Abstract
Studies have shown that women are at a greater risk of developing Alzheimer’s disease (AD) than men, and although the reason behind this is not very clear, a longer life span than men cannot be the whole answer as to why women are more likely than men to develop Alzheimer’s disease, because even among individuals who are living and of the same age, women are more likely to be diagnosed with Alzheimer’s than men. The longer life spans observed in women do not fully explain the sex bias for Alzheimer’s disease but increase the overall prevalence of all-cause dementia in women among the oldest old.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
Dementia is an umbrella term that houses a group of diseases and illnesses that affect thinking, memory, reasoning, personality, mood, and behavior (Fig. 4.1). Dementia which was previously seen as a Western world problem has gradually become a serious stigma for people in the low- and middle-income countries. It is the most dreaded condition of our time but is highly neglected in Nigeria. The World Health Organization (WHO, 2021), estimates that the number of individuals with dementia worldwide is approximately 55 million, with this number expected to reach approximately 78 million by 2030 and 139 million by 2050.
Alzheimer’s disease (AD) is the most common form of dementia, accounting for approximately 60–70% of cases (Villemagne et al. 2013). Alzheimer’s disease is a type of brain disease, just as coronary artery disease is a type of heart disease. It is a progressive disease, meaning that it becomes worse with time. It is degenerative, which means cells degenerate or break down. It is irreversible, which means damage cannot be repaired.
Alzheimer’s starts with changes in the brain that are unnoticeable to the person affected. Only after years of brain changes do individuals experience noticeable symptoms such as memory loss and language problems. Symptoms occur because nerve cells (neurons) in parts of the brain involved in thinking, learning, and memory (cognitive function) have been damaged or destroyed (Fig. 4.2). As the disease progresses, neurons in other parts of the brain are damaged or destroyed as well (Figs. 4.3 and 4.4). Eventually, neurons in parts of the brain that enable a person to carry out basic bodily functions, such as walking and swallowing, are affected. Individuals become bed-bound and require around-the-clock care. Alzheimer’s disease is ultimately fatal (Jack et al. 2009; Braak et al. 2011; Villemagne et al. 2013; Bateman et al. 2012; Reiman et al. 2012; Gordon et al. 2018).
4.2 Alzheimer’s Disproportionately Affects Women than Men
Clinical studies indicate that Alzheimer’s disease disproportionately affects women in both disease prevalence and rate of symptom progression, but the mechanisms underlying this sexual divergence are unknown (Daniel et al. 2018). AD is one of the leading causes of death in the world, currently ranked sixth. Approximately 5.7 million Americans suffer from Alzheimer’s, of which almost two-thirds are women (Alzheimer’s Association). Of the 6.5 million people aged 65 and older with Alzheimer’s in the United States, four million are women and 2.5 million are men (Rajan et al. 2021, Bureau). This represents 12% of women and 9% of men aged 65 and older in the United States (U.S. Census Bureau 2014). Women live longer than men on average, and older age is the greatest risk factor for Alzheimer’s (Chene et al. 2015; Seshadri et al. 1997; Hebert et al. 2001). This survival difference contributes to a higher prevalence of Alzheimer’s and other dementias in women compared with men.
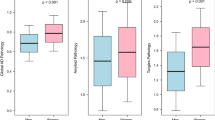
Every sixty-five seconds, another person develops Alzheimer’s disease, and of these newcomers, roughly two-thirds will be women. For a woman over 60, the risk of developing Alzheimer’s is twice that of developing breast cancer (Shriver). One study followed 16,926 people in Sweden and found that, beginning around age 80, women were more likely to be diagnosed with Alzheimer’s disease than men of the same age (Beam et al. 2018). Similarly, a study based in Taiwan found that one’s chances of developing Alzheimer’s disease over seven years were greater in women compared to men (Liu et al. 2019). A meta-analysis examining the incidence of Alzheimer’s disease in Europe found that approximately 13 women out of 1000 developed Alzheimer’s each year, compared to only seven men (Niu et al. 2017). Our study on Sexual Dimorphism in Dementia and Alzheimer Diseases analyzed 82 Alzheimer’s and dementia patients admitted in the Psychiatric hospital rumuigbo, Port-Harcourt, Nigeria showed that a greater number of women than men were affected by Alzheimer’s disease (Ibeachu et al. 2022) (Fig. 4.5).
