Abstract
Since the outbreak of the first SARS-CoV-2 epidemic in China, pharmacists have rapidly engaged and developed strategies for pharmaceutical care and supply. According to the guidelines of the International Pharmaceutical Federation (FIP), clinical pharmacists/hospital pharmacists, as members of care teams, play one of the most important roles in the pharmaceutical care of patients with COVID-19. During this pandemic, many immuno-enhancing adjuvant agents have become critical in addition to antivirals and vaccines in order to overcome the disease more easily. The liquid extract obtained from the Pelargonium sidoides plant is used for many indications such as colds, coughs, upper respiratory tract infections, sore throat, and acute bronchitis. The extract obtained from the roots of the plant has been observed to have antiviral and immunomodulatory activity. In addition to its anti-inflammatory and antioxidant effects, melatonin plays a role in suppressing the cytokine storm that can develop during COVID-19 infection. Knowing that the severity and duration of COVID-19 symptoms vary within 24 hours and/or in different time periods indicates that COVID-19 requires a chronotherapeutic approach. Our goal in the management of acute and long COVID is to synchronize the medication regimen with the patient’s biological rhythm. This chapter provides a comprehensive review of the existing and emerging literature on the chronobiological use of Pelargonium sidoides and melatonin during acute and prolonged COVID-19 episodes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Due to its global spread, the World Health Organization (WHO) classified coronavirus disease (COVID-19) as a pandemic in March 2020 [1]. The virus can be transmitted through the air, surface, or by contact [2]. Entry of SARS-CoV-2 into cells is mediated by angiotensin converting enzyme-2 (ACE2) [3]. ACE2 binds to the receptor-binding domain (RBD) of the SARS-CoV-2 spike (S) protein. In addition, production of the viral S protein for entry into the host cell is necessary for its fusion with the host cell membrane [4]. The S protein is cleaved at the host cell membrane by transmembrane serine protease 2 (TMPRSS2) [5]. Since the pandemic was declared, scientists have conducted several scientific studies to treat and prevent the spread of COVID-19. However, only vaccines, some monoclonal antibodies, and antiviral agents are currently available to treat COVID-19 [6]. One of the most prominent of these is bebtelovimab, which has high neutralizing activity against all subvariants of Omicron [6]. Furthermore, molnupiravir, one of the antiviral agents with proven efficacy against COVID-19, belongs to the therapeutic category [7].
Although many variants of COVID-19 have emerged, the latest and most dominant variant announced by the WHO is the Omicron variant. Omicron was identified as an alarming variant by the WHO in November 2021 [8]. Compared to other known variants, the Omicron variant is more dominant over other variants in terms of mortality and transmission rate [8]. Omicron subvariants, namely, BA.1, BA. 2, BA.3, were found at the same time and reported to be more contagious than the previously dominant Delta variant but have a milder disease course [9]. Subvariant BA.4 was first discovered in January 2022 and subvariant BA.5 in February in South Africa [10]. It is known that the BA.4 and BA.5 subvariants have higher infectivity rates than others [10]. The difference between the new subvariants and their predecessors is that the symptoms last longer. While the average recovery time in patients with the Omicron variant BA.1/2/3 is 4–5 days, it can be up to 10 days for the BA.4/5 subvariants [11].
Therefore, new treatments against SARS-CoV-2 disease are urgently needed as a therapeutic strategy against COVID-19 to reduce the effectiveness of the virus, prevent transmission, and eliminate severe inflammation as a result of the cytokine storm effect triggered by the virus [12]. Today, as the disease is being caught at an increasingly early stage, many patients try to overcome the infection process by isolating at home unless their condition worsens. The number of patients applying their own treatment in isolation at home is also increasing.
In many cases, infection by the SARS-CoV-2 virus may cause few or no symptoms. However, the absence of severe symptoms does not usually mean that the patient has fully recovered. Coronaviruses can now persist in cells for a long time [13]. According to the terminology of the American Infectious Diseases Association (IDSA), this phenomenon is referred to as “long covid,” “post-covid syndrome,” or “post-acute covid-19 syndrome” [14]. According to numerous reports, most patients who had COVID-19 are likely to develop a long COVID condition [15]. Some of these patients cannot undergo surgery because of the irreversible damage to their organs [16]. Although there is no visible organ damage in some individuals with other diseases, a condition that mimics the symptoms of the disease still exists. In these cases, COVID-19 can hide under various masks of symptoms. Researchers have identified more than 200 post-COVID symptoms in 10 organ systems [17].
Common pathophysiological syndromes of prolonged COVID-19 are also listed as four clinical pictures. These are systemic inflammation, endothelitis, pulmonitis, and asthenic syndrome [18]. Systemic inflammation is the result of a systemic hyperimmune response. Cytokines continue to be released like a cytokine storm in the lungs. This can also be accompanied by immune inflammation in brainstem structures that trigger the development of neurological complications. Endotheliitis is the general inflammatory damage to vascular endothelial cells. This situation triggers a disturbance of coagulation homeostasis linked to thromboembolisms, decreased energy supply to the myocardium, development of myocardial infarction, stroke, and myocarditis [18]. Pulmonitis is a lung injury that develops due to vascular and alveolocyte damage by viruses and cytokines. The process of fibrosis of lung tissue is activated and lung function (vital capacity) decreases [19]. Asthenic syndrome is a leading clinical syndrome that significantly worsens quality of life and reduces work capacity [19].
