Abstract
Gastric cancer is the fifth most common type of cancer and the fourth leading cause of cancer-related death; nevertheless, genetic predisposition to this malignancy is still widely unexplored.
Besides hereditary diffuse gastric cancer (HDGC), associated with germline CDH1 and CTNNA1 pathogenic variants, other genetic syndromes characterized by high risk to develop gastric cancer have been described, encompassing gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS), associated with germline genetic variants in the APC promoter, and familial intestinal gastric cancer (FIGC), still lacking a clear genetic cause.
Moreover, gastric cancer risk is associated with pathogenic variants in genes involved in DNA mismatch repair, such as MLH1 and MSH2 (Lynch syndrome), apoptosis, including TP53 (Li-Fraumeni syndrome) and double-strand break repair, such as BRCA1/BRCA2 and PALB2 (hereditary breast and ovarian cancer syndrome).
Furthermore, gastric cancer can be a manifestation of gastrointestinal polyposis syndromes, such as those associated with APC (familial adenomatous polyposis), MUTYH (MUTYH-associated polyposis), BMPR1A/SMAD4 (juvenile polyposis syndrome), STK11 (Peutz-Jeghers syndrome), and PTEN (Cowden syndrome) genes.
Recent advances in molecular techniques, such as next-generation sequencing, led to the identification of many new genes involved in the predisposition to gastric cancer, some of which are low or moderate penetrant that predispose to other syndromes.
Consequently, in patients with early onset gastric cancer and/or strong gastric cancer family history, the use of multigene panel testing should be considered in cancer risk assessment, including different surveillance recommendations for each syndrome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Familial predisposition to gastric cancer (GC) has been categorized into three main syndromes with primary predisposition to the stomach: (1) hereditary diffuse gastric cancer (HDGC), (2) familial intestinal gastric cancer (FIGC), and (3) gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS). While tumor burden and main genetic causality are established for HDGC (CDH1, CTNNA1) and GAPPS (APC), FIGC remains genetically unexplained and understudied. Nevertheless, other genes that predispose for other cancer syndromes encompass GC within their tumor spectrum: (1) MLH1, MSH2, MSH6, and PMS2 (Lynch syndrome, LS, or hereditary nonpolyposis colorectal cancer, HNPCC), (2) TP53 (Li-Fraumeni syndrome, LFS), (3) BRCA1, BRCA2, and PALB2 (hereditary breast and ovarian cancer, HBOC), (4) APC (familial adenomatous polyposis, FAP), (5) MUTYH (MUTYH-associated polyposis, MAP), (6) BMPR1A and SMAD4 (juvenile polyposis syndrome, JPS), (7) STK11 (Peutz-Jeghers syndrome, PJS), and (8) PTEN (PTEN Hamartoma Tumor syndrome, PHTS) (Table 7.1) [1].
2 HDGC
Pathogenic or likely pathogenic variants in CDH1 predispose to HDGC, an autosomal dominant syndrome characterized by diffuse gastric cancer (DGC) and lobular breast cancer (LBC) [2].
In recent years, next-generation sequencing (NGS) approaches have evolved exponentially, leading to the identification of new genes in HDGC. In 2013, the first germline truncating variant in CTNNA1, encoding the α-E-catenin protein, was described in an HDGC family [3]. To date, and after multiple HDGC families being identified to carry CTNNA1 truncating variants, CTNNA1 remains the only gene, besides CDH1, clearly associated with the HDGC syndrome [4, 5]. Germline mutations in MAP3K6 and MYD88 have also been reported in HDGC families [6, 7]; however, the specific role of these genes remains unclear and their involvement in GC predisposition is still questionable [4]. In 2015, a targeted analysis with a panel of 55 cancer-related genes performed on 144 CDH1-negative cases found candidate mutations in 16 probands (11%), including high and moderate penetrance mutations in CTNNA1, BRCA2, STK11, SDHB, PRSS1, ATM, MSR1, and PALB2 [8]. Very recently, a whole exome analysis on 54 CDH1-negative GC patients did not identify obvious candidates for GC predisposition [9], while, a gene panel-based analysis of 333 HDGC and non-HDGC cases identified 11 mutation carriers of PALB2, BRCA1, and RAD51C, which are genes involved in DNA homologous recombination (HR) [10]. A recent meta-analysis, performed on NGS published data, identified a list of genes carrying deleterious variants in families meeting the 2020 HDGC clinical criteria [11]. Pathogenic or likely pathogenic variants were found in candidate genes involved in DNA damage response pathways [11], encompassing ATM [12, 13], BRCA1 [13], BRCA2 [8, 13], PALB2 [8, 10, 13, 14], RAD51C [10], and ATR [14]. In fact, PALB2 and ATM were the most frequently mutated genes in the HDGC setting [11]. The former has been extensively associated with breast cancer predisposition [15], while the latter has been associated with both breast and gastric cancer susceptibility [16, 17]. Interestingly, PALB2 loss of function variants have been shown to be enriched in the HDGC setting, compared to the general population [14]. While PALB2 association with HDGC holds promise, ATM pleiotropy prevents a clear association with this disease.
3 GAPPS
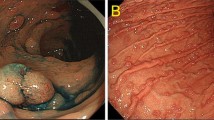
In 2012, GAPPS, was described as an autosomal dominant syndrome [18]. The key clinical features of GAPPS include fundic gland polyposis (FGP) of the stomach with occasional hyperplastic and adenomatous polyps, focal foveolar-type dysplasia, hyperproliferative aberrant pits and development of adenomas with gastric type dysplasia or intestinal-/mixed-type gastric adenocarcinoma [18, 36, 37]. Current diagnostic criteria are depicted in Table 7.2 [36, 38].
In 2016, linkage analysis on six selected families mapped the gene to the 5q22 chromosomal region. Through Sanger sequencing, point mutations in APC promoter 1B, that co-segregated with the disease in all three families, were identified [38, 39]. Therefore, GAPPS is considered a part of a broad phenotypic spectrum of inherited polyposis associated with APC germline defects, but with tropism to the stomach (see paragraph “Familial Adenomatous Polyposis”). Since then, 12 additional families were found to harbor APC promoter 1B single nucleotide variants (SNVs) [40,41,42,43]. Two SNVs were found co-segregating within a family with severer phenotype, but their individual contribution remains unclear [38].
GAPPS phenotypes are diverse among individuals, in the number of polyps, from 30 to hundreds and GC age of onset ranging from 23 to 75 years of age [18, 43]. In fact, third-generation individuals display a much severer phenotype than first-generation obligated carriers [18]. Altogether, these observations suggest incomplete penetrance of APC promoter 1B SNVs that may be aggravated by environmental factors and moderate/low penetrance variants. Risk to develop intestinal- or mixed-type GC is 13% (Table 7.1) [18].
Surveillance of GAPPS families includes endoscopic surveillance with biopsies and prophylactic gastrectomy, due to a rapid malignant progression of FGP [18, 40, 43].
