Abstract
Diabetes mellitus has been reaching pandemic proportions as 537 million adults are living with diabetes worldwide. At the same time, we have witnessed the infectious pandemic of COVID-19 with over 557 million cases as of 15-Jul-2022. Diabetes has been one of the major risk factors for COVID-19 morbidity and mortality; on the other hand, COVID-19 has resulted in an increase of diabetes prevalence, including iatrogenic diabetes due to corticosteroids used for its treatment. Diabetes care through telemedicine has been critical for avoiding physical visits of people with diabetes (PwD) at out-patient clinics thus preventing the risk of COVID-19 infection. The role of the National e-Health System (NeHS) as a Telemedicine Platform for Preventive, Predictive, and Personalized (3P) Diabetes Care has been of utmost importance during the COVID-19 pandemics through its use for (1) monitoring metabolic control and comorbidities, (2) resupply of insulin and other antidiabetic treatment, and (3) monitoring of COVID-19 status (tests, hospitalizations, vaccinations) in PwD. The NeHS has been used as a telemedicine platform for 3P diabetes care for monitoring metabolic control and comorbidities through evaluation of uploaded laboratory reports, blood glucose monitor (BGM) and continuous glucose monitor (CGM) reports, as well as medical reports for complications and comorbidities of PwD. Treatment adjustments based on metabolic parameters and comorbidities have been recorded in the NeHS without the need of physical visit by PwD. Diabetes consults for hospitalized COVID-19 patients have been done based on the information in the NeHS thus preventing the unnecessary exposure of healthcare staff in the “red zones” of COVID-19 centers. The use of the NeHS as a telemedicine platform for 3P diabetes care has enabled the monitoring of COVID-19 status, as COVID-19 tests, COVID-19 related hospitalizations, and immunization status have been recorded in their individual EHRs. The NeHS has a critical role as a telemedicine platform for 3P diabetes care during COVID-19 pandemics, enabling monitoring of metabolic control and comorbidities, treatment adjustment and evaluation of COVID-19 status, hence providing personalized diabetes care by predicting and preventing risks of both micro- and macrovascular diabetes complications, including COVID-19 morbidity and mortality.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Telemedicine
- Predictive, preventive, personalized medicine (3 PM/PPPM)
- Diabetes care
- COVID-19
- National e-Health System, NeHS
1 The Rising Diabetes Prevalence Has a Huge Impact on the Healthcare Systems
Diabetes mellitus has been reaching pandemic proportions as it has been estimated that 537 million adults were living with diabetes worldwide in 2021 [1, 2]. The vast majority, over 75% of people with diabetes (PwD), are living in middle or low-income countries having already limited resources allocated for diabetes care [1, 3]. In addition, diabetes is among the top causes of mortality in the adult population, responsible for 6.7 million deaths in 2021 [1]. Diabetes related expenditures have increased by more than three times in the last 15 years, estimated at 966 billion USD in 2021 [1].
Diabetes drivers, such as prediabetes, might result in even higher diabetes prevalence in the future. Current estimates suggest 541 million people worldwide have impaired glucose tolerance, a form of prediabetes, and a huge number of them would eventually be diagnosed with diabetes in near future [1]. The number of PwD is, unfortunately, predicted to further rise to 643 million by 2030 and 783 million by 2045 [1]. Due to the very high and rising prevalence, it is one of the biggest healthcare challenges humanity has ever faced.
The Republic of North Macedonia is a developing country with one of the highest diabetes prevalence in Europe [1, 3,4,5,6]. The increasing prevalence of type 2 diabetes in the past three decades has been alarming and had a significant impact on the healthcare system in the country [3]. The estimated total diabetes prevalence, of both diagnosed and undiagnosed cases, in the Republic of North Macedonia was approximately 80,000 people in 2004 [3,4,5]. Diabetes prevalence has more than doubled in the last 15 years, and the estimate of total diabetes prevalence was 175,100 in 2019, with national diabetes prevalence of 11.2% (20–79 years), and age-adjusted comparative prevalence of 9.3% [3,4,5,6].
Such high national diabetes prevalence has been explained by similar dietary habits and lifestyle to Turkey, having the highest diabetes prevalence in Europe, i.e., food abundant in wheat flour, bread, pastry, lots of sweets, and high-fat meals [3,4,5]. Total caloric intake in the country per person per day increased by almost 50% from 1993 to 2011, which in combination with inadequate physical activity has resulted in 53% of the population being overweight and 20% obese [3,4,5].