After acute COVID-19, mandatory monitoring of respiratory function, cardiac symptoms, nervous system, and mental functions is required, along with a focus primarily on eliminating systemic background inflammation and improving function. In addition, monitoring should be extended to detect the presence of long COVID-19, as evidenced by the persistence of symptoms for more than 1 month after initial diagnosis [20]. Considering their low cost and wide availability, increasing attention is now being paid to the potential use of herbal preparations containing agents as adjunctive treatments against the cytokine storm effects resulting from SARS-CoV-2 infections. Due to the clinical safety of Pelargonium sidoides extract [21], along with its antiviral and/or immunomodulatory activity, the use of this extract may be desirable as an adjuvant in daytime management of COVID-19 [22]. Pelargonium sidoides preparations have been used as a herbal supplement to treat viral diseases prior to the COVID-19 pandemic [23]. In addition, melatonin, which is a key component of circadian rhythm, could be used as an adjuvant in treatment due to its immunosuppressive properties against the bedtime cytokine storm caused by COVID-19 infection [24,25,26]. Pelargonium sidoides extracts and melatonin are among the commonly used prescription and over-the-counter drugs in pharmacies for the treatment of COVID-19. Although clinical trials of the antiviral efficacy of both drugs were conducted prior to COVID-19, no clinical trials of their use in combination therapy have been conducted during this pandemic. However, distribution of these prescription and over-the-counter drugs through pharmacies continues. Community pharmacists, as well as clinical pharmacists, are responsible for providing information and educating their patients on this topic. This chapter aims to evaluate the possible mechanisms of action when both drugs are used in combination against acute and long COVID from a chronobiological perspective.
2 The Possible Chronobiological Efficiency of Melatonin in Acute and Long COVID-19 Period
Chronopharmacology is the branch of chronobiology that studies the effects of drugs on the timing and rhythms of biological events and the relationship between biological timing and drug effects [26]. It is used as an important tool in optimizing drugs, maximizing the desired effect and minimizing the undesirable effects of a drug. Processes such as tissue growth, blood pressure, heart rate, and blood glucose level are regulated by a biological clock [27]. The mammalian circadian system is regulated by the suprachiasmatic nucleus (SCN), the central oscillator located in the hypothalamus. The rhythm that occurs in the SCN due to daylight ensures that the peripheral clocks in all cells are synchronized through many neuronal and hormonal rhythms [27]. Peripheral tissue synchronization is related to peripheral clocks. It may also be related to SCN-mediated hormone release and environmental factors.
Melatonin is a hormone secreted in humans under the influence of darkness, suppressed by light, and regulated by the SCN [28]. In mammals, circadian rhythm is influenced by how the SCN center of the hypothalamus is organized in the brain. Pineal gland functions are acutely suppressed when exposed to light [28]. Therefore, the amount of synthesized melatonin changes depending on the day-night rhythm and synthesis peaks at night. Melatonin is known to reduce oxidative stress [29]. Its antioxidant effect comes from scavenging free radicals, reducing metals, and taking part in the secretion of enzymes related to our redox system: catalase, glutathione peroxidase, and superoxide dismutase. It is also effective in the regulation of mitochondrial functions that cause free radical production and related oxidative stress [29]. Melatonin also reduces the production of pro-oxidant nitric oxide synthase and lipoxygenase enzymes [30]. For these reasons, it has become the target of many research and clinical studies as a therapeutic approach during the COVID-19 pandemic.
Melatonin has recently been proposed as a possible first-line treatment for acute COVID-19 [31]. However, it may also be useful for treating long COVID patients with neuropsychiatric symptoms such as anxiety, insomnia, and depression [32]. The most well-known neurological and psychiatric symptoms of long COVID are impaired smell and taste, sleep problems, memory problems, depression, and anxiety. According to the chronopharmacological approach, taking melatonin before bedtime may positively affect the therapy, especially for people in high-risk groups such as those with type-2 diabetes, asthma, and hypertensive patients, in order to prevent both acute and long COVID-19 symptoms.
3 Melatonin and Its Effect on the Immune System
Melatonin is synthesized from tryptophan and secreted mainly by the pineal gland [33]. Melatonin has strong lipophilic and hydrophilic properties, and it mixes with blood and body fluids without being stored in the body. Most of the melatonin in the blood is bound to albumin [34]. This hormone is primarily metabolized in the liver and secondarily in the kidneys to 6-hydroxymelatonin sulfate and 6-hydroxymelatonin glucuronide [34]. These molecules are excreted from the body in the urine. Due to the rhythmic release of melatonin, the amount of metabolites in the urine is higher at night [33]. Mammals have two distinct melatonin receptors that pharmacologically bind to their cell membranes. These are the MT1 (high affinity) and MT2 (low affinity) receptors [35].
The most important functions of melatonin are the regulation of biological rhythms and sleep patterns. However, many studies have been conducted on its ability to reduce stress and the signs of aging by directly increasing life expectancy [36]. In addition to all of these effects, melatonin has also been shown to directly interact with T lymphocytes in the immune system and increase immunity at the cellular level [37]. Melatonin also has anti-inflammatory effects in addition to having an impact on reactive oxygen species (ROS) [38]. As a result, numerous studies have been conducted on this hormone, and it has been proposed as an adjuvant therapy for several viral diseases that trigger a cascade of immunoinflammatory responses [38]. This is due to its capacity as a potent scavenger of hydroxyl radicals and an inducer of superoxide dismutase and glutathione reductase and several other enzymes. Because of these effects, melatonin elicits an effective immune response against cellular oxidative damage [38]. Melatonin also attenuates negative immunological responses in a number of viral activities, including the COVID-19-induced cytokine storm effect [39]. It has been established that some viruses act to prevent the synthesis of melatonin in order to prevent their own destruction and to allow their replication inside the host cell. The mechanism of this is due to a viral-mediated decrease in gene expression of certain enzymes involved in the formation of the melatonin-synthesizing amino acid tryptophan. This is consistent with the finding that many viral infections are exacerbated by the decrease in melatonin levels in cells [39].