4 FIGC
FIGC is the HDGC counterpart that predisposes to intestinal-type gastric cancer (IGC). Current clinical criteria have been defined by the international gastric cancer linkage consortium (IGCLC) in 1999, depending on the GC incidence in the population and are depicted in Table 7.3 [44, 45]. Countries with a high GC incidence, such as Japan and Portugal, should use criteria analogous to those proposed for Lynch syndrome [46], while in countries with a low GC incidence, including USA and UK, FIGC selection criteria are more restrictive.
To date, no germline defects have been found to be recurrently associated with FIGC predisposition, which currently has unknown age of onset, tumor spectrum, and penetrance. Thus, clinical criteria have not been updated or validated since firstly described in 1999 [44]. Recently, the average IGC age of onset in FIGC families was found to be 10 years earlier than observed for the sporadic setting [19]. At the somatic level, TP53, BRCA2, ATM, FOXF1, FHIT, SDHB, MSH6, CTNNA1, and PXN were found mutated at higher frequencies in tumors from FIGC patients than in sporadic IGC, which also correlates with increased MSI frequency. The FIGC tumor spectrum is broad and predisposes to IGC, but also to colorectal and breast cancer, at lower frequencies [19]. A recent meta-analysis found BRCA2 as the most frequently mutated gene in the germline DNA of FIGC probands, reaching 17% [11], a frequency that was similar to that of BRCA2 somatic variants in sporadic IGC (9%) and higher than that of sporadic DGC (5%) [47].
Carvalho and colleagues [19] hint toward FIGC as a polygenic syndrome, since germline defects in major genes were not found in a large FIGC cohort. These authors also proposed redefinition of clinical criteria for FIGC to at least 2 GC cases diagnosed at any age, with one histologically confirmed as IGC [19].
Considering the number of genes that can be involved in this disease, the lifetime GC risk is not easy to determine due to the high genetic variability (Table 7.1).
Current surveillance is evaluated and applied on a case-by-case basis, yet recommendations include endoscopy in first-degree relatives, 10 years earlier than the earliest IGC age of onset [48], or gastroduodenoscopy at 40 years of age or 5 years earlier than the youngest IGC diagnosed in the family [49]. Eradication of H. pylori infection is recommended in FIGC families, due to its high frequency in this setting [49].
5 Non-polyposis Syndromes
5.1 Lynch Syndrome
Lynch syndrome (LS) predisposes to colorectal and endometrial cancers and follow an autosomal dominant inheritance pattern [50]. LS is caused by pathogenic variants in MLH1, MSH2, MSH6, and PMS2, that encode the DNA mismatch repair (MMR) proteins [51], or by large deletions of the EPCAM gene, located upstream of MSH2 [52]. MMR proteins work in a coordinated mode to repair the DNA mismatches that arise during DNA replication and recombination [53].
LS patients also have an increased risk of developing other tumors [54, 55], encompassing a lifetime risk to develop gastric cancer, estimated to be 1–10%, according to the altered gene (Table 7.1).
Regarding GC surveillance, LS patients with an MLH1/MSH2 pathogenic variant, a family history of GC, and other risk factors should undergo upper endoscopy every 3–5 years beginning at age 40 [24].
Moreover, patients with LS, who have a deficiency of the MMR system (dMMR), can benefit from chemoprevention based on the daily use of aspirin [56] and, in case MSI cancers develop, may be treated with anti-PD-1/PD-L1 therapy [57, 58].
5.2 Li-Fraumeni Syndrome
The TP53 gene is located on chromosome 17p13.1 and encodes the p53 protein, a tumor suppressor that responds to different cellular stresses to regulate expression of target genes, thereby inducing cell cycle arrest, apoptosis, senescence, DNA repair, or metabolism changes [59]. Due to its crucial function in maintaining the genomic stability, p53 has been defined as “the guardian of the genome” and, indeed, TP53 somatic alterations are present in approximately 50% of sporadic tumors [60], conferring to p53 an important role as a biomarker for the diagnosis, tumor progression, poor prognosis, and reduced sensitivity for anticancer drugs [61].
Germline pathogenic variants in the TP53 gene are associated with Li-Fraumeni syndrome (LFS), a rare autosomal dominant disorder characterized by a high predisposition to several types of cancer, such as brain tumors, breast cancer, sarcomas, acute leukemia, and adrenocortical tumors [28, 62,63,64,65,66,67,68,69,70,71].
The lifetime risk of GC for patients with LFS, although not consensual, has been estimated to be 2–5% (Table 7.1) [28, 72, 73].
Given the risk of developing gastrointestinal cancers, the guidelines suggest that LFS patients should undergo upper endoscopy and colonoscopy every 2–5 years starting from age 25 years [29]. Moreover, in children, the recommendations are to perform clinical examination and abdominal ultrasound every 6 months, annual whole-body MRI, and brain MRI from the first year of life, if the TP53 variant is known to be associated with childhood cancers. In adults, the surveillance should include every year clinical examination, whole-body MRI, breast MRI in females from 20 until 65 years, and brain MRI until 50 years [63].
5.3 BRCA1- and BRCA2-Associated Hereditary Breast and Ovarian Cancer
The BRCA1 gene, located on chromosome 17q21.31, encodes a nuclear protein involved in DNA repair, cell cycle checkpoint control, and maintenance of genomic stability forming a large multi-subunit protein complex known as BRCA1-associated genome surveillance complex (BASC) [74,75,76,77].
The BRCA2 gene is located on chromosome 13q13.1 and encodes a nuclear protein involved in repairing damaged DNA, recruiting the recombinase RAD51 to the DNA double-strand breaks (DSBs) through the formation of a BRCA1-PALB2-BRCA2 complex [74, 75, 78, 79].
Germline pathogenic variants in BRCA1 and BRCA2 genes are associated with the hereditary breast and ovarian cancer (HBOC) syndrome [80], characterized by a high risk of developing breast and ovarian cancer in females [81,82,83], breast and prostate cancer in males [84,85,86,87] and pancreatic cancer in both sexes [88,89,90].
Further, BRCA1 pathogenic variants have been associated with an increased risk of colon cancer [91] and BRCA2 pathogenic variants have been associated with uveal melanoma [92, 93].
Recently, pathogenic variants in BRCA1/2 and other genes involved in breast/ovarian cancer predisposition have been associated with an increased GC risk [8, 10, 12,13,14]. The IGC risk is estimated to be 2% in BRCA1/2 pathogenic variant carriers (Table 7.1) [30], however prevention should be evaluated on the basis of family history [24].
Moreover, the discovery of the therapeutic potential of inhibitors of the poly adenosine-diphosphate ribose polymerase (PARP) in carriers of germline/somatic BRCA1/2 pathogenic variants with ovarian, breast, prostate, and pancreatic cancers led to a revolution in the treatment of these tumors [94,95,96,97,98,99,100]. PARP inhibitors have shown their efficacy also in patients with pathogenic variants in genes involved in the HR pathway [101,102,103,104]. These results pave the way for the future use of PARP inhibitors in all tumors with a deficiency of the HR system, independently of the germline or somatic nature of the alteration, including GC [105].
