Abstract
Malaria remains one of the world’s most important public health threats, and prompt, precise diagnosis is still an essential component of malaria control and elimination strategies, even in the postelimination phase. There are many kinds of diagnostic tools used for malaria diagnosis, including microscopy, rapid diagnostic tests, and nucleic acid amplification testing. There are advantages and disadvantages among these methods in practice. In this chapter, we introduce different techniques for the immunodiagnosis of malaria based on malarial antigens and antibodies and provide recommendations for the future research and development of novel technologies for malaria diagnosis and transmission risk evaluation in China after malaria elimination.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
With the advancement of the global malaria control process, an increasing number of countries have entered the preelimination stage or the malaria elimination stage (WHO 2021a). However, the trends have been partially stalled by COVID-19, and a significant increase in malaria cases and deaths were reported in 2020 in the World Malaria Report 2021 (WHO 2021b), where the estimated number of cases in 87 endemic countries in the world reached 241 million, and the estimated number of deaths reached 627,000. This was attributed to the disruption of medical services for malaria due to the COVID-19 pandemic. Therefore, there is still a long way to go to achieve the global eradication of malaria.
Prompt, precise diagnosis is an essential component of malaria control and elimination strategies, and parasitological testing is the only way for accurate malaria diagnosis in febrile patients (WHO 2011). It is also critical to the reliability of surveillance data and the understanding of malaria transmission. There are several methods to detect the presence of malaria parasites in the blood. The gold standard method is microscopy, although rapid diagnostic tests (RDTs) have rapidly become a primary diagnostic test in many endemic areas. Furthermore, many kinds of novel serological and molecular methods have been developed and assessed to overcome the limitations of microscopy and RDTs.
In this chapter, immunoassays for malarial antigen or antibody detection are discussed.
7.2 Immunoassays for Antigen Detection
7.2.1 Rapid Diagnostic Tests
Immunochromatographic-based diagnostic tests are already the most common diagnostic methods for malaria that detect antigens, and they are also known as rapid diagnostic tests (RDTs), which are extensively used worldwide (Wilson 2012). These methods are lateral flow assays usually in the format of cassettes, dipsticks, or cards, consisting of capture antibodies against Plasmodium-specific antigens immobilized on nitrocellulose membranes and bound to gold particles or other visually detectable markers (labeled antibodies) in the mobile phase. Antigens of the parasite are detected when the blood of a person suspected of having malaria is dropped in a membrane strip, where the liquid sample flows across. As a result, the immobilized complexes “capture antibody–antigen–labeled antibody” will be formed and can be visualized with colored lines when the blood is infected with Plasmodium (Gimenez et al. 2021).
RDTs are cost-effective and simple to operate, the results are displayed in less than 30 min and are easy to interpret, and little infrastructure and no electrical equipment are required (Mukkala et al. 2018). They are important alternatives for malaria diagnosis in areas where microscopy or other approaches are used to detect malaria parasites in the blood. Meanwhile, they are the most commonly used method for malaria diagnosis in resource-limited endemic settings. Not only are they increasingly used in malaria screening and epidemic investigations, but they are also useful tool for malaria self-diagnosis. It was reported that 3.1 billion malaria RDTs were sold globally in 2010–2020, with nearly 81% of these sales going to sub-Saharan African countries (WHO 2021b). Correspondingly, 2.2 billion RDTs were distributed by national malaria programmes, with approximately 88% in sub-Saharan Africa (WHO 2021b).