4 The Antiviral Effects of Melatonin and Its Use Against COVID-19
Both melatonin and Pelargonium sidoides root extract have been shown to be curative for their respective therapies in previous studies [40, 41]. The SARS-CoV-2 virus is similar to the respiratory syncytial virus (RSV) that emerged in the pre-pandemic period in terms of the damage it inflicts on the body. RSV infection, like that of SARS-CoV-2, causes degeneration of bronchial epithelial cells. This is achieved by RSV acting through the toll-like receptor 3 (TLR3) to activate the transcription factor nuclear factor kappa B (NF-κB) [42]. This can lead to a massive infiltration of the lung parenchyma by lymphocytes, neutrophils, and macrophages, resulting in damage due to pro-inflammatory and non-specific oxidative stress [43].
Inhibition of NF-κB activation reduces the hyperinflammatory response of the cell to respiratory viruses. In line with this, melatonin administration has been reported to inhibit TLR3-mediated gene expression in RSV-infected macrophages [44]. Melatonin was found to significantly reverse lung injury and suppress tumor necrosis factor (TNF-α) production by CD8 cells in the lungs and spleen of mice infected with influenza A [45]. In addition, treatment with high doses of melatonin has been found to upregulate anti-inflammatory cytokines, such as interleukin IL-10, and this can further reduce the inflammatory response elicited by viruses infecting the lungs [46]. Treatment of RSV-infected mice with melatonin resulted in a normalizing effect on nitric oxide, malondialdehyde, hydroxyl, GSH and SOD levels, which formed the basis of RSV-related acute oxidative lung injury [47].
In other studies, melatonin has been shown to have a protective effect against another viral disease, the Ebola virus, which has numerous similarities with COVID-19 [48]. Melatonin also prevents the severe vascular endothelial damage that leads to multi-organ bleeding caused by the Ebola virus. The harmful effects of the Ebola virus include the induction of inflammatory chemokines and cytokines like monocyte chemoattractant protein-1 (MCP-1), tissue factor, interferon, IL-6, and IL-8. Melatonin‘s ability to counteract Ebola can be attributed to its ability to increase type 2 T helper cytokine production, interferon-gamma response, and natural killer cell activity while decreasing ROS caused by cytokine storms and viral infections [49]. However, melatonin also inhibits Ebola replication by inducing an enzyme called heme-oxygenase-1. Ultimately, melatonin inhibits pro-inflammatory processes, activates endogenous antioxidants, enhances mitochondrial activity, and thus protects endothelial barriers in septic shock, as well as in disseminated intravascular coagulation [49].
Plasma melatonin levels in patients with hemorrhagic fever are significantly low [50]. Therefore, melatonin could possibly act as a protective agent against encephalitis-causing viruses such as West Nile virus and the virus that causes rabbit hemorrhagic disease [50]. Several studies have shown that melatonin significantly reduces viral load in the blood, decreases mortality, and attenuates disease severity [51]. TNF-α increases intercellular adhesion molecules, alters the blood–brain barrier permeability, and promotes lymphocyte entry into the central nervous system (CNS) [52]. Melatonin treatment reduces the damaging hyperinflammatory effects of TNF-α in the CNS while at the same time causing an increase in astrocytic release of nerve growth factor as a protective measure [53].
Melatonin can be used to treat SARS-CoV-2 viral infections, severe inflammatory responses, and the effects of virus-induced oxidative stress [54]. The S1 and S2 subunits of the viral S protein are used by SARS-CoV-2 to enter alveolar epithelial cells via ACE2 [54]. While binding to ACE2 occurs at S1, the S2 mediates cell membrane fusion. At the plasma membrane, calmodulin regulates ACE2 surface area and uptake [55]. Melatonin, on the other hand, inhibits calmodulin and, hence, indirectly prevents ACE2 from binding to SARS-CoV-2 during the infection process [55]. Melatonin also blocks the activity of the primary protease enzyme of SARS-CoV-2 involved in cleavage of the viral polyprotein and the replication process [56]. Binding of SARS-CoV-2 to ACE2 leads to generation of angiotensin II. When angiotensin II is formed, the antioxidant and anti-inflammatory properties of the angiotensin-1-7 peptide are significantly diminished [57]. Left unchecked, angiotensin II overproduction triggers NF-κB signaling, allowing the production of IL-6 and constriction of blood vessels [57]. The cumulative effect of these events leads to lung cell damage which triggers significant inflammatory and adaptive immune responses. However, melatonin is an angiotensin 1–7 agonist and can thereby act as an inhibitor of angiotensin II activation in the above damaging cascade.
5 Anti-Inflammatory Effect of Melatonin in SARS-CoV-2 Infection
SARS-CoV-2 triggers programmed cell death by causing pyroptosis, a highly inflammatory state and consequential severe lung pathologies [58]. A viral protein produced by SARS-CoV-2 interacts with the inflammatory domain of the NLR family pyrin-domain containing 3 (NLRP3) inflammasome at the peak of infection, resulting in an inflammatory release of cellular contents that ruptures the host cell membrane. In addition, activation of NLPR3 stimulates the release of damaging pro-inflammatory cytokines [59].
Melatonin has an anti-inflammatory action in the cell because it prevents pyroptosis and inhibits the activity of NLRP3 [60]. A cytokine storm characterized by elevated levels of some inflammatory interleukins, C-reactive protein, and TNF-α follows the increased levels of neutrophils brought on by the innate response to SARS-CoV-2 infection [61]. In addition, melatonin inhibits inducible nitric oxide synthase, NF-kB signaling, and cyclooxygenase-2 levels [62].
