Abstract
COVID-19 stands for Corona Virus Disease 2019, which starts as a viral infection that provokes illness with different symptoms and severity. The infected individuals can be asymptomatic or present with mild, moderate, severe, and critical illness with acute respiratory distress syndrome (ARDS), acute cardiac injury, and multiorgan failure. When the virus enters the cells, it replicates and provokes responses. Most diseased individuals resolve the problems in a short time but unfortunately, some may die, and almost 3 years after the first reported cases, COVID-19 still kills thousands per day worldwide. One of the problems in not curing the viral infection is that the virus passes by undetected in cells. This can be caused by the lack of pathogen-associated molecular patterns (PAMPs) that start an orchestrated immune response, such as activation of type 1 interferons (IFNs), inflammatory cytokines, chemokines, and antiviral defenses. Before all of these events can happen, the virus uses the infected cells and numerous small molecules as sources of energy and building blocks for newly synthesized viral nanoparticles that travel to and infect other host cells. Therefore, studying the cell metabolome and metabolomic changes in biofluids might give insights into the state of the viral infection, viral loads, and defense response. NMR-metabolomics can help in solving the real-time host interactions by monitoring concentration changes in metabolites. This chapter addresses the state of the art of COVIDomics by NMR analyses and presents exemplified biomolecules identified in different world regions and gravities of illness as potential biomarkers.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Coronaviruses belong to a group of infectious viruses, which infect animals and humans, causing respiratory illness [1, 2]. In December 2019, a new zoonotic coronavirus was reported in Wuhan City, China [2, 3]. This was designated as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causal agent of coronavirus disease 2019 (COVID-19), which is highly transmissible, as seen by its rapid spread all over the world. It was estimated that 17.1 million to 19.6 million people died in 2020 and 2021 due to COVID-19 complications [4]. Even now, the virus is causing infections and deaths although vaccination has mitigated the COVID-19 pandemic situation. There is still the risk of the emergence of new coronavirus variants because low-income and middle-income countries (LMICs) are only partially vaccinated, due to limited access to vaccines or the lack of awareness of the importance of vaccination [5].
The clinical features of COVID-19 are classified into cases with different severity such as asymptomatic, mild disease (fever, fatigue, myalgia, dry cough, sore throat, and headache), moderate (fever greater than 37.8 °C and symptoms of pneumonia), severe (dyspnea and hospitalization in intensive care unit), and critical cases (acute respiratory distress syndrome [ARDS], acute cardiac injury, and multiorgan failure) (Fig. 10.1) [2, 6]. The gravity of the symptoms is linked to age, comorbidities (diabetes, cardiovascular disease, hypertension, and others), genetic factors, unhealthy eating habits, and lifestyle factors, such as the lack of physical exercise [2, 7].
In this sense, it is important to diagnose COVID-19 during the asymptomatic stage or when the first mild symptoms appear because the infected individuals with SARS-CoV-2 in this disease stage are a source of infection [8].
Diverse strategies have been tested and/or used for the discovery of COVID-19 biomarkers to aid in diagnosis [9,10,11], with mass spectrometry and NMR spectroscopy being the most commonly used techniques in COVID-19 metabolomics research [12]. NMR-based metabolomics is an approach that has allowed the identification of biomarkers in different sample types and biological mixtures [13]. Furthermore, NMR spectroscopy is a suitable analytical platform for disease studies, because it is a highly reproducible technique, which can be used in studies that require large-scale and longitudinal research [12, 14].
In addition to the identification of biomarkers for COVID-19 disease severity, NMR spectroscopy has also been used for metabolite quantification [15], evaluation of vaccine effects [16, 17], studies of viral cell shielding [18], identification of the etiological causes of ARDS [19], and monitoring the mental health of patients affected by COVID-19 [20]. In this chapter, we discuss about the COVID-19 severity biomarkers detected by NMR spectroscopy approaches and those found in cardiovascular and thrombosis risks resulting from the disease.
