2):131–6.
Asadi-Pooya AA, Shabo L, Wyeth D, Nei M. Ictal coughing: clinical features and differential diagnoses. Epilepsy Behav. 2017;73:51–3. https://doi.org/10.1016/j.yebeh.2017.04.044. Epub 2017 Jun 12.
Musilová K, Kuba R, Brázdil M, Tyrlíková I, Rektor I. Occurrence and lateralizing value of “rare” peri-ictal vegetative symptoms in temporal lobe epilepsy. Epilepsy Behav. 2010;19(3):372–5. https://doi.org/10.1016/j.yebeh.2010.07.010. Epub 2010 Aug 25.
Hoffmann JM, Elger CE, Kleefuss-Lie AA. The localizing value of hypersalivation and postictal coughing in temporal lobe epilepsy. Epilepsy Res. 2009;87(2–3):144–7. https://doi.org/10.1016/j.eplepsyres.2009.08.005. Epub 2009 Sep 11.
Cannistraro RJ, Middlebrooks EH, Brinkmann BH, Feyissa AM. Paroxysmal epileptic laryngospasms: frequent nightly awakenings. Neurol Clin Pract. 2018;8(6):e46–8. https://doi.org/10.1212/CPJ.0000000000000554.
Terzaghi M, Sartori I, Cremascoli R, Rustioni V, Manni R. Choking in the night due to NFLE seizures in a patient with comorbid OSA. J Clin Sleep Med. 2014;10(10):1149–52. https://doi.org/10.5664/jcsm.4122.
Janszky J, Fogarasi A, Toth V, Magalova V, Gyimesi C, Kovacs N, Schulz R, Ebner A. Peri-ictal vegetative symptoms in temporal lobe epilepsy. Epilepsy Behav. 2007;11(1):125–9. https://doi.org/10.1016/j.yebeh.2007.04.015. Epub 2007 Jun 20.
Ye BS, Cho YJ, Jang SH, Lee MK, Lee BI, Heo K. The localizing and lateralizing value of auras in lesional partial epilepsy patients. Yonsei Med J. 2012;53(3):477–85. https://doi.org/10.3349/ymj.2012.53.3.477.
Marks WJ Jr, Laxer KD. Semiology of temporal lobe seizures: value in lateralizing the seizure focus. Epilepsia. 1998;39(7):721–6. https://doi.org/10.1111/j.1528-1157.1998.tb01157.x.
Kramer RE, Lüders H, Goldstick LP, Dinner DS, Morris HH, Lesser RP, Wyllie E. Ictus emeticus: an electroclinical analysis. Neurology. 1988;38(7):1048–52. https://doi.org/10.1212/wnl.38.7.1048.
Devinsky O, Frasca J, Pacia SV, Luciano DJ, Paraiso J, Doyle W. Ictus emeticus: further evidence of nondominant temporal involvement. Neurology. 1995;45(6):1158–60. https://doi.org/10.1212/wnl.45.6.1158.
Schindler K, Wieser HG. Ictal vomiting in a left hemisphere language-dominant patient with left-sided temporal lobe epilepsy. Epilepsy Behav. 2006;8(1):323–7. https://doi.org/10.1016/j.yebeh.2005.10.014. Epub 2005 Dec 6.
Kotagal P, Lüders HO, Williams G, Nichols TR, McPherson J. Psychomotor seizures of temporal lobe onset: analysis of symptom clusters and sequences. Epilepsy Res. 1995;20(1):49–67. https://doi.org/10.1016/0920-1211(94)00055-2.
Chen C, Yen DJ, Yiu CH, Shih YH, Yu HY, Su MS. Ictal vomiting in partial seizures of temporal lobe origin. Eur Neurol. 1999;42(4):235–9. https://doi.org/10.1159/000008114.
Schäuble B, Britton JW, Mullan BP, Watson J, Sharbrough FW, Marsh WR. Ictal vomiting in association with left temporal lobe seizures in a left hemisphere language-dominant patient. Epilepsia. 2002;43(11):1432–5. https://doi.org/10.1046/j.1528-1157.2002.40701.x.
Tarnutzer AA, Mothersill I, Imbach LL. Ictal nausea and vomiting—is it left or right? Seizure. 2018;61:83–8. https://doi.org/10.1016/j.seizure.2018.08.011. Epub 2018 Aug 12.
Isnard J, Guénot M, Sindou M, Mauguière F. Clinical manifestations of insular lobe seizures: a stereo-electroencephalographic study. Epilepsia. 2004;45(9):1079–90. https://doi.org/10.1111/j.0013-9580.2004.68903.x.
Pugnaghi M, Meletti S, Castana L, Francione S, Nobili L, Mai R, Tassi L. Features of somatosensory manifestations induced by intracranial electrical stimulations of the human insula. Clin Neurophysiol. 2011;122(10):2049–58. https://doi.org/10.1016/j.clinph.2011.03.013. Epub 2011 Apr 14.
Carbonari G, Tonti G, Di Pisa V, Franzoni E, Cordelli DM. Pediatric epilepsies misdiagnosed as gastrointestinal disorders. Epilepsy Behav. 2018;83:137–9. https://doi.org/10.1016/j.yebeh.2018.03.034. Epub 2018 Apr 26.
Fogarasi A, Janszky J, Tuxhorn I. Ictal pallor is associated with left temporal seizure onset zone in children. Epilepsy Res. 2005;67(3):117–21. https://doi.org/10.1016/j.eplepsyres.2005.09.001. Epub 2005 Oct 17.
Loddenkemper T, Kellinghaus C, Gandjour J, Nair DR, Najm IM, Bingaman W, Lüders HO. Localising and lateralising value of ictal piloerection. J Neurol Neurosurg Psychiatry. 2004;75(6):879–83. https://doi.org/10.1136/jnnp.2003.023333.
Rocamora R, Becerra JL, Fossas P, Gomez M, Vivanco-Hidalgo RM, Mauri JA, Molins A. Pilomotor seizures: an autonomic semiology of limbic encephalitis? Seizure. 2014;23(8):670–3. https://doi.org/10.1016/j.seizure.2014.04.013. Epub 2014 May 2.
Fisch L, Mégevand P, Badoud S, Seeck M, Burkhard PR. Pilomotor seizure: when paroxysmal gooseflesh heralds brain tumor. Neurology. 2012;78(15):1189. https://doi.org/10.1212/WNL.0b013e31824f80f5. Erratum in: Neurology. 2012 Jul 10;79(2):199. Badoud, A [corrected to Badoud, S].
Franco AC, Noachtar S, Rémi J. Ictal ipsilateral sweating in focal epilepsy. Seizure. 2017;50:4–5. https://doi.org/10.1016/j.seizure.2017.05.009. Epub 2017 May 12.
Leutmezer F, Serles W, Bacher J, Gröppel G, Pataraia E, Aull S, Olbrich A, Czech T, Baumgartner C. Genital automatisms in complex partial seizures. Neurology. 1999;52(6):1188–91. https://doi.org/10.1212/wnl.52.6.1188.
Janszky J, Szücs A, Halász P, Borbély C, Holló A, Barsi P, Mirnics Z. Orgasmic aura originates from the right hemisphere. Neurology. 2002;58(2):302–4. https://doi.org/10.1212/wnl.58.2.302.
York GK, Gabor AJ, Dreyfus PM. Paroxysmal genital pain: an unusual manifestation of epilepsy. Neurology. 1979;29(4):516–9. https://doi.org/10.1212/wnl.29.4.516.
Spencer SS, Spencer DD, Williamson PD, Mattson RH. Sexual automatisms in complex partial seizures. Neurology. 1983;33(5):527–33. https://doi.org/10.1212/wnl.33.5.527.