Data from the Framingham Study, which enrolled a total of 2611 cognitively intact participants (1550 women and 1061 men) and followed up on many for 20 years, indicated that for a 65-year-old man, the remaining lifetime risk of AD was 6.3% (95% confidence interval [CI], 3.9 to 8.7) and remaining lifetime risk of developing any dementing illness was 10.9% (95% CI, 8.0 to 13.8); corresponding risks for a 65-year-old woman were 12% (95% CI, 9.2 to 14.8) and 19% (95% CI, 17.2 to 22.5), almost twice that of men (Seshadri et al. 1997).
Several epidemiologic studies show that neurodegeneration and clinical symptoms occur more rapidly for females once a diagnosis is suspected (Lin et al. 2015; Sinforiani et al. 2010; Hebert et al. 2013). Researchers have hypothesized that this is due to longer female life expectancy or sociocultural detection bias (Mielke et al. 2014); however, there is support that faster progression is due to neurobiological vulnerability in postmenopausal females (Seshadri et al. 1997; Lin et al. 2015). Though the progression of the disease may be more rapid among elderly women, studies conducted in the United States and the United Kingdom suggest that males with AD have a shorter survival time (Kua et al. 2014; Burns et al. 1991). Women are often diagnosed earlier during illness than men, which could confound the determination of postdiagnosis longevity (Podcasy and Epperson 2016).
4.3 Brief History of Alzheimer’s Disease
The brain disease that has come to be known as Alzheimer’s disease was first described in November of 1901. The chain of events began when Karl Deter brought his wife, Auguste, to the StädtischeHeilanstaltfürIrre und Epileptische (City Hospital for the Mentally Ill and Epileptics) in Frankfurt, Germany. Auguste’s behavior made it almost impossible for Karl to work anymore. She would sometimes wake up in the night and scream for hours. Knowing what we know now of Alzheimer’s disease, she undoubtedly needed a lot of personal care. Upon her admission, she was interviewed by a resident at the hospital, a young doctor named Aloysius Alzheimer. He had joined the staff at the hospital 13 years earlier and was pursuing his interests in psychiatry and neuropathology. Auguste Deter had problems with memory and with reading and writing, and she showed signs of disorientation. She was diagnosed with presenile dementia.
4.4 The Hallmarks of Alzheimer’s
-
Amyloid plaques and neurofibrillary tangles are considered the “hallmark” of Alzheimer’s disease.
-
They form in and around the existing healthy brain cells, often choking them out and causing the brain cells to shrink and die off.
-
The brain can shrink up to two-thirds of its original size and weight throughout the course of the disease.
4.5 Risk Factors for Alzheimer’s Disease
4.5.1 Non-modifiable Risk Factors
Age
Age is the greatest of these three risk factors. The percentage of people with Alzheimer’s dementia increases dramatically with age: 5.0% of people aged 65 to 74, 13.1% of people aged 75 to 84, and 33.2% of people aged 85 or older have Alzheimer’s dementia.
Family History
Those who have a parent, sibling, or child with Alzheimer’s are more likely to get Alzheimer’s.
Genetics (Heredity)
Less than 1% of Alzheimer’s cases are caused by deterministic genes (genes that cause a disease, rather than increase the risk of developing a disease). APOE e4- increases the risk of Alzheimer’s.
Gender
Women are more likely to develop AD than men.
4.5.2 Modifiable Risk Factors
Mild cognitive impairment, high blood pressure, cholesterol, poorly controlled diabetes, limited education, traumatic brain injury, depression, sleep deprivation/insomnia, obesity BMI > 30, alcohol>21/week, smoking, and social isolation.