2 Biomarkers of COVID-19 Severity
Since the escalation of the first COVID-19 cases, the scientific community has performed a collective effort to ameliorate the pandemic situation. Omic-based searches have acquired, interpreted, and integrated different data about this concern, which has been named “COVIDomics.” Blood plasma and serum have been mostly used as biological samples in metabolomics studies [21]. Table 10.1 and Fig. 10.1 summarize the metabolites detected by 1H-NMR spectroscopy as biomarkers of different COVID-19 stages.
There are few studies which have used saliva as an NMR sample, which could indicate the nasopharyngeal state of COVID-19 patients [12]. However, there are some limitations to the use of these approaches, such as the low concentration of metabolites (99% water and 1% inorganic and organic compounds), diary fluctuations of metabolite concentrations, and the possible influence of oral injuries. In these cases, it would be necessary to perform metabolomics analyses in an NMR spectrometer with pulsed and magnetic field gradients to improve sensitivity and accuracy [12, 22].
Glutamine deficiency has been reported in severe COVID-19 patients [23, 26, 30]. The acute inflammatory process featured in COVID-19 requires energy from an increase in the concentration of some metabolites of the tricarboxylic acid cycle (TCA), such as glucose and glutamine [31]. When the endogenous synthesis of glutamine is not sufficient to supply all the needs of the infected body, the plasma glutamine levels are reduced [23]. The use of glutamine supplementation has been suggested for COVID-19 patients [30], since glutamine performs important roles in energy metabolism, the immune response, and cytokine production [23, 26].
Like glutamine, glutamate also takes part in energy metabolism, being the first step in glutathione biosynthesis. Furthermore, glutamate and glutamine act in nucleotide biosynthesis as nitrogen donors [26, 30]. In COVID-19, the unregulated glutamate levels in patients with hypoxia may cause neurological abnormalities since glutamate is also an important neurotransmitter [32]. Reductions in glutamine and increased glutamate in blood plasma are associated with health risks [30].
Elevated creatine levels have been associated with muscular energy metabolism in severe COVID-19 patients [15, 23]. Creatine-kinase converts creatine to the energy storage form of phosphocreatine. The high creatine concentration in infected cells is possibly related to the energy consumption changes during viral replication [15], as well as in COVID-19 patients, who spend significant time in the hospital without utilizing muscular energy [23].
Unregulated leucine, isoleucine, and valine concentrations in blood plasma are harmful to the organism, because these compounds may cause inflammation and neurological impact, and promote oxidative stress [23]. Other unregulated amino acid concentrations observed in severe COVID-19 groups include phenylalanine and tyrosine [33]. Barberis et al. observed perturbations in phenylalanine metabolism, arachidonic acid metabolism, and tricarboxylic acid cycle (TCA) in COVID-19 patients [33]. Since this report, the increase in phenylalanine and tyrosine concentrations in blood samples has been reported in a various researches on this issue (Table 10.1). Correia et al. quantified these amino acids and observed that although tyrosine concentration increased with COVID-19 severity, tyrosine levels remained slightly lower than those of phenylalanine during the infection process, which may point to a disturbance in the immune system [15].
The increase in pyruvate levels in blood samples from COVID-19 patients may be related to breathing difficulties felt by these individuals, which decreases the oxygenation rate essential in biochemical processes. In aerobic conditions, pyruvate is converted to lactate and eliminated from the TCA [15]. However, in hypoxic conditions, pyruvate is regulated by anoxic respiration, which increases the NADH concentration. Under these conditions, pyruvate dehydrogenase is allosterically hampered in performing pyruvate oxidation [27].
Pyruvate is not commonly used as a biomarker because it is sensitive to preanalytical procedures [34]. Due to this problem, other methods to monitor COVID-19 have been performed through measurements of lactate or the lactate-to-pyruvate conversion rate, which has been reported as a biomarker of severe respiratory dysfunctions [26]. Hyperlactatemia is featured in sepsis and some damages caused by COVID-19 such as end-organ injury, systemic dysfunctions, ischemia, and thrombosis [35].