Exacerbation of COVID-19 disease is due to the accumulation of monocytes and macrophages in the respiratory tract, which causes hyperinflammation during the infection process [63]. The switch to cytosolic anaerobic glycolysis for adenosine triphosphate synthesis results in an increase in the generation of cytokines, killer T cells, and eventual destruction of the alveolar cells [63]. Melatonin induces the transformation of pro-inflammatory glycolytic macrophages into anti-inflammatory macrophages, which allows oxidative phosphorylation to occur [64]. In addition, melatonin inhibits the production of hyperinflammatory macrophages by interacting with multiple signaling pathways such as sirtuin 1 [64].
Upon entry into SARS-CoV-2 cells, deleterious oxidative effects can cause epithelial cell damage with uncontrolled release of mitochondrial ROS [65]. As part of the host immunological response, it also induces macrophages, monocytes, and neutrophils to release ROS [65]. Counter to this, melatonin exerts its antioxidant properties by stimulating antioxidant enzymes to scavenge the damaging oxygen and nitrogen-containing free radicals [66]. It can also achieve this by maintaining mitochondrial homeostasis and suppressing production of pro-oxidative enzymes. Melatonin is also known to regulate autophagy, endoplasmic reticulum stress, and apoptosis through its antioxidant properties [66], and it prevents acute oxidative injury by suppressing ROS and restoring antioxidant enzyme levels [47, 67]. ROS has been identified as a key factor in the hypoxic respiratory failure that occurs in the most severe SARS-CoV-2 infections because of its adverse effects on lung and red blood cell function. High amounts of ROS have an adverse effect on the cytoplasmic and membrane lipids in circulating cells [68]. Red blood cells are a typical example because they show considerable lipid alterations in the capillary bed that influences both red blood cell smoothness and gas transport. These ROS-induced alterations can lead to thrombotic states that adversely impair normal oxygen delivery and vasodilation. Melatonin combats these ROS effects by activating the electron transport chain, preventing ROS damage, and boosting mitochondrial respiration and adenosine triphosphate synthesis [69, 70].
The anti-inflammatory and antioxidant properties of melatonin make it a potentially effective therapy for COVID-19, as it affects all phases of the viral life cycle, including viral entry and deleterious signaling pathways [71]. Theoretically, melatonin should be given at the onset of infection, where it will have the most significant impact on management of COVID-19. It is inexpensive compared with other drugs used for treatment, it is readily available in pharmacies, and has an acceptable safety profile [72]. While it is used to prevent early viral replication, it could also be employed as a preventative measure against viral infection and as remedy in existing COVID-19 patients [73]. In line with this, a single-blind, randomized trial demonstrated that melatonin, when combined with acyclovir, significantly diminished the symptoms of herpes simplex virus [51].
6 Pelargonium sidoides Root Extract as an Adjuvant for the Treatment of Acute and Long COVID-19
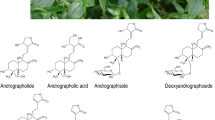
Pelargonium sidoides commonly known as “African Sardinia” is a perennial plant of the Geraniaceae family that grows in the highlands of South Africa and Lesotho [74]. It has been used therapeutically for diarrhea, colds, skin infections, infections of the upper respiratory tract, and tuberculosis [74]. Pelargonium sidoides drew the attention of European scientists in the nineteenth century due to its therapeutic properties against tuberculosis and was brought to Europe for this purpose [74]. The use of Pelargonium sidoides root extract gained notice across Europe after it was found out that its root extract could treat severe cases of tuberculosis [75]. The pharmacological activity of Pelargonium sidoides has been linked to the biological activity of its constituent flavonoids, coumarins, phenolic, gallic, and hydroxycinnamic acid derivatives [76]. Based on this, Pelargonium sidoides extracts are under investigation for antibacterial, antiparasitic, and antiviral properties, especially against Streptococcus, Leishmania amazonensis, and RSV strains [76]. In their study on the root extract of Pelargonium sidoides, Papies et al. found that it has various immunomodulatory and antiviral effects that strengthen host defense mechanisms and reduce inflammation [77].
Another study found reduction of nasally secreted chemokines and epithelial-neutrophil activating peptide (ENA-78) associated with improvement of symptoms in patients with acute bacterial rhinosinusitis treated with Pelargonium sidoides [78]. Moreover, an increase in the levels of motif chemokine ligand 10 and 2 suggested that this extract has selective immunomodulatory effects in acute respiratory infections [78]. In particular, Papies et al. investigated the potential effect of Pelargonium sidoides against SARS-CoV-2 infection in human lung cells. Their results showed that the extract limited the ability of the virus to spread and differentially controlled the release of immunomodulatory cytokines such as IL-1β [77].
Phytochemical characterization of Pelargonium sidoides fractions identified proanthocyanidins as the main active compounds [79]. The immunomodulatory effects of these compounds on pro-inflammatory IL-1 and anti-inflammatory TNF Alpha Induced Protein 3 (TNFAIP3) were found to more potent than those in the extract [79]. Pelargonium sidoides suppresses the release of several cytokines and growth factors involved in SARS-CoV-2 infection [80]. The results of these studies are also consistent with the previously studied anti-influenza effects of Pelargonium sidoides as well as by inhibitory effects on other viruses [81].
Pelargonium sidoides is a daytime flowering plant [82]. Therefore, from a chronobiological point of view, it is possible that it is more biologically active during the day. In addition, the recommended use of herbal products containing Pelargonium sidoides by the European Medicines Agency (EMA) is three times a day: morning, noon, and evening [82]. Therefore, in addition to the use of Pelargonium sidoides preparations during the day, nocturnal melatonin supplementation may add a complementary effect by reducing the symptoms commonly observed in the acute and persistent phase of COVID and to facilitate the treatment process.