However, various factors, such as Plasmodium species, level of parasitemia, storage conditions, interpretation of the results, and the variability of the parasite antigen tested, may impact the performance of RDTs. First, RDTs are only suitable for the diagnosis of P. falciparum- and P. vivax-specific infections thus far. Currently, commercial RDTs available on the market are mostly able to detect P. falciparum-specific histidine-rich protein 2 (HRP2), P. vivax-specific lactate dehydrogenase, Plasmodium panspecific lactate dehydrogenase (pLDH), or Plasmodium spp. aldolase. However, their sensitivity to detect nonfalciparum spp. is low overall (Yerlikaya et al. 2018), and even for the detection of P. vivax, the sensitivity of the most frequently used RDTs was 75–87% compared to microscopy (Abba et al. 2014). Moreover, no RDTs can specifically detect P. ovale, P. malariae, or P. knowlesi, even with high sensitivity. Second, the performance of RDTs is also limited to low parasitemia, and they usually have the capability of detecting >100 parasites/μl. It is worth noting that the presence of a low number of parasites is relevant, especially for pregnant women and children under the age of 5 years, who are the most vulnerable populations. Third, humidity and extreme temperatures tend to easily affect RDT performance, and persistence of antigens in the patient’s blood circulation after treatment may lead to false positives (Yan et al. 2013). Fourth, interpretation of results can be confusing when testing for combinations of antigens, especially when control and Plasmodium panspecific lines are displayed together. Fifth, the emergence and spread of PfHRP2/3-deleted strains in countries where malaria is endemic results in the increasing occurrence of false negativity in symptomatic patients who are infected with variants of P. falciparum that do not express HRP2 (Cheng et al. 2014). It was reported that PfLDH-based RDTs could be used for P. falciparum detection in PfHRP2-deleted samples at high density but vary greatly at lower densities (Gatton et al. 2020).
Therefore, quality-assured RDTs can be important for case diagnosis and case management, and users such as clinicians and laboratory personnel must be familiar with the RDTs used in their facilities and their associated performance characteristics, while the causes of fever in nonmalarial patients should be followed up and properly managed appropriately. Consequently, the minimum procurement criteria were recommended by the WHO Malaria Policy Advisory Committee, and independent global quality assessment programmes for malaria RDT lots have been carried out by the WHO in collaboration with other Malaria programmes, such as the Foundation for Innovative New Diagnostics (FIND), and coordinated the WHO Malaria RDT Product Testing Programme (Cunningham et al. 2019). In detail, any RDT should be fast and independent of the device, available to those who need it, and require minimal training. Furthermore, their sensitivity and specificity were recommended to reach at least a 75% “panel detection score” at 200 parasites/μL, with a false positive rate of less than 10% and an invalid rate of <5%, for the detection of P. falciparum and, if applicable for P. vivax, in all transmission settings (https://www.who.int/teams/global-malaria-programme/case-management/diagnosis/rapid-diagnostic-tests). To date, eight rounds of WHO product testing of malaria RDTs have been completed since 2008, and the summary results of malaria RDT performance have been published (Malaria Rapid Diagnostic Test Performance Summary results of WHO product testing of malaria RDTs: rounds 1–8 (2008–2018)) (Cunningham et al. 2019).
Given the significantly lower sensitivities for nonfalciparum species mainly due to the lower parasitemia and the importance for the detection of low levels of parasitemia, malaria RDTs used for malaria diagnosis should be confirmed by other laboratory tests (e.g., blood film examination and nucleic acid amplification test). Moreover, high-sensitivity RDTs for P. falciparum, such as Alere Malaria Ag P. f (Alere) and NxTek Eliminate Malaria P. f (Abbott), have been developed and tested for their ability to detect malaria infection in asymptomatic individuals or individuals with very low parasitemia, and this might be a good strategy to better detect malaria parasites in the future, especially in the low-transmission setting or malaria-eliminated areas. In addition, there are also real-world implications for the discovery of new malaria RDT candidate antigens. One is Plasmodium glutamate dehydrogenase (pGDH), which has come to the attention of researchers; it is specific to Plasmodium, but the similarity among different species is so high that it is difficult to identify different Plasmodium spp. (Ahmad et al. 2019; Krishna et al. 2015). The other is GAPDH, which includes unique regions that make it possible to raise antibodies against pan-Plasmodium specificity and to detect P. falciparum or rodent malaria parasites specifically, but other species-specific detection for GAPDH has not been reported (Krause et al. 2017). Therefore, more work is needed in the future to determine whether pGDH-based or GAPDH-based RDTs can be used to detect malaria parasites.