Elevated formate levels in plasma and urine samples have been associated with indicators of environmental exposure to contaminants or as biomarkers of impaired one-carbon metabolism [25, 36]. However, in COVID-19 cases, patients with moderate and severe disease may be in isolation or hospitalized. Therefore, they are not likely to be exposed to environmental contaminants. In these cases, formate changes may be related to sarcopenia or kidney damage [25].
It is worth mentioning that acetylated glycoproteins and phospholipids have been reported as changed in COVID-19 and might be considered important inflammatory biomarkers that can be measured in clinics by applying low-field NMR [37]. For instance, N-acetyl signals from glycosylated serum proteins were found to be elevated and phospholipids showed an inverse relationship in COVID-19 patients. Therefore, the phospholipid:acetylated glycoprotein ratio has been suggested as a biomarker for inflammation assessment [26, 37, 38].
Finally, it can be assumed that NMR-monitored metabolic changes during COVID-19 are driven by immune system regulation of key metabolic enzymes by cytokines, the energy consumption of cytokine-secreting cells, or by the effect of immune cells on other tissues [39]. In line with this, altered lipid metabolism has been observed in COVID-19, including effects on cholesterol and cholesterol esters, sphingolipids, and saturated fatty acids (FAs). Furthermore, an increase in the triglyceride levels of lipoproteins with different densities, such as very-low (VLDLs), low- (LDLs), and high-density lipoproteins (HDLs), and the fatty acids (FAs) saturation state have been associated with increased disease severity.
3 Principal Risks Caused by COVID-19
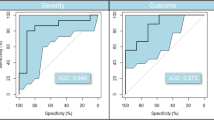
There are many consequences reported in convalescent COVID-19 patients, some of which have been linked to thromboembolic episodes. Therefore, it is crucial to understand in which way COVID and post-COVID syndrome metabolomic and lipidomic alterations are linked to thrombosis. Although NMR studies of blood metabolite alterations in thrombosis have not been thoroughly explored in the literature [40, 41], some works have reported effects on lipids, free fatty acids (FFAs), acylcarnitines, trimethylamine N-oxide, and their involvement in thromboinflammation and platelet dysfunctions [42]. It is also important to note that low-density lipoproteins (LDLs) and their oxidation products (oxLDLs) take part in prothrombotic responses. Another important class of metabolites linked to thrombosis is sterol and derivatives, such as cholesterol and cholesterol esters. Their involvement in thrombosis is expected, as well as other thrombotic risks, such as hypercholesterolemia, the enhanced inflammatory potential of lipid-laden platelets, and changes in circulatory lipids and atherogenic chemokines. Also, imbalances in the ratio of branched-chain amino acids (BCAAs) to alanine, as seen in thrombosis [41], as well as alterations in lipids, acetoacetate, pyruvate, glucose, 3-hydroxybutyrate, lactate, creatine, and phenylalanine [41, 43], might be linked to pathological conditions in thrombosis and have been observed in COVID-19 (Fig. 10.2). Thus, these represent potential biomarker candidates for prediction of thrombotic risk in moderate and severe patients. It is worth mentioning that, of the 20 biomarkers reported for thrombosis, most of them are also increased in COVID-19 patients. In addition, the potential role of platelets beyond thrombosis and hemostasis is coming under increasing attention. It is known that platelets mediate inflammation through interactions with immune cells or cytokine/chemokine secretion [44] and patients affected by COVID-19 have been reported to have micro-thromboses due to altered immune function [45]. Furthermore, pro- and anti-inflammatory lipid mediators may be generated by activated platelets during the inflammation course [42].
