Abstract
Purpose of Review
Modern advances in malaria rapid diagnostic test (RDT) technology have increased demand for low-cost, easy-to-use assays in areas endemic for malaria. Substantial developments in diagnostic sensitivity and specificity, improvements in non-falciparum RDTs, and novel biotechnological innovations are gradually aligning the performance of RDTs with reference-level diagnostics including PCR and expert microscopy gold standards.
Recent Findings
Trends have emerged in recent malaria RDT literature: (1) improvements in the sensitivity and specificity of RDTs for Plasmodium falciparum diagnosis, making them comparable to expert microscopic examination; (2) reduced false-positive and false-negative reactions with novel antibody development; (3) improved sensitivity and specificity capabilities of Plasmodium vivax-specific RDTs; (4) developing RDTs for co-endemic mixed infection differentiation; (5) significant improvements of RDTs for Plasmodium knowlesi; (6) a global push towards assessing and confronting the growing concerns of widespread pfhrp2 gene deletions; and (7) original innovation in loop-mediated isothermal amplification (LAMP) biotechnological RDT-like platforms that demonstrate promising performance characteristics for P. falciparum, P. vivax, and P. knowlesi infections.
Summary
The past 5 years have been characterized by increasing demand for malaria RDTs, translating into meaningful improvements in performance and novel biotechnological innovation. Future work should facilitate the development of improved RDT platforms for Plasmodium ovale, P. knowlesi, and Plasmodium malariae, and surmount the issue of pfhrp2 gene deletions, while maintaining comparable performance to both PCR and expert microscopy reference standards.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria is a mosquito-borne parasitic disease caused by protozoans of the Plasmodium genus and transmitted by the female Anopheles mosquito. To date, six species have been found to cause illness in humans: Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, and Plasmodium malariae, along with the simian malaria species Plasmodium knowlesi and, more recently, Plasmodium simium [1,2,3]. Malaria can cause a spectrum of disease ranging from asymptomatic parasitemia to uncomplicated malaria (characterized by flu-like symptoms, fever, sweats, general malaise, chills, headaches, nausea, vomiting body aches), to severe malaria (characterized by infection of vital organs leading to dysfunction, coma, pulmonary edema, shock, and death) [1,2,3,4,5].
Despite recent progresses, malaria remains one of the most important diseases affecting human health. Nearly half of the world’s population is at risk for malaria infection [1] and in 2016, there were an estimated 216 million cases (95% CI: 196–263 million) of malaria with half a million deaths globally; the majority being children less than 5 years of age. Ninety percent of cases were in the WHO African Region with P. falciparum being the most prevalent species and accounting for the majority of malaria deaths [1]. Between 2013 and 2015, almost 31% of suspected clinical cases of malaria in sub-Saharan Africa were left unconfirmed, likely resulting in over-usage of antimalarial drugs [1, 6]. The ability to diagnose malaria quickly and species-specifically is crucial for selection of effective therapy and, in turn, good prognosis.
Malaria is primarily diagnosed by three categories of tools: expert light microscopy (examination of Giemsa- or Wright-stained thick and thin blood films); immunochromatographic test (ICT)—also referred to as rapid diagnostic test (RDT) or rapid antigen test (RAT); and nucleic acid amplification with end-point polymerase chain reaction (PCR) or real-time quantitative polymerase chain reaction (qPCR) [1,2,3]. Expert light microscopy is the oldest of these diagnostic methods and has been long considered to be the gold standard. PCR has been emerging as another conceivable gold standard with greater sensitivity and specificity in diagnosis and speciation [2]. Lack of experienced personnel and high overhead costs can make microscopy and PCR difficult to utilize, respectively, especially in low resource settings such as sub-Saharan Africa, where there is a high burden of malaria. Global attrition of, and lack of training programs to replace expert microscopists, in the context of recent dramatic improvements in malaria control leading to fewer true positive smears being read at individual laboratories, have also contributed to occasional reports of extremely poor performance of “expert” microscopy [7]. RDTs are rapid, have become increasingly inexpensive, and do not require overhead investment (Table 1). As a result, they are of increasing utility in both endemic and traveler populations as alternatives or supplementary instruments for malaria diagnostics [1, 2, 8].
RDTs are ready-to-use assays that utilize mono- or polyclonal antibodies to detect malaria-specific antigens in blood samples via a colorimetric transformation on nitrocellulose strips [4,5,6]. The main five antigens malaria RDTs currently detect include: P. falciparum-specific histidine-rich protein-2 (PfHRP2) and P. falciparum-specific lactate dehydrogenase (Pf-pLDH), P. vivax-specific lactate dehydrogenase (Pv-pLDH), as well as, pan-pLDH and pan-aldolase, both of which are common to all human-infecting Plasmodium species [2,3,4,5]. Currently, there are no species-specific RDTs for P. malariae, P. ovale, and P. knowlesi.