6 Polyposis Syndromes
6.1 Familial Adenomatous Polyposis
The APC protein is a tumor suppressor that acts as a Wnt signaling antagonist, and regulates transcriptional activation, cell migration and apoptosis [106]. Pathogenic or likely pathogenic alterations in the APC gene (chromosome 5q22.2) predispose to familial adenomatous polyposis (FAP) [107, 108]. This autosomal dominant syndrome is characterized by polyposis and carcinomas in the gastrointestinal tract, as well as, extra-gastrointestinal carcinomas, such as thyroid [34]. While classical FAP predisposes to hundreds to thousands of colonic and rectal polyps that may develop into colorectal carcinoma, attenuated FAP (AFAP) displays a much milder phenotype [34, 109]. Families with AFAP present fewer and latter-onset of both polyps and carcinomas, as well as cancer-decreased risk [110]. The phenotype severity is dependent on the mutation location within the APC gene [111], as above mentioned for GAPPS with unique predisposition to the stomach [38].
FAP and AFAP also predispose to gastric polyps in >60% and 93% of patients, respectively [112]. However, gastric adenocarcinoma risk ranges between 4% and 7% in the Asian population, with no increased risk for the western population (Table 7.1) [24, 31]. In fact, FGP and focal low-grade dysplasia in the stomach commonly do not undergo malignant transformation [113, 114]. Nevertheless, increased risk is observed in the presence of FGP stomach carpeting, polyps larger than 20 mm, tubular adenomas, high-grade dysplasia polyps, pyloric gland adenomas, and in specific geographical areas [31, 115, 116]. According to these high-risk features and family history, specialized surveillance or gastrectomy may be recommended [24].
6.2 MUTYH-Associated Polyposis
The MUTYH gene is located on chromosome 1p34.1 and encodes the MutY DNA glycosylase, involved in oxidative DNA damage repair and, if unrepaired, apoptosis signaling [117].
MUTYH-associated polyposis (MAP) distinguishes from (A)FAP by presenting a recessive inheritance pattern with reduced risk for colonic and duodenal adenomas (fewer than 100) and carcinomas (5%). Thus, biallelic pathogenic or likely pathogenic variants in MUTYH (chromosome 1p34.1) predispose to MAP [118]. Risk to develop IGC ranges from 2% for females to 4% for males (Table 7.1) [32].
Current surveillance measurements include upper endoscopy and side viewing duodenoscopy every 3 months to 4 years beginning at age 30–35 years with subsequent follow-up based on initial findings [24, 119, 120].
6.3 Juvenile Polyposis Syndrome
The BMPR1A gene, located on chromosome 10q23.2, encodes the bone morphogenetic protein receptor type IA, a transmembrane serine/threonine kinase that binds members of the TGF-β superfamily and plays a role in signal transduction, apoptosis and cell differentiation [121].
The SMAD4 gene (chromosome 18q21.2) encodes a member of the Smad family of signal transduction proteins that are activated by transmembrane serine-threonine receptor kinases in response to TGF-β and bone morphogenetic protein signaling pathways. SMAD4 is a transcription factor that acts as a tumor suppressor and inhibits epithelial cell proliferation [122].
Germline pathogenic variants in BMPR1A and SMAD4 genes are associated with juvenile polyposis syndrome (JPS), an autosomal dominant disorder, that predisposes to hamartomatous polyps in the gastrointestinal tract, specifically in the stomach, small intestine, colon, and rectum [123].
The majority of juvenile polyps are benign, however can undergo malignant transformation. Lifetime estimates of developing gastrointestinal cancers in families with JPS range from 11% to 86%, with variability by region, time period included, and associated gene [124,125,126,127,128]. In fact, approximately 15% of JPS individuals develop cancer [127, 129]. While, the GC incidence is approximately around 10–30% in JPS patients with gastric polyps (Table 7.1) [130, 131], the risk of colorectal cancer ranges between 17% and 22% by 35 years of age and approaches 68% by 60 years of age [132]. In JPS context, small bowel and pancreatic cancers have also been reported [133,134,135,136,137]. Individuals with SMAD4-related JPS are more likely to have a personal or family history of upper gastrointestinal polyps than individuals with a BMPR1A pathogenic variant. The gastric phenotype in individuals with a SMAD4 pathogenic variant tends to be more aggressive with significant polyposis, anemia, and a higher GC risk [125, 127, 128].
According to the clinical practice guidelines for JPS, the gastric surveillance recommended for individuals with a BMPR1A or SMAD4 pathogenic variant includes colonoscopy and upper endoscopy every 3 years beginning at age 15 or earlier if symptomatic. If polyps are found, after polyp treatment an annual screening is recommended until no polyps are found, followed by a screening every 3 years [24, 138, 139].
6.4 Peutz-Jeghers Syndrome
The STK11 gene (formerly LKB1) is located on chromosome 19p13.3 and encodes a serine/threonine kinase that acts as a tumor suppressor, regulating energy metabolism and cell polarity [140].
Germline pathogenic variants in the STK11 gene are associated with Peutz-Jeghers syndrome (PJS), an autosomal dominant syndrome. PJS is characterized by melanocytic macules of the lips, buccal mucosa and digits, multiple gastrointestinal hamartomatous polyps, and an increased risk for different tumors, encompassing colorectal, gastric, pancreatic, breast, and ovarian cancers [141].
In STK11 pathogenic variant carriers, the lifetime GC risk is estimated to be 29% (Table 7.1) [33, 34, 142, 143]. For this reason, the clinical guidelines suggest that PJS patients should undergo upper endoscopy with polypectomy every 2–3 years, starting at the age of 18; shorter intervals may be indicated based on polyp size, number, and pathology [24].
6.5 PTEN Hamartoma Tumor Syndrome
The PTEN gene (chromosome 10q23.31) encodes a phosphatase which antagonizes the PI3K signaling pathway and negatively regulates the MAPK pathway [144].
Germline pathogenic variants in PTEN are associated with the PTEN hamartoma tumor syndrome (PHTS) that includes Cowden syndrome, Bannayan-Riley-Ruvalcaba syndrome, PTEN-related Proteus syndrome, and PTEN-related proteus-like syndrome [145].
Cowden syndrome (CS) is an autosomal dominant disorder that predisposes to benign hamartomas and increased lifetime risk of breast, thyroid, uterine, colorectal, and other cancers, including stomach [145,146,147]. Upper or lower gastrointestinal polyps occur in more than 90% of individuals with a PTEN pathogenic variant [148]. In the stomach, the most common findings are hyperplastic polyps, hamartomas, and ganglioneuromas [149,150,151].
Cowden syndrome does not have increased risk of gastric malignancy (Table 7.1); however, complications of benign neoplasm can occur [35]. Indeed, some CS patients have symptoms including hemorrhage, obstruction, and pain [35]. According to the guidelines, PHTS patients should undergo upper and lower endoscopy with removal of polyps beginning at age 35 years with frequency dependent on degree of polyposis identified [145].
7 Conclusions
GC is one of the most common and deadly tumors and, among risk factors for the development of this cancer, genetic predisposition plays an important role.