Principal risks associated with COVID-19 disease: (a) cardiovascular diseases, (b) pneumonia, (c) diabetes, and (d) thrombosis. The associated metabolites are also indicated by either increased (up, red arrows) or decreased (down, blue arrows) concentrations. Heart, lung, and vein were adapted from link smart.servier.com (free medical images)
Other important roles of platelets in the immune response have been recognized, such as the capacity to guide immune cells to the infected area and in recognizing and neutralizing pathogens. Platelets also play an important role in the coagulation cascade and in resolving bleeding problems during vascular injuries, but their inappropriate activation can cause thrombosis. Many proteins that interact with platelets, such as fibrin and collagen, are also recognized as key players in the clotting process.
Platelets are blood cells that circulate freely till the moment the blood vessel suffers an injury. Then, the platelets organize themselves and initiate clot formation by forming spider-net-like 3D structures with actin and fibrin, which are adhesion matrix proteins with motifs that recognize and stick to the platelets. As stated earlier, platelets also take part in immune responses. For example, CD8+ T-cells which take part in the adaptive immune response are orchestrated by platelets against viral hepatitis [46]. Considering these dual roles, an infection can cause secondary thrombocytosis, a condition marked by increased platelets and thrombosis formation.
During the process of clot formation, platelets participate in the regulation, recruitment, and functions of innate immune cells. As part of this, the platelets release the following mediators: chemokine ligand 1 (CXCL 1), CXCL 3, 5, and 7, and beta-chemokines ligand 5 (CCL 5) and 7, among others that trigger receptors expressed on myeloid cells. There are two families of cytokines which can be distinguished based on the first cysteine residue. The first is the family called CC chemokines, also known as beta-chemokines, and the second is called CXC chemokines, alpha-chemokines, which have an amino acid between the first two cysteines. CC chemokines mainly stimulate monocytes, as well as basophils, eosinophils, T-lymphocytes, and natural killer (NK) cells. On the other hand, CXC chemokines, which primarily stimulate neutrophil chemotaxis, contain a glutamate-leucine-arginine (ELR) sequence at the N-terminus that is essential for receptor binding. These mediators support leukocyte accumulation and promote their microbicidal activity. Furthermore, platelets interact with innate immune cells affecting effector functions such as the formation of extracellular neutrophil trap (NETosis) and cell migration. During the formation of neutrophils and other white blood cells, such cells expel their chromatin content, which participates in the formation of the extracellular fiber network, capturing and eliminating pathogens. So, NETs act in different biological activities through activation and promotion of recruitment of platelets as well as their feedback mechanisms, thus causing a thrombosis [46, 47].
Although NETose is generally associated with responses against extracellular pathogens, there is increasing evidence that NETose also occurs in viral infections [48]. During the COVID-19 pandemic, several reviews cited the formation of NETs as a major defense mechanism [49]. This was especially marked in the cases of ARDS, being easy to identify due to its high presence in plasma [49, 50]; Autopsy of COVID-19 victims also showed a high number of neutrophils [51].
In addition to immunothrombosis, COVID-19 can cause hyperinflammation and hypercoagulopathy [47]. One of the causes of hyperinflammation is ARDS, which is triggered by primary micro-thrombi in the pulmonary vessels, evolving to systemic microangiopathy and can lead to a variety of damaging scenarios in the COVID-19 patient such as the encompassing cardiomyopathy, multiple organ dysfunction syndromes (MODS), hepatic and renal failure, mesenteric ischemia, and neurological dysfunctions (Fig. 10.2) [47]. Another cause of hyperinflammation commonly seen in COVID-19 is the NLRP3 inflammasome activation, which can result in various cardiovascular disorders [52], characterized by increasing concentrations of plasminogen activator inhibitor I (PAI-1), free fatty acids (FFAs), leptin, interleukin-6 (IL-6), and monocyte chemoattractant protein-1 (MCP-1) [53].