Dobesberger J, Walser G, Unterberger I, Embacher N, Luef G, Bauer G, Benke T, Bartha L, Ulmer H, Ortler M, Trinka E. Genital automatisms: a video-EEG study in patients with medically refractory seizures. Epilepsia. 2004;45(7):777–80. https://doi.org/10.1111/j.0013-9580.2004.44003.x.
Mascia A, Di Gennaro G, Esposito V, Grammaldo LG, Meldolesi GN, Giampà T, Sebastiano F, Falco C, Onorati P, Manfredi M, Cantore G, Quarato PP. Genital and sexual manifestations in drug-resistant partial epilepsy. Seizure. 2005;14(2):133–8. https://doi.org/10.1016/j.seizure.2004.12.002.
Dede HÖ, Bebek N, Gürses C, Baysal-Kıraç L, Baykan B, Gökyiğit A. Genital automatisms: reappraisal of a remarkable but ignored symptom of focal seizures. Epilepsy Behav. 2018;80:84–9. https://doi.org/10.1016/j.yebeh.2017.12.023. Epub 2018 Feb 2.
Rémillard GM, Andermann F, Testa GF, Gloor P, Aubé M, Martin JB, Feindel W, Guberman A, Simpson C. Sexual ictal manifestations predominate in women with temporal lobe epilepsy: a finding suggesting sexual dimorphism in the human brain. Neurology. 1983;33(3):323–30. https://doi.org/10.1212/wnl.33.3.323.
Gurgenashvili K, Massey SL, Grant M, Piatt J Jr, Legido A, Valencia I. Intracranial localisation of ictal urinary urge epileptogenic zone to the non-dominant temporal lobe. Epileptic Disord. 2011;13(4):430–4. https://doi.org/10.1684/epd.2011.0476.
Loddenkemper T, Foldvary N, Raja S, Neme S, Lüders HO. Ictal urinary urge: further evidence for lateralization to the nondominant hemisphere. Epilepsia. 2003;44(1):124–6. https://doi.org/10.1046/j.1528-1157.2003.26202.x.
Vojvodic N, Ristic AJ, Bascarevic V, Popovic L, Parojcic A, Koprivsek K, Sveljo O, Sokic D. Ictal spitting in left temporal lobe epilepsy and fMRI speech lateralization. Clin Neurol Neurosurg. 2013;115(4):495–7. https://doi.org/10.1016/j.clineuro.2012.06.009. Epub 2012 Jul 3.
Quevedo-Diaz M, Campo AT, Vila-Vidal M, Principe A, Ley M, Rocamora R. Ictal spitting in non-dominant temporal lobe epilepsy: an anatomo-electrophysiological correlation. Epileptic Disord. 2018;20(2):139–45. https://doi.org/10.1684/epd.2018.0963.
Kellinghaus C, Loddenkemper T, Kotagal P. Ictal spitting: clinical and electroencephalographic features. Epilepsia. 2003;44(8):1064–9. https://doi.org/10.1046/j.1528-1157.2003.67302.x.
Fejerman N, Caraballo RH, Dalla BB. Benign childhood epilepsy with centrotemporal spikes. In: Benign focal epilepsies in infancy, childhood and adolescence. Surrey: John Libbey Eurotext Limited; 2007. p. 113.
Fejerman N, Caraballo RH. Early-onset benign childhood occipital epilepsy (Panayiotopoulos type). In: Benign focal epilepsies in infancy, childhood and adolescence. Surrey: John Libbey Eurotext Limited; 2007. p. 220.
Shah J, Zhai H, Fuerst D, Watson C. Hypersalivation in temporal lobe epilepsy. Epilepsia. 2006;47(3):644–51. https://doi.org/10.1111/j.1528-1167.2006.00480.x.
Denton D, Shade R, Zamarippa F, Egan G, Blair-West J, McKinley M, Fox P. Correlation of regional cerebral blood flow and change of plasma sodium concentration during genesis and satiation of thirst. Proc Natl Acad Sci U S A. 1999;96(5):2532–7. https://doi.org/10.1073/pnas.96.5.2532.
Trinka E, Walser G, Unterberger I, Luef G, Benke T, Bartha L, Ortler M, Bauer G. Peri-ictal water drinking lateralizes seizure onset to the nondominant temporal lobe. Neurology. 2003;60(5):873–6. https://doi.org/10.1212/01.wnl.0000049459.83589.6c.
Hauser WA, Annegers JF, Rocca WA. Descriptive epidemiology of epilepsy: contributions of population-based studies from Rochester, Minnesota. Mayo Clin Proc. 1996;71(6):576–86. https://doi.org/10.4065/71.6.576.
Cendes F. Progressive hippocampal and extrahippocampal atrophy in drug resistant epilepsy. Curr Opin Neurol. 2005;18(2):173–7. https://doi.org/10.1097/01.wco.0000162860.49842.90.
Blümcke I, Thom M, Wiestler OD. Ammon’s horn sclerosis: a maldevelopmental disorder associated with temporal lobe epilepsy. Brain Pathol. 2002;12(2):199–211. https://doi.org/10.1111/j.1750-3639.2002.tb00436.x.
Blair RD. Temporal lobe epilepsy semiology. Epilepsy Res Treat. 2012;2012:751510. https://doi.org/10.1155/2012/751510. Epub 2012 Mar 7.
Tatum WO 4th. Mesial temporal lobe epilepsy. J Clin Neurophysiol. 2012;29(5):356–65. https://doi.org/10.1097/WNP.0b013e31826b3ab7.
Bercovici E, Kumar BS, Mirsattari SM. Neocortical temporal lobe epilepsy. Epilepsy Res Treat. 2012;2012:103160. https://doi.org/10.1155/2012/103160. Epub 2012 Jul 16.
Van Buren JM. Sensory, motor and autonomic effects of mesial temporal stimulation in man. J Neurosurg. 1961;18:273–88. https://doi.org/10.3171/jns.1961.18.3.0273.
Lathers CM, Schraeder PL. Review of autonomic dysfunction, cardiac arrhythmias, and epileptogenic activity. J Clin Pharmacol. 1987;27(5):346–56. https://doi.org/10.1002/j.1552-4604.1987.tb03030.x.
Loddenkemper T, Kotagal P. Lateralizing signs during seizures in focal epilepsy. Epilepsy Behav. 2005;7(1):1–17. https://doi.org/10.1016/j.yebeh.2005.04.004.
Foldvary-Schaefer N, Unnwongse K. Localizing and lateralizing features of auras and seizures. Epilepsy Behav. 2011;20(2):160–6. https://doi.org/10.1016/j.yebeh.2010.08.034.
Athira SB, Pal P, Nair PP, Nanda N, Aghoram R. Cardiovascular autonomic function and baroreflex sensitivity in drug-resistant temporal lobe epilepsy. Epilepsy Behav. 2023;138:109013. https://doi.org/10.1016/j.yebeh.2022.109013. Epub 2022 Dec 14.
Noachtar S, Peters AS. Semiology of epileptic seizures: a critical review. Epilepsy Behav. 2009;15(1):2–9. https://doi.org/10.1016/j.yebeh.2009.02.029. Epub 2009 Feb 21.
Jan MM, Girvin JP. Seizure semiology: value in identifying seizure origin. Can J Neurol Sci. 2008;35(1):22–30. https://doi.org/10.1017/s0317167100007526.
Chen C, Shih YH, Yen DJ, Lirng JF, Guo YC, Yu HY, Yiu CH. Olfactory auras in patients with temporal lobe epilepsy. Epilepsia. 2003;44(2):257–60. https://doi.org/10.1046/j.1528-1157.2003.25902.x.
Bien CG, Benninger FO, Urbach H, Schramm J, Kurthen M, Elger CE. Localizing value of epileptic visual auras. Brain. 2000;123(Pt 2):244–53. https://doi.org/10.1093/brain/123.2.244.
Biraben A, Taussig D, Thomas P, Even C, Vignal JP, Scarabin JM, Chauvel P. Fear as the main feature of epileptic seizures. J Neurol Neurosurg Psychiatry. 2001;70(2):186–91. https://doi.org/10.1136/jnnp.70.2.186.