Besides HDGC, associated with CDH1 and CTNNA1 pathogenic variants, other genetic syndromes characterized by high risk to develop GC have been described: GAPPS, associated with genetic variants in the APC promoter, and FIGC, still lacking a clear genetic cause.
In addition to these three syndromes, genes including TP53, BRCA1/2, and MMR genes, whose variants are associated with other cancer genetic syndromes, also include an increased risk for GC (Table 7.1).
Moreover, genes associated with the development of gastrointestinal polyps, such as APC, MUTYH, BMPR1A, SMAD4, STK1, and PTEN may also evolve in GC (Table 7.1).
The evidence of GC risk associated with these syndromes and the availability of recommendations for the management of variant carriers suggest that these genes should be included in a gene panel for the identification of patients at risk of developing GC.
In summary, new genes are constantly emerging from NGS studies, showing that GC predisposition is distributed over several genes, with only a small portion of genes being recurrently mutated.
These findings address the choice of wide panels, including the genes involved in the main cancer syndromes. This creates new diagnostic opportunities but also increases the risk of an incorrect genetic diagnosis [152]. Importantly, the identification of a pathogenic germline variant can not only guide the choice of the best chemoprevention and prophylactic surgeries but also the choice of novel targeted therapies, toward personalized medicine based on the genetic characteristics of each patient.
References
van der Post RS, Vogelaar IP, Carneiro F et al (2015) Hereditary diffuse gastric cancer: updated clinical guidelines with an emphasis on germline CDH1 mutation carriers. J Med Genet 52:361–374. https://doi.org/10.1136/jmedgenet-2015-103094
Guilford P, Hopkins J, Harraway J et al (1998) E-cadherin germline mutations in familial gastric cancer. Nature 392:402–405. https://doi.org/10.1038/32918
Majewski IJ, Kluijt I, Cats A et al (2013) An α-E-catenin (CTNNA1) mutation in hereditary diffuse gastric cancer. J Pathol 229:621–629. https://doi.org/10.1002/path.4152
Weren RDA, van der Post RS, Vogelaar IP et al (2018) Role of germline aberrations affecting CTNNA1, MAP3K6 and MYD88 in gastric cancer susceptibility. J Med Genet 55:669–674. https://doi.org/10.1136/jmedgenet-2017-104962
Lobo S, Benusiglio PR, Coulet F et al (2021) Cancer predisposition and germline CTNNA1 variants. Eur J Med Genet 64:104316. https://doi.org/10.1016/j.ejmg.2021.104316
Gaston D, Hansford S, Oliveira C et al (2014) Germline mutations in MAP3K6 are associated with familial gastric cancer. PLoS Genet 10:e1004669. https://doi.org/10.1371/journal.pgen.1004669
Vogelaar IP, Ligtenberg MJL, van der Post RS et al (2016) Recurrent candidiasis and early-onset gastric cancer in a patient with a genetically defined partial MYD88 defect. Familial Cancer 15:289–296. https://doi.org/10.1007/s10689-015-9859-z
Hansford S, Kaurah P, Li-Chang H et al (2015) Hereditary diffuse gastric cancer syndrome: CDH1 mutations and beyond. JAMA Oncol 1:23–32. https://doi.org/10.1001/jamaoncol.2014.168
Vogelaar IP, van der Post RS, van Krieken JHJ et al (2017) Unraveling genetic predisposition to familial or early onset gastric cancer using germline whole-exome sequencing. Eur J Hum Genet 25:1246–1252. https://doi.org/10.1038/ejhg.2017.138
Sahasrabudhe R, Lott P, Bohorquez M et al (2017) Germline mutations in PALB2, BRCA1, and RAD51C, which regulate DNA recombination repair, in patients with gastric cancer. Gastroenterology 152:983–986.e6. https://doi.org/10.1053/j.gastro.2016.12.010
Garcia-Pelaez J, Barbosa-Matos R, São José C et al (2022) Gastric cancer genetic predisposition and clinical presentations: established heritable causes and potential candidate genes. Eur J Med Genet 65:104401. https://doi.org/10.1016/j.ejmg.2021.104401
Slavin T, Neuhausen SL, Rybak C et al (2017) Genetic gastric cancer susceptibility in the international clinical cancer genomics community research network. Cancer Genet 216–217:111–119. https://doi.org/10.1016/j.cancergen.2017.08.001
Tedaldi G, Pirini F, Tebaldi M et al (2019) Multigene panel testing increases the number of loci associated with gastric cancer predisposition. Cancers (Basel) 11. https://doi.org/10.3390/cancers11091340
Fewings E, Larionov A, Redman J et al (2018) Germline pathogenic variants in PALB2 and other cancer-predisposing genes in families with hereditary diffuse gastric cancer without CDH1 mutation: a whole-exome sequencing study. Lancet Gastroenterol Hepatol 3:489–498. https://doi.org/10.1016/S2468-1253(18)30079-7
Antoniou AC, Casadei S, Heikkinen T et al (2014) Breast-cancer risk in families with mutations in PALB2. N Engl J Med 371:497–506. https://doi.org/10.1056/NEJMoa1400382
Helgason H, Rafnar T, Olafsdottir HS et al (2015) Loss-of-function variants in ATM confer risk of gastric cancer. Nat Genet 47:906–910. https://doi.org/10.1038/ng.3342
Moslemi M, Moradi Y, Dehghanbanadaki H et al (2021) The association between ATM variants and risk of breast cancer: a systematic review and meta-analysis. BMC Cancer 21:27. https://doi.org/10.1186/s12885-020-07749-6
Worthley DL, Phillips KD, Wayte N et al (2012) Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS): a new autosomal dominant syndrome. Gut 61:774–779. https://doi.org/10.1136/gutjnl-2011-300348
Carvalho J, Oliveira P, Senz J et al (2020) Redefinition of familial intestinal gastric cancer: clinical and genetic perspectives. J Med Genet 58:1. https://doi.org/10.1136/jmedgenet-2019-106346
Cheng L, Eng C, Nieman LZ et al (2011) Trends in colorectal cancer incidence by anatomic site and disease stage in the United States from 1976 to 2005. Am J Clin Oncol 34:573–580. https://doi.org/10.1097/COC.0b013e3181fe41ed
Siegel RL, Medhanie GA, Fedewa SA, Jemal A (2019) State variation in early-onset colorectal cancer in the United States, 1995-2015. J Natl Cancer Inst 111:1104–1106. https://doi.org/10.1093/jnci/djz098
Giardiello FM, Offerhaus JG Phenotype and cancer risk of various polyposis syndromes. Eur J Cancer 31A:1085–7. https://doi.org/10.1016/0959-8049(95)00139-a