The NLRP3 inflammasome (NOD-, LRR-, and pyrin domain-containing protein 3) is a sensor, with an adapter (ASC or PYCARD) and an effector (caspase 1). For example, the protein (NLRP3) that plays an important function is a three-domain ATPase, which also has a purine domain on its amino-terminal, and a carboxy-terminal rich in leucine and arginine residues (LRR domain). Its central domain is an ATPase that is crucial for self-association and function. The final LRR domain is considered important for self-inhibition by reducing the ATPase function and stopping the auto-oligomerization. NLRP3 oligomers recruit ASC using homotypic interactions of the pyrin domain (PYD–PYD interactions) and act through nucleation in the formation of helical ASC filaments, which also occur by PYD–PYD interactions. Then, the multiple ASC filaments coalesce into a macromolecular focus, named the ASC spot. Further, processing between the carboxy-terminal caspase recruitment domain (CARD) and p20 releases p20–p10 from the ASC. The protease activity of the p20-p10 heterotetramer is lost in the cell, due to its instability. Recently, NIMA-related kinase 7 (NEK7), an enzyme that plays a role during the mitosis process, has been reported as an essential enzyme for the NLRP3 inflammasome activation. The assembly of NEK7 leads to caspase 1-dependent release of antibodies (IL-1β and IL-18) and gasdermin D-mediated pyroptosis. Activation of NLRP3 results in several biochemical responses, most of which are not mutually exclusive, including ion efflux (K+ and Cl−), calcium ion flux, metabolic changes, and cellular consequences such as mitochondrial dysfunction, lysosomal disruption, and trans-Golgi disassembly [54].
As explained briefly, blood clotting is a complex process involving an orchestrated and precise action of many proteins such as clotting factors, chemokines, receptors, binding motifs, signaling molecules, and the participation of platelets. Nevertheless, if provoked by inflammation and unchecked by normal feedback mechanisms, enhanced clotting can occur, which can cause severe damage to health and even death, as in embolisms, stroke, or other grave thrombotic events. It appears that in COVID and post-COVID micro-thrombosis, the associated hyperinflammation and altered blood metabolites can drive such undesired and uncontrollable clotting events, leading to thrombosis and potentially fatal outcomes.
4 Conclusions and Perspectives
COVIDomics by NMR has shown significant potential in mapping serum and plasma samples, and some blood metabolites are now being considered as potentially disease-relevant prognostic biomarkers. We have cited the main roles and explored the potential of the most common metabolites described in the recent literature. Among these, the lipoproteins, some lipids, lactate, glucose, aromatic amino acids, and creatine draw the most attention and concerns when disease gravity is discussed. Interestingly, most of the discovered metabolites showed higher concentrations of biofluids in the disease state, which might point to the changing viscosity of the blood and increased ionic force. This suggests that the resulting concentrated blood may lead to an increased risk for coagulation abnormalities and blood clotting dysregulation as shown by the micro-thrombotic events and thromboses in COVID-19.
Alongside mapping blood alterations provoked by COVID-19, there are many efforts to link the disease hallmarks with factors such as the risk of hospitalization and negative outcomes. As NMR-metabolomics is expensive due to equipment costs, and due to practical considerations such as the lack of trained professionals in clinics, the new wave in exploring NMR-metabolomics in COVID-19 research is to design pulse-sequences for low-field and portable NMR types of equipment that trained professionals without a strong background in NMR can use with ease and obtain similar results as with the high-field equipment. The progress in this regard is not only relevant for COVID-19 risks but also for clinical monitoring of other diseases that are still challenged with imprecise or doubtful diagnoses or with difficulties in predicting outcomes or treatment effects.
Another important issue is the critical factor of obtaining reliable samples for NMR analysis and overcoming any bioanalytical drawbacks among the different sample handling and storage steps [49]. This is especially so when the samples in question have a viral and potentially life-threatening origin. Even so, recent procedures have been put in place to overcome these issues [55].
Last, but not least, NMR-metabolomics might shed the light on disease mechanisms and immune response, track early markers of disease severity, and bring insights into treatment effects, among others, therefore enabling us to estimate the recovery or the need for hospitalization. Many benefits of metabolomics by NMR in revealing COVID-19 early markers might positively affect the present and future pandemics, making this exciting research field one of the most important diagnostics and prognostics tools.