Oehl B, Schulze-Bonhage A, Lanz M, Brandt A, Altenmüller DM. Occipital lobe epilepsy with fear as leading ictal symptom. Epilepsy Behav. 2012;23(3):379–83. https://doi.org/10.1016/j.yebeh.2011.12.014. Epub 2012 Feb 27.
Yaşgüçlükal MA, Makhalova J, Carron R, Bartolomei F. Ictal fear during parietal seizures. Epileptic Disord. 2021;23(5):793–8. https://doi.org/10.1684/epd.2021.1321.
Cao Q, Cui T, Wang Q, Li ZM, Fan SH, Xiao ZM, Pan SQ, Zhou Q, Lu ZN, Shao XQ. The localization and lateralization of fear aura and its surgical prognostic value in patients with focal epilepsy. Ann Clin Transl Neurol. 2022;9(8):1116–24. https://doi.org/10.1002/acn3.51607. Epub 2022 Jun 14.
Parikh S, Gupta A. Autonomic dysfunction in epilepsy and mitochondrial diseases. Semin Pediatr Neurol. 2013;20(1):31–4. https://doi.org/10.1016/j.spen.2013.01.003.
You SM, Jo HJ, Cho BH, Song JY, Kim DY, Hwang YH, Shon YM, Seo DW, Kim IY. Comparing ictal cardiac autonomic changes in patients with frontal lobe epilepsy and temporal lobe epilepsy by ultra-short-term heart rate variability analysis. Medicina (Kaunas). 2021;57(7):666. https://doi.org/10.3390/medicina57070666.
Panayiotopoulos CP. Autonomic seizures and autonomic status epilepticus peculiar to childhood: diagnosis and management. Epilepsy Behav. 2004;5(3):286–95. https://doi.org/10.1016/j.yebeh.2004.01.013.
Okanishi T, Maegaki Y, Ohno K, Togari H. Underlying neurologic disorders and recurrence rates of status epilepticus in childhood. Brain Dev. 2008;30(10):624–8. https://doi.org/10.1016/j.braindev.2008.02.003. Epub 2008 Mar 24.
Specchio N, Trivisano M, Claps D, Battaglia D, Fusco L, Vigevano F. Documentation of autonomic seizures and autonomic status epilepticus with ictal EEG in Panayiotopoulos syndrome. Epilepsy Behav. 2010;19(3):383–93. https://doi.org/10.1016/j.yebeh.2010.06.046. Epub 2010 Aug 24.
Panayiotopoulos CP. Panayiotopoulos syndrome: a common and benign childhood epileptic syndrome. London: John Libbey; 2002.
Panayiotopoulos CP. Early-onset benign childhood occipital seizure susceptibility syndrome: a syndrome to recognize. Epilepsia. 1999;40(5):621–30. https://doi.org/10.1111/j.1528-1157.1999.tb05565.x.
Lada C, Skiadas K, Theodorou V, Loli N, Covanis A. A study of 43 patients with panayiotopoulos syndrome, a common and benign childhood seizure susceptibility. Epilepsia. 2003;44(1):81–8. https://doi.org/10.1046/j.1528-1157.2003.32602.x.
Durá-Travé T, Yoldi-Petri ME, Gallinas-Victoriano F. Incidence of epilepsies and epileptic syndromes among children in Navarre, Spain: 2002 through 2005. J Child Neurol. 2008;23(8):878–82. https://doi.org/10.1177/0883073808314898.
Panayiotopoulos CP. Vomiting as an ictal manifestation of epileptic seizures and syndromes. J Neurol Neurosurg Psychiatry. 1988;51(11):1448–51. https://doi.org/10.1136/jnnp.51.11.1448.
Ferrie C, Caraballo R, Covanis A, Demirbilek V, Dervent A, Kivity S, Koutroumanidis M, Martinovic Z, Oguni H, Verrotti A, Vigevano F, Watanabe K, Yalcin D, Yoshinaga H. Panayiotopoulos syndrome: a consensus view. Dev Med Child Neurol. 2006;48(3):236–40. https://doi.org/10.1017/S0012162206000508.
Panayiotopoulos CP, Michael M, Sanders S, Valeta T, Koutroumanidis M. Benign childhood focal epilepsies: assessment of established and newly recognized syndromes. Brain. 2008;131(Pt 9):2264–86. https://doi.org/10.1093/brain/awn162. Epub 2008 Aug 21.
Covanis A, Lada C, Skiadas K. Children with Rolandic spikes and ictal vomiting: Rolandic epilepsy or Panayiotopoulos syndrome? Epileptic Disord. 2003;5(3):139–43.
Parisi P, Villa MP, Pelliccia A, Rollo VC, Chiarelli F, Verrotti A. Panayiotopoulos syndrome: diagnosis and management. Neurol Sci. 2007;28(2):72–9. https://doi.org/10.1007/s10072-007-0790-4.
Caraballo R, Cersósimo R, Fejerman N. Panayiotopoulos syndrome: a prospective study of 192 patients. Epilepsia. 2007;48(6):1054–61. https://doi.org/10.1111/j.1528-1167.2007.01085.x. Epub 2007 Apr 18.
Ferrie CD, Grünewald RA. Panayiotopoulos syndrome: a common and benign childhood epilepsy. Lancet. 2001;357(9259):821–3. https://doi.org/10.1016/S0140-6736(00)04192-1.
Koutroumanidis M. Panayiotopoulos syndrome. BMJ. 2002;324(7348):1228–9. https://doi.org/10.1136/bmj.324.7348.1228.
Specchio N, Trivisano M, Di Ciommo V, Cappelletti S, Masciarelli G, Volkov J, Fusco L, Vigevano F. Panayiotopoulos syndrome: a clinical, EEG, and neuropsychological study of 93 consecutive patients. Epilepsia. 2010;51(10):2098–107. https://doi.org/10.1111/j.1528-1167.2010.02639.x. Epub 2010 Sep 21.
Sanders S, Rowlinson S, Manidakis I, Ferrie CD, Koutroumanidis M. The contribution of the EEG technologists in the diagnosis of Panayiotopoulos syndrome (susceptibility to early onset benign childhood autonomic seizures). Seizure. 2004;13(8):565–73. https://doi.org/10.1016/j.seizure.2004.01.006.
Taylor I, Berkovic SF, Kivity S, Scheffer IE. Benign occipital epilepsies of childhood: clinical features and genetics. Brain. 2008;131(Pt 9):2287–94. https://doi.org/10.1093/brain/awn138. Epub 2008 Jul 9.
Michael M, Tsatsou K, Ferrie CD. Panayiotopoulos syndrome: an important childhood autonomic epilepsy to be differentiated from occipital epilepsy and acute non-epileptic disorders. Brain Dev. 2010;32(1):4–9. https://doi.org/10.1016/j.braindev.2009.03.002. Epub 2009 Apr 21.
Berg AT, Coffman K, Gaebler-Spira D. Dysautonomia and functional impairment in rare developmental and epileptic encephalopathies: the other nervous system. Dev Med Child Neurol. 2021;63(12):1433–40. https://doi.org/10.1111/dmcn.14990. Epub 2021 Jul 11.
Steffenburg U, Hagberg G, Hagberg B. Epilepsy in a representative series of Rett syndrome. Acta Paediatr. 2001;90:34–9.
Neul JL, Kaufmann WE, Glaze DG, Christodoulou J, Clarke AJ, Bahi-Buisson N, Leonard H, Bailey ME, Schanen NC, Zappella M, Renieri A, Huppke P, Percy AK, RettSearch Consortium. Rett syndrome: revised diagnostic criteria and nomenclature. Ann Neurol. 2010;68(6):944–50. https://doi.org/10.1002/ana.22124.