7.2.2 Other Laboratory Assays for the Detection of Malaria Parasite Antigens
The development of assays used in the laboratory for malaria antigen testing has greatly benefited from the significant advances in the development of stable hybridomas as sources of monoclonal antibodies and improvements in immunoassay platforms throughout the decades (Plucinski et al. 2021). For example, a colorimetric sandwich ELISA has the capacity to detect HRP2 at levels of <100 pg/ml, with assay wells showing the intensity of color proportional to the amount of antigen in the sample (Jang et al. 2018). Other multiplexed detection systems for malaria diagnosis using different panels of PfHRP2 and panmalarial antigen targets to differentiate species in malaria infection have been developed, such as the Luminex xMAP bead-based assay (Martianez-Vendrell et al. 2020) and the Quansys Q-Plex Human Malaria assay (Jang et al. 2019). For instance, the former assay can screen P. falciparum with simultaneous analysis of glutamate-rich protein (GLURP) antigens R0 and R2, merozoite surface protein 3 (MSP3), MSP1 hybrid, and apical merozoite antigen 1 (AMA1) in blood from a person suspected of having malaria infection, according to the fluorescence intensity signals for different antigen targets for samples (Rogier et al. 2017). Furthermore, these assays are usually sensitive to detect malaria parasite antigens at low concentrations, plus their operator independence and reliability; thus, they have routine clinical application for malaria diagnosis. In addition, some promising laboratory tests of nontraditional immunoassays and aptamer-based antigen detection systems with good sensitivity and specificity have been developed (Frith et al. 2018; Mu et al. 2017; Hemben et al. 2017; Paul et al. 2017).
7.3 Immunoassays for Antibody Detection
Although serologic testing is generally not recommended for the routine diagnosis of malaria, it is still used for some cases, such as febrile patients traveling to malaria-endemic areas with repeatedly negative blood smears and cases of suspected topical splenomegaly syndrome. Moreover, it is also used to screen blood donors and evaluate donors with suspected cases of transfusion-transmitted malaria. Additionally, it is used for detecting malarial antibodies in seroepidemiological studies for monitoring malaria control and elimination under specific and predictable requirements. Thus, the ideal test should be high throughput, easy to operate, easy to interpret, and quick to display the results. Most of the tests available are either immunofluorescence assays or enzyme immunoassays and can be performed on serum or plasma.
7.3.1 Complement Fixation Test
The complement fixation test (CFT) is a classical laboratory testing and one of the earliest methods for malarial antibody detection, which is more sensitive than microscopy of peripheral blood smears for detecting current infections (Thomson 1918). The test is based on the capacity of complement, a group of heat-labile proteins present in the plasma, to bind to antigen–antibody complexes. When the complexes are present on the surface of red blood cells, complement causes their lysis, which can be measured photospectronically. In practice, heating the serum first leads to the destruction of complement, and then the serum is mixed with the appropriate pathogenic antigen and incubated. Next, exogenous complement is added into the mixture when the antigen–antibody complexes are formed. This complement then binds to the complexes and is “fixed,” no longer able to cause lysis of the added indicator red blood cells. The test measures certain types of antibodies (mainly IgG antibodies) that occur only during the acute phase of pathogenic infection and has been widely used as an alternative for malaria diagnosis. However, this method is less sensitive and more complex, as well as labor intensive; thus, it has been increasingly replaced by modern immunoassays such as enzyme-linked immunosorbent assay (ELISA) (Wilson et al. 1975; Drakeley and Cook 2009).
7.3.2 Indirect Hemagglutination Assay
Indirect hemagglutination assays (IHAs) have been developed and optimized continuously and used for detecting malarial antibodies. This method initially used tanned formolized sheep red blood cells sensitized with an antigen prepared from erythrocytic Plasmodium released from the red blood cells (Bray 1966). For instance, it was reported that soluble antigens prepared from P. falciparum and P. vivax could attach to aldehyde-fixed type “O” erythrocytes and detect antibodies in more than 91% of infections with homologous Plasmodium species and 72–76% of infections caused by heterologous species using the IHA (Mathews et al. 1975). Sera are tested by serial dilution but are difficult to standardize, resulting in limitations of cross-comparison of data from different research groups.