Another factor contributing to the high increase of diabetes prevalence has been the psychosocial stress associated with the so-called transitional economy, i.e., a transition from planned economy with job security in the past to market economy with unprecedented rise in unemployment and associated stress, especially among the middle-aged population [3,4,5]. Additionally, the country has been in the top 10 countries in smoking prevalence worldwide [3,4,5]. The first stratified analysis of diabetes prevalence in the country found a difference in the place of living, with the population living in rural areas having higher diabetes prevalence [3,4,5].
2 COVID-19 Infection in People with Diabetes: A Perfect Storm
Another pandemic, an infectious one, COVID-19 has been an ongoing public health crisis, with over 557,917,904 confirmed cases globally, including 6,358,899 deaths, as reported to the World Health Organization (WHO) as of 15-July-2022 [7]. The Republic of North Macedonia has also been strongly affected by the COVID-19 pandemics with 317,634 confirmed cases of COVID-19 and 9,337 deaths, reported to the WHO as of 15-July-2022 (Fig. 1) [7]. The country has been ranked fifth worldwide in terms of COVID-19 mortality rate, as of 15-July-2022 [7, 8].
Adapted from the WHO data for COVID-19 (confirmed cases and deaths) for the Republic of North Macedonia, as of 15-July-2022 [7]
Recent meta-analysis has demonstrated that diabetes is significantly associated with increased odds of severe COVID-19, increased acute respiratory distress syndrome (ARDS) rate, mortality, and need for mechanical ventilation in hospitalized patients [9]. The estimated overall pooled prevalence of diabetes has been 31% in hospitalized COVID-19 patients [9].
The co-existence of COVID-19 and diabetes has been labeled as a perfect storm [10]. The COVID-19 infection is associated with acute inflammatory response and cytokine storm, acute tissue damage, acute coronary ischemia, acute kidney injury, ARDS, hyperglycemic surges, hypercoagulability, endothelial function, and fibrosis [10]. On the other hand, diabetes is associated with chronic, low-grade inflammatory response and insulin resistance, slowly progressing tissue damage, cardiovascular disease, chronic kidney disease, neuropathy, brain changes, glucose variability, hypercoagulability, endothelial dysfunction, and fibrosis [10]. Despite the marked difference in the duration of inflammation, both COVID-19 and diabetes ultimately share the same pathway resulting in glucose disturbances, hypercoagulability, endothelial dysfunction, and fibrosis [10].
Diabetes mellitus has been the most common co-occurring chronic disease in patients with multi-morbidity testing positive for COVID-19 [11]. In addition, diabetes has been the second most prevalent co-morbidity, after hypertension, in people with COVID-19 admitted to hospital [12]. It has already been emphasized that PwD were predicted to have increased risk of severe form of COVID-19 pneumonia and hospitalization [9, 12].
Of those hospitalized, people with type 1 diabetes were predicted to have approximately three times higher risk of in-hospital mortality, whereas people with type 2 diabetes were predicted to have approximately two times higher risk of in-hospital mortality compared to matched controls [13]. It has been demonstrated that poor glycemic control increases the mortality of PwD hospitalized due to COVID-19 as early as within 28 days after admission [14].
Furthermore, hazard ratio for all-cause mortality was higher in patients with higher values of fasting plasma glucose among COVID-19 patients even without known diabetes, when adjusted for age, sex, smoking, systolic blood pressure and total cholesterol [15]. A meta-analysis has demonstrated a high proportion of newly diagnosed diabetes in COVID-19 patients [16]. Newly diagnosed diabetes has been associated with higher risk of mortality than known diabetes in hospitalized patients with COVID-19 [15]. In addition, the post-discharge rate of new-onset diabetes was elevated in hospitalized COVID-19 patients compared with matched controls [17].
Public health crises, such as COVID-19, pose risks to people with diabetes, in terms of their (1) Outcomes, as PwD experience worse outcomes than the general population; (2) Access to care and management, as PwD experience reduced access to diabetes care and management; (3) Adherence to treatment, as long-term treatments have become more difficult for PwD to maintain; and (4) Psychosocial impact, as emotional and behavioral changes are increasing for PwD in response to a crisis [18, 19]. A global survey of healthcare professionals has listed diabetes on the top of the list of chronic diseases and comorbidities most impacted by COVID-19 due to the reduction in care [20].