7 The Role of Clinical Pharmacists in Adjuvant Chronotherapy for Acute and Ongoing COVID-19
Chronotherapy is a way to increase the efficacy and safety of therapy by administering drugs according to rhythmic changes in disease exposure to the drugs and/or the patient’s tolerance to the side effects of the drug [83]. In other words, the goal of chronotherapy is to optimize the expected effects of the drug over time while minimizing its side effects. Determining the appropriate time to administer the drug in the appropriate indication, through the appropriate route of administration and ensuring patient compliance are key objectives in this endeavor [83]. As part of the process, clinical pharmacists have important responsibilities related to the timing of drug administration. Answering questions such as at what time of day the patient’s symptoms are worse, the duration of the drug’s effects, and what times of the day the patient feels most comfortable, will contribute to the prevalence of such time orientation in drug use [83].
7.1 The Role of the Pharmacist
In addition to the traditional role of pharmacists, such as clinical pharmacy and pharmaceutical care, improving the quality of life and achieving positive clinical outcomes, cognitive services are also evolving in this field worldwide [84]. During the pandemic in particular, the role of pharmacists has become patient service-oriented [84]. Because of these changes, pharmacies and pharmacists have assumed new roles during the acute and long COVID-19 periods, and individuals can more easily access medical treatment and supportive care.
In many countries like the United States and the United Kingdom, pharmacies have served as vaccination centers and PCR centers in addition to selling and prescribing medicines during the COVID-19 pandemic [85]. Also, during this pandemic, online pharmacies evolved to minimize physical contact and also served as an escape from some of the bureaucracy that slows down healthcare services. Through this, pharmacists have worked with patients to ensure that they understand their prescriptions correctly and adhere to their therapies. In addition, pharmacists have been able to track updates on long COVID developments through these online networks [86].
Because of their experience with other viruses that have similar effects as SARS-CoV-2, pharmacists can quickly and confidently determine an appropriate treatment plan for the patient. In this regard, pharmacies also offer herbal and hormonal dietary supplements [87] such as Pelargonium sidoides and melatonin. Based on the importance of chronotherapy described in this chapter, advice concerning the timing of when a patient should take these remedies would be of critical importance. The chronobiological use of Pelargonium sidoides in combination with melatonin in long COVID is shown in Fig. 23.1.
8 Conclusions and Future Perspectives
In this chapter, we have described how the use of melatonin along with Pelargonium extract as adjuvant therapy may be effective in both the acute and chronic phases of COVID-19 disease. One of the reasons melatonin can be used as an adjunct in the treatment of COVID-19 is its ability to reduce toxicity and increase drug efficacy. In severe cases of acute SARS-CoV-2 infection and in patients at high risk of long COVID illness, melatonin and Pelargonium sidoides may be preferred for the treatment of COVID-19 due to their tolerable side effects, low cost, ease of use, and accessibility. However, the chronobiological effects of this combination therapy should be considered to maximize efficacy and reduce potential side effects. Regarding the role of pharmacies and pharmacists in the acute phase, and long COVID, it has been shown that community pharmacies are likely to be part of the front line of health services in future pandemics. Thus, they may play a significant role in the administration of compounds such as Pelargonium sidoides and melatonin in acute and persistent viral infections which have chronobiological effects. Taking all of these factors into account, it is clear that further studies are warranted at the laboratory and clinical levels on the use of these compounds as potential viral remedies.
References
Cucinotta D, Vanelli M (2020) WHO Declares COVID-19 a Pandemic. Acta Biomed 91(1):157–160
Jayaweera M, Perera H, Gunawardana B, Manatunge J (2020) Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ Res 188:109819. https://doi.org/10.1016/j.envres.2020.109819
Beyerstedt S, Casaro EB, Rangel ÉB (2021) COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur J Clin Microbiol Infect Dis 40(5):905–919
Jackson CB, Farzan M, Chen B, Choe H (2022) Mechanisms of SARS-CoV-2 entry into cells. Nature reviews. Mol Cell Biol 23(1):3–20
Bollavaram K, Leeman TH, Lee MW, et al (2021) Multiple sites on SARS-CoV-2 spike protein are susceptible to proteolysis by cathepsins B, K, L, S, and V. Protein Sci 30(6):1131–1143
Cao Y, Yisimayi A, Jian F, et al (2022) BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by Omicron infection. Nature 608(7923):593–602
Pourkarim F, Pourtaghi-Anvarian S, Rezaee H (2022). Molnupiravir: A new candidate for COVID-19 treatment. Pharmacol Res Perspect 10(1):e00909. https://doi.org/10.1002/prp2.909