Møller P, Seppälä TT, Bernstein I et al (2018) Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the prospective Lynch syndrome database. Gut 67:1306–1316. https://doi.org/10.1136/gutjnl-2017-314057
National Comprehensive Cancer Network (NCCN) (2022) Genetic/Familial High-Risk Assessment: Colorectal v 2.2021. https://www.nccn.org/professionals/physician_gls/pdf/genetics_colon.pdf
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33. https://doi.org/10.3322/caac.21708
Bailey CE, Hu C-Y, You YN et al (2015) Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg 150:17–22. https://doi.org/10.1001/jamasurg.2014.1756
Rumilla K, Schowalter KV, Lindor NM et al (2011) Frequency of deletions of EPCAM (TACSTD1) in MSH2-associated Lynch syndrome cases. J Mol Diagn 13:93–99. https://doi.org/10.1016/j.jmoldx.2010.11.011
Masciari S, Dewanwala A, Stoffel EM et al (2011) Gastric cancer in individuals with Li-Fraumeni syndrome. Genet Med 13:651–657. https://doi.org/10.1097/GIM.0b013e31821628b6
National Comprehensive Cancer Network (NCCN) (2022) Genetic/familial high-risk assessment: breast, ovarian, and pancreatic v. 2.2022. https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf
Friedenson B (2005) BRCA1 and BRCA2 pathways and the risk of cancers other than breast or ovarian. MedGenMed 7:60
Shibata C, Ogawa H, Miura K et al (2013) Clinical characteristics of gastric cancer in patients with familial adenomatous polyposis. Tohoku J Exp Med 229:143–146. https://doi.org/10.1620/tjem.229.143
Win AK, Reece JC, Dowty JG et al (2016) Risk of extracolonic cancers for people with biallelic and monoallelic mutations in MUTYH. Int J Cancer 139:1557–1563. https://doi.org/10.1002/ijc.30197
Hearle N, Schumacher V, Menko FH et al (2006) Frequency and spectrum of cancers in the Peutz-Jeghers syndrome. Clin Cancer Res 12:3209–3215. https://doi.org/10.1158/1078-0432.CCR-06-0083
Syngal S, Brand RE, Church JM et al (2015) ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol 110:223–262. https://doi.org/10.1038/ajg.2014.435
Correia TF, Mesquita I, Marcos M, et al (2021) Surgical approach to gastric polyposis in Cowen syndrome-case report. J Surg Case Rep 2021:rjab258. https://doi.org/10.1093/jscr/rjab258
Rudloff U (2018) Gastric adenocarcinoma and proximal polyposis of the stomach: diagnosis and clinical perspectives. Clin Exp Gastroenterol 11:447–459. https://doi.org/10.2147/CEG.S163227
Gullo I, van der Post RS, Carneiro F (2021) Recent advances in the pathology of heritable gastric cancer syndromes. Histopathology 78:125–147. https://doi.org/10.1111/his.14228
Li J, Woods SL, Healey S et al (2016) Point mutations in exon 1B of APC reveal gastric adenocarcinoma and proximal polyposis of the stomach as a familial adenomatous polyposis variant. Am J Hum Genet 98:830–842. https://doi.org/10.1016/j.ajhg.2016.03.001
Beer A, Streubel B, Asari R et al (2017) Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS) - a rare recently described gastric polyposis syndrome - report of a case. Z Gastroenterol 55:1131–1134. https://doi.org/10.1055/s-0043-117182
Foretová L, Navrátilová M, Svoboda M et al (2019) GAPPS - gastric adenocarcinoma and proximal polyposis of the stomach syndrome in 8 families tested at Masaryk Memorial Cancer Institute - prevention and prophylactic gastrectomies. Klin Onkol 32:109–117. https://doi.org/10.14735/amko2019S109
Kanemitsu K, Iwatsuki M, Yamashita K et al (2021) Two Asian families with gastric adenocarcinoma and proximal polyposis of the stomach successfully treated via laparoscopic total gastrectomy. Clin J Gastroenterol 14:92–97. https://doi.org/10.1007/s12328-020-01290-6
Mitsui Y, Yokoyama R, Fujimoto S et al (2018) First report of an Asian family with gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS) revealed with the germline mutation of the APC exon 1B promoter region. Gastric Cancer 21:1058–1063. https://doi.org/10.1007/s10120-018-0855-5
Repak R, Kohoutova D, Podhola M et al (2016) The first European family with gastric adenocarcinoma and proximal polyposis of the stomach: case report and review of the literature. Gastrointest Endosc 84:718–725. https://doi.org/10.1016/j.gie.2016.06.023
Caldas C, Carneiro F, Lynch HT et al (1999) Familial gastric cancer: overview and guidelines for management. J Med Genet 36:873–880
Oliveira C, Suriano G, Ferreira P et al (2004) Genetic screening for familial gastric cancer. Hered Cancer Clin Pract 2:51–64. https://doi.org/10.1186/1897-4287-2-2-51
Shinmura K, Kohno T, Takahashi M et al (1999) Familial gastric cancer: clinicopathological characteristics, RER phenotype and germline p53 and E-cadherin mutations. Carcinogenesis 20:1127–1131. https://doi.org/10.1093/carcin/20.6.1127
Garcia-Pelaez J, Barbosa-Matos R, Gullo I et al (2021) Histological and mutational profile of diffuse gastric cancer: current knowledge and future challenges. Mol Oncol 1–27:2841. https://doi.org/10.1002/1878-0261.12948
Sereno M, Aguayo C, Guillén Ponce C et al (2011) Gastric tumours in hereditary cancer syndromes: clinical features, molecular biology and strategies for prevention. Clin Transl Oncol 13:599–610. https://doi.org/10.1007/s12094-011-0705-y
Corso G, Roncalli F, Marrelli D et al (2013) History, pathogenesis, and management of familial gastric cancer: original study of John XXIII’s family. Biomed Res Int 2013:385132. https://doi.org/10.1155/2013/385132
Kohlmann W, Gruber SB (2004) Lynch syndrome. GeneReviews® (updated 2021)
Chung DC, Rustgi AK (1995) DNA mismatch repair and cancer. Gastroenterology 109:1685–1699. https://doi.org/10.1016/0016-5085(95)90660-6
Tutlewska K, Lubinski J, Kurzawski G (2013) Germline deletions in the EPCAM gene as a cause of Lynch syndrome - literature review. Hered Cancer Clin Pract 11:9. https://doi.org/10.1186/1897-4287-11-9
Iyer RR, Pluciennik A, Burdett V, Modrich PL (2006) DNA mismatch repair: functions and mechanisms. Chem Rev 106:302–323. https://doi.org/10.1021/cr0404794
Bonadona V, Bonaïti B, Olschwang S et al (2011) Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 305:2304–2310. https://doi.org/10.1001/jama.2011.743