3 Telemedicine as a Platform for 3P Diabetes Care During the COVID-19 Pandemics
Taking into consideration the magnitude of the healthcare challenge of co-existence of diabetes and COVID-19, application of Predictive, Preventive, and Personalized (3P) Medicine approach in diabetes care during COVID-19 pandemic has been of critical importance, with Predictive Medicine covering the predicted risk of related morbidity and mortality, Preventive Medicine covering the prevention of micro- and macrovascular complications, and Personalized Medicine covering personalized monitoring and treatment (Fig. 2) [21].
Diabetes has been one of the major risk factors for COVID-19 morbidity and mortality [22]; on the other hand, COVID-19 has resulted in an increase of diabetes prevalence, including iatrogenic diabetes due to corticosteroids used for its treatment [23]. Our response has been swift when it comes to infectious pandemic such as COVID-19 infection; however, when we have to deal with another pandemic developing more insidiously over years, such as diabetes, our action has not been so effective [3].
The introduction of the National e-Health System (NeHS) in the Republic of North Macedonia on 01-July-2013 was an immense step in the monitoring and improving the performance of the national healthcare system [3]. The comprehensive, national Electronic Healthcare Record (EHR) system covered all citizens across the three healthcare levels: primary care provided by family physicians, secondary care provided by specialists in general and regional hospitals, and tertiary care provided by university clinics. Implementation of the NeHS has been praised internationally as a key platform for improving the performance of the national healthcare system [3, 24].
Since the beginning of 2015, the diabetes care module in the NeHS has been upgraded with the possibility to record diabetes treatment, metabolic parameters, and diabetes complications [3, 24]. In that way, the NeHS has enabled for monitoring the prevalence of morbidities and mortalities, prescribed medications, referrals across the system, and metabolic control in one of the worst affected populations in Europe [3, 24]. Furthermore, NeHS has become an essential platform for 3P diabetes care, covering the total population of the Republic of North Macedonia [3, 24].
The concept of 3P medicine has emerged as the focal point of efforts in healthcare aimed at controlling the prevalence and management of non-communicable chronic diseases, including diabetes [3, 24,25,26,27,28]. The management of diabetes and the critical role of 3P medicine in modernization of healthcare have been acknowledged as priorities by global and regional organizations and health-related institutions such as the Organization of the United Nations, the European Union, and the National Institutes of Health [3, 24,25,26,27,28].
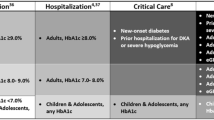
The role of the NeHS as a telemedicine platform for 3P diabetes care has been of utmost importance during the COVID-19 pandemics through its use for (1) monitoring metabolic control and comorbidities, (2) resupply of insulin and other antidiabetic treatment, and (3) monitoring of COVID-19 status (tests, hospitalizations, vaccinations) in PwD (Table 1) [3, 24].
4 Monitoring Metabolic Control and Comorbidities
In order to avoid unnecessary physical visits of PwD at out-patient clinics, the NeHS has been used as a telemedicine platform for 3P diabetes care for monitoring metabolic control through evaluation of uploaded laboratory reports, blood glucose monitor (BGM) and continuous glucose monitor (CGM) reports (Fig. 3).
By reviewing the recorded data in the NeHS, it was possible for the clinicians to provide necessary treatment recommendations. In addition, the NeHS diabetes module allows recording of metabolic parameters, such as HbA1c, glycemic profile, systolic blood pressure (SBP), diastolic blood pressure (DBP), Body Mass Index (BMI), and diabetes complications—retinopathy, nephropathy, neuropathy, peripheral artery disease, coronary artery disease, cerebrovascular disease, diabetic foot. Monitoring metabolic parameters and diabetes complications has been the cornerstone of the 3P diabetes care concept.
The NeHS as a telemedicine platform for 3P diabetes care for monitoring metabolic control and comorbidities has been essential for the PwD hospitalized due to COVID-19, or for those who have developed new-onset diabetes during COVID-19 hospitalization. Taking into consideration the above elaborated close relation between the adequate glycemic control and COVID-19 outcomes, there has been a need for frequent diabetes consultations as most of the hospitalized patients were receiving insulin treatment for achieving glycemic control. In order to alleviate the acute cytokine storm, the majority of hospitalized patients were administered pulse treatment with high doses of corticosteroids resulting in hyperglycemic surges increasing the risk of new-onset diabetes, or worsening the glycemic control of patients already diagnosed with diabetes.