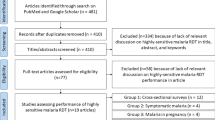
This review encompasses selected and noteworthy literature from the past 5 years surrounding development, testing, and performance of malaria RDTs for the four human malaria species as well as P. knowlesi. Strengths, limitations, species-specific advances, new technologies, and future challenges in malaria RDTs are illuminated.
Strengths of Malaria RDTs
Malaria RDTs provide an easy-to-use, relatively inexpensive, and low-expertise methodology to quickly diagnose mostly P. falciparum, and more recently, P. vivax infections within minutes [1,2,3,4,5,6,7, 9, 10, 11•]. Whereas expert personnel with substantial training are required for both PCR-based and microscopic diagnosis, RDTs can be used with less than a few minutes of training and in low-resource settings, and are thus an invaluable tool in the arsenal to fight malaria [2, 3]. The utility of microscopy and PCR are limited in resource-constrained areas by old or non-existent equipment and lack of reliable power, compared to RDTs, which require no electrical supply, special training, or bulky and costly laboratory equipment [3].
Performance characteristics are also a strength of existing RDTs. WHO has both a yearly RDT product-testing program for quality assurance [6], and general guidelines for RDT procurement [10]. WHO’s selection criteria for RDT procurement are threefold: (a) the panel detection score must be at least 75% at 200 parasites/μL for both P. falciparum and P. vivax; (b) the false-positive rate should be less than 10%; and (c) the invalid rate should be less than 5% [10]. Estimates from meta-analyses place sensitivities and specificities for PfHRP2-detecting RDTs at an average of 95.0% (95% CI: 93.5–96.2%) and 95.2% (95% CI: 93.4–99.4%), respectively [3]. Pf-pLDH-detecting RDTs have marginally lower average sensitivities at 93.2% (95% CI: 88.0–96.2%) but higher specificities of 98.5% (95% CI: 96.7–99.4%) [3]. Pv-pLDH RDTs also have similar pooled sensitivity of 95% (95% CI: 86–99%) and specificity of 99% (95% CI: 99–100%) compared to reference microscopy in endemic settings [11•]. However, when a subset of Pv-pLDH-detecting RDT studies used PCR as the reference, both sensitivities and specificities dropped to 59–77% and 97–100%, respectively [11•]. This is likely secondary to the inherent subjectivity of microscopy, while PCR is more objective by design. Using PCR as the reference standard may derive discrepant results as the number of RDT false negatives may be higher in this particular subset due to the superior sensitivity of PCR, which has a parasite density threshold of detection of 5 parasites/uL (0.0001% parasitemia) compared to light microscopic examination (50–100 parasites/uL; 0.001–0.002% parasitemia), and RDT (100 parasites/uL; 0.002% parasitemia) [2].
Variability in usage, storage, and end-user standardization have resulted in a range of reported RDT sensitivities for P. falciparum from 88.0–100% (for all antigens) [2]. RDT sensitivities for P. vivax range between 77.4–97.2%, at parasitemia greater than 500 parasites/μL (~ 0.01% parasitemia) [4, 5], although recent literature has shown increased sensitivities and specificities [1]. Diagnostic sensitivities of RDT for P. ovale and P. malariae remain poor ranging from 5.5 t o86.7% and 21.4 to 45.2%, respectively [6]. Effective P. knowlesi-specific RDTs are commercially unavailable; however, other DNA-based RDT technologies are in development with promising initial results (reviewed here [12•]). Sensitivities universally decrease for all RDTs at low parasitemia (< 100 parasites/μL) [2]. Expert reference-level microscopy performs at a sensitivity of 86.2% and specificity of 99.6%, when using qPCR as the comparator standard [11•]. qPCR sensitivity is 99.4% and specificity is 90.9%, when compared to expert reference-level microscopy [11•]. These numbers will naturally fluctuate according to the training, resources, and laboratory conditions under which malaria diagnosticians perform.
Limitations of Malaria RDTs
Despite their potential widespread utility, RDTs have intrinsic limitations that hinder their performance in a variety of contexts. For example, among 53 cases of imported malaria to London where RDT was performed, discordance with microscopy occurred in two (3.8%): in one case, a microscopically confirmed P. vivax was misclassified as P. falciparum, while in another, RDT was negative with P. falciparum parasitemia of 0.1% [13]. The possible explanations for such phenomena are discussed below. RDTs are principally designed for the detection P. falciparum, and sensitivity tends to be lower for P. vivax and poorer still for P. malariae, P. ovale, and P. knowlesi, for which there can also be false-positive and false-negative reactions [4, 5].