Walsh MD, Buchanan DD, Cummings MC et al (2010) Lynch syndrome-associated breast cancers: clinicopathologic characteristics of a case series from the colon cancer family registry. Clin Cancer Res 16:2214–2224. https://doi.org/10.1158/1078-0432.CCR-09-3058
Burn J, Bishop DT, Mecklin J-P et al (2008) Effect of aspirin or resistant starch on colorectal neoplasia in the Lynch syndrome. N Engl J Med 359:2567–2578. https://doi.org/10.1056/NEJMoa0801297
Le DT, Uram JN, Wang H et al (2015) PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 372:2509–2520. https://doi.org/10.1056/NEJMoa1500596
Zhao P, Li L, Jiang X, Li Q (2019) Mismatch repair deficiency/microsatellite instability-high as a predictor for anti-PD-1/PD-L1 immunotherapy efficacy. J Hematol Oncol 12:54. https://doi.org/10.1186/s13045-019-0738-1
Harris CC (1996) Structure and function of the p53 tumor suppressor gene: clues for rational cancer therapeutic strategies. J Natl Cancer Inst 88:1442–1455. https://doi.org/10.1093/jnci/88.20.1442
Ozaki T, Nakagawara A (2011) p53: the attractive tumor suppressor in the cancer research field. J Biomed Biotechnol 2011:603925. https://doi.org/10.1155/2011/603925
Boyd MT, Vlatkovic N (2008) p53: a molecular marker for the detection of cancer. Expert Opin Med Diagn 2:1013–1024. https://doi.org/10.1517/17530059.2.9.1013
Schneider K, Zelley K, Nichols KE, Garber J (1999) Li-Fraumeni Syndrome. GeneReviews® (updated 2019)
Frebourg T, Bajalica Lagercrantz S, Oliveira C et al (2020) Guidelines for the Li-Fraumeni and heritable TP53-related cancer syndromes. Eur J Hum Genet 28:1379–1386. https://doi.org/10.1038/s41431-020-0638-4
Li FP, Fraumeni JF (1969) Soft-tissue sarcomas, breast cancer, and other neoplasms. A familial syndrome? Ann Intern Med 71:747–752. https://doi.org/10.7326/0003-4819-71-4-747
Chompret A, Brugières L, Ronsin M et al (2000) P53 germline mutations in childhood cancers and cancer risk for carrier individuals. Br J Cancer 82:1932–1937. https://doi.org/10.1054/bjoc.2000.1167
Nichols KE, Malkin D, Garber JE et al (2001) Germ-line p53 mutations predispose to a wide spectrum of early-onset cancers. Cancer Epidemiol Biomark Prev 10:83–87
Olivier M, Goldgar DE, Sodha N et al (2003) Li-Fraumeni and related syndromes: correlation between tumor type, family structure, and TP53 genotype. Cancer Res 63:6643–6650
Varley JM (2003) Germline TP53 mutations and Li-Fraumeni syndrome. Hum Mutat 21:313–320. https://doi.org/10.1002/humu.10185
Gonzalez KD, Noltner KA, Buzin CH et al (2009) Beyond Li Fraumeni syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol 27:1250–1256. https://doi.org/10.1200/JCO.2008.16.6959
Wong P, Verselis SJ, Garber JE et al (2006) Prevalence of early onset colorectal cancer in 397 patients with classic Li-Fraumeni syndrome. Gastroenterology 130:73–79. https://doi.org/10.1053/j.gastro.2005.10.014
Birch JM, Alston RD, McNally RJ et al (2001) Relative frequency and morphology of cancers in carriers of germline TP53 mutations. Oncogene 20:4621–4628. https://doi.org/10.1038/sj.onc.1204621
Bougeard G, Renaux-Petel M, Flaman JM et al (2015) Revisiting Li-Fraumeni syndrome from TP53 mutation carriers. J Clin Oncol 33:2345–2352. https://doi.org/10.1200/JCO.2014.59.5728
Mai PL, Best AF, Peters JA et al (2016) Risks of first and subsequent cancers among TP53 mutation carriers in the National Cancer Institute Li-Fraumeni syndrome cohort. Cancer 122:3673–3681. https://doi.org/10.1002/cncr.30248
Roy R, Chun J, Powell SN (2011) BRCA1 and BRCA2: different roles in a common pathway of genome protection. Nat Rev Cancer 12:68–78. https://doi.org/10.1038/nrc3181
Foulkes WD, Shuen AY (2013) In brief: BRCA1 and BRCA2. J Pathol 230:347–349. https://doi.org/10.1002/path.4205
Wang Y, Cortez D, Yazdi P et al (2000) BASC, a super complex of BRCA1-associated proteins involved in the recognition and repair of aberrant DNA structures. Genes Dev 14:927–939
Hedenfalk IA, Ringnér M, Trent JM, Borg A (2002) Gene expression in inherited breast cancer. Adv Cancer Res 84:1–34
Xia B, Sheng Q, Nakanishi K et al (2006) Control of BRCA2 cellular and clinical functions by a nuclear partner, PALB2. Mol Cell 22:719–729. https://doi.org/10.1016/j.molcel.2006.05.022
Buisson R, Dion-Côté A-M, Coulombe Y et al (2010) Cooperation of breast cancer proteins PALB2 and piccolo BRCA2 in stimulating homologous recombination. Nat Struct Mol Biol 17:1247–1254. https://doi.org/10.1038/nsmb.1915
Petrucelli N, Daly MB, Pal T (1998) BRCA1- and BRCA2-associated hereditary breast and ovarian cancer. GeneReviews® (updated 2022)
Antoniou A, Pharoah PDP, Narod S et al (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72:1117–1130. https://doi.org/10.1086/375033
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25:1329–1333. https://doi.org/10.1200/JCO.2006.09.1066
Mavaddat N, Peock S, Frost D et al (2013) Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst 105:812–822. https://doi.org/10.1093/jnci/djt095
Tai YC, Domchek S, Parmigiani G, Chen S (2007) Breast cancer risk among male BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst 99:1811–1814. https://doi.org/10.1093/jnci/djm203
Leongamornlert D, Mahmud N, Tymrakiewicz M et al (2012) Germline BRCA1 mutations increase prostate cancer risk. Br J Cancer 106:1697–1701. https://doi.org/10.1038/bjc.2012.146
Kote-Jarai Z, Leongamornlert D, Saunders E et al (2011) BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer 105:1230–1234. https://doi.org/10.1038/bjc.2011.383
Tedaldi G, Tebaldi M, Zampiga V et al (2020) Male breast cancer: results of the application of multigene panel testing to an Italian cohort of patients. Diagnostics (Basel, Switzerland) 10. https://doi.org/10.3390/diagnostics10050269
Thompson D, Easton DF, Breast Cancer Linkage Consortium (2002) Cancer incidence in BRCA1 mutation carriers. J Natl Cancer Inst 94:1358–1365. https://doi.org/10.1093/jnci/94.18.1358
Ghiorzo P, Pensotti V, Fornarini G et al (2012) Contribution of germline mutations in the BRCA and PALB2 genes to pancreatic cancer in Italy. Familial Cancer 11:41–47. https://doi.org/10.1007/s10689-011-9483-5
Iqbal J, Ragone A, Lubinski J et al (2012) The incidence of pancreatic cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer 107:2005–2009. https://doi.org/10.1038/bjc.2012.483