4.6 Evidence-Based Study on the Sex Differences in Alzheimer’s Disease
Sexual dimorphism in dementia and Alzheimer diseases: A neuropsychiatric hospital-based study (Ibeachu et al. 2022)
4.7 Facts about Women
-
1.
Stress-related disorders such as anxiety and depression (postpartum) occur twice as often in women than in men. The question is what accounts for this big difference between men and women?
-
2.
Most women are emotionally and psychologically traumatized.
-
3.
Women suffer sleep deprivation more than men (starting from puberty, pregnancy, and parturition).
-
4.
Women are caregivers to their children, parents, and even extended family members.
-
5.
Women are over three times more likely than men to be diagnosed with an autoimmune disorder, including those that attack the brain, like multiple sclerosis.
-
6.
Women are up to four times more likely to suffer from migraines and headaches than men.
-
7.
Women are more prone than men to developing meningiomas, the most common brain tumor. Strokes kill more women than men (Lisa Mosconi, The XX Brain).
4.8 Facts about Women and Alzheimer’s
The statistics on women and Alzheimer’s disease are very startling.
-
1.
Do you know that women are disproportionately affected by Alzheimer’s disease more than men?
-
2.
More women are affected by dementia worldwide than men, for every man with dementia there are two women (Mielke et al. 2014).
-
3.
Brain scan tells us that the rate at which brain cells are dying in the brain is faster in women than in men.
-
4.
Women are more likely to live longer than men. However, although the risk increases with age, dementia is caused by the disease of the brain and not age alone.
-
5.
Women in their 60 s are more than twice as likely to develop Alzheimer’s disease over the rest of their lives as they are to develop breast cancer (Mielke et al. 2014).
-
6.
Every 66 s someone in the United States develops Alzheimer’s, and by 2050, it will be every 33 s; it may interest you to know that two-thirds of them are women.
-
7.
Another disconcerting stat is that once women develop mild cognitive impairment, their cognitive decline is two times faster than men.
4.9 Factors that Place Women at Greater Risk
It’s not exactly clear why women are more affected by Alzheimer’s than men, but there may be several factors at play. According to Dr. Caldwell, women tend to decline faster than men after receiving a diagnosis for Alzheimer’s. I believe that women’s vulnerability to Alzheimer’s disease is multifactorial and studies should look beyond age and embark on a holistic research to investigate why women are disproportionately affected by Alzheimer’s disease. Women typically live longer than men, too, and while the No. 1 risk factor for Alzheimer’s is aging, that may not be the whole story (Dr. Caldwell 2022).
4.10 The Factors that Contribute Greatly
Longevity
Age is a risk factor. Scientists once thought that women were harder hit by Alzheimer’s because of generally living longer than men. Heather Snyder, senior director of medical and scientific operations for the Alzheimer’s Association, says that this isn’t the case and that new studies suggest there are different biological pathways in women’s brains and that hormones or even the way women’s brains metabolize food differently may explain why Alzheimer’s manifests itself more in women. Again, Alzheimer’s is not a natural aging sickness, and studies have shown that Alzheimer’s disease is thought to begin 20 years or more before symptoms arise. Women’s brains have unique risk factors for dementia that until now have been ignored by science (Mielke et al. 2014).
Female Hormone
Estrogen gives a neuroprotective effect to the brain. A decline in estrogen is the leading cause of problems that affect women after age 35. It has been hypothesized that the rapid decrease in estrogen during menopause functions as a trigger for the development of AD in women due to these neuroprotective abilities (Paganini-Hill and Henderson 1994).
Menopause
Menopause and estrogen loss are a huge area of investigation for Alzheimer’s because estrogen supports an area of the brain (the hippocampus) responsible for forming new memories. It’s this part of the brain that’s first targeted when Alzheimer’s develops, so as women age, they may be even more affected. Plus, women have a greater increase in Alzheimer’s risk, compared to men, when they carry a gene associated with late-onset Alzheimer’s. But on the other hand, there is a line of research that suggests having two X-chromosomes might put women at an advantage. The menopause state in midlife is associated with a decline in the brain’s ability to utilize glucose as its primary fuel and an increase in neuro-inflammatory responses in the brain. That combination is a dual hit for the female brain (Roberta Diaz Brinton n.d.).