Weese-Mayer DE, Lieske SP, Boothby CM, Kenny AS, Bennett HL, Ramirez J-M. Autonomic dysregulation in young girls with Rett syndrome during nighttime in-home recordings. Pediatr Pulmonol. 2008;43:1045–60.
Nissenkorn A, Levy-Drummer RS, Bondi O, Renieri A, Villard L, Mari F, Mencarelli MA, Lo Rizzo C, Meloni I, Pineda M, Armstrong J, Clarke A, Bahi-Buisson N, Mejaski BV, Djuric M, Craiu D, Djukic A, Pini G, Bisgaard AM, Melegh B, Vignoli A, Russo S, Anghelescu C, Veneselli E, Hayek J, Ben-Zeev B. Epilepsy in Rett syndrome—lessons from the Rett networked database. Epilepsia. 2015;56(4):569–76. https://doi.org/10.1111/epi.12941. Epub 2015 Mar 19.
Glaze DG. Neurophysiology of Rett syndrome. J Child Neurol. 2005;20:740–6.
Wolff M, Casse-Perrot C, Dravet C. Severe myoclonic epilepsy of infants (Dravet syndrome): natural history and neuropsychological findings. Epilepsia. 2006;47(Suppl. 2):45–8.
Skluzacek JV, Watts KP, Parsy O, Wical B, Camfield P. Dravet syndrome and parent associations: the IDEA League experience with comorbid conditions, mortality, management, adaptation, and grief. Epilepsia. 2011;52:95–101.
Delogu AB, Spinelli A, Battaglia D, Dravet C, De Nisco A, Saracino A, Romagnoli C, Lanza GA, Crea F. Electrical and autonomic cardiac function in patients with Dravet syndrome. Epilepsia. 2011;52(Suppl 2):55–8. https://doi.org/10.1111/j.1528-1167.2011.03003.x.
Trivisano M, Pavia GC, Ferretti A, Fusco L, Vigevano F, Specchio N. Generalized tonic seizures with autonomic signs are the hallmark of SCN8A developmental and epileptic encephalopathy. Epilepsy Behav. 2019;96:219–23. https://doi.org/10.1016/j.yebeh.2019.03.043. Epub 2019 Jun 4.
Pons L, Lesca G, Sanlaville D, Chatron N, Labalme A, Manel V, Arzimanoglou A, de Bellescize J, Lion-François L. Neonatal tremor episodes and hyperekplexia-like presentation at onset in a child with SCN8A developmental and epileptic encephalopathy. Epileptic Disord. 2018;20:289–94.
Negishi Y, Aoki Y, Itomi K, Yasuda K, Taniguchi H, Ishida A, Arakawa T, Miyamoto S, Nakashima M, Saitsu H, Saitoh S. SCN8A-related developmental and epileptic encephalopathy with ictal asystole requiring cardiac pacemaker implantation. Brain Dev. 2021;43(7):804–8. https://doi.org/10.1016/j.braindev.2021.03.004. Epub 2021 Apr 4.
Byard RW. Forensic issues and possible mechanisms of sudden death in Rett syndrome. J Clin Forensic Med. 2006;13(2):96–9. https://doi.org/10.1016/j.jcfm.2005.08.013. Epub 2005 Nov 2.
Goswami I, Maguire B, Chau V, Tam EW, Pinchefsky E, Whitney R, Wilson D, Miller SP, Cortez MA. Early transient dysautonomia predicts the risk of infantile epileptic spasm syndrome onset: a prospective cohort study. Front Neurol. 2022;13:1090155. https://doi.org/10.3389/fneur.2022.1090155.
Ficker DM, So EL, Shen WK, Annegers JF, O’Brien PC, Cascino GD, Belau PG. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology. 1998;51(5):1270–4. https://doi.org/10.1212/wnl.51.5.1270.
Mazzola L, Rheims S. Ictal and interictal cardiac manifestations in epilepsy. A review of their relation with an altered central control of autonomic functions and with the risk of SUDEP. Front Neurol. 2021;12:642645.
Nashef L, So EL, Ryvlin P, Tomson T. Unifying the definitions of sudden unexpected death in epilepsy. Epilepsia. 2012;53(2):227–33. https://doi.org/10.1111/j.1528-1167.2011.03358.x.
Harden C, Tomson T, Gloss D, Buchhalter J, Cross JH, Donner E, French JA, Gil-Nagel A, Hesdorffer DC, Smithson WH, Spitz MC, Walczak TS, Sander JW, Ryvlin P. Practice guideline summary: sudden unexpected death in epilepsy incidence rates and risk factors: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2017;88(17):1674–80. https://doi.org/10.1212/WNL.0000000000003685. Erratum in: Neurology. 2019 Nov 26;93(22):982. Erratum in: Neurology. 2020;94(9):414.
Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol. 2008;7:1021–31.
Sveinsson O, Andersson T, Carlsson S, Tomson T. The incidence of SUDEP: a nationwide population-based cohort study. Neurology. 2017;89:170–7.
Keller AE, Whitney R, Li SA, Pollanen MS, Donner EJ. Incidence of sudden unexpected death in epilepsy in children is similar to adults. Neurology. 2018;91:e107–11.
Devinsky O, Bundock E, Hesdorffer D, Donner E, Moseley B, Cihan E, Hussain F, Friedman D. Resolving ambiguities in SUDEP classification. Epilepsia. 2018;59(6):1220–33. https://doi.org/10.1111/epi.14195. Epub 2018 May 23.
Ryvlin P, Nashef L, Lhatoo SD, Bateman LM, Bird J, Bleasel A, Boon P, Crespel A, Dworetzky BA, Høgenhaven H, Lerche H, Maillard L, Malter MP, Marchal C, Murthy JMK, Nitsche M, Pataraia E, Rabben T, Rheims S, Sadzot B, Schulze-Bonhage A, Seyal M, So EL, Spitz M, Szucs A, Tan M, Tao JX, Tomson T. Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study. Lancet Neurol. 2013;12(10):966–77. https://doi.org/10.1016/S1474-4422(13)70214-X.
Langan Y, Nashef L, Sander JW. Sudden unexpected death in epilepsy: a series of witnessed deaths. J Neurol Neurosurg Psychiatry. 2000;68(2):211–3.
Mueller SG, Nei M, Bateman LM, Knowlton R, Laxer KD, Friedman D, Devinsky O, Goldman AM. Brainstem network disruption: a pathway to sudden unexplained death in epilepsy? Hum Brain Mapp. 2018;39(12):4820–30. https://doi.org/10.1002/hbm.24325.
Walczak TS, Leppik IE, D’Amelio M, Rarick J, So E, Ahman P, Ruggles K, Cascino GD, Annegers JF, Hauser WA. Incidence and risk factors in sudden unexpected death in epilepsy: a prospective cohort study. Neurology. 2001;56(4):519–25.
Sperling MR, Harris A, Nei M, Liporace JD, O’Connor MJ. Mortality after epilepsy surgery. Epilepsia. 2005;46(s11):49–53. https://doi.org/10.1111/j.1528-1167.2005.00410.x.
Verducci C, Hussain F, Donner E, Moseley BD, Buchhalter J, Hesdorffer D, Friedman D, Devinsky O. SUDEP in the North American SUDEP Registry: the full spectrum of epilepsies. Neurology. 2019;93(3):e227–36. https://doi.org/10.1212/WNL.0000000000007778. Epub 2019 Jun 19.
Hebel JM, Surges R, Stodieck SRG, Lanz M. SUDEP following the second seizure in new-onset epilepsy due to limbic encephalitis. Seizure. 2018;62:124–6.
Lhatoo SD, Nei M, Raghavan M, Sperling M, Zonjy B, Lacuey N, Devinsky O. Nonseizure SUDEP: sudden unexpected death in epilepsy without preceding epileptic seizures. Epilepsia. 2016;57(7):1161–8. https://doi.org/10.1111/epi.13419. Epub 2016 May 25.