7.3.3 Immunofluorescence Antibody Test
The Immunofluorescence Antibody Test (IFAT) was extensively used for malaria seroepidemiology (Drakeley and Cook 2009). First, the whole parasitized red blood cells with the antigen of interest were fixed on a microscope slide, and then the sera sample was incubated on the slide. Finally, the resulting fluorescence according to the binding of a secondary antibody coupled with a fluorescent compound and the bound antibodies in the serum was examined using a specialized microscope. Compared with other methods, it is easier to prepare whole malarial parasite antigens, and these antigens are more stable than extracts of soluble antigens (Ambroise-Thomas 1976). However, this method is also difficult to standardize, and the fluorescence is subjectively determined by visual examination. Moreover, the sensitivity is limited due to the antigens used not being from the target malarial parasites, although P. falciparum culture became available as a stable source of antigen. In addition, it is also labor intensive for slide preparation, and the derived antibody responses are not specific since all parasitized red blood cells are used (Drakeley and Cook 2009).
7.3.4 Enzyme-Linked Immunosorbent Assay
The principle of Enzyme-Linked Immunosorbent Assay (ELISA) is similar to that of IFA, but the antigens of ELISA are coated on the microtiter plate instead of the glass slide of IFA, and the antigens are often single recombinant proteins. The bound antibodies are detected with a secondary antibody linked with an enzyme, and color change or fluorescence is quantified by a spectrophotometer if the bound enzyme is present in the well. Furthermore, it is relatively cheap and easy to perform and generates objective results. Additionally, it is also a high-throughput, standardizable test that can be compared from different laboratories with robust results (Drakeley and Cook 2009; Esposito et al. 1990).
7.3.5 Protein Microarray
Protein microarray is similar to ELISA, but recombinant proteins are bound to a microarray slide in nanogram quantities and screen thousands of antigens simultaneously and have a greater dynamic detection range than ELISA; thus, it is much more suitable for antigen discovery and broad assessments of the immune response to malaria. However, it is not available for field investigation due to many factors, such as equipment requirements and signal variation between slides (Drakeley and Cook 2009; Doolan et al. 2009; Gray et al. 2007).
7.3.6 Cytometric Bead Array
Flow cytometric bead-based Cytometric Bead Array (CBA) can measure the response to multiple antigens in biological and environmental samples simultaneously. There are several advantages: it allows the assessment of multiple analytes in a single sample, collects data with minimal sample size, is reproducible, and can be compared with results from previous experiments and results from other assays, as well as evaluate multiple samples faster. There were different cytokine/chemokine kits, two flow cytometry-based (eBioscience® FlowCytomix™ and BD™ Cytometric Bead Array Human Enhanced Sensitivity) and four Luminex®-based (Invitrogen™ Human Cytokine 25-Plex Panel, Invitrogen™ Human Cytokine Magnetic 30-Plex Panel, Bio-Rad® Bio-Plex Pro™ Human Cytokine Plex Assay, and Millipore™ MILLIPLEX® MAP Plex Kit) kits used to quantify and compare cytokine and chemokine responses in culture supernatants from P. falciparum stimulations (Moncunill et al. 2013). Moreover, the protein levels of the cytokines IL-2, IL-6, IL-10, IL-17, IFN-γ, and TNF in the serum, frontal cortex, and hippocampus of controls and P. berghei-infected mice treated or not treated with artesunate were determined using a CBA kit (Miranda et al. 2013).
7.3.7 Engineered Yeast Agglutination Assay
A new agglutination assay named the Engineered Yeast Agglutination Assay (Cruz et al. 2022) was developed using modified Saccharomyces cerevisiae cells as antigen-displaying bead-like particles to capture malaria antibodies. The epidermal growth factor-1-like domain (EGF1) of P. falciparum merozoite surface protein-1 (PfMSP-119) was displayed on the yeast surface and shown to bind antimalarial antibodies. After mixing with a second yeast strain showing the Z domain of Protein A from Staphylococcus aureus and settling in a round-bottomed well, the yeast produced a visually distinctive agglutination test result. This method is relatively inexpensive and may have the potential for regions seeking malaria surveillance information to guide their elimination programmes.