References
Newman A, Smith D, Ghai RR, et al (2020) First reported cases of SARS-CoV-2 infection in companion animals - New York, March-April 2020. Morb Mortal Wkly Rep 69(23):710–713
Hu B, Guo H, Zhou P, Shi ZL (2021) Characteristics of SARS-CoV-2 and COVID-19. Nat Rev 19(3):141–154
Wu F, Zhao S, Yu B, et al (2020) A new coronavirus associated with human respiratory disease in China. Nature 579(7798):265–269
COVID-19 Excess Mortality Collaborators (2022) Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet 399(10334):1513–1536
Oliu-Barton M, Pradelski BSR, Algan Y, et al (2022) Elimination versus mitigation of SARS-CoV-2 in the presence of effective vaccines. Lancet Glob Health 10(1):e142-e147
Baj J, Karakuła-Juchnowicz H, Teresínski G, et al (2020) COVID-19: Specific and non-specific clinical manifestations and symptoms: The current state of knowledge. J Clin Med 9(6):1753
Chesnut WM, MacDonald S, Wambier CG (2021) Could diet and exercise reduce risk of COVID-19 syndemic? Med Hypotheses 148:110502
Tan J, Liu S, Zhuang L, et al (2020) Transmission and clinical characteristics of asymptomatic patients with SARS-CoV-2 infection. Future Virol 15(6):373–380
Jalandra R, Yadav AK, Verma D, et al (2020) Strategies and perspectives to develop SARS-CoV-2 detection methods and diagnostics. Biomed Pharmacother 129: 110446
Abid SA, Muneer AA, Al-Kadmy IMS, et al (2021) Biosensors as a future diagnostic approach for COVID-19. Life Sci 273:119117
Nascimento ED, Fonseca WT, Oliveira TR, et al (2022) COVID-19 diagnosis by SARS-CoV-2 spike protein detection in saliva using an ultrasensitive magneto-assay based on disposable electrochemical sensor. Sens Actuators B Chem 353: 131128
Santos Junior GC, Pereira CM, Fidalgo TKS, Valente AP (2020) Saliva NMR-based metabolomics in the war against COVID-19. Anal Chem 92(24):15688–15692
Pontes JGM, Brasil AJM, Cruz GCF, et al (2017) NMR-based metabolomics strategies: plants, animals and humans. Anal Methods 9(7):1078–1096
Emwas AHM, Salek RM, Griffin JL, Merzaban J (2013) NMR-based metabolomics in human disease diagnosis: applications, limitations, and recommendations. Metabolomics 9:1048–1072
Correia BSB, Ferreira VG, Piagge PMFD, et al (2022) 1H qNMR-based metabolomics discrimination of COVID-19 severity. J Proteome Res 21(7):1640–1653
Ali S, Nedvědová S, Badshah G, et al (2022) NMR spectroscopy spotlighting immunogenicity induced by COVID-19 vaccination to mitigate future health concerns. Curr Res Immunol 3:199–214
Dagla I, Iliou A, Benaki D, et al (2022) Plasma metabolomic alterations induced by COVID-19 vaccination reveal putative biomarkers reflecting the immune response. Cells 11(7):1241
Stanisic D, Cruz GCF, Elias LA, et al (2022) High-Resolution Magic-Angle Spinning NMR spectroscopy for evaluation of cell shielding by virucidal composites based on biogenic silver nanoparticles, flexible cellulose nanofibers and graphene oxide. Front Bioeng Biotechnol 10:858156
Lorente JA, Nin N, Villa P, et al (2021) Metabolomic differences between COVID-19 and H1N1 influenza induced ARDS. Crit Care 25(1):390
Yang L, Zhou M, Li L, et al (2021) Characteristics of mental health implications and plasma metabolomics in patients recently recovered from COVID-19. Transl Psychiatry 11(1):307
Costanzo M, Caterino M, Fedele R, et al (2022) COVIDomics: The proteomic and metabolomic signatures of COVID-19. Int J Mol Sci 23(5):2414