False negative PfHRP2 RDT reactions occur largely due to heterogeneity in or deletion of the HRP2 gene; HRP2 being poorly expressed and therefore leading to low detectability in blood; and prozone effect, whereby an excess of antigens (due to high parasitemia) or antibodies blocks detection in the RDT [2,3,4,5]. False positive reactions, reflecting an absence of clinically relevant asexual parasitemia, occur mostly due to the presence of autoantibodies (such as rheumatoid factor); persistent post-treatment HRP2 antigenemia (median persistence = 35 days) [14•]; the presence of circulating, but clinically irrelevant, P. falciparum gametocytes [15]; cross-reactivity with other Plasmodium species and other infections such as: trypanosomiasis, schistosomiasis, leishmaniasis, toxoplasmosis, dengue, hepatitis C, and tuberculosis [2, 4, 5, 9, 11•, 12•, 14•]. In a survival analysis of diagnostic assays for P. falciparum malaria, it was demonstrated that microscopy remains the only reliable method to differentiate asexual parasitemia from post-treatment circulating antigens and DNA [14•].
WHO recommends lab training to be advantageous to standardization of RDT interpretation in endemic areas [3]. Storage and proper execution of manufacturer instructions is crucial to reduce lot-to-lot variation in performance of RDT kits [8, 10]. Storage conditions should reflect both temperature and humidity level considerations [2, 3].
Performance limitations of RDTs arise with low parasitemia (i.e., less than 200 parasites/μL) [2]. Interpretation of RDTs should be done with extreme care in the cases of children and pregnant women because these patient populations are more likely to manifest symptoms at low parasite loads [10, 16]. The ability to diagnose malaria in children under 5 years of age is of particular interest in RDT development.
RDTs are unable to differentiate between viable RBC-infecting asexual parasites, non-RBC infecting, clinically irrelevant gametocytes, and non-viable parasite components and antigens. Inspection of thick and thin blood smears by microscopy is the only method to reliably differentiate between clinically relevant asexual parasitemia and clinically irrelevant isolated gametocytemia [15, 16]. RDTs, by nature, are also qualitative, rather than providing a quantitative result, which is required for appropriate treatment stratification [17•].
Developments in RDTs for P. falciparum and P. vivax
RDTs for P. falciparum are well-established, and their utility is well-tested by both the WHO and reference laboratories. The challenge is to further improve their sensitivity and specificity while incorporating the advantages of expert microscopy and PCR, such as quantification of parasitemia, which will enable these point-of-care diagnostics to supplant the more complex, expensive, and labor-intensive methodologies. Recent years have shown some steps towards this with improvements in P. falciparum and P. vivax RDT sensitivities and specificities [6].
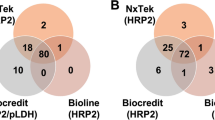
Where definitive microscopic diagnosis is impossible to access, it is logistically safe and even preferred to use reliable, well-tested P. falciparum and P. vivax RDTs [18]. Diagnostic performance testing, against thick film microscopy, of the CareStart Malaria Pf/Pv Combo Test in an endemic region of Northwest Ethiopia demonstrates the recent large gains in sensitivity and specificity of RDTs for P. vivax infections: 99.7% (95% CI: 97.1–100%) sensitivity and 97.8% (95% CI: 94.7–99.1%) specificity for P. falciparum, as well as 99.9% (95% CI: 98.8–100%) sensitivity and 99.9% (95% CI: 98.8–100%) specificity for P. vivax [18]. Of note, RDTs for P. falciparum and P. vivax are becoming increasingly cost-effective, sustainable, with minimal need for technical expertise, while at the same time delivering results comparable to expert reference microscopy [18]. This result, however, is product-specific, making WHO procurement standardization all the more necessary and useful [10]. Products that test for pan-pLDH for example, are inherently non-specific, making them disadvantageous for the diagnosis of travel acquired malaria or possible co-infections [19]. In contrast, three-band RDTs with PfHRP2 and pLDH (instead of two-band usually with only PfHRP2) have been shown to noticeably increase specificity in P. falciparum malaria, particularly in Ugandan children who are prone to manifest symptoms of low parasitemia [20]. Maintaining standardization becomes increasingly important and potentially more difficult in low-resource settings that have limited regulations or point-of-care accreditation standards.
Regions where P. falciparum and P. vivax are co-endemic and thus are more likely to cause co-infections are particular challenges for RDTs. Detection of P. falciparum and P. vivax co-infections can be difficult even by expert microscopy, emphasizing the need for enhanced diagnostics worldwide. In a study by Ehtesham and colleagues, light microscopy had a sensitivity of 16.6% (95% CI: 3–49.1%) for mixed-species infections [21•]. Conversely, the CareStart Pv/Pf Combo kit RDT had a sensitivity of 58.3% (95% CI: 28.5–83.5%), referencing to nested PCR, highlighting the usefulness of RDTs in specifically differentiating mixed infections in endemic contexts [21•]. Despite an overall sensitivity that is far below the required standard, particularly for RDT use in highly-endemic P. falciparum areas such as West Africa, RDTs were more diagnostically effective than microscopy in this mixed-infection study [21•].