7.4 Challenges and Perspectives
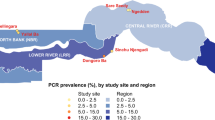
China officially achieved the elimination of malaria (Zhou 2021), but malaria remains one of the world’s most important public health threats, and China also faces numerous challenges in the prevention of malaria re-establishment of transmission (Yin et al. 2022b). For instance, a large number of imported malaria cases continue to be reported per year, including border malaria cases, especially at the China–Myanmar border. Moreover, there are potentially unknown infections, including asymptomatic infections and P. falciparum with HRP2/3 gene deletions, which are easily missed. Currently, malaria microscopy and RDTs are still the main methods for malaria diagnosis in the first line, but microscopy competency is difficult to maintain, and there is a shortage of sensitive species-specific RDTs except for P. falciparum and P. vivax in China (Yin et al. 2022a). Moreover, there are no suitable kits for malaria seroepidemiology for the evaluation of malaria transmission after malaria elimination. Therefore, it is still critical to strengthen the detection capacity to meet the timely detection of these sources of infection in the postelimination phase, which will contribute to the prevention of malaria re-establishment in areas with malaria transmission environments.
First, the research and development of improved diagnostic tools, including antigen detection and antibody detection for malaria diagnosis, need to be accelerated, and they can detect asymptomatic infections of very low parasite densities. Moreover, they should be cost-effective, easy to operate and interpret, and thereby suitable for mass screening and surveillance. Additionally, it is recommended to integrate malaria testing into diagnostics for other febrile diseases in health systems after malaria elimination.
Second, more antigen targets should be identified for rapid malaria diagnosis, especially for species-specific identification, not only for P. falciparum and P. vivax or pan-Plasmodium. Furthermore, it is best for the new targets to solve the challenge in P. falciparum with HRP2/3 gene deletions simultaneously.
Third, serologic methods are valuable tools for the measurement of transmission, especially in the postelimination phase. To date, there are many different serologic methods for the detection of malarial antibodies, but the results from different methods cannot be compared. Therefore, method standardization, including antigen standardization, is an important area for further research.
Fourth, noninvasive testing in samples such as saliva or other bodily fluids rather than currently the most commonly used blood deserves further exploration.
In conclusion, although traditional techniques, such as microscopy and RDTs, are still being used in the field, the exploration and field implementation of advanced technologies, including immunoassays for malaria diagnosis, are still needed in the postelimination phase in China. Not only for the detection of the presence of malaria parasites in the blood of the suspected individuals but also to evaluate the transmission risk through seroepidemiology. It will continue to maintain and strengthen the surveillance and response of imported malaria and contribute to the prevention of malaria re-establishment of transmission.