Allen LA, Harper RM, Lhatoo S, Lemieux L, Diehl B. Neuroimaging of sudden unexpected death in epilepsy (SUDEP): insights from structural and resting-state functional MRI studies. Front Neurol. 2019;10:185. https://doi.org/10.3389/fneur.2019.00185.
Poh MZ, Loddenkemper T, Reinsberger C, Swenson NC, Goyal S, Madsen JR, Picard RW. Autonomic changes with seizures correlate with postictal EEG suppression. Neurology. 2012;8(23):1868–76. https://doi.org/10.1212/WNL.0b013e318258f7f1.
Myers KA, Sivathamboo S, Perucca P. Heart rate variability measurement in epilepsy: How can we move from research to clinical practice? Epilepsia. 2018;59(12):2169–78. https://doi.org/10.1111/epi.14587.
Ansakorpi H, Korpelainen JT, Suominen K, Tolonen U, Myllylä VV, Isojärvi JIT. Interictal cardiovascular autonomic responses in patients with temporal lobe epilepsy. Epilepsia. 2000;41(1):42–7. https://doi.org/10.1111/j.1528-1157.2000.tb01503.x.
Ferri R, Curzi-Dascalova L, Arzimanoglou A, Bourgeois M, Beaud C, Nunes M, Elia M, Musumeci SA, Tripodi M. Heart rate variability during sleep in children with partial epilepsy. J Sleep Res. 2002;11(2):153–60. https://doi.org/10.1046/j.1365-2869.2002.00283.x.
Tomson T, Ericson M, Ihrman C, Lindblad LE. Heart rate variability in patients with epilepsy. Presented in part at the 2nd European Congress of Epileptology, The Hague, September, 1996. Epilepsy Res. 1998;30(1):77–83. https://doi.org/10.1016/S0920-1211(97)00094-6.
Devinsky O, Perrine K, Theodore WH. Interictal autonomic nervous system function in patients with epilepsy. Epilepsia. 1994;35(1):199–204. https://doi.org/10.1111/j.1528-1157.1994.tb02933.x.
Kolsal E, Serdaroğlu A, Çilsal E, Kula S, Soysal AŞ, Kurt ANÇ, Arhan E. Can heart rate variability in children with epilepsy be used to predict seizures? Seizure. 2014;23(5):357–62. https://doi.org/10.1016/j.seizure.2014.01.025.
Ergul Y, Ekici B, Tatli B, Nisli K, Ozmen M. QT and P wave dispersion and heart rate variability in patients with Dravet syndrome. Acta Neurol Belg. 2013;113(2):161–6. https://doi.org/10.1007/s13760-012-0140-z.
Page T, Rugg-Gunn FJ. Bitemporal seizure spread and its effect on autonomic dysfunction. Epilepsy Behav. 2018;84:166–72. https://doi.org/10.1016/j.yebeh.2018.03.016.
Jeppesen J, Fuglsang-Frederiksen A, Brugada R, Pedersen B, Rubboli G, Johansen P, Beniczky S. Heart rate variability analysis indicates preictal parasympathetic overdrive preceding seizure-induced cardiac dysrhythmias leading to sudden unexpected death in a patient with epilepsy. Epilepsia. 2014;55(7):67. https://doi.org/10.1111/epi.12614.
Surges R, Henneberger C, Adjei P, Scott CA, Sander JW, Walker MC. Do alterations in inter-ictal heart rate variability predict sudden unexpected death in epilepsy? Epilepsy Res. 2009;87(2–3):277–80. https://doi.org/10.1016/j.eplepsyres.2009.08.008.
Bank AM, Dworetzky BA, Lee JW. Sudden unexpected death in epilepsy in a patient with a cardiac pacemaker. Seizure. 2018;61:38–40.
Surges R, Adjei P, Kallis C, Erhuero J, Scott CA, Bell GS, Sander JW, Walker MC. Pathologic cardiac repolarization in pharmacoresistant epilepsy and its potential role in sudden unexpected death in epilepsy: a case-control study. Epilepsia. 2010;51(2):233–42. https://doi.org/10.1111/j.1528-1167.2009.02330.x. Epub 2009 Oct 8.
Schuele SU, Bermeo AC, Locatelli E, Burgess RC, Lüders HO. Ictal asystole: a benign condition? Epilepsia. 2008;49:168–71.
Chaila E, Bhangu J, Tirupathi S, Delanty N. Ictal bradycardia and asystole associated with intractable epilepsy: a case series. Br J Cardiol. 2010;17:245–8.
Sveinsson O, Andersson T, Carlsson S, Tomson T. Circumstances of SUDEP: a nationwide population-based case series. Epilepsia. 2018;59:1074–82.
Stecker EC, Reinier K, Uy-Evanado A, Teodorescu C, Chugh H, Gunson K, Jui J, Chugh SS. Relationship between seizure episode and sudden cardiac arrest in patients with epilepsy: a community-based study. Circ Arrhythm Electrophysiol. 2013;6(5):912–6. https://doi.org/10.1161/CIRCEP.113.000544. Epub 2013 Aug 21.
Nei M, Ho RT, Abou-Khalil BW, Drislane FW, Liporace J, Romeo A, Sperling MR. EEG and ECG in sudden unexplained death in epilepsy. Epilepsia. 2004;45(4):338–45. https://doi.org/10.1111/j.0013-9580.2004.05503.
Bruno E, Biondi A, Richardson MP. Pre-ictal heart rate changes: a systematic review and meta-analysis. Seizure. 2018;55:48–56.
Beniczky S, Arbune AA, Jeppesen J, Ryvlin P. Biomarkers of seizure severity derived from wearable devices. Epilepsia. 2020;61(Suppl. 1):S61–6.
Sivathamboo S, Constantino TN, Chen Z, Sparks PB, Goldin J, Velakoulis D, Jones NC, Kwan P, Macefield VG, O’Brien TJ, Perucca P. Cardiorespiratory and autonomic function in epileptic seizures: a video-EEG monitoring study. Epilepsy Behav. 2020;111:107271. https://doi.org/10.1016/j.yebeh.2020.107271. Epub 2020 Jul 10.
Chouchou F, Bouet R, Pichot V, Catenoix H, Mauguière F, Jung J. The neural bases of ictal tachycardia in temporal lobe seizures. Clin Neurophysiol. 2017;128(9):1810–9. https://doi.org/10.1016/j.clinph.2017.06.033. Epub 2017 Jun 27.
Surges R, Jordan A, Elger CE. Ictal modulation of cardiac repolarization, but not of heart rate, is lateralized in mesial temporal lobe epilepsy. PLoS One. 2013;8:e64765.
van Westrhenen A, De Cooman T, Lazeron RHC, Van Huffel S, Thijs RD. Ictal autonomic changes as a tool for seizure detection: a systematic review. Clin Auton Res. 2019;29:161–81.
Stefanidou M, Carlson C, Friedman D. The relationship between seizure onset zone and ictal tachycardia: an intracranial EEG study. Clin Neurophysiol. 2015;126:2255–60.
Opherk C, Coromilas J, Hirsch LJ. Heart rate and EKG changes in 102 seizures: analysis of influencing factors. Epilepsy Res. 2002;52(2):117–27.
Pang TD, Nearing BD, Krishnamurthy KB, Olin B, Schachter SC, Verrier RL. Cardiac electrical instability in newly diagnosed/chronic epilepsy tracked by Holter and ECG patch. Neurology. 2019;93(10):450–8.
Surges R, Taggart P, Sander JW, Walker MC. Too long or too short? New insights into abnormal cardiac repolarization in people with chronic epilepsy and its potential role in sudden unexpected death. Epilepsia. 2010;51:738–44.