APOE e4 Gene
It is unclear whether genetic risk operates differently in women and men in the development of, or susceptibility to, Alzheimer’s pathology (Carter et al. 2012). Several studies have shown that the APOE-e4 genotype, the best-known common genetic risk factor for Alzheimer’s dementia, may have a stronger association with Alzheimer’s dementia (Altmann et al. 2014; Ungar et al. 2014) and neurodegeneration (Hohman et al. 2018) in women than in men. A recent meta-analysis found no difference between men and women in the association between APOE-e4 and Alzheimer’s dementia overall, although age played an interesting interactive role. That is, APOE-e4 was related to higher Alzheimer’s risk in women than men between ages 55 and 70, when APOE-e4 is thought to exert its largest effects (Neu et al. 2017). It is unclear whether the influence of APOE-e4 may depend on the sex hormone estrogen (Yaffe et al. 2000; Kang and Grodstein 2012).
New Gene Linked to the Increased Risk of Alzheimer’s in Women
Recent research has shown the Genome-wide association studies (GWAS), O6-methylguanine-DNA methyltransferase, MGMT gene may be associated with a higher risk of AD in two different populations, particularly in women without APOE e4. About 60% of people with AD don’t express apolipoprotein E (APOE e4), its most established genetic risk factor. The study found that the expression of MGMT contributes to the development of toxic proteins associated with Alzheimer’s, especially in women: To understand if other genes involved in tau-related diseases are related to AD risk in women, the researchers performed GWAS on two different populations:
-
Thirty-one members of the Hutterites, a group of people with common ancestry, recognized for their relatively small gene pool, 22 of whom were women.
-
10,340 women without APOE e4, who were part of the Alzheimer’s Disease Genetics Consortium (ADGC). These included 3399 AD cases and 6905 controls. They found that in both populations, the MGMT gene was associated with AD risk in women lacking APOE e4 (Chung et al. 2022).
Stress and Sleep Deprivation
Another brain region which is affected by the decline in estrogen is the brain stem. The brain stem regulates sleep and stress. Stress increases the cortisol level in the body which leads to a decrease in estrogen, hence sleep deprivation. All these happen because women juggle a lot of things. Puberty, pregnancy, and parturition cause negative changes in a woman’s brain. Sleep deprivation as a mother and a caregiver also affects hormones and neuronal connectivity.
Education Women
are generally less educated than men. People with more years of formal education are at lower risk for Alzheimer’s and other dementias than those with fewer years of formal education (Kukull et al. 2002; Evans et al. 2003, Fitzpatrick et al. 2004, Sando et al. 2008, Stern 2012, Hendrie et al. 2018). The underlying reasons for the relationship between formal education and reduced Alzheimer’s risk are unclear. Some researchers believe that having more years of education builds “cognitive reserve.” Cognitive reserve refers to the brain’s ability to make flexible and efficient use of cognitive networks (networks of neuron-to-neuron connections) to enable a person to continue to carry out cognitive tasks despite brain changes (Stern 2002; Stern et al. 2018). The number of years of formal education is not the only determinant of cognitive reserve. Having a mentally stimulating job and engaging in other mentally stimulating activities may also help build cognitive reserve (Fisher et al. 2014; Grzywacz et al. 2016; Pool et al. 2016; Then et al. 2014).
4.11 Way Forward: Change in Lifestyle Can Reverse or Slow the Early Onset of Alzheimer’s
There is increasing evidence that there are steps people can take to reduce their risk of developing certain dementias or to delay their onset. In 2015, the Alzheimer’s Association evaluated the state of the evidence on the effects of modifiable risk factors. They concluded that “regular physical activity and management of cardiovascular risk factors (especially diabetes, obesity, smoking and hypertension) reduce the risk of cognitive decline and may reduce the risk of dementia.” A healthy diet and lifelong learning/cognitive training may also reduce the risk of cognitive decline. These findings were largely confirmed by the Institute of Medicine in 2015. The possible ways to reduce, reverse, or slow the risk of developing Alzheimer’s are as follows:
Early Detection
Early detection of Alzheimer’s signs and symptoms will be very useful in making better decisions on the treatment plan, which if properly adopted will slow down or reverse the progression of Alzheimer’s disease.