References
Abba K, Kirkham AJ, Olliaro PL, Deeks JJ, Donegan S, Garner P, Takwoingi Y (2014) Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or plasmodium vivax malaria in endemic countries. Cochrane Database Syst Rev 12:CD011431
Ahmad A, Verma AK, Krishna S, Sharma A, Singh N, Bharti PK (2019) Plasmodium falciparum glutamate dehydrogenase is genetically conserved across eight malaria endemic states of India: exploring new avenues of malaria elimination. PLoS One 14(6):e0218210
Ambroise-Thomas P (1976) Immunofluorescence in the diagnosis, therapeutic follow-up and sero-epidemiological studies of some parasitic diseases. Trans R Soc Trop Med Hyg 70(2):107–112
Bray RS (1966) el-Nahal HM: indirect haemagglutination test for malarial antibody. Nature 212(5057):83
Cheng Q, Gatton ML, Barnwell J, Chiodini P, McCarthy J, Bell D, Cunningham J (2014) Plasmodium falciparum parasites lacking histidine-rich protein 2 and 3: a review and recommendations for accurate reporting. Malar J 13:283
Cruz CJG, Kil R, Wong S, Dacquay LC, Mirano-Bascos D, Rivera PT, McMillen DR (2022) Malarial antibody detection with an engineered yeast agglutination assay. ACS Synth Biol 11(9):2938–2946
Cunningham J, Jones S, Gatton ML, Barnwell JW, Cheng Q, Chiodini PL, Glenn J, Incardona S, Kosack C, Luchavez J et al (2019) A review of the WHO malaria rapid diagnostic test product testing programme (2008-2018): performance, procurement and policy. Malar J 18(1):387
Doolan DL, Dobano C, Baird JK (2009) Acquired immunity to malaria. Clin Microbiol Rev 22(1):13–36
Drakeley C, Cook J (2009) Chapter 5. Potential contribution of sero-epidemiological analysis for monitoring malaria control and elimination: historical and current perspectives. Adv Parasitol 69:299–352
Esposito F, Fabrizi P, Provvedi A, Tarli P, Habluetzel A, Lombardi S (1990) Evaluation of an ELISA kit for epidemiological detection of antibodies to plasmodium falciparum sporozoites in human sera and bloodspot eluates. Acta Trop 47(1):1–10
Frith KA, Fogel R, Goldring JPD, Krause RGE, Khati M, Hoppe H, Cromhout ME, Jiwaji M, Limson JL (2018) Towards development of aptamers that specifically bind to lactate dehydrogenase of plasmodium falciparum through epitopic targeting. Malar J 17(1):191
Gatton ML, Chaudhry A, Glenn J, Wilson S, Ah Y, Kong A, Ord RL, Rees-Channer RR, Chiodini P, Incardona S et al (2020) Impact of plasmodium falciparum gene deletions on malaria rapid diagnostic test performance. Malar J 19(1):392
Gimenez AM, Marques RF, Regiart M, Bargieri DY (2021) Diagnostic methods for non-falciparum malaria. Front Cell Infect Microbiol 11:681063
Gray JC, Corran PH, Mangia E, Gaunt MW, Li Q, Tetteh KK, Polley SD, Conway DJ, Holder AA, Bacarese-Hamilton T et al (2007) Profiling the antibody immune response against blood stage malaria vaccine candidates. Clin Chem 53(7):1244–1253
Hemben A, Ashley J, Tothill IE (2017) Development of an immunosensor for PfHRP 2 as a biomarker for malaria detection. Biosensors 7(3):28
Jang IK, Das S, Barney RS, Peck RB, Rashid A, Proux S, Arinaitwe E, Rek J, Murphy M, Bowers K et al (2018) A new highly sensitive enzyme-linked immunosorbent assay for the detection of plasmodium falciparum histidine-rich protein 2 in whole blood. Malar J 17(1):403
Jang IK, Tyler A, Lyman C, Kahn M, Kalnoky M, Rek JC, Arinaitwe E, Adrama H, Murphy M, Imwong M et al (2019) Simultaneous quantification of plasmodium antigens and host factor C-reactive protein in asymptomatic individuals with confirmed malaria by use of a novel multiplex immunoassay. J Clin Microbiol 57(1):e00948
Krause RGE, Hurdayal R, Choveaux D, Przyborski JM, Coetzer THT, Goldring JPD (2017) Plasmodium glyceraldehyde-3-phosphate dehydrogenase: a potential malaria diagnostic target. Exp Parasitol 179:7–19
Krishna S, Bharti PK, Chandel HS, Ahmad A, Kumar R, Singh PP, Singh MP, Singh N (2015) Detection of mixed infections with plasmodium spp. by PCR, India, 2014. Emerg Infect Dis 21(10):1853–1857