Ford D, Easton DF, Bishop DT et al (1994) Risks of cancer in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Lancet 343:692–695. https://doi.org/10.1016/s0140-6736(94)91578-4
Moran A, O’Hara C, Khan S et al (2012) Risk of cancer other than breast or ovarian in individuals with BRCA1 and BRCA2 mutations. Familial Cancer 11:235–242. https://doi.org/10.1007/s10689-011-9506-2
Breast Cancer Linkage Consortium (1999) Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 91:1310–1316. https://doi.org/10.1093/jnci/91.15.1310
Fong PC, Boss DS, Yap TA et al (2009) Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med 361:123–134. https://doi.org/10.1056/NEJMoa0900212
Sandhu SK, Schelman WR, Wilding G et al (2013) The poly(ADP-ribose) polymerase inhibitor niraparib (MK4827) in BRCA mutation carriers and patients with sporadic cancer: a phase 1 dose-escalation trial. Lancet Oncol 14:882–892. https://doi.org/10.1016/S1470-2045(13)70240-7
Cortesi L, Rugo HS, Jackisch C (2021) An overview of PARP inhibitors for the treatment of breast cancer. Target Oncol 16:255. https://doi.org/10.1007/s11523-021-00796-4
Audeh MW, Carmichael J, Penson RT et al (2010) Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept trial. Lancet 376:245–251. https://doi.org/10.1016/S0140-6736(10)60893-8
Tutt A, Robson M, Garber JE et al (2010) Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet (London, England) 376:235–244. https://doi.org/10.1016/S0140-6736(10)60892-6
Sandhu SK, Omlin A, Hylands L et al (2013) Poly (ADP-ribose) polymerase (PARP) inhibitors for the treatment of advanced germline BRCA2 mutant prostate cancer. Ann Oncol 24:1416–1418. https://doi.org/10.1093/annonc/mdt074
Golan T, Hammel P, Reni M et al (2019) Maintenance Olaparib for germline BRCA-mutated metastatic pancreatic cancer. N Engl J Med 381:317–327. https://doi.org/10.1056/NEJMoa1903387
Hodgson DR, Dougherty BA, Lai Z et al (2018) Candidate biomarkers of PARP inhibitor sensitivity in ovarian cancer beyond the BRCA genes. Br J Cancer 119:1401–1409. https://doi.org/10.1038/s41416-018-0274-8
Li A, Geyer FC, Blecua P et al (2019) Homologous recombination DNA repair defects in PALB2-associated breast cancers. NPJ Breast Cancer 5:23. https://doi.org/10.1038/s41523-019-0115-9
Konstantinopoulos PA, Spentzos D, Karlan BY et al (2010) Gene expression profile of BRCAness that correlates with responsiveness to chemotherapy and with outcome in patients with epithelial ovarian cancer. J Clin Oncol 28:3555–3561. https://doi.org/10.1200/JCO.2009.27.5719
Mateo J, Lord CJ, Serra V et al (2019) A decade of clinical development of PARP inhibitors in perspective. Ann Oncol 30:1437. https://doi.org/10.1093/annonc/mdz192
Wang Y, Zheng K, Huang Y et al (2021) PARP inhibitors in gastric cancer: beacon of hope. J Exp Clin Cancer Res 40:211. https://doi.org/10.1186/s13046-021-02005-6
Ilyas M, Tomlinson IP (1997) The interactions of APC, E-cadherin and beta-catenin in tumour development and progression. J Pathol 182:128–137. https://doi.org/10.1002/(SICI)1096-9896(199706)182:2<128::AID-PATH839>3.0.CO;2-Q
Dinarvand P, Davaro EP, Doan JV et al (2019) Familial adenomatous polyposis syndrome: an update and review of extraintestinal manifestations. Arch Pathol Lab Med 143:1382–1398. https://doi.org/10.5858/arpa.2018-0570-RA
Jasperson KW, Patel SG, Ahnen DJ (1998) APC-associated polyposis conditions. GeneReviews® (updated 2022)
Ma H, Brosens LAA, Offerhaus GJA et al (2018) Pathology and genetics of hereditary colorectal cancer. Pathology 50:49–59. https://doi.org/10.1016/j.pathol.2017.09.004
Knudsen AL, Bülow S, Tomlinson I et al (2010) Attenuated familial adenomatous polyposis: results from an international collaborative study. Color Dis 12:e243–e249. https://doi.org/10.1111/j.1463-1318.2010.02218.x
Nieuwenhuis MH, Vasen HFA (2007) Correlations between mutation site in APC and phenotype of familial adenomatous polyposis (FAP): a review of the literature. Crit Rev Oncol Hematol 61:153–161. https://doi.org/10.1016/j.critrevonc.2006.07.004
Lynch HT, Smyrk T, McGinn T et al (1995) Attenuated familial adenomatous polyposis (AFAP). A phenotypically and genotypically distinctive variant of FAP. Cancer 76:2427–2433. https://doi.org/10.1002/1097-0142(19951215)76:12<2427::aid-cncr2820761205>3.0.co;2-b
Garrean S, Hering J, Saied A et al (2008) Gastric adenocarcinoma arising from fundic gland polyps in a patient with familial adenomatous polyposis syndrome. Am Surg 74:79–83
Arnason T, Liang W-Y, Alfaro E et al (2014) Morphology and natural history of familial adenomatous polyposis-associated dysplastic fundic gland polyps. Histopathology 65:353–362. https://doi.org/10.1111/his.12393
Leone PJ, Mankaney G, Sarvapelli S et al (2019) Endoscopic and histologic features associated with gastric cancer in familial adenomatous polyposis. Gastrointest Endosc 89:961–968. https://doi.org/10.1016/j.gie.2018.12.018
Mankaney G, Leone P, Cruise M et al (2017) Gastric cancer in FAP: a concerning rise in incidence. Familial Cancer 16:371–376. https://doi.org/10.1007/s10689-017-9971-3
Slupska MM, Baikalov C, Luther WM et al (1996) Cloning and sequencing a human homolog (hMYH) of the Escherichia coli mutY gene whose function is required for the repair of oxidative DNA damage. J Bacteriol 178:3885–3892. https://doi.org/10.1128/jb.178.13.3885-3892.1996
Nielsen M, Infante E, Brand R (2012) MUTYH Polyposis. GeneReviews® (updated 2021)
Hurley JJ, Thomas LE, Walton S-J et al (2018) The impact of chromoendoscopy for surveillance of the duodenum in patients with MUTYH-associated polyposis and familial adenomatous polyposis. Gastrointest Endosc 88:665–673. https://doi.org/10.1016/j.gie.2018.04.2347
Spigelman AD, Williams CB, Talbot IC et al (1989) Upper gastrointestinal cancer in patients with familial adenomatous polyposis. Lancet (London, England) 2:783–785. https://doi.org/10.1016/s0140-6736(89)90840-4
Mishina Y, Starbuck MW, Gentile MA et al (2004) Bone morphogenetic protein type IA receptor signaling regulates postnatal osteoblast function and bone remodeling. J Biol Chem 279:27560–27566. https://doi.org/10.1074/jbc.M404222200