Exercise and Stay Physically Active
Exercise is a great fuel to the brain because it increases blood flow to the brain and also can build new brain cells. Exercise regularly and be physically active. Physical exercises such as dancing, walking, jogging, biking, swimming, or aerobic classes at least 30 min per day, 5 days per week have proven very effective in improving brain function, slowing down the disease progression and reducing brain cell loss in older persons. It reduces the risk of heart-related disease, and thus can also be protective against dementia. It does not have to be strenuous: It is most effective when combined with social activity and a brain-healthy diet. Physical activity that combines mental activity with social activity (e.g., going for a walk and mentally planning the route) may also be effective.
Healthy Diet
Eat right and maintain a healthy weight. It is important to cut down on the Western diet and eat more of a Mediterranean-style diet.
-
Reduce intake of foods high in fat or cholesterol:
High saturated fat and cholesterol clog the arteries. People living with high cholesterol or high blood pressure were six times as likely to develop AD. “Good” cholesterol, or HDL, may protect the brain (e.g., olive oil). Bake or grill instead of frying foods.
-
Increase your intake of protective foods:
Dark-skinned fruits and vegetables have the highest level of antioxidants.
-
Kale, spinach, brussels sprouts, alfalfa sprouts, broccoli, beets, red bell pepper, onion, corn, and eggplant.
-
Prunes, raisins, blueberries, blackberries, strawberries, raspberries, plums, oranges, red grapes, and cherries.
-
Cold water fish contain beneficial omega-3 fatty acids: halibut, mackerel, salmon, trout, and tuna.
-
Nuts can be a useful part of your diet; almonds, pecans, and walnuts are a good source of vitamin E, an antioxidant.
-
Seeds: pumpkin seeds, flaxseeds, chia seeds, sunflower seeds.
-
Seed oil: Flaxseed oil is very good for phyto-estrogen. Eat other foods sparingly.
-
Taken from: http://www.alz.org/we_can_help_brain_health_maintain_your_brain.asp.
Remain Socially Active
Stay socially connected, attend social gatherings occasionally. Recent research suggests that those who combine physical, mental, and social activity are most likely to prevent dementia. Consider doing the following: stay active in the workplace; volunteer in community groups and causes; join bridge clubs, square dancing clubs, or other social groups; and travel.
-
Sleep: Quality sleep helps to wipe out some Alzheimer’s disease plagues.
-
Meditation.
-
Avoid drinking too much alcohol.
-
Stop smoking.
Get Educated to Stay Mentally Active
The idea here is to build a better brain, or what Dr. Caldwell refers to as “cognitive reserve.” By getting your formal education and continuing to learn and practice what you’ve learned over time, you’re strengthening your brain along the way, almost like a suit of armor. “The better brain you build, the more you have to draw from if you were to ever get a neurodegenerative disorder like Alzheimer’s disease,” says Dr. Caldwell.
It’s possible that pushing yourself to actively learn whenever possible can strengthen your cognitive abilities, so even if you have Alzheimer’s, your symptoms may show up later in life, or in the best-case scenario, not at all. Keep your brain active every day, start with something small, then add another change each day. Stay curious and involved—commit to lifelong learning, read, write, work crossword or other puzzles, and attend lectures and plays. Enroll in courses at your local adult education center, community college, or other community groups (Taken from: http://www.alz.org/we_can_help_brain_health_maintain_your_brain.asp).
4.12 Implication for SDG 3
4.12.1 SDG3, Target 3.3
By 2030, end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases and combat hepatitis, water-borne diseases, and other communicable diseases: Dementia, which was previously seen as a Western world problem, has gradually become a serious stigma for people in the low- and middle-income countries.