Mussap M, Fanos V (2021) Could metabolomics drive the fate of COVID-19 pandemic? A narrative review on lights and shadows. Clin Chem Lab Med 59(12):1891–1905
Baranovicova E, Bobcakova A, Vysehradsky R, et al (2021) The ability to normalise energy metabolism in advanced COVID-19 disease seems to be one of the key factors determining the disease progression - A metabolomic NMR study on blood plasma. Appl Sci 11:4231
Masuda R, Lodge S, Nitschke P, et al (2021) Integrative modeling of plasma metabolic and lipoprotein biomarkers of SARS-CoV‑2 infection in Spanish and Australian COVID-19 patient cohorts. J Proteome Res 20(8):4139–4152
Marhuenda-Egea FC, Narro-Serrano J, Shalabi-Benavent MJ, et al (2022) Focusing on the metabolic changes caused by the COVID-19 disease. A Metabolomic approach using urine. Res Square 1(3):1–18
Kimhofer T, Lodge S, Whiley L, et al (2020) Integrative modeling of quantitative plasma lipoprotein, metabolic, and amino acid data reveals a multiorgan pathological signature of SARS-CoV‑2 infection. J Proteome Res 19(11):4442–4454
Bizkarguenaga M, Bruzzone C, Gil-Redondo R, D et al (2022) Uneven metabolic and lipidomic profiles in recovered COVID-19 patients as investigated by plasma NMR metabolomics. NMR Biomed 35(2):e4637
Luporini RL, Pott-Junior H, Di Medeiros Leal MCB, et al (2021) Phenylalanine and COVID-19: Tracking disease severity markers. Int Immunopharmacol 101 (Pt A):108313
Ghini V, Meoni G, Pelagatti L, et al (2022) Profiling metabolites and lipoproteins in COMETA, an Italian cohort of COVID-19 patients. PLOS Pathog 18(4):1010443
Matsuyama T, Yoshinaga SK, Shibue K, Mak TW (2021) Comorbidity-associated glutamine deficiency is a predisposition to severe COVID-19. CDD Press 28(12):3199–3213
Shah AM, Wang Z, Ma J (2021) Glutamine metabolism and its role in immunity, a comprehensive review. Animals 11(2):905
Páez-Franco JC, Torres-Ruiz J, Sosa-Hernández VA, et al (2021) Metabolomics analysis reveals a modified amino acid metabolism that correlates with altered oxygen homeostasis in COVID‑19 patients. Sci Rep 11(1):6350
Barberis E, Timo S, Amede E, et al (2020) Large-scale plasma analysis revealed new mechanisms and molecules associated with the host response to SARS-CoV-2. Int J Mol Sci 21(22):8623
Meoni G, Ghini V, Maggi L, et al (2021) Metabolomic/lipidomic profiling of COVID-19 and individual response to tocilizumab. PLOS Pathog 17(2):e1009243
Carpenè G, Onorato D, Nocini R, et al (2022) Blood lactate concentration in COVID-19: a systematic literature review. Clin Chem Lab Med 60(3):332–337
Lamarre SG, Morrow G, Macmillan L, et al (2013) Formate: an essential metabolite, a biomarker, or more? Clin Chem Lab Med. 51(3):571–578
Nitschke P, Lodge S, Hall D, et al (2022) Direct low field J-edited diffusional proton NMR spectroscopic measurement of COVID-19 inflammatory biomarkers in human serum. Analyst 147(19):4213–4221
Lodge S, Nitschke P, Kimhofer T, et al (2021) NMR spectroscopic windows on the systemic effects of SARS-CoV‑2 infection on plasma lipoproteins and metabolites in relation to circulating cytokines. J Proteome Res 20(2):1382–1396
Rendeiro AF, Vorkas CK, Krumsiek J, et al (2022) Metabolic and immune markers for precise monitoring of COVID-19 severity and treatment. Front Immunol. 12:809937
Quintero M, Tasic L, Annichino-Bizzacchi JM (2020) Thrombosis: Current knowledge based on metabolomics by nuclear magnetic resonance (NMR) spectroscopy and mass spectrometry (MS). Thrombosis Update 1:100011.