All diabetes consultations for hospitalized COVID-19 patients have been done through telemedicine—based on the information recorded in the NeHS, thus preventing the unnecessary exposure of the clinicians/healthcare professionals in the red zones of the COVID-19 departments where COVID-19 patients have been hospitalized. By preventing the unnecessary exposure, the risk for contracting COVID-19 infection among the healthcare professionals has been greatly reduced.
Clinicians were able to evaluate not only the glycemic profiles in order to initiate or titrate insulin therapy, but also to assess the medical reports of other specialists as well as the diabetes complications and comorbidities recorded in the NeHS. Treatment adjustments based on metabolic parameters and comorbidities have been recorded in the NeHS without any need of physical visit by the PwD who were not hospitalized due to COVID-19, thus minimizing their risk of contracting the infection.
5 Resupply of Insulin and Other Antidiabetic Treatment
As outlined in Table 1, the NeHS as a telemedicine platform for 3P diabetes care during COVID-19 pandemics has been used for the resupply of insulin and other antidiabetic treatment (SGLT2 inhibitors, GLP-1 Receptor agonists, DPP-4 inhibitors) dispensed by the insulin pharmacies. There have been 41 insulin pharmacies throughout the country integrated with the NeHS, so based on the report and prescription by the diabetologists they would dispense the adequate treatment. Diabetologists were again able to evaluate the laboratory reports, BGM or CGM reports, diabetes metabolic parameters and comorbidities, and other medical reports, and to recommend the appropriate antidiabetic treatment.
Thus, PwD were not required to physically attend the out-patient clinics in order to obtain their life-saving medicine, and the total consultation has been through the NeHS as a telemedicine platform for 3P diabetes care, thereby preventing the risk of acquiring or spreading the COVID-19 infection. Metformin, sulphonylureas, and thiazolidinediones have been dispensed through the regular (non-insulin) pharmacies, being also integrated with the NeHS.
6 Monitoring of COVID-19 Status in People with Diabetes
In addition, the use of the NeHS as a telemedicine platform for 3P diabetes care has enabled the monitoring of COVID-19 status of PwD, as COVID-19 tests, COVID-19 related hospitalizations, and immunization status have been recorded in their individual EHRs. It has been possible for the clinicians to evaluate if the PwD tested positive for COVID-19, or if PwD were hospitalized due to COVID-19 with all the necessary laboratory and imaging reports, therapies provided, or other medical reports being available through their individual EHR as part of the NeHS. It has also been possible to evaluate the vaccination status, number of doses, type of vaccine administered, date of vaccination, any reactions to vaccines, batch number and expiry date of the vaccines, place of vaccination, and physician responsible for the vaccination.
Despite the availability of the NeHS in the country and the importance of its use as a telemedicine platform for 3P diabetes care during COVID-19 pandemics, it has been reported that the Republic of North Macedonia has one of the highest COVID-19 mortality rates worldwide. One of the reasons for the high mortality rate was related to the lack of intensive care units (ICU) capacities, i.e., a lack of necessary infrastructure for severe cases (non-invasive and invasive ventilation, central monitoring stations), and lack of experienced and competent ICU healthcare personnel. Another reason could be the lack of standardized COVID-19 national treatment protocols and training of healthcare personnel and use of different treatment approaches in COVID-19 departments across the country. Delay in massive vaccination of the population, and regional differences in adoption of vaccination have also contributed to the poor general COVID-19 outcomes, with regions reporting lower vaccination rates associated with higher hospitalization and mortality rates. Inadequate transmission control might also have contributed to the higher COVID-19 mortality rates, with lack of adequate border control (entrance in the country without negative tests or vaccination certificate), and selective and inconsistent social distancing measures across the country.
7 Conclusions and Expert Recommendation in the Frame-Work of 3P Medicine
As a conclusion, the NeHS has had a critical role as a telemedicine platform for the 3P diabetes care during COVID-19 pandemics, enabling monitoring of metabolic control and comorbidities, treatment adjustment and evaluation of COVID-19 status. The insights for the role of telemedicine in delivering 3P care derived from PwD and COVID-19 could certainly be applied to other clinical areas as well.
8 Predictive Approach
The use of NeHS as a telemedicine platform has enabled the prediction of higher risk for diabetes complications, including COVID-19 morbidity and mortality, taking into consideration the poor outcomes of COVID-19 in people with diabetes.
9 Targeted Prevention
The identified higher risk by the use of NeHS as a telemedicine platform has enabled targeted prevention of COVID-19 morbidity and mortality in people with diabetes, by monitoring the metabolic control and comorbidities, adjusting and resupplying the necessary antidiabetic treatment, and monitoring of COVID-19 status.