4.12.2 Target 3.7
By 2030, ensure universal access to sexual and reproductive healthcare services, including family planning, information and education, and the integration of reproductive health into national strategies and programs: Women are generally less educated than men. People with more years of formal education are at lower risk for Alzheimer’s and other dementias than those with fewer years of formal education.
4.12.3 Target 3.8
Achieve universal health coverage, including financial risk protection; access to quality essential healthcare services; and access to safe, effective, quality, and affordable essential medicines and vaccines for all: Early detection of Alzheimer’s signs and symptoms will be very useful in making better decisions on the treatment plan, which if properly adopted will slow down or reverse the progression of Alzheimer’s disease.
4.12.4 Target 3.9
By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water, and soil pollution and contamination: AD is one of the leading causes of death in the world, currently ranked sixth.
4.13 Conclusion
Alzheimer’s disease is tagged as an old-age problem and therefore receives little or no attention. Females suffering from this disease are stigmatized and the families are advised not to waste their resources in treatment. The gender disparity in dementia and AD is alarming, hence strategic plans to help women suffering from this condition are highly recommended because dementia is not just a natural aging problem but a progressive distortion in the brain tissues caused by the accumulation of hormonal imbalances, emotional trauma, abuse, and other stress-related conditions that females encounter at different stages of their lifetime.
People of all ages are to live healthy lives and to advance well-being, according to SDG 3. At every stage of one’s life, beginning at birth, health and well-being are crucial. However, it is impossible to discuss health and happiness without mentioning mental health. The brain is the central processing unit that steers all bodily functions. Alzheimer’s disease is a serious public health problem that challenges the well-being of an individual. A type of dementia that affects older people more frequently is Alzheimer’s disease. Memory loss, confusion, personality changes, and other symptoms of dementia can all have an impact on a person’s overall health, including the caregiver.
References
Altmann A, Tian L, Henderson VW, Greicius MD. Alzheimer’s Disease Neuroimaging Initiative Investigators. Sex modifies the APOE-related risk of developing Alzheimer disease. Ann Neurol. 2014;75(4):563–73.
Bateman RJ, Xiong C, Benzinger TL, Fagan AM, Goate A, Fox NC, et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N Engl J Med. 2012;367(9):795–804.
Beam CR, Kaneshiro C, Jang JY, Reynolds CA, Pedersen NL, Gatz M. Differences between women and men in incidence rates of dementia and Alzheimer’s disease. J Alzheimers Dis. 2018;64(4):1077–83. https://doi.org/10.3233/JAD-180141. PMID: 30010124; PMCID: PMC6226313
Braak H, Thal DR, Ghebremedhin E, Del Tredici K. Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. J Neuropathol Exp Neurol. 2011;70(11):960–9.
Roberta Diaz Brinton, PhD, director of the Center for Innovation in Brain Science at the University of Arizona and a leading neuroscientist in the field of Alzheimer’s and the aging female brain.
Burns A, Lewis G, Jacoby R, Levy R. Factors affecting survival in Alzheimer's disease. Psychol Med. 1991;21(2):363–70.
Caldwell J. Sex and gender in Alzheimer’s disease risk and resilience 2022.
Carter CL, Resnick EM, Mallampalli M, Kalbarczyk A. Sex and gender differences in Alzheimer’s disease: recommendations for future research. J Women's Health. 2012;21(10):1018–23.
Chene G, Beiser A, Au R, Preis SR, Wolf PA, Dufouil C, et al. Gender and incidence of dementia in the Framingham Heart Study from mid-adult life. Alzheimers Dement. 2015;11(3):310–20.
Chung J, Das A, Sun X, et al. Genome-wide association and multi omics studies identify MGMT as a novel risk gene for Alzheimer’s disease among women. Alzheimers Dement. 2022:1–13.
Daniel WF, Bennett DA, Dong H. Sexual dimorphism in predisposition to Alzheimer’s disease. Neurobiol Aging. 2018;70:308–24.
Evans DA, Bennett DA, Wilson RS, Bienias JL, Morris MC, Scherr PA, et al. Incidence of Alzheimer disease in a biracial urban community: relation to apolipoprotein E allele status. Arch Neurol. 2003;60(2):185–9.