Daria S, Bhuiyan MA, Islam MR (2022) Detection of highly muted coronavirus variant Omicron (B.1.1.529) is triggering the alarm for South Asian countries: Associated risk factors and preventive actions. Journal of medical virology, 94(4):1267–1268
Dhawan M, Saied AA, Mitra S, et al (2022) Omicron variant (B.1.1.529) and its sublineages: What do we know so far amid the emergence of recombinant variants of SARS-CoV-2?. Biomed Pharmacother 154:113522. https://doi.org/10.1016/j.biopha.2022.113522
Tallei TE, Alhumaid S, AlMusa Z, et al (2022) Update on the omicron sub-variants BA.4 and BA.5. Rev Med Virol; e2391. https://doi.org/10.1002/rmv.2391
Xu A, Hong B, Lou F, et al (2022) Sub-lineages of the SARS-CoV-2 Omicron variants: Characteristics and prevention. MedComm 3(3):e172. https://doi.org/10.1002/mco2.172
Diamond MS, Kanneganti TD (2022). Innate immunity: the first line of defense against SARS-CoV-2. Nat Immunol 23(2):165–176
Spudich S, Nath A (2022) Nervous system consequences of COVID-19. Science 375(6578):267–269
Kikkenborg Berg S, Dam Nielsen S, Nygaard U, et al (2022) Long COVID symptoms in SARS-CoV-2-positive adolescents and matched controls (LongCOVIDKidsDK): a national, cross-sectional study. Lancet Child Adolesc Health 6(4):240–248
Abacioglu N (2022) The situation in the world in the Covid-19 pandemic (Turkish). https://ilerihaber.org/yazar/covid-19-pandemisinde-dunyadaki-durum-145315
Stefanou MI, Palaiodimou L, Bakola E, et al (2022). Neurological manifestations of long-COVID syndrome: a narrative review. Ther Adv Chronic Dis 13:20406223221076890. https://doi.org/10.1177/20406223221076890
Aiyegbusi OL, Hughes SE, Turner G, et al (2021) Symptoms, complications and management of long COVID: a review. J Royal Soc Med 114(9):428–442
Silva Andrade B, Siqueira S, de Assis Soares WR, et al (2021). Long-COVID and Post-COVID Health Complications: An Up-to-Date Review on Clinical Conditions and Their Possible Molecular Mechanisms. Viruses 13(4):700. https://doi.org/10.3390/v13040700
Zolotovskaia IA, Shatskaia PR, Davydkin IL, Shavlovskaya OA (2021) Astenicheskii sindrom u patsientov, perenesshikh COVID-19 [Post-COVID-19 asthenic syndrome]. Zh Nevrol Psikhiatr Im S S Korsakova 121(4)25–30
van Kessel S, Olde Hartman TC, Lucassen P, van Jaarsveld C (2022) Post-acute and long-COVID-19 symptoms in patients with mild diseases: a systematic review. Fam Pract 39(1):159–167
Murgia V, Ciprandi G, Votto M, et al (2021) Natural remedies for acute post-viral cough in children. Allergol Immunopathol (Madr) 49(3):173–184
Gajewski A, Kośmider A, Nowacka A, et al (2021). Potential of herbal products in prevention and treatment of COVID-19. Literature review. Biomed Pharmacother 143:112150. https://doi.org/10.1016/j.biopha.2021.112150
Khan T, Khan MA, Mashwani ZU, et al (2021) Therapeutic potential of medicinal plants against COVID-19: The role of antiviral medicinal metabolites. Biocatal Agric Biotechnol 31:101890. https://doi.org/10.1016/j.bcab.2020.101890
Sun SY, Chen GH (2022). Treatment of Circadian Rhythm Sleep-Wake Disorders. Curr Neuropharmacol 20(6):1022–1034
Zhai X, Wang N, Jiao H, et al (2021) Melatonin and other indoles show antiviral activities against swine coronaviruses in vitro at pharmacological concentrations. J Pineal Res 71(2):e12754. https://doi.org/10.1111/jpi.12754
Abacioglu N (2017) Fundamentals of Chronobiology, Chronopharmacology and Chronotherapy with Questions (Turkish), Etkin Eczacılık Derneği Ankara, Turkey. pp. 1–46.
Peng F, Li X, Xiao F, et al (2022) Circadian clock, diurnal glucose metabolic rhythm, and dawn phenomenon. Trends Neurosci 45(6):471–482
Fowler S, Hoedt EC, Talley NJ, et al (2022) Circadian Rhythms and Melatonin Metabolism in Patients With Disorders of Gut-Brain Interactions. Front Neurosci 16:825246. https://doi.org/10.3389/fnins.2022.825246
Jarrott B, Head R, Pringle KG, et al (2022) "LONG COVID"-A hypothesis for understanding the biological basis and pharmacological treatment strategy. Pharmacol Res Perspect 10(1):e00911. https://doi.org/10.1002/prp2.911
Wang Y, Zhang S, Ma Y, et al. (2022) Melatonin protected against myocardial infarction injury in rats through a Sirt6-dependent antioxidant pathway. Adv Clin Exp Med 31(3):277–284
Loh D, Reiter RJ (2022). Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19. Int J Mol Sci 23(15):8122. https://doi.org/10.3390/ijms23158122
Xerfan E, Morelhao PK, Arakaki FH, et al (2022) Could melatonin have a potential adjuvant role in the treatment of the lasting anosmia associated with COVID-19? A review. Int J Dev Neurosci 82(6):465–470
Bantounou M, Plascevic J, Galley HF (2022) Melatonin and Related Compounds: Antioxidant and Anti-Inflammatory Actions. Antioxidants (Basel) 11(3):532. https://doi.org/10.3390/antiox11030532
Rzepka-Migut, B, Paprocka J (2020) Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature. Int J Environ Res Public Health 17(6):1916. https://doi.org/10.3390/ijerph17061916
Gao Y, Zhao S, Zhang Y, Zhang Q (2022) Melatonin Receptors: A Key Mediator in Animal Reproduction. Vet Sci 9(7):309. https://doi.org/10.3390/vetsci9070309
Cardinali DP (2021) Melatonin and healthy aging. Vitam Horm 115:67–88