Martianez-Vendrell X, Jimenez A, Vasquez A, Campillo A, Incardona S, Gonzalez R, Gamboa D, Torres K, Oyibo W, Faye B et al (2020) Quantification of malaria antigens PfHRP2 and pLDH by quantitative suspension array technology in whole blood, dried blood spot and plasma. Malar J 19(1):12
Mathews HM, Fried JA, Kagan IG (1975) The indirect hemagglutination test for malaria. Evaluation of antigens prepared from plasmodium falciparum and plasmodium vivax. Am J Trop Med Hyg 24(3):417–421
Miranda AS, Brant F, Rocha NP, Cisalpino D, Rodrigues DH, Souza DG, Machado FS, Rachid MA, Teixeira AL Jr, Campos AC (2013) Further evidence for an anti-inflammatory role of artesunate in experimental cerebral malaria. Malar J 12:388
Moncunill G, Aponte JJ, Nhabomba AJ, Dobano C (2013) Performance of multiplex commercial kits to quantify cytokine and chemokine responses in culture supernatants from plasmodium falciparum stimulations. PLoS One 8(1):e52587
Mu J, Andersen JF, Valenzuela JG, Wellems TE (2017) High-sensitivity assays for plasmodium falciparum infection by Immuno-polymerase chain reaction detection of PfIDEh and PfLDH antigens. J Infect Dis 216(6):713–722
Mukkala AN, Kwan J, Lau R, Harris D, Kain D, Boggild AK (2018) An update on malaria rapid diagnostic tests. Curr Infect Dis Rep 20(12):49
Paul KB, Panigrahi AK, Singh V, Singh SG (2017) A multi-walled carbon nanotube-zinc oxide nanofiber based flexible chemiresistive biosensor for malaria biomarker detection. Analyst 142(12):2128–2135
Plucinski M, Aidoo M, Rogier E (2021) Laboratory detection of malaria antigens: a strong tool for malaria research, diagnosis, and epidemiology. Clin Microbiol Rev 34(3):e0025020
Rogier E, Plucinski M, Lucchi N, Mace K, Chang M, Lemoine JF, Candrinho B, Colborn J, Dimbu R, Fortes F et al (2017) Bead-based immunoassay allows sub-picogram detection of histidine-rich protein 2 from plasmodium falciparum and estimates reliability of malaria rapid diagnostic tests. PLoS One 12(2):e0172139
Thomson JG (1918) Preliminary note on the complement deviation in cases of malaria: a new aid to diagnosis. Br Med J 2(3023):628–629
WHO (2011) Universal access to malaria diagnostic testing: an operational manual: World Health Organization
WHO (2021a) Zeroing in on malaria elimination: final report of the E-2020 initiative: World Health Organization
WHO (2021b) World Malaria Report 2021: World Health Organization
Wilson ML (2012) Malaria rapid diagnostic tests. Clin Infect Dis 54(11):1637–1641
Wilson M, Fife EH Jr, Mathews HM, Sulzer AJ (1975) Comparison of the complement fixation, indirect immunofluorescence, and indirect hemagglutination tests for malaria. Am J Trop Med Hyg 24(5):755–759
Yan J, Li N, Wei X, Li P, Zhao Z, Wang L, Li S, Li X, Wang Y, Li S et al (2013) Performance of two rapid diagnostic tests for malaria diagnosis at the China-Myanmar border area. Malar J 12:73
Yerlikaya S, Campillo A, Gonzalez IJ (2018) A systematic review: performance of rapid diagnostic tests for the detection of plasmodium knowlesi, plasmodium malariae, and plasmodium ovale Monoinfections in human blood. J Infect Dis 218(2):265–276
Yin J, Li M, Yan H, Zhou S, Xia Z (2022a) Laboratory diagnosis for malaria in the elimination phase in China: efforts and challenges. Front Med 16(1):10–16
Yin J, Yan H, Li M (2022b) Prompt and precise identification of various sources of infection in response to the prevention of malaria re-establishment in China. Infect Dis Poverty 11(1):45
Zhou XN (2021) China declared malaria-free: a milestone in the world malaria eradication and Chinese public health. Infect Dis Poverty 10(1):98
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yin, J., Yan, H., Li, J. (2023). Immunodiagonsis of Malaria. In: Mehlhorn, H., Li, J., Wu, K. (eds) Malaria Control and Elimination in China. Parasitology Research Monographs, vol 18. Springer, Cham. https://doi.org/10.1007/978-3-031-32902-9_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-32902-9_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-32901-2
Online ISBN: 978-3-031-32902-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)