Abstract
Purpose of review
Gastric cancer is a leading cause of cancer death in the world. Between 1 and 3% of cases are associated with specific genetic cancer risk syndromes. The purpose of this article is to review the latest insights, as well as gaps in knowledge, regarding some of the most common hereditary gastric cancer syndromes: hereditary diffuse gastric cancer (HDGC), gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS), Lynch syndrome, the adenomatous polyposis syndromes, and the hamartomatous polyposis syndromes.
Recent findings
Patients carrying pathogenic variants in CDH1, but not meeting clinical criteria for HDGC, are increasingly being identified thanks to multigene panel testing; their absence from previous analyses overestimated gastric cancer penetrance. GAPPS is a recently described hereditary gastric cancer syndrome associated with specific point mutations in the promoter 1B region of the APC gene.
Summary
Risk of gastric cancer is highest among carriers of pathogenic variants in CDH1, with cumulative incidences approximately 40% and 30% for men and women, respectively. Mutations associated with Lynch syndrome and adenomatous polyposis syndromes confer greatest risk for gastric cancer in East Asian populations. Risk of gastric cancer in GAPPS and hamartomatous polyposis syndromes is difficult to estimate due to their rarity, but mutation status likely determines risk. Future research is needed to more precisely define risk of gastric cancer in these syndromes, so strategies for screening and prophylactic gastrectomy can be optimized.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fifth leading cause of cancer and the third most common cause of cancer deaths in the world, with an estimated 819,000 deaths annually [1]. Gastric adenocarcinoma is by far the most common histologic subtype of gastric cancer, comprising 95% of cases [2]. Both genetic and environmental factors contribute to the development of this type of cancer. Recognized risk factors include advanced age, male sex, tobacco use, diets high in salt, and smoked foods, as well as H. pylori infection, which has been implicated in 65–80% of cases [3]. Whereas about 90% of gastric cancers appear to be sporadic, 10% exhibit familial clustering, and 1–3% can be linked to specific hereditary cancer syndromes [4]. In this paper, we review the most common hereditary gastric cancer syndromes: hereditary diffuse gastric cancer, gastric adenocarcinoma and proximal polyposis of the stomach, Lynch syndrome, the adenomatous polyposis syndromes, and the hamartomatous polyposis syndromes. Due to space constraints, we do not address Li-Fraumeni syndrome or hereditary breast-ovarian syndrome. Nor do we discuss familial intestinal gastric cancer, which is defined as non-diffuse gastric cancer inherited in an autosomal dominant manner. The genetic basis for this condition remains to be elucidated, and it may, in fact, result from a combination of heritable and environmental factors [5].
This review is not comprehensive; rather, we aim to highlight the latest insights and critically appraise management strategies wherever possible (Table 1).
Hereditary diffuse gastric cancer
Hereditary diffuse gastric cancer (HDGC) is an autosomal dominant syndrome characterized by early-onset diffuse gastric cancer (DGC), as well as lobular breast cancer (LBC). Pathogenic germline variants in the CDH1 gene have been identified as a major cause of this syndrome [6]. CDH1 is the gene that codes for E-cadherin, an important cell-cell adhesion protein [7]. Mutations in CTNNA1, the gene that encodes α-catenin (a protein that interacts with E-cadherin in adherens junctions), have also been found in some HDGC patients [8]. While mutations in other genes (e.g., MAP3K6, BRCA2, PALB2) have also been reported, their significance is unclear, and they likely represent a very small fraction of HDGC cases [9]. DGC has a poor prognosis, in large part because patients often presents with vague symptoms of abdominal discomfort or bloating. Furthermore, as this type of cancer infiltrates the submucosa, it is often hard to identify on endoscopy. Consequently, diagnoses are commonly made at advanced stages. Prognosis is poor, and, even among patients with potentially curative disease, median survival is just 17 months [10]. DGC is diagnosed histologically by neoplastic epithelial cells with signet ring morphology infiltrating the stomach lining.
In order to assist in identifying families who could carry CDH1 or CTNNA1 pathogenic variants and thus have HDGC syndrome, the International Gastric Cancer Linkage Consortium (IGCLC) suggested a set of clinical criteria in 1999, subsequently updated in 2010, 2015, and 2020 [6, 11, 12, 13••]. According to the 2020 criteria, genetic testing for germline mutations should be offered to patients whose families (including first- and second-degree relatives) have any of the following: (1) at least two cases of gastric cancer, regardless of age, one of which confirmed to be DGC; (2) one case of DGC diagnosed at any age and one case of LBC before the age of 70, in different family members; and (