Development of novel monoclonal antibodies (mAb) for more specific and sensitive detection of P. vivax by RDTs is revolutionizing malaria diagnostics [22]. Usage of both LDH and aldolase specific antigens is likely to improve P. vivax diagnosis, especially with usage of the novel aldolase mAb:PvALDO [22]. A study by Dzakah and colleagues demonstrated that when aldolase or LDH mAb RDTs are used independently, they performed differently in different samples, and hence there would be a high risk of misdiagnosis [22]. Specifically, these authors noted that their in-house mAb PvALDO RDT had a specificity and sensitivity of 100 and 97.4%, respectively [22]. Five (6.5%) of the microscopically-confirmed P. vivax (n = 77) positive samples were also positively detected by the two aldolase RDTs (mAb 1C3-12 F10 and ParaHit Total ver.1.0); however, the two LDH RDTs (One Step Malaria P.f/P.v and SD Bioline) were unable to identify them [21•]. Two LDH RDT–positive samples (2.6%) were also undetected by the aldolase RDTs [21•]. Therefore, combination usage of LDH and aldolase RDTs would improve the overall sensitivity of the assay in detecting P. vivax malaria [21•].
Rising concerns around the prevalence of pfhrp2 and pfhrp3 deletion mutations have prompted studies to evaluate their effects on PfHRP2/3-detecting RDTs [23•]. In one study by Wurtz and colleagues in Senegal, concerns were raised about the poor performance of RDTs using anti-pfhrp antibodies in an area with malaria having a high rate of pfhrp2 deletion mutations [23•]. Results showed that all of the parasites with a confirmed pfhrp2 deletion were undetected by the PfHRP2 RDT [23•]. That Senegal is endemic for P. falciparum isolates with highly polymorphic pfhrp2 sequences can affect utility of RDTs in this endemic area of Africa [23•]. Furthermore, a similar rate of polymorphism has been detected in Uganda, India, the Asia-Pacific region, and Madagascar, and at much higher rates (up to 41%) in Peruvian isolates [23•]. The interpretation of negative pfhrp2 RDT results in these countries should be corroborated with another diagnostic assay. Further work around the extent of these polymorphisms is needed to ensure quick adaptation to other antigens for the majority of malaria RDTs [23•].
Questions around the clinical, patient-level, significance of RDTs often arise in non-endemic regions, especially in the context of therapeutic delay [24•]. To answer these questions, Ota-Sullivan and colleagues conducted a study in a pediatric non-endemic cohort to evaluate the effect of RDT implementation on laboratory turnaround times [24•]. In fact, confirming the powerful utility of RDTs, a markedly significant reduction in turnaround time was noted pre- and post-RDT introduction: 9.8 h to 1.7 h to diagnosis of any Plasmodium species (p < 0.001), and 10.2 h to 1.6 h for diagnosis of P. falciparum infection (p < 0.001) [24•]. Prompt diagnosis is especially important in pediatric populations, where untreated disease can progress to severity with greater frequency.
Developments in RDTs for P. knowlesi, P. ovale, and P. malariae
Developments in RDTs for P. ovale and P. malariae remain limited due to their lower incidence and milder symptomology; however, initial results in P. knowlesi are promising. The origin of antigens used for antibody production can perhaps shed light on the low sensitivity and specificity in P. ovale and P. malariae detection [25]. P. simium is only a recently recognized pathogen with potential to emerge in humans, and as such, RDTs have yet to be developed. Even with panel RDTs, the general opinion is that P. ovale infections ideally should be diagnosed via microscopy and PCR [26]. Recent literature does not cover P. malariae RDT evaluative studies, nor are there significant novel technologies in development.
Current novel and experimental RDTs detect P. knowlesi infections with low sensitivities and specificities. Evaluation of three popular RDTs place sensitivities for P. knowlesi at 29–71%, noting sharp drops at lower parasitemia, specifically for BinaxNOW® Malaria: 0% at < 5000 parasites/μL and 44% > 5000 parasites/μL [27]. However, combining two RDTs (OptiMAL-IT which uses Pf-pLDH with CareStart which uses non-P. falciparum VOM-pLDH/Pf-HRP2) has been shown to improve specificity to 97% (95% CI: 92–99%), while still having poor sensitivity at only 25% (95% CI: 19–32%) for detection of P. knowlesi [28]. Of note, specificity to P. falciparum and P. vivax is decreased due to P. knowlesi antigen cross-reactivity [28]. Caution should be exercised when using standalone RDTs in P. falciparum and P. knowlesi co-endemic regions such as Southeast Asia [28].
Novel loop-mediated isothermal amplification (LAMP) technology, which allows DNA amplification within an hour at a constant temperature, is currently the most promising field-diagnostic available for P. knowlesi [29•]. The LAMP technology is relatively new and poorly tested in the field, but initial results show extremely high sensitivities for P. knowlesi, P. falciparum, and P. vivax. The sensitivity and specificity of the LAMP assay for P. knowlesi were both 100% (95% CI: 92.9–100%) [29•]. The pan LAMP assay also had a very low limit of detection of 2 parasites/μL [29•]. These technical results are promising; with crude samples used directly for LAMP and simpler assay format by visualizing amplicons on a chromatographic dipstick, their implementation would greatly assist in field diagnostics in endemic settings [29•]. Of note, there are RDT-like LAMP chromatographic lateral flow dipstick (LFD) methodologies that are in development [30•]. Surprisingly, the LAMP-LFD format has a 10-fold higher detection limit when compared to PCR assays [30•]. Lengthy, time-consuming protocols for PCR-based diagnostics for malaria are not conducive to field applications, and therefore this novel LAMP-LFD would be of great potential diagnostic efficacy [30•]. The encouraging results from the LAMP-LFD assay showed reduced assay turnaround time of approximately 1.5 h and ease of use [30•]. Further exploration of LAMP RDTs is warranted.