Quintero-Escobar M, Tasic L, Costa TBBCD, et al (2021) Serum metabolic profiles based on Nuclear Magnetic Resonance Spectroscopy among patients with deep vein thrombosis and healthy controls. Metabolites 11(12):874
Chatterjee M (2022) Platelet lipidome: Dismantling the "Trojan horse" in the bloodstream. J Thromb Haemost 18(3):543–557
Cao J, Jin Qq, Wang GM, et al (2018) Comparison of the serum metabolic signatures based on 1H NMR between patients and a rat model of deep vein thrombosis. Sci Rep 8(1):7837
Martinod K, Deppermann C (2021) Immunothrombosis and thromboinflammation in host defense and disease. Platelets 32(3):314–324
Bonaventura A, Vecchié A, Dagna L, et al (2021) Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol 21(5):319–329
Gaertner F, Massberg S (2016) Blood coagulation in immunothrombosis—At the frontline of intravascular immunity. Semin Immunol 28(6):561–569
Henry BM, Vikse J, Benoit S, et al (2020) Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: a novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. Clin Chim Acta 507:167–173
Schönrich G, Raftery MJ (2016) Neutrophil extracellular traps go viral. Front Immunol. 7:366
Loo J, Spittle DA, Newnham M (2021) COVID-19, immunothrombosis and venous thromboembolism: biological mechanisms. Thorax 76(4):412–420
Middleton EA, He XY, Denorme F, et al (2020) Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood 136(10):1169–1179
Fang XZ, Wang YX, Xu JQ, et al (2021) Immunothrombosis in acute respiratory dysfunction of COVID-19. Front Immunol. 12:651545
Gedefaw L, Ullah S, Leung PHM, et al (2021) Inflammasome activation-induced hypercoagulopathy: Impact on cardiovascular dysfunction triggered in COVID-19 patients. Cells 10(4):916
Pasquarelli-do-Nascimento G, Braz-de-Melo HA, Faria SS, et al (2020) Hypercoagulopathy and adipose tissue exacerbated inflammation may explain higher mortality in COVID-19 patients with obesity. Front Endocrinol. 11:530
Swanson KV, Deng M, Ting JPY (2019) The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 19(8):477–489
Loo RL, Lodge S, Kimhofer T, Bong SH et al (2020) Quantitative in-vitro diagnostic NMR spectroscopy for lipoprotein and metabolite measurements in plasma and serum: Recommendations for analytical artifact minimization with special reference to COVID-19/SARS-CoV-2 samples. J Proteome Res. Nov 19(11):4428–4441.
Acknowledgements
The authors would like to acknowledge the funding from the Sao Paulo Research Foundation (FAPESP) grants #2018/24069-3 and # 2014/50867-3 (INCTBio), National Council for Scientific and Technological Development (CNPq #401256/2020-0), and Higher Education Personnel Improvement Coordination (CAPES, Finance Code 001). We thank Guilherme Crispim de Faria Cruz and Abstract Science for the graphical design.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
de Moraes Pontes, J.G., dos Santos, R.V., Tasic, L. (2023). NMR-Metabolomics in COVID-19 Research. In: Guest , P.C. (eds) Application of Omic Techniques to Identify New Biomarkers and Drug Targets for COVID-19. Advances in Experimental Medicine and Biology(), vol 1412. Springer, Cham. https://doi.org/10.1007/978-3-031-28012-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-28012-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28011-5
Online ISBN: 978-3-031-28012-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)