Liu Y, Chen XQ, Wang F, et al (2022) Melatonin relieves Th17/CD4-CD8- T cells inflammatory responses via nuclear-receptor dependent manner in peripheral blood of primary Sjögren’s syndrome. Int Immunopharmacol 109:108778. https://doi.org/10.1016/j.intimp.2022.108778
Camp OG, Bai D, Gonullu DC, et al (2021) Melatonin interferes with COVID-19 at several distinct ROS-related steps. J Inorg Biochem 223:111546. https://doi.org/10.1016/j.jinorgbio.2021.111546
Reiter RJ, Sharma R, Simko F, et al (2022) Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection. Cell Mol Life Sci 79(3):143. https://doi.org/10.1007/s00018-021-04102-3
Suriagandhi V, Nachiappan V (2022) Protective Effects of Melatonin against Obesity-Induced by Leptin Resistance. Behav Brain Res 417:113598. https://doi.org/10.1016/j.bbr.2021.113598
Born TA (2020) A Pragmatic Approach to Immunity & Respiratory Viral Infections. Integr Med (Encinitas) 19(5):8–15
Yoboua F, Martel A, Duval A, et al (2010) Respiratory syncytial virus-mediated NF-kappa B p65 phosphorylation at serine 536 is dependent on RIG-I, TRAF6, and IKK beta. J Virol 84(14):7267–7277
Kalil AC, Thomas PG (2019) Influenza virus-related critical illness: pathophysiology and epidemiology. Crit Care 23(1):258. https://doi.org/10.1186/s13054-019-2539-x
Huang SH, Cao XJ, Wei W (2008) Melatonin decreases TLR3-mediated inflammatory factor expression via inhibition of NF-kappa B activation in respiratory syncytial virus-infected RAW264.7 macrophages. J Pineal Res 45(1):93–100
Sehirli AÖ, Chukwunyere U, Aksoy U, et al (2021) The circadian clock gene Bmal1: Role in COVID-19 and periodontitis. Chronobiol Int 38(6):779–784
Wichniak A, Kania A, Siemiński M, Cubała WJ (2021) Melatonin as a Potential Adjuvant Treatment for COVID-19 beyond Sleep Disorders. Int J Mol Sci 22(16):8623. https://doi.org/10.3390/ijms22168623
Huang SH, Cao XJ, Liu W, et al (2010) Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice. J Pineal Res 48(2):109–116
Afolabi MO, Folayan MO, Munung NS, et al (2021) Lessons from the Ebola epidemics and their applications for COVID-19 pandemic response in sub-Saharan Africa. Dev World Bioeth 21(1):25–30
Tan DX, Korkmaz A, Reiter RJ, Manchester LC (2014) Ebola virus disease: potential use of melatonin as a treatment. J Pineal Res 57(4):381–384
Qin S, Underwood D, Driver L, et al (2018) Evaluation of a duplex reverse-transcription real-time PCR assay for the detection of encephalomyocarditis virus. J Vet Diagn Invest 30(4):554–559
Cross KM, Landis DM, Sehgal L, Payne JD (2021) Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy. Endocr Pract 27(8):850–855
Corti A, Calimeri T, Curnis F, Ferreri A (2022) Targeting the Blood-Brain Tumor Barrier with Tumor Necrosis Factor-α. Pharmaceutics 14(7):1414. https://doi.org/10.3390/pharmaceutics14071414
Linnerbauer M, Rothhammer V (2020) Protective Functions of Reactive Astrocytes Following Central Nervous System Insult. Front Immunol 11:573256. https://doi.org/10.3389/fimmu.2020.573256
Shchetinin E, Baturin V, Arushanyan E, et al (2022) Potential and Possible Therapeutic Effects of Melatonin on SARS-CoV-2 Infection. Antioxidants (Basel) 11(1):140. https://doi.org/10.3390/antiox11010140
Cecon E, Fernandois D, Renault N, et al (2022) Melatonin drugs inhibit SARS-CoV-2 entry into the brain and virus-induced damage of cerebral small vessels. Cell Mol Life Sci 79(7):361. https://doi.org/10.1007/s00018-022-04390-3
Feitosa EL, Júnior F, Nery Neto J, et al (2020) COVID-19: Rational discovery of the therapeutic potential of Melatonin as a SARS-CoV-2 main Protease Inhibitor. Int J Med Sci 17(14):2133–2146
Issa H, Eid AH, Berry B, et al (2021) Combination of Angiotensin (1-7) Agonists and Convalescent Plasma as a New Strategy to Overcome Angiotensin Converting Enzyme 2 (ACE2) Inhibition for the Treatment of COVID-19. Frontiers in Medicine. https://doi.org/10.3389/fmed.2021.620990
Bittner ZA, Schrader M, George SE, Amann R (2022) Pyroptosis and Its Role in SARS-CoV-2 Infection. Cells 11(10):1717. https://doi.org/10.3390/cells11101717
Chan AH, Schroder K (2020). Inflammasome signaling and regulation of interleukin-1 family cytokines. J Exp Med 217(1):e20190314. https://doi.org/10.1084/jem.20190314
Arioz BI, Tarakcioglu E, Olcum M, Genc S (2021) The Role of Melatonin on NLRP3 Inflammasome Activation in Diseases. Antioxidants (Basel) 10(7):1020. https://doi.org/10.3390/antiox10071020
Zivancevic-Simonovic S, Jovanovic D, Cupurdija V, et al (2022) Cytokine producing ability of peripheral blood cells from COVID-19 patients after unspecific in vitro stimulation. Inflamm Res 71(3):331–341
Hardeland R (2021) Melatonin and Microglia. Int J Mol Sci 22(15):8296. https://doi.org/10.3390/ijms22158296
Knoll R, Schultze JL, Schulte-Schrepping J (2021) Monocytes and Macrophages in COVID-19. Front Immunol 12:720109. https://doi.org/10.3389/fimmu.2021.720109
Tan DX, Reiter RJ (2022) Mechanisms and clinical evidence to support melatonin’s use in severe COVID-19 patients to lower mortality. Life Sci 294:120368. https://doi.org/10.1016/j.lfs.2022.120368
Wieczfinska J, Kleniewska P, Pawliczak R (2022) Oxidative Stress-Related Mechanisms in SARS-CoV-2 Infections. Oxid Med Cell Longev 2022:5589089. https://doi.org/10.1155/2022/5589089