RDTs in Endemic vs. Non-Endemic Settings
Recent literature focuses more on validating existing RDTs in endemic settings, whereas non-endemic settings aimed to develop novel assays with LAMP, gelled nested PCR and, reducing turnaround time in the laboratory [24•, 31, 32]. End-user (e.g., village worker, pharmacist, physician, medical center staff) validation of RDTs in highly endemic areas of malaria prevalence is important for ensuring widespread adoption and practicality of use in real-world settings. VIKIA Malaria Ag Pf/Pan test and Asan EasyTest Malaria Pf/Pan Ag were evaluated in Cambodia and Uganda, respectively, by end-users, to answer questions surrounding lab to point-of-care concordance and ease-of-use [31, 32]. It was found that RDT end-user performance in field-testing had a high concordance with laboratory personnel, highlighting their ease-of-use, good sensitivity (95.8%), and reliability [31, 32].
Recently, the increased role of standby emergency treatment (SBET) in malaria is discussed as an increasingly useful preventative measure in the traveler population [33, 34]. SBET for malaria provides travelers with self-administered treatment, where no standard medical attention is available [33, 34]. The usefulness of this strategy is presumed to be dependent on the associated risk of acquiring malaria [33, 34]. Similarly, it may be more appropriate to also include malaria RDTs in the traveler’s arsenal, although comprehensive pre-travel education would be required for proper interpretation of results [33]. Including RDTs in an SBET strategy could potentially avert needless administration of empiric antimalarials in febrile travelers to moderate-risk areas of the world [33]. Suitably identifying candidate patients and providing RDTs and SBET for malaria as part of a malaria preventive strategy could be considered in the pre-travel setting. On the other hand, the cost and potential health implications of such a paradigm shift in pre-travel malaria care, at least on the part of North Americas, are multitudinous and complex.
New Technologies and Future Challenges
Use of non-invasively obtained specimens, such as urine samples, rather than blood, is a novel strategy in malaria diagnostics, and one that would eliminate the risk of sharps injury to the healthcare worker engaged in specimen collection. The urine gold nanoparticle (AuNP)-based colorimetric assay detects MSP10 of P. vivax and demonstrates both high sensitivity (84%) and specificity (97%) [35•]. The ease-of-use in detecting a simple color change makes test result allocation potentially less prone to misinterpretation [35•]. The utility of this new antigen is of particular interest in countries such as Peru where pfhrp2 gene deletions are prevalent [35•].
In order to address the growing concerns around the increasing prevalence of pfhrp2 and pfhrp3 gene deletions and polymorphisms, WHO has recently begun a study to accurately measure the prevalence of pfhrp mutations to inform strategic diagnostic directions in malaria [36]. To tackle the diagnosis of malaria parasites with pfhrp mutations, other groups have taken a protein-level bioengineering approach to develop novel mAbs based on the HRP2 exon II [17•]. Kang and colleagues demonstrated that the two new mAbs performed with high overall sensitivity (99.1%) and specificity (100%) in detecting P. falciparum infection [17•]. Where widespread genetic heterogeneity may render current commercial RDTs ineffective and prone to false-negativity, it is crucial to advance alternatives [17•, 36].
WHO-FIND also has a summarized, interactive tool for the selection of RDTs that have been tested by their product testing program and those which passed their criteria [37]. The information here is sortable by panel detection score and various other parameters noted by the WHO when choosing from an array of over a hundred RDTs [37].
LAMP-based diagnostic technology is on the rise in malaria, in light of its cost-effectiveness, ease-of-use, and microscopy-level performance comparability [38•]. PCR malaria diagnostic assays are widely considered to be extremely sensitive tests, but the high costs and related infrastructural requirements make them relatively inaccessible in low- and middle-income countries with high malaria endemicity [38•]. Therefore, if a low-cost, LAMP-based assay without high instrumentation costs could prove to be of comparable performance to PCR, the potential to further develop this technology increases many-fold. Marti and colleagues demonstrated that LAMP assays are able to perform to the same level of qPCR diagnostics, at 100% sensitivity (95% CI: 92.4–100%) and 100% specificity (95% CI: 97.7–100%) compared to qPCR and microscopy, for P. falciparum malaria [38•]. The LAMP-based diagnostic technology platform has huge potential for future development of currently unavailable assays specific for P. ovale, P. malariae, and P. knowlesi where RDT technology is unlikely to supplant microscopy or PCR for detection and quantification of these particular species.