Fisher GG, Stachowski A, Infurna FJ, Faul JD, Grosch J, Tetrick LE. Mental work demands, retirement, and longitudinal trajectories of cognitive functioning. J Occup Health Psychol. 2014;19(2):231–42.
Fitzpatrick AL, Kuller LH, Ives DG, Lopez OL, Jagust W, Breitner JC, et al. Incidence and prevalence of dementia in the cardiovascular health study. J Am Geriatr Soc. 2004;52(2):195–204.
Gordon BA, Blazey TM, Su Y, Hari-Raj A, Dincer A, Flores S, et al. Spatial patterns of neuroimaging biomarker change in individuals from families with autosomal dominant Alzheimer’s disease: a longitudinal study. Lancet Neurol. 2018;17(3):241–50.
Grzywacz JG, Segel-Karpas D, Lachman ME. Workplace exposures and cognitive function during adulthood: Evidence from National Survey of Midlife Development and the O*NET. J Occup Environ Med. 2016;58(6):535–41.
Hebert LE, Scherr PA, McCann JJ, Beckett LA, Evans DA. Is the risk of developing Alzheimer’s disease greater for women than for men? Am J Epidemiol. 2001;153(2):132–6.
Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology. 2013;80(19):1778–83.
Hendrie HC, Smith-Gamble V, Lane KA, Purnell C, Clark DO, Gao S. The Association of early life factors and declining incidence rates of dementia in an elderly population of African Americans. J Gerontol B Psychol Sci Soc Sci. 2018;16(73, suppl 1):S82-9.
Hohman TJ, Dumitrescu L, Barnes LL, Thambisetty M, Beecham G, Kunkle B, et al. Sex-specific association of apolipoprotein E with cerebrospinal fluid levels of tau. JAMA Neurol. 2018;75(8):989–98.
Ibeachu PC, Uahomo PO, David LK. Sexual dimorphism in dementia and Alzheimer diseases—A neuropsychiatric hospital based study. Int Neuropsychiatr Dis J. 2022;17(1):36–45.
Jack CR, Lowe VJ, Weigand SD, Wiste HJ, Senjem ML, Knopman DS, et al. Serial PiB and MRI in normal, mild cognitive impairment and Alzheimer’s disease: implications for sequence of pathological events in Alzheimer’s disease. Brain. 2009;132:1355–65.
Kang JH, Grodstein F. Postmenopausal hormone therapy, timing of initiation, APOE and cognitive decline. Neurobiol Aging. 2012;33(7):1129–37.
Kua EH, Ho E, Tan HH, Tsoi C, Thng C, Mahendran R. The natural history of dementia. Psychogeriatrics. 2014;14(3):196–201.
Kukull WA, Higdon R, Bowen JD, McCormick WC, Teri L, Schellenberg GD, et al. Dementia and Alzheimer disease incidence: a prospective cohort study. Arch Neurol. 2002;59(11):1737–46.
Lin FC, Chuang YS, Hsieh HM, et al. Early statin use and the progression of Alzheimer disease: a total population-based case-control study. Medicine (Baltimore). 2015;94(47):e2143.
Liu CC, Li CY, Sun Y, Hu SC. Gender and age differences and the trend in the incidence and prevalence of dementia and Alzheimer's disease in Taiwan: a 7-year National Population-Based Study. Biomed Res Int. 2019;5378540 https://doi.org/10.1155/2019/5378540. PMID: 31815145; PMCID: PMC6878786
Mielke MM, Vemuri P, Rocca WA. Clinical epidemiology of Alzheimer's disease: assessing sex and gender differences. Clin Epidemiol. 2014;6:37–48.
Neu SC, Pa J, Kukull W, Beekly D, Kuzma A, Gangadharan P, et al. Apolipoprotein E genotype and sex risk factors for Alzheimer disease: a meta-analysis. JAMA Neurol. 2017;74(10):1178–89.