Strzelczyk A, Adjei P, Scott CA, Bauer S, Rosenow F, Walker MC, Surges R. Postictal increase in T-wave alternans after generalized tonic-clonic seizures. Epilepsia. 2011;52(11):2112–7. https://doi.org/10.1111/j.1528-1167.2011.03266.x. Epub 2011 Sep 20.
Bardai A, Lamberts RJ, Blom MT, Spanjaart AM, Berdowski J, van der Staal SR, Brouwer HJ, Koster RW, Sander JW, Thijs RD, Tan HL. Epilepsy is a risk factor for sudden cardiac arrest in the general population. PLoS One. 2012;7(8):e42749. https://doi.org/10.1371/journal.pone.0042749.
Devinsky O, Friedman D, Cheng JY, Moffatt E, Kim A, Tseng ZH. Underestimation of sudden deaths among patients with seizures and epilepsy. Neurology. 2017;89(9):886–92. https://doi.org/10.1212/WNL.0000000000004292.
Surges R, Thijs RD, Tan HL, Sander JW. Sudden unexpected death in epilepsy: risk factors and potential pathomechanisms. Nat Rev Neurol. 2009;5:492–504.
Rugg-Gunn FJ, Simister RJ, Squirrell M, Holdright DR, Duncan JS. Cardiac arrhythmias in focal epilepsy: a prospective long-term study. Lancet. 2004;364(9452):2212–9. https://doi.org/10.1016/S0140-6736(04)17594-6.
Nei M, Mintzer S, Skidmore C, Sperling MR, Ho RT. Heart rate and blood pressure in sudden unexpected death in epilepsy (SUDEP). Epilepsy Res. 2016;122:44–6. https://doi.org/10.1016/j.eplepsyres.2016.02.008.
Hampel KG, Jahanbekam A, Elger CE, Surges R. Seizure-related modulation of systemic arterial blood pressure in focal epilepsy. Epilepsia. 2016;57:1709–18.
Esmaeili B, Kaffashi F, Theeranaew W, Dabir A, Lhatoo SD, Loparo KA. Post-ictal modulation of baroreflex sensitivity in patients with intractable epilepsy. Front Neurol. 2018;9:793.
Nass RD, Hampel KG, Elger CE, Surges R. Blood pressure in seizures and epilepsy. Front Neurol. 2019;10:501. https://doi.org/10.3389/fneur.2019.00501.
Liebenthal JA, Wu S, Rose S, Ebersole JS, Tao JX. Association of prone position with sudden unexpected death in epilepsy. Neurology. 2015;84(7):703–9. https://doi.org/10.1212/WNL.0000000000001260.
Nashef L, Fish DR, Sander JW, Shorvon SD. Incidence of sudden unexpected death in an adult outpatient cohort with epilepsy at a tertiary referral centre. J Neurol Neurosurg Psychiatry. 1995;58(4):462–4.
Lamberts RJ, Thijs RD, Laffan A, Langan Y, Sander JW. Sudden expected death in epilepsy: people with nocturnal seizures may be at highest risk. Epilepsia. 2012;53:253–7.
Dlouhy BJ, Gehlbach BK, Kreple CJ, Kawasaki H, Oya H, Buzza C, Granner MA, Welsh MJ, Howard MA, Wemmie JA, Richerson GB. Breathing inhibited when seizures spread to the amygdala and upon amygdala stimulation. J Neurosci. 2015;35(28):10281–9. https://doi.org/10.1523/jneurosci.0888-15.2015.
Rhone AE, Kovach CK, Harmata GI, Sullivan AW, Tranel D, Ciliberto MA, Howard MA, Richerson GB, Steinschneider M, Wemmie JA. A human amygdala site that inhibits respiration and elicits apnea in pediatric epilepsy. JCI Insight. 2020;5(6):e134852. https://doi.org/10.1172/jci.insight.134852.
Park KJ, Sharma G, Kennedy JD, Seyal M. Potentially high-risk cardiac arrhythmias with focal to bilateral tonic-clonic seizures and generalized tonic-clonic seizures are associated with the duration of periictal hypoxemia. Epilepsia. 2017;58(12):2164–71. https://doi.org/10.1111/epi.13934.
Venit EL, Shepard BD, Seyfried TN. Oxygenation prevents sudden death in seizure-prone mice. Epilepsia. 2004;45(8):993–6. https://doi.org/10.1111/j.0013-9580.2004.02304.x.
Uteshev VV, Tupal S, Mhaskar Y, Faingold CL. Abnormal serotonin receptor expression in DBA/2 mice associated with susceptibility to sudden death due to respiratory arrest. Epilepsy Res. 2010;88(2–3):183–8. https://doi.org/10.1016/j.eplepsyres.2009.11.004.
Tupal S, Faingold CL. Evidence supporting a role of serotonin in modulation of sudden death induced by seizures in DBA/2 mice. Epilepsia. 2006;47(1):21–6. https://doi.org/10.1111/j.1528-1167.2006.00365.x.
Faingold CL, Randall M, Kommajosyula SP. Susceptibility to seizure-induced sudden death in DBA/2 mice is altered by adenosine. Epilepsy Res. 2016;124:49–54. https://doi.org/10.1016/j.eplepsyres.2016.05.007.
Richerson GB, Buchanan GF. The serotonin axis: shared mechanisms in seizures, depression, and SUDEP. Epilepsia. 2011;52(Suppl 1):28–38. https://doi.org/10.1111/j.1528-1167.2010.02908.x.
Bruno E, Richardson MP. Postictal generalized EEG suppression and postictal immobility: what do we know? Epileptic Disord. 2020;22:245–51.
Moseley BD, So E, Wirrell EC, Nelson C, Lee RW, Mandrekar J, Britton JW. Characteristics of postictal generalized EEG suppression in children. Epilepsy Res. 2013;106(1–2):123–7. https://doi.org/10.1016/j.eplepsyres.2013.05.007.
Tang Y, Xia W, Yan B, Zhao L, An D, Zhou D. Periictal electroclinical characteristics of postictal generalized electroencephalographic suppression after generalized convulsive seizures. Medicine. 2020;99(20):e19940. https://doi.org/10.1097/MD.0000000000019940.
Kuo J, Zhao W, Li C-S, Kennedy JD, Seyal M. Postictal immobility and generalized EEG suppression are associated with the severity of respiratory dysfunction. Epilepsia. 2016;57(3):412–7. https://doi.org/10.1111/epi.13312.
Critchley HD. Electrodermal responses: what happens in the brain. Neuroscientist. 2002;8(2):132–42. https://doi.org/10.1177/107385840200800209.
Sarkis RA, Thome-Souza S, Poh MZ, Llewellyn N, Klehm J, Madsen JR, Picard R, Pennell PB, Dworetzky BA, Loddenkemper T, Reinsberger C. Autonomic changes following generalized tonic clonic seizures: an analysis of adult and pediatric patients with epilepsy. Epilepsy Res. 2015;115:113–8. https://doi.org/10.1016/j.eplepsyres.2015.06.005.
Mueller SG, Bateman LM, Laxer KD. Evidence for brainstem network disruption in temporal lobe epilepsy and sudden unexplained death in epilepsy. Neuroimage Clin. 2014;5:208–16. https://doi.org/10.1016/j.nicl.2014.06.010.
Allen LA, Vos SB, Kumar R, Ogren JA, Harper RK, Winston GP, Balestrini S, Wandschneider B, Scott A, Ourselin S, Duncan JS, Lhatoo SD, Harper RM, Diehl B. Cerebellar, limbic, and midbrain volume alterations in sudden unexpected death in epilepsy. Epilepsia. 2019;60(4):718–29. https://doi.org/10.1111/epi.14689. Epub 2019 Mar 14.
Wandschneider B, Koepp M, Scott C, Micallef C, Balestrini S, Sisodiya SM, Thom M, Harper RM, Sander JW, Vos SB, Duncan JS, Lhatoo S, Diehl B. Structural imaging biomarkers of sudden unexpected death in epilepsy. Brain. 2015;138(Pt 10):2907–19. https://doi.org/10.1093/brain/awv233. Epub 2015 Aug 10.