Conclusions
RDTs are promptly advancing to the forefront of malaria diagnostics, especially in P. falciparum, and more recently in P. vivax. Sensitivities and specificities are reaching high levels, and meeting WHO guidelines for RDT procurement, which are product-specific. PCR should also become the reference standard for RDTs as it is challenging to differentiate species specific microscopic morphology in low parasitemia samples, as well as in the simian malarias P. knowlesi and P. simium, which microscopically resemble P. malariae and P. vivax, respectively.
Improvements, not only in P. falciparum RDT performance, but also in P. vivax have quickly progressed to meet growing demand for low-cost, easy-to-use methodology. The clinical utility of P. ovale and P. malariae-specific RDTs continues to be limited by suboptimal sensitivity, thus, diagnostic arbitration is still required in suspected cases of such infections. LAMP platforms are reaching near ideal sensitivity and specificity and, barring novel disruption, will likely emerge as the next step in malaria point-of-care diagnostics.
WHO and many independent groups are working to address the issues of false-positives, false-negatives, and pfhrp gene deletions, via novel biotechnology development along with large-scale global efforts to quantify polymorphism and mutation prevalence. New antibodies and DNA-based diagnostic technology are enhancing malaria RDT usability and reliability. Limitations of RDTs still exist, but product-specific limitations are being overcome with technological and process innovations leading to improved standardization and performance. The advancement of LAMP amplicons analyzed on chromatographic LFD provides potential for development of currently unavailable P. malaraie, P. ovale, P. knowlesi, and P. simium species-specific RDTs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
World Health Organization (WHO). World malaria report 2017 [Internet]. Geneva: World Health Organization; 2017. [cited 2018 Mar 4]. Available from: http://apps.who.int/iris/bitstream/10665/259492/1/9789241565523-eng.pdf?ua=1.
Committee to Advise on Tropical Medicine and Travel (CATMAT). Canadian recommendations for the prevention and treatment of malaria [Internet]. Ottawa: Public Health Agency of Canada; 2014. [cited 2018 Mar 4]. Available from: http://publications.gc.ca/collections/collection_2014/aspc-phac/HP40-102-2014-eng.pdf.
World Health Organization (WHO). Guidelines for the treatment of malaria [Internet]. third ed. Geneva: World Health Organization; 2015. [cited 2018 Mar 4]. Available from: http://apps.who.int/iris/bitstream/10665/162441/1/9789241549127_eng.pdf?ua=1&ua=1.
Maltha J, Gillet P, Jacobs JJ. Malaria rapid diagnostic tests in endemic settings. Clin Microbiol Infect. 2013;19(5):399–407. https://doi.org/10.1111/1469-0691.
Maltha J, Gillet P, Jacobs JJ. Malaria rapid diagnostic tests in travel medicine. Clin Microbiol Infect. 2013;19(5):408–15. https://doi.org/10.1111/1469-0691.
World Health Organization (WHO). Malaria rapid diagnostic test performance: summary results of WHO product testing of malaria RDTs: round 1-7 (2008–2016) [Internet]. Geneva: World Health Organization; 2017. [cited 2018 Mar 4]. Available from: http://apps.who.int/iris/bitstream/10665/258597/1/9789241512916-eng.pdf?ua=1.
Yegorov S, Galiwango RM, Ssemaganda A, Muwanga M, Wesonga I, Miiro G, et al. Low prevalence of laboratory-confirmed malaria in clinically diagnosed adult women from the Wakiso district of Uganda. Malar J. 2016;15(1):555. https://doi.org/10.1186/s12936-016-1604-z.
Center for Disease Control and Prevention. Malaria [Internet]. Atlanta: Center for Disease Control and Prevention; 2015. [cited 2018 Mar 23]. Available from: https://www.cdc.gov/malaria/about/disease.html.
Thompson CA, Boggild AK. Five things to know about: rapid diagnostic tests for imported malaria. CMAJ. 2014;186:E557. https://doi.org/10.1503/cmaj.131794.
World Health Organization (WHO). Recommended selection criteria for procurement of malaria rapid diagnostic tests [Internet]. Geneva: World Health Organization; 2018. [cited 2018 Mar 4]. Available from: http://apps.who.int/iris/bitstream/10665/259870/1/WHO-CDS-GMP-2018.01-eng.pdf?ua=1.
• Abba K, Kirkham AJ, Olliaro PL, Deeks JJ, Donegan S, Garner P, et al. Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or Plasmodium vivax malaria in endemic countries. Cochrane Database Syst Rev. 2014;12:CD011431. https://doi.org/10.1002/14651858.CD011431 A comprehensive systematic review outlining the efficacy of malaria RDTs specifically for non- falciparum / P. vivax forms of the disease.
• Grigg MJ, William T, Barber BE, Parameswaran U, Bird E, Piera K, et al. Combining parasite lactate dehydrogenase-based and histidine-rich protein 2-based rapid tests to improve specificity for diagnosis of malaria due to Plasmodium knowlesi and other Plasmodium species in Sabah, Malaysia. J Clin Microbiol. 2014;52(6):2053–60. https://doi.org/10.1128/JCM.00181-14 An analysis of 323 PCR-confirmed malaria patients that showed improvements in performance when LDH and HRP2-based RDTs were used in combination.