10 Personalized Medical Services
Concurrently with the prediction of higher risk and implementation of targeted prevention, the NeHS as a telemedicine platform has enabled personalized medical services by providing individually adjusted care in people with diabetes and COVID-19 infection, based on the data recorded in the system.
11 Outlook
Diabetes associated small vessel disease and neuro-retinal changes create a vicious cycle resulting in systemic health adverse effects such excessive mitochondrial and retinal cell damage, chronic inflammation, neovascularization, and reduced visual field. To this end, proliferative diabetic retinopathy is considered an early and independent predictor of other severe diabetic complications such as ischemic stroke. A “domino effect” is highly characteristic for the cascading diabetic complications in which specifically mitochondrial health control is clinically relevant in overall disease management. Multiomic tear fluid analysis is considered instrumental for predictive and prognostic approach [28, 29].
Abbreviations
- 3P:
-
Predictive, preventive, and personalized
- ARDS:
-
Acute respiratory distress syndrome
- BGM:
-
Blood glucose meter
- BMI:
-
Body mass index
- CGM:
-
Continuous glucose monitor
- DBP:
-
Diastolic blood pressure
- DPP-4:
-
Dipeptidyl peptidase-4
- EHR:
-
Electronic healthcare record
- GLP-1:
-
Glucagon-like peptide-1
- HbA1c:
-
Glycated hemoglobin A1c
- ICU:
-
Intensive care unit
- NeHS:
-
National e-Health System
- PwD:
-
People with diabetes
- SBP:
-
Systolic blood pressure
- SGLT2:
-
Sodium glucose cotransporter 2
- USD:
-
United States dollars
- WHO:
-
World Health Organization
References
International Diabetes Federation (2021) IDF diabetes atlas, 10th edn. International Diabetes Federation, Brussels
Duarte AA, Mohsin S, Golubnitschaja O (2018) Diabetes care in figures: current pitfalls and future scenarios. EPMA J 9:125–131
Smokovski I (2021) Managing diabetes in low income countries. Springer, Cham
Smokovski I, Milenkovic T, Trapp C, Mitov A (2015) Diabetes care in the Republic of Macedonia: challenges and opportunities. Ann Glob Health 81(6):792–802
Smokovski I, Milenkovic T, Cho HN (2018) First stratified diabetes prevalence data for the Republic of Macedonia derived from the national e-health system. Diabetes Res Clin Pract 143:179–183
International Diabetes Federation (2019) IDF diabetes atlas, 9th edn. International Diabetes Federation, Brussels
World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 15 July. https://covid19.who.int/. Accessed 15 Jul 2022
COVID-19 pandemics data. https://www.worldometers.info/coronavirus/#countries. Accessed 15 Jul 2022
Bradley S, Banach M, Alvarado N, Smokovski I, Bhaskar MMS (2022) Prevalence and impact of diabetes in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Diabetes 14(2):144
Feldman E, Savelieff GM, Hayek SS, Pennathur S, Kretzler M, Pop-Busui R (2020) COVID-19 and diabetes: a collision and collusion of two diseases. Diabetes 69(12):2549–2565
Chudasama YV, Gillies LC, Appiah K, Zaccardi F, Razieh C, Davies JM, Yates T, Khunti K (2020) Multimorbidity and SARS-CoV-2 infection in UK biobank. Diabetes Metab Syndr 14(5):775–776
Singh KA, Gillies LC, Singh R, Singh A, Chudasama Y, Coles B, Seidu S, Zaccardi F, Davies JM, Kamlesh K (2020) Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab 22:1915–1924
Barron E, Bakhai C, Kar P, Weaver A, Bradley D, Ismail H, Knighton P, Holman N, Khunti K, Sattar N, Wareham JN, Young B, Valabhji J (2020) Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol 8(10):813–822
Zhu L, She ZG, Cheng X, Qin JJ, Zhang XJ, Cai J, Lei F, Wang H, Xie J, Wang W, Li H, Zhang P, Song X, Chen X, Xiang M, Zhang C, Bai L, Xiang D, Chen MM, Liu Y, Yan Y, Liu M, Mao W, Zou J, Liu L, Chen G, Luo P, Xiao B, Zhang C, Zhang Z, Lu Z, Wang J, Lu H, Xia X, Wang D, Liao X, Peng G, Ye P, Yang J, Yuan Y, Huang X, Guo J, Zhang BH, Li H (2020) Association of Blood Glucose Control and Outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab 31(6):1068–1077
Li H, Tian S, Chen T, Cui Z, Shi N, Zhong X, Qiu K, Zhang J, Zeng T, Chen L, Zheng J (2020) Newly diagnosed diabetes is associated with a higher risk of mortality than known diabetes in hospitalized patients with COVID-19. Diabetes Obes Metab 22(10):1897–1906
Satish T, Kapoor N, Cao Y, Tapp JR, Zimmet P (2021) Proportion of newly diagnosed diabetes in COVID-19 patients: a systematic review and meta-analysis. Diabetes Obes Metab 23(3):870–874
Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A (2021) Post-covid syndrome in individuals admitted to hospital with COVID-19: retrospective cohort study. BMJ 31(372):n693
Disaster Response Task Force (2007) ADA statement of emergency and disaster preparedness: a report of the disaster response task force. Diabetes Care 30(9):2395–2398
Kocurek B, Cryar K (2018) Information for HealthCare professionals. Switching between insulin products in disaster response situations. https://diabetesdisasterresponse.org/healthcare-providers-resources. Accessed on 15 Jul 2022.