Gigout S, Wierschke C, Dehnicke R. Deisz, different pharmacology of N-desmethylclozapine at human and rat M2 and M4 mAChRs in neocortex, Naunyn Schmiedeberg’s. Arch Pharmacol. 2015;388:487–96.
Broncel A, Bocian R, Kłos-Wojtczak P, Konopacki J. Medial septal cholinergic mediation of hippocampal theta rhythm induced by vagal nerve stimulation. PLoS One. 2018;13:e0206532.
Akyuz E, Polat AK, Eroglu E, Kullu I, Angelopoulou E, Paudel YN. Revisiting the role of neurotransmitters in epilepsy: an updated review. Life Sci. 2021;265:118826.
Tupal S, Faingold CL. Fenfluramine, a serotonin-releasing drug, prevents seizure-induced respiratory arrest and is anticonvulsant in the DBA/1 mouse model of SUDEP. Epilepsia. 2019;60:485–94.
Patodia S, Somani A, O’Hare M, Venkateswaran R, Liu J, Michalak Z, Ellis M, Scheffer IE, Diehl B, Sisodiya SM, Thom M. The ventrolateral medulla and medullary raphe in sudden unexpected death in epilepsy. Brain. 2018;141(6):1719–33. https://doi.org/10.1093/brain/awy078.
Goldman AM, Glasscock E, Yoo J, Chen TT, Klassen TL, Noebels JL. Arrhythmia in heart and brain: KCNQ1 mutations link epilepsy and sudden unexplained death. Sci Transl Med. 2009;1(2):2ra6. https://doi.org/10.1126/scitranslmed.3000289.
Li Michael CH, O’Brien Terence J, Todaro M, Powell KL. Acquired cardiac channelopathies in epilepsy: evidence, mechanisms, and clinical significance. Epilepsia. 2019;60:1753–67. https://doi.org/10.1111/epi.16301.
Bagnall RD, Crompton DE, Petrovski S, Lam L, Cutmore C, Garry SI, Sadleir LG, Dibbens LM, Cairns A, Kivity S, Afawi Z, Regan BM, Duflou J, Berkovic SF, Scheffer IE, Semsarian C. Exome-based analysis of cardiac arrhythmia, respiratory control, and epilepsy genes in sudden unexpected death in epilepsy. Ann Neurol. 2016;79(4):522–34. https://doi.org/10.1002/ana.24596. Epub 2016 Feb 2.
Auerbach DS, Jones J, Clawson BC, Offord J, Lenk GM, Ogiwara I, Yamakawa K, Meisler MH, Parent JM, Isom LL. Altered cardiac electrophysiology and SUDEP in a model of Dravet syndrome. PLoS One. 2013;8(10):e77843. https://doi.org/10.1371/journal.pone.0077843.
Frasier CR, Zhang H, Offord J, Dang LT, Auerbach DS, Shi H, Chen C, Goldman AM, Eckhardt LL, Bezzerides VJ, Parent JM, Isom LL. Channelopathy as a SUDEP biomarker in Dravet syndrome patient-derived cardiac myocytes. Stem Cell Rep. 2018;11(3):626–34. https://doi.org/10.1016/j.stemcr.2018.07.012. Epub 2018 Aug 23.
Kalume F, Westenbroek RE, Cheah CS, Yu FH, Oakley JC, Scheuer T, Catterall WA. Sudden unexpected death in a mouse model of Dravet syndrome. J Clin Invest. 2013;123:1798–808. https://doi.org/10.1172/JCI66220.
Auerbach DS, McNitt S, Gross RA, Zareba W, Dirksen RT, Moss AJ. Genetic biomarkers for the risk of seizures in long QT syndrome. Neurology. 2016;87(16):1660–8. https://doi.org/10.1212/WNL.0000000000003056. Epub 2016 Jul 27. Erratum in: Neurology. 2018;90(24):1127.
Coll M, Striano P, Ferrer-Costa C, Campuzano O, Matés J, Del Olmo B, Iglesias A, Pérez-Serra A, Mademont I, Picó F, Oliva A, Brugada R. Targeted next-generation sequencing provides novel clues for associated epilepsy and cardiac conduction disorder/SUDEP. PLoS One. 2017;12(12):e0189618. https://doi.org/10.1371/journal.pone.0189618.
Sahly AN, Shevell M, Sadleir LG, Myers KA. SUDEP risk and autonomic dysfunction in genetic epilepsies. Auton Neurosci. 2022;237:102907. https://doi.org/10.1016/j.autneu.2021.102907. Epub 2021 Nov 10.
Costagliola G, Orsini A, Coll M, Brugada R, Parisi P, Striano P. The brain-heart interaction in epilepsy: implications for diagnosis, therapy, and SUDEP prevention. Ann Clin Transl Neurol. 2021;8(7):1557–68. https://doi.org/10.1002/acn3.51382. Epub 2021 May 28.
Parisi P, Oliva A, Coll Vidal M, Partemi S, Campuzano O, Iglesias A, Pisani D, Pascali VL, Paolino MC, Villa MP, Zara F, Tassinari CA, Striano P, Brugada R. Coexistence of epilepsy and Brugada syndrome in a family with SCN5A mutation. Epilepsy Res. 2013;105(3):415–8. https://doi.org/10.1016/j.eplepsyres.2013.02.024. Epub 2013 Mar 25.
Ramachandrannair R, Jack SM. SUDEP: what do adult patients want to know? Epilepsy Behav. 2016;64(Pt A):195–9. https://doi.org/10.1016/j.yebeh.2016.09.022.
Ramachandrannair R, Jack SM, Meaney BF, Ronen GM. SUDEP: what do parents want to know? Epilepsy Behav. 2013;29(3):560–4. https://doi.org/10.1016/j.yebeh.2013.09.040.
Strzelczyk A, Zschebek G, Bauer S, Baumgartner C, Grond M, Hermsen A, Kieslich M, Krämer G, Kurlemann G, May TW, Mayer T, Neubauer BA, Pfäfflin M, Plecko B, Ryvlin P, Schubert-Bast S, Stefan H, Trinka E, Knake S, Seifart C, Rosenow F. Predictors of and attitudes toward counseling about SUDEP and other epilepsy risk factors among Austrian, German, and Swiss neurologists and neuropediatricians. Epilepsia. 2016;57(4):612–20. https://doi.org/10.1111/epi.13337.
Casciato S, Quarato PP, Mascia A, D’Aniello A, Esposito V, Morace R, Pavone L, Di Bonaventura C, Tombini M, Assenza G, Di Gennaro G. Ictal asystole in drug-resistant focal epilepsy: two decades of experience from an epilepsy monitoring unit. Brain Sci. 2020;10(7):443. https://doi.org/10.3390/brainsci10070443.
Kohno R, Abe H, Akamatsu N, Benditt DG. Long-term follow-up of ictal asystole in temporal lobe epilepsy: is permanent pacemaker therapy needed? J Cardiovasc Electrophysiol. 2016;27:930–6.
Benditt DG, van Dijk G, Thijs RD. Ictal asystole: life-threatening vagal storm or a benign seizure selftermination mechanism? Circ Arrhythm Electrophysiol. 2015;8:11–4.
Ruiz-Giménez J, Sánchez-Álvarez JC, Cañadillas-Hidalgo F, Serrano-Castro PJ. Antiepileptic treatment in patients with epilepsy and other comorbidities. Seizure. 2010;19(7):375–82. https://doi.org/10.1016/j.seizure.2010.05.008.
Olesen JB, Abildstrøm SZ, Erdal J, Gislason GH, Weeke P, Andersson C, Torp-Pedersen C, Hansen PR. Effects of epilepsy and selected antiepileptic drugs on risk of myocardial infarction, stroke, and death in patients with or without previous stroke: a nationwide cohort study. Pharmacoepidemiol Drug Saf. 2011;20(9):964–71. https://doi.org/10.1002/pds.2186.