Francis B, Gonzalo X, Duggineni S, Thomas JM, NicFhogartaigh C, Babiker ZO. Epidemiology and clinical features of imported malaria in East London. J Travel Med. 2016;23(6):1. https://doi.org/10.1093/jtm/taw060.
• Phuong M, Lau R, Ralevski F, Boggild AK. Survival analysis of diagnostic assays in Plasmodium falciparum malaria. Malar J. 2015;14(350):1–6. https://doi.org/10.1186/s12936-015-0882-1 A survival analysis between RDT, qPCR and microscopic diagnostics for clinically relevant asexual parasitemia in post-treatment specimens, highlighting that microscopy remains the only reliable method that can ascertain between asexual parasitemia and prolonged clearance of antigen.
Lau R, Phuong M, Ralevski F, Boggild AK. Correlating quantitative real-time PCR to rapid diagnostic test and RNA transcript expression in isolated gametocytemia and asexual parasitemia of Plasmodium falciparum malaria. Trop Dis Travel Med Vaccines. 2015;1:8. https://doi.org/10.1186/s40794-015-0008-3.
Tiono AB, Ouédraogo A, Diarra A, Coulibaly S, Soulama I, Konaté AT, et al. Lessons learned from the use of HRP-2 based rapid diagnostic test in community-wide screening and treatment of asymptomatic carriers of Plasmodium falciparum in Burkina Faso. Malar J. 2014;13:30. https://doi.org/10.1186/1475-2875-13-30.
• Kang K, Dzakah E, Li W, Xie M, Luo X, Liu H. Novel monoclonal antibodies against Plasmodium falciparum histidine-rich protein 2: development and application in rapid diagnostic tests of malaria in hyperendemic regions of China and Myanmar. BMC Microbiol. 2015;15(98). https://doi.org/10.1186/s12866-015-0429-1 Production and testing of novel monoclonal RDT antibodies to P. falciparum HRP-2 exon II immunogenic sites demonstrate high sensitivity and specificity.
Hailu T, Kebede T. Assessing the performance of CareStart malaria Pf/Pv combo test against thick blood film in the diagnosis of malaria in Northwest Ethiopia. Am J Trop Med Hyg. 2014;90(6):1109–12. https://doi.org/10.4269/ajtmh.13-0607.
Kim J-Y, Ji S-Y, Goo Y-K, Na B-K, Pyo H-J, Lee H-N, et al. Comparison of rapid diagnostic tests for the detection of Plasmodium vivax malaria in South Korea. PLoS One. 2013;8(5):e64353. https://doi.org/10.1371/journal.pone.0064353.
Hawkes M, Conroy AL, Opoka RO, Namasopo S, Liles WC, John CC, et al. Use of a three-band HRP2/pLDH combination rapid diagnostic test increases diagnostic specificity for falciparum malaria in Ugandan children. Malar J. 2014;13:43. https://doi.org/10.1186/1475-2875-13-43.
• Ehtesham R, Fazaeli A, Raeisi A, Keshavarz H, Heidari A. Detection of mixed-species infections of Plasmodium falciparum and Plasmodium vivax by nested PCR and rapid diagnostic tests in southeastern Iran. Am J Trop Med Hyg. 2015;93(1):181–5. https://doi.org/10.4269/ajtmh.14-0650 The study demonstrates the usefulness of RDTs in differentiating between mixed-species infections especially in areas where chloroquine resistance is elevated.
Dzakah EE, Kang K, Ni C, Tang S, Wang J, Wang J. Comparative performance of aldolase and lactate dehydrogenase rapid diagnostic tests in Plasmodium vivax detection. Malar J. 2014;13(372):272. https://doi.org/10.1186/1475-2875-13-272.
• Wurtz N, Fall B, Bui K, Pascual A, Fall M, Camara C, et al. Pfhrp2 and pfhrp3 polymorphisms in Plasmodium falciparum isolates from Dakar, Senegal: impact on rapid malaria diagnostic tests. Malar J. 2013;12(34). https://doi.org/10.1186/1475-2875-12-34 A report illustrating the inaccuracy and inability of RDTs to detect malaria in parasites with high pfhrp2 and pfhrp3 polymorphisms.
• Ota-Sullivan K, Blecker-Shelly DL. Use of the rapid BinaxNOW malaria test in a 24-hour laboratory associated with accurate detection and decreased malaria testing turnaround times in a pediatric setting where malaria is not endemic. J Clin Microbiol. 2013;51(5):1567–9. https://doi.org/10.1128/JCM.00293-13 RDT proves to be significantly useful in non-endemic pediatric populations, especially at reducing turnaround time.
Mouatcho JC, Goldring JP. Malaria rapid diagnostic tests: challenges and prospects. J Med Microbiol. 2013;62:1491–505. https://doi.org/10.1099/jmm.0.052506-0.