Niu H, Álvarez-Álvarez I, Guillén-Grima F, Aguinaga-Ontoso I. Prevalence and incidence of Alzheimer's disease in Europe: a meta-analysis. Neurologia. 2017;32(8):523–32. https://doi.org/10.1016/j.nrl.2016.02.016. English, Spanish Epub 2016 Apr 26. PMID: 27130306
Paganini-Hill A, Henderson V. Estrogen deficiency and risk of Alzheimer's disease in women. Am J Epidemiol. 1994;140:256–61.
Podcasy JL, Epperson CN. Considering sex and gender in Alzheimer disease and other dementias. Dialogues Clin Neurosci. 2016;18(4):437–46. https://doi.org/10.31887/DCNS.2016.18.4/cepperson. PMID: 28179815; PMCID: PMC5286729
Pool LR, Weuve J, Wilson RS, Bültmann U, Evans DA, Mendes de Leon CF. Occupational cognitive requirements and late-life cognitive aging. Neurology. 2016;86(15):1386–92.
Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical AD and mild cognitive impairment in the United States (2020-2060). Alzheimers Dement. 2021; https://doi.org/10.1002/alz.12362. Online ahead of print.
Reiman EM, Quiroz YT, Fleisher AS, Chen K, Velez-Pardos C, Jimenez-Del-Rio M, et al. Brain imaging and fluid biomarker analysis in young adults at genetic risk for autosomal dominant Alzheimer’s disease in the presenilin 1 E280A kindred: a case-control study. Lancet Neurol. 2012;11(2):1048–56.
Sando SB, Melquist S, Cannon A, Hutton M, Sletvold O, Saltvedt I, et al. Risk-reducing effect of education in Alzheimer’s disease. Int J Geriatr Psychiatry. 2008;23(11):1156–62.
Seshadri S, Wolf PA, Beiser A, Au R, McNulty K, White R, et al. Lifetime risk of dementia and Alzheimer’s disease. The impact of mortality on risk estimates in the Framingham study. Neurology. 1997;49(6):1498–504.
Sinforiani E, Citterio A, Zucchella C, et al. Impact of gender differences on the outcome of Alzheimer's disease. Dement Geriatr Cogn Disord. 2010;30:147–54.
Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8:448–60.
Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11(11):1006–12.
Stern Y, Arenaza-Urquijo EM, Bartres-Faz D, Belleville S, Cantilon M, Chetelat G, et al. Whitepaper: defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimers Dement. 2018; pii:S1552-5260(18): 33491-5
Then FS, Luck T, Luppa M, Arelin K, Schroeter ML, Engel C, et al. Association between mental demands at work and cognitive functioning in the general population: results of the health study of the Leipzig research Center for Civilization Diseases. J Occup Med Toxicol. 2014;9:23.
U.S. Census Bureau. National population projections: downloadable files 2014. Available at: https://www.census.gov/data/datasets/2014/demo/popproj/2014-popproj.html. Accessed December 18, 2021.
Ungar L, Altmann A, Greicius MD. Apolipoprotein E, gender, and Alzheimer’s disease: an overlooked, but potent and promising interaction. Brain Imaging Behav. 2014;8(2):262–73.
Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O, et al. Amyloid ß deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12(4):357–67.
Yaffe K, Haan M, Byers A, Tangen C, Kuller L. Estrogen use, APOE, and cognitive decline: evidence of gene-environment interaction. Neurology. 2000;54(10):1949–54.
World Health Organization. Geneva, Switzerland: World Health Organization; 2021. Fact sheets of dementia [Internet] [cited 2022 Apr 13]. Available from: https://www.who.int/news-room/factsheets/detail/dementia. [Google Scholar].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ibeachu, C.P. (2023). Women at Greater Risk of Alzheimer’s: Way Forward. In: Nwaichi, E.O. (eds) Modernity in Health and Disease Diagnosis: The Account from STEM Women. Sustainable Development Goals Series. Springer, Cham. https://doi.org/10.1007/978-3-031-34963-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-34963-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-34962-1
Online ISBN: 978-3-031-34963-8
eBook Packages: MedicineMedicine (R0)