Kasarskis EJ, Kuo CS, Berger R, Nelson KR. Carbamazepine-induced cardiac dysfunction. Characterization of two distinct clinical syndromes. Arch Intern Med. 1992;152:186–91. https://doi.org/10.1001/archinte.152.1.186.
Randazzo DN, Ciccone A, Schweitzer P, Winters SL. Complete atrioventricular block with ventricular asystole following infusion of intravenous phenytoin. J Electrocardiol. 1995;28:157–9. https://doi.org/10.1016/S0022-0736(05)80287-0.
Nizam A, Mylavarapu K, Thomas D, Briskin K, Wu B, Saluja D, Wong S. Lacosamide-induced second-degree atrioventricular block in a patient with partial epilepsy. Epilepsia. 2011;52(10):e153–5. https://doi.org/10.1111/j.1528-1167.2011.03212.x. Epub 2011 Jul 29.
Chinnasami S, Rathore C, Duncan JS. Sinus node dysfunction: an adverse effect of lacosamide. Epilepsia. 2013;54:e90–3. https://doi.org/10.1111/epi.12108.
Degiorgio CM. Atrial flutter/atrial fibrillation associated with lacosamide for partial seizures. Epilepsy Behav. 2010;18:322–4. https://doi.org/10.1016/j.yebeh.2010.04.043.
Ryvlin P, Cucherat M, Rheims S. Risk of sudden unexpected death in epilepsy in patients given adjunctive antiepileptic treatment for refractory seizures: a meta-analysis of placebo-controlled randomised trials. Lancet Neurol. 2011;10(11):961–8. https://doi.org/10.1016/S1474-4422(11)70193-4.
Sperling MR, Barshow S, Nei M, Asadi-Pooya AA. A reappraisal of mortality after epilepsy surgery. Neurology. 2016;86(21):1938–44. https://doi.org/10.1212/WNL.0000000000002700. Epub 2016 Apr 27.
Sperling MR, Feldman H, Kinman J, Liporace JD, O’Connor MJ. Seizure control and mortality in epilepsy. Ann Neurol. 1999;46(1):45–50. https://doi.org/10.1002/1531-8249(199907)46:1<45::aid-ana8>3.0.co;2-i.
Salanova V, Markand O, Worth R. Temporal lobe epilepsy surgery: outcome, complications, and late mortality rate in 215 patients. Epilepsia. 2002;43:170–4.
Bestawros M, Darbar D, Arain A, Abou-Khalil B, Plummer D, Dupont WD, Raj SR. Ictal asystole and ictal syncope: insights into clinical management. Circ Arrhythm Electrophysiol. 2015;8(1):159–64. https://doi.org/10.1161/CIRCEP.114.001667. Epub 2014 Nov 12.
Moseley BD, Ghearing GR, Benarroch EE, Britton JW. Early seizure termination in ictal asystole. Epilepsy Res. 2011;97(1–2):220–4. https://doi.org/10.1016/j.eplepsyres.2011.08.008. Epub 2011 Sep 6.
van Westrhenen A, Shmuely S, Surges R, Diehl B, Friedman D, Leijten FSS, van Hoey SJ, Benditt DG, van Dijk JG, Thijs RD. Timing of syncope in ictal asystole as a guide when considering pacemaker implantation. J Cardiovasc Electrophysiol. 2021;32(11):3019–26. https://doi.org/10.1111/jce.15239. Epub 2021 Sep 19.
Garamendi I, Acera M, Agundez M, Galbarriatu L, Marinas A, Pomposo I, Valle E, Palma JA, Gomez-Esteban JC. Cardiovascular autonomic and hemodynamic responses to vagus nerve stimulation in drug-resistant epilepsy. Seizure. 2017;45:56–60. https://doi.org/10.1016/j.seizure.2016.11.018. Epub 2016 Dec 2.
Sveinsson O, Andersson T, Mattsson P, Carlsson S, Tomson T. Clinical risk factors in SUDEP: a nationwide population-based case-control study. Neurology. 2020;94:e419–29.
Ryvlin P, So EL, Gordon CM, Hesdorffer DC, Sperling MR, Devinsky O, Bunker MT, Olin B, Friedman D. Long-term surveillance of SUDEP in drug-resistant epilepsy patients treated with VNS therapy. Epilepsia. 2018;59(3):562–72. https://doi.org/10.1111/epi.14002. Epub 2018 Jan 16.
Verrier RL, Nearing BD, Olin B, Boon P, Schachter SC. Baseline elevation and reduction in cardiac electrical instability assessed by quantitative T-wave alternans in patients with drug-resistant epilepsy treated with vagus nerve stimulation in the AspireSR E-36 trial. Epilepsy Behav. 2016;62:85–9.
Langan Y, Nashef L, Sander JW. Case-control study of SUDEP. Neurology. 2005;64:1131–3.
Maguire MJ, Jackson CF, Marson AG, Nevitt SJ. Treatments for the prevention of sudden unexpected death in epilepsy (SUDEP). Cochrane Database Syst Rev. 2020;4:CD011792.
van der Lende M, Hesdorffer DC, Sander JW, Thijs RD. Nocturnal supervision and SUDEP risk at different epilepsy care settings. Neurology. 2018;91:e1508–18.
Seyal M, Bateman LM, Li CS. Impact of periictal interventions on respiratory dysfunction, postictal EEG suppression, and postictal immobility. Epilepsia. 2013;54(2):377–82. https://doi.org/10.1111/j.1528-1167.2012.03691.x.
Kang JY, Rabiei AH, Myint L, Nei M. Equivocal significance of post-ictal generalized EEG suppression as a marker of SUDEP risk. Seizure. 2017;48:28–32. https://doi.org/10.1016/j.seizure.2017.03.017.
Nagai Y, Aram J, Koepp M, Lemieux L, Mula M, Critchley H, Sisodiya S, Cercignani M. Epileptic seizures are reduced by autonomic biofeedback therapy through enhancement of fronto-limbic connectivity: a controlled trial and neuroimaging study. EBioMedicine. 2018;27:112–22.
Lee J, Devinsky O. The role of autonomic dysfunction in sudden unexplained death in epilepsy patients. Rev Neurol Dis. 2005;2(2):61–9.
Ryvlin P, Ciumas C, Wisniewski I, Beniczky S. Wearable devices for sudden unexpected death in epilepsy prevention. Epilepsia. 2018;59(Suppl. 1):61–6.
Rheims S. Wearable devices for seizure detection: is it time to translate into our clinical practice. Rev Neurol. 2020;176:480–4. https://doi.org/10.1016/j.neurol.2019.12.012.
Beniczky S, Jeppesen J. Non-electroencephalography-based seizure detection. Curr Opin Neurol. 2019;32:198–204. https://doi.org/10.1097/WCO.0000000000000658.
Schuele SU, Widdess-Walsh P, Bermeo A, Lüders HO. Sudden unexplained death in epilepsy: the role of the heart. Clevel Clin J Med. 2007;74(Suppl 1):121.
Schuele SU, Bermeo AC, Alexopoulos AV, Burgess RC. Anoxia-ischemia: a mechanism of seizure termination in ictal asystole. Epilepsia. 2010;51(1):170–3. https://doi.org/10.1111/j.1528-1167.2009.02168.x.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Parisi, P., Sciruicchio, V., D’Agnano, D., Raieli, V., Di Nardo, G., Ferretti, A. (2023). Autonomic Involvement in Childhood Epilepsy. In: Micieli, G., Hilz, M., Cortelli, P. (eds) Autonomic Disorders in Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-031-43036-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-43036-7_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-43035-0
Online ISBN: 978-3-031-43036-7
eBook Packages: MedicineMedicine (R0)