Yang J, Tang Q, Zeng Y (2022) Melatonin: Potential avenue for treating iron overload disorders. Ageing Res Rev 81:101717. https://doi.org/10.1016/j.arr.2022.101717
Nita M, Grzybowski A (2016) The Role of the Reactive Oxygen Species and Oxidative Stress in the Pathomechanism of the Age-Related Ocular Diseases and Other Pathologies of the Anterior and Posterior Eye Segments in Adults. Oxid Med Cell Longev 2016:3164734. https://doi.org/10.1155/2016/3164734
Juan CA, Pérez de la Lastra JM, Plou FJ, Pérez-Lebeña E (2021) The Chemistry of Reactive Oxygen Species (ROS) Revisited: Outlining Their Role in Biological Macromolecules (DNA, Lipids and Proteins) and Induced Pathologies. Int J Mol Sci 22(9):4642. https://doi.org/10.3390/ijms22094642
Chen Q, Wang Q, Zhu J, et al (2018) Reactive oxygen species: key regulators in vascular health and diseases. Br J Pharmacol 175(8):1279–1292
Guan Q, Wang Z, Cao J, et al (2021) Mechanisms of Melatonin in Obesity: A Review. Int J Mol Sci 23(1):218. https://doi.org/10.3390/ijms23010218
Loh D, Reiter RJ (2022) Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19. Int J Mol Sci 23(15):8122. https://doi.org/10.3390/ijms23158122
Reiter R.J, Sharma R, Simko F, et al (2022) Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection. Cell Mol Life Sci 79(3):143. https://doi.org/10.1007/s00018-021-04102-3
Zhang R, Wang X, Ni L, et al (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sci 250:117583. https://doi.org/10.1016/j.lfs.2020.117583
Panara A, Aalizadeh R, Thomaidis NS (2022) Chemical characterisation of Pelargonium sidoides root based on LC-QToF-MS non-target screening strategies. Phytochem Anal 33(1):40–56
Lukman V, Odeyemi SW, Roth RL, et al (2020) Novel kinase platform for the validation of the anti-tubercular activities of Pelargonium sidoides (Geraniaceae). BMC Biotechnol 20(1):50. https://doi.org/10.1186/s12896-020-00643-w
Kolodziej H, Kiderlen AF (2007) In vitro evaluation of antibacterial and immunomodulatory activities of Pelargonium reniforme, Pelargonium sidoides and the related herbal drug preparation EPs 7630. Phytomedicine 14 Suppl 6:18–26
Papies J, Emanuel J, Heinemann N, et al (2021) Antiviral and Immunomodulatory Effects of Pelargonium sidoides DC. Root Extract EPs® 7630 in SARS-CoV-2-Infected Human Lung Cells. Front Pharmacol 12:757666. https://doi.org/10.3389/fphar.2021.757666
Perić A, Vezmar Kovačević S, Barać A, et al (2020) Effects of Pelargonium sidoides extract on chemokine levels in nasal secretions of patients with non-purulent acute rhinosinusitis. J Drug Assess 9(1):145–150
Savickiene N, Jekabsone A, Raudone L, et al (2018) Efficacy of Proanthocyanidins from Pelargonium sidoides Root Extract in Reducing P. gingivalis Viability While Preserving Oral Commensal S. salivarius. Materials (Basel) 11(9): 1499. https://doi.org/10.3390/ma11091499
Gudowska-Sawczuk M, Mroczko B (2022) What Is Currently Known about the Role of CXCL10 in SARS-CoV-2 Infection?. Int J Mol Sci 23(7):3673. https://doi.org/10.3390/ijms23073673
Michaelis M, Doerr HW, Cinatl J Jr (2011) Investigation of the influence of EPs® 7630, a herbal drug preparation from Pelargonium sidoides, on replication of a broad panel of respiratory viruses. Phytomedicine 18(5):384–386
Kamin W, Lehmacher W, Zimmermann A, et al (2022) Treatment of sore throat and hoarseness with Pelargonium sidoides extract EPs 7630: a meta-analysis. Pharmadvances 4(2):88–103
Abacioglu N (1999) A general approach to chronobiology and cardiovascular system rhythms. In: Fundamentals of Chronobiology and Chronotherapy; Abacioglu N, Zegil H (eds) Palme Yayincilik; Ankara, Turkey. pp. 1–14
Shrestha S, Shrestha R, Ahmed A, et al (2022). Impact of pharmacist services on economic, clinical, and humanistic outcome (ECHO) of South Asian patients: a systematic review. J Pharm Policy Pract 15(1):37. https://doi.org/10.1186/s40545-022-00431-1
Mohamed Ibrahim O, Ibrahim RM, Ibrahim YA, et al (2022) Shedding the light on Pharmacists’ roles during COVID-19 global pandemic. Saudi Pharm J 30(1):14–27. https://doi.org/10.1016/j.jsps.2021.12.003
Li H, Zheng S, Li D, et al (2021) The Establishment and Practice of Pharmacy Care Service Based on Internet Social Media: Telemedicine in Response to the COVID-19 Pandemic. Front Pharmacol 12:707442. https://doi.org/10.3389/fphar.2021.707442
Wahab M, Jalani MM, Goh KW, et al (2022) Why Did I Consult My Pharmacist about Herbal and Dietary Supplements? An Online Survey Amid the COVID-19 Pandemic in Malaysia. Int J Environ Res Public Health 19(17):10994. https://doi.org/10.3390/ijerph191710994
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Taner, N. et al. (2023). Chronobiological Efficacy of Combined Therapy of Pelargonium Sidoides and Melatonin in Acute and Persistent Cases of COVID-19: A Hypothetical Approach. In: Guest , P.C. (eds) Application of Omic Techniques to Identify New Biomarkers and Drug Targets for COVID-19. Advances in Experimental Medicine and Biology(), vol 1412. Springer, Cham. https://doi.org/10.1007/978-3-031-28012-2_23
Download citation
DOI: https://doi.org/10.1007/978-3-031-28012-2_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28011-5
Online ISBN: 978-3-031-28012-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)