Chudasama YV, Gillies LC, Zaccardi F, Coles B, Davies JM, Seidu S, Khunti K (2020) Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr 14(5):965–967
Golubnitschaja O, Costigliola V (2012) General report & recommendations in predictive, preventive and personalized medicine 2012: white paper of the European Association for Predictive, preventive and personalized medicine. EPMA J 3(1):14
Wang LY, Cui JJ, OuYang QY, Zhan Y, Wang YM, Xu XY, Yu LL, Yin H, Wang Y, Luo CH, Guo CX, Yin JY (2021) Complex analysis of the personalized pharmacotherapy in the management of COVID-19 patients and suggestions for applications of predictive, preventive, and personalized medicine attitude. EPMA J 12:307–324
Centers for Disease Control and Prevention. COVID-19 information—people at increased risk. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed 15 Jul 2022
Smokovski I, Sadikario S, Cibisev A (2020) National eHealth System in Republic of North Macedonia—platform for preventive, predictive and personalized metabolic control in diabetes patients in Golubnitschaja O, et al. 10th Anniversary of the European association for predictive, preventive and personalized (3P) medicine—EPMA world congress supplement. EPMA J 11:2020. https://doi.org/10.1007/s13167-020-00206-1
Golubnitschaja O, Kinkorova J, Costigliola V (2014) Predictive, preventive and personalised medicine as the hardcore of ‘Horizon 2020’: EPMA position paper. EPMA J 5(1):6
Golubnitschaja O, Costigliola V (2011) European strategies in predictive, preventive and personalized medicine: highlights of the EPMA world congress 2011. EPMA J 2(4):315–332
Golubnitschaja O (2012) Time for new guidelines in advanced healthcare: the mission of the EPMA journal to promote an integrative view in predictive, preventive and personalized medicine. EPMA J 3(1):5
Kropp M, Golubnitschaja O, Mazurakova A, Koklesova L, Sargheini N, Vo TKS, de Clerck E, Polivka J Jr, Potuznik P, Polivka J, Stetkarova I, Kubatka P, Thumann G (2023) Diabetic retinopathy as the leading cause of blindness and early predictor of cascading complications-risks and mitigation. EPMA J 14(1):21–42. https://doi.org/10.1007/s13167-023-00314-8
Kropp M, De Clerck E, Vo TKS, Thumann G, Costigliola V, Golubnitschaja O (2023) Short communication: unique metabolic signature of proliferative retinopathy in the tear fluid of diabetic patients with comorbidities—preliminary data for PPPM validation. EPMA J 14(1):43–51. https://doi.org/10.1007/s13167-023-00318-4
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Smokovski, I., Srceva, M.J., Petkovska, L., Golubnitschaja, O. (2023). Critical Role of Telemedicine as a Platform for Predictive, Preventive, and Personalized Diabetes Care During the COVID-19 Pandemics. In: Podbielska, H., Kapalla, M. (eds) Predictive, Preventive, and Personalised Medicine: From Bench to Bedside. Advances in Predictive, Preventive and Personalised Medicine, vol 17. Springer, Cham. https://doi.org/10.1007/978-3-031-34884-6_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-34884-6_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-34883-9
Online ISBN: 978-3-031-34884-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)