Massagué J (2012) TGFβ signalling in context. Nat Rev Mol Cell Biol 13:616–630. https://doi.org/10.1038/nrm3434
Larsen Haidle J, Howe JR (2003) Juvenile polyposis syndrome. GeneReviews® (updated 2022)
Latchford AR, Neale K, Phillips RKS, Clark SK (2012) Juvenile polyposis syndrome: a study of genotype, phenotype, and long-term outcome. Dis Colon Rectum 55:1038–1043. https://doi.org/10.1097/DCR.0b013e31826278b3
Aytac E, Sulu B, Heald B et al (2015) Genotype-defined cancer risk in juvenile polyposis syndrome. Br J Surg 102:114–118. https://doi.org/10.1002/bjs.9693
Ishida H, Ishibashi K, Iwama T (2018) Malignant tumors associated with juvenile polyposis syndrome in Japan. Surg Today 48:253–263. https://doi.org/10.1007/s00595-017-1538-2
Blatter R, Tschupp B, Aretz S et al (2020) Disease expression in juvenile polyposis syndrome: a retrospective survey on a cohort of 221 European patients and comparison with a literature-derived cohort of 473 SMAD4/BMPR1A pathogenic variant carriers. Genet Med 22:1524–1532. https://doi.org/10.1038/s41436-020-0826-1
MacFarland SP, Ebrahimzadeh JE, Zelley K et al (2021) Phenotypic differences in juvenile polyposis syndrome with or without a disease-causing SMAD4/BMPR1A variant. Cancer Prev Res (Phila) 14:215–222. https://doi.org/10.1158/1940-6207.CAPR-20-0348
Howe JR, Roth S, Ringold JC et al (1998) Mutations in the SMAD4/DPC4 gene in juvenile polyposis. Science 280:1086–1088. https://doi.org/10.1126/science.280.5366.1086
Ma C, Giardiello FM, Montgomery EA (2014) Upper tract juvenile polyps in juvenile polyposis patients: dysplasia and malignancy are associated with foveolar, intestinal, and pyloric differentiation. Am J Surg Pathol 38:1618–1626. https://doi.org/10.1097/PAS.0000000000000283
Aretz S, Stienen D, Uhlhaas S et al (2007) High proportion of large genomic deletions and a genotype phenotype update in 80 unrelated families with juvenile polyposis syndrome. J Med Genet 44:702–709. https://doi.org/10.1136/jmg.2007.052506
Brosens LAA, van Hattem A, Hylind LM et al (2007) Risk of colorectal cancer in juvenile polyposis. Gut 56:965–967. https://doi.org/10.1136/gut.2006.116913
Höfting I, Pott G, Stolte M (1993) The syndrome of juvenile polyposis. Leber Magen Darm 23(107–8):111–112
Howe JR, Mitros FA, Summers RW (1998) The risk of gastrointestinal carcinoma in familial juvenile polyposis. Ann Surg Oncol 5:751–756. https://doi.org/10.1007/BF02303487
Agnifili A, Verzaro R, Gola P et al (1999) Juvenile polyposis: case report and assessment of the neoplastic risk in 271 patients reported in the literature. Dig Surg 16:161–166. https://doi.org/10.1159/000018711
Goff V Transparency and disclosure: the route to accountability. Issue Brief (Inst Health Care Costs Solut) 2:1–12
Woodford-Richens K, Bevan S, Churchman M et al (2000) Analysis of genetic and phenotypic heterogeneity in juvenile polyposis. Gut 46:656–660. https://doi.org/10.1136/gut.46.5.656
Achatz MI, Porter CC, Brugières L et al (2017) Cancer screening recommendations and clinical Management of Inherited Gastrointestinal Cancer Syndromes in childhood. Clin Cancer Res 23:e107–e114. https://doi.org/10.1158/1078-0432.CCR-17-0790
Cohen S, Hyer W, Mas E et al (2019) Management of Juvenile Polyposis Syndrome in children and adolescents: a position paper from the ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr 68:453–462. https://doi.org/10.1097/MPG.0000000000002246
Xu X, Jin D, Durgan J, Hall A (2013) LKB1 controls human bronchial epithelial morphogenesis through p114RhoGEF-dependent RhoA activation. Mol Cell Biol 33:2671–2682. https://doi.org/10.1128/MCB.00154-13
McGarrity TJ, Amos CI, Baker MJ (2001) Peutz-Jeghers Syndrome. GeneReviews® (updated 2021)
Lim W, Olschwang S, Keller JJ et al (2004) Relative frequency and morphology of cancers in STK11 mutation carriers. Gastroenterology 126:1788–1794. https://doi.org/10.1053/j.gastro.2004.03.014
Giardiello FM, Brensinger JD, Tersmette AC et al (2000) Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology 119:1447–1453. https://doi.org/10.1053/gast.2000.20228
Pezzolesi MG, Zbuk KM, Waite KA, Eng C (2007) Comparative genomic and functional analyses reveal a novel cis-acting PTEN regulatory element as a highly conserved functional E-box motif deleted in Cowden syndrome. Hum Mol Genet 16:1058–1071. https://doi.org/10.1093/hmg/ddm053
Yehia L, Eng C (2001) PTEN Hamartoma Tumor Syndrome. GeneReviews® (updated 2021)
Mester J, Eng C (2015) Cowden syndrome: recognizing and managing a not-so-rare hereditary cancer syndrome. J Surg Oncol 111:125–130. https://doi.org/10.1002/jso.23735
Tan M-H, Mester JL, Ngeow J et al (2012) Lifetime cancer risks in individuals with germline PTEN mutations. Clin Cancer Res 18:400–407. https://doi.org/10.1158/1078-0432.CCR-11-2283
Heald B, Mester J, Rybicki L et al (2010) Frequent gastrointestinal polyps and colorectal adenocarcinomas in a prospective series of PTEN mutation carriers. Gastroenterology 139:1927–1933. https://doi.org/10.1053/j.gastro.2010.06.061
Ngeow J, Eng C (2015) PTEN hamartoma tumor syndrome: clinical risk assessment and management protocol. Methods 77–78:11–19. https://doi.org/10.1016/j.ymeth.2014.10.011
Zbuk KM, Eng C (2007) Hamartomatous polyposis syndromes. Nat Clin Pract Gastroenterol Hepatol 4:492–502. https://doi.org/10.1038/ncpgasthep0902
Rosty C (2018) The role of the surgical pathologist in the diagnosis of gastrointestinal polyposis syndromes. Adv Anat Pathol 25:1–13. https://doi.org/10.1097/PAP.0000000000000173
Adams DR, Eng CM (2018) Next-generation sequencing to diagnose suspected genetic disorders. N Engl J Med 379:1353–1362. https://doi.org/10.1056/NEJMra1711801
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tedaldi, G., São José, C., Oliveira, C. (2023). Other Syndromes and Genes Associated with Gastric Cancer Predisposition. In: Corso, G., Veronesi, P., Roviello, F. (eds) Hereditary Gastric and Breast Cancer Syndrome. Springer, Cham. https://doi.org/10.1007/978-3-031-21317-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-21317-5_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-21316-8
Online ISBN: 978-3-031-21317-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)