Tanizaki R, Kato Y, Iwagami M, Kutsuna S, Ujiie M, Takeshita N, et al. Performance of rapid diagnostic tests for Plasmodium ovale malaria in Japanese Travellers. Trop Med Health. 2014;42(4):149–53. https://doi.org/10.2149/tmh.2014-07.
Foster D, Cox-Singh J, Mohamad DSA, Krishna S, Chin PP, Singh B. Evaluation of three rapid diagnostic tests for the detection of human infections with Plasmodium knowlesi. Malar J. 2013;13(60). https://doi.org/10.1186/1475-2875-13-60.
Grigg MJ, William T, Barber BE, Parameswaran U, Bird E, Piera K, et al. Combining parasite lactate dehydrogenase-based and histidine-rich protein 2-based rapid tests to improve specificity for diagnosis of malaria due to Plasmodium knowlesi and other Plasmodium species in Sabah, Malaysia. J Clin Microbiol. 2014;52(6):2053–60. https://doi.org/10.1128/JCM.00181-14.
• Piera KA, Aziz A, William T, Bell D, Gonzalez IJ, Barber BE, et al. Detection of Plasmodium knowlesi, Plasmodium falciparum and Plasmodium vivax using loop-mediated isothermal amplification (LAMP) in a co-endemic area in Malaysia. Malar J. 2017;16(29). https://doi.org/10.1186/s12936-016-1676-9 Novel LAMP RDT is able to detect P. knowlesi infections with great accuracy, making huge strides in previously unavailable non- falciparum diagnostics.
• Yongkiettrakul S, Jaroenram W, Arunrut N, Chareanchim W, Pannengpetch S, Suebsing R, et al. Application of loop-mediated isothermal amplification assay combined with lateral flow dipstick for detection of Plasmodium falciparum and Plasmodium vivax. Parasitol Int. 2014;63(6):777–84. https://doi.org/10.1016/j.parint.2014.06.004 LAMP in the form of a dipstick proves to be extremely useful in reducing time-to-diagnosis and depicts a 10-fold higher detection limit than PCR.
Kim S, Nhem S, Dourng D, Menard D. Malaria rapid diagnostic test as point-of-care test: study protocol for evaluating the VIKIA malaria Ag Pf/Pan. Malar J. 2015;14:114. https://doi.org/10.1186/s12936-015-0633-3.
Chong C-K, Cho PY, Na B-K, Ahn SK, Kim JS, Lee J-S, et al. Evaluation of the accuracy of the EasyTest malaria Pf/Pan Ag, a rapid diagnostic test, in Uganda. Korean J Parasitol. 2014;52(5):501–5. https://doi.org/10.3347/kjp.2014.52.5.501.
Genton B, D’Acremont V. Standby emergency treatment of malaria in travellers (SBET): so be eager to test. J Travel Med. 2017;24(5). https://doi.org/10.1093/jtm/tax032.
Behrens R. Standby emergency treatment of malaria for travellers to low transmission destinations. Does it make sense or save lives? J Travel Med. 2017;24(5). https://doi.org/10.1093/jtm/tax034.
• Alnasser Y, Ferradas C, Clark T, Calderon M, Gurbillon A, Gamboa D, et al. Colorimetric detection of Plasmodium vivax in urine using MSP10 Oligonucleotides and Gold nanoparticles. PLoS Negl Trop Dis. 2016;10:e0005029. https://doi.org/10.1371/journal.pntd.0005029 The report demonstrates a novel gold nanoparticle-based colorimetric diagnostic assay using only urine, with moderate sensitivity and high specificity.
World Health Organization (WHO). Protocol for estimating the prevalence of pfhrp2/pfhrp3 gene deletions among symptomatic falciparum patients with false-negative RDT results [Internet]. Geneva: World Health Organization; 2018. [cited 2018 Mar 5]. Available from: http://apps.who.int/iris/bitstream/10665/260140/1/WHO-CDS-GMP-2018.03-eng.pdf?ua=1.
World Health Organization and FIND. Malaria RDT product testing: interactive guide [Internet]. Geneva: World Health Organization; 2017. [cited 2018 Mar 23]. Available from: http://www.rdt-interactive-guide.org/.
• Marti H, Stalder C, Gonzalez IJ. Diagnostic accuracy of a LAMP kit for diagnosis of imported malaria in Switzerland. Travel Med Infect Dis. 2015;13:167–71. https://doi.org/10.1016/j.tmaid.2014.12.016 Usage of LAMP in a non-endemic traveler population shows that it has versatile applications with comparable performance results to qPCR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Tropical, Travel and Emerging Infections
Rights and permissions
About this article
Cite this article
Mukkala, A.N., Kwan, J., Lau, R. et al. An Update on Malaria Rapid Diagnostic Tests. Curr Infect Dis Rep 20, 49 (2018). https://doi.org/10.1007/s11908-018-0655-4
Published:
DOI: https://doi.org/10.1007/s11908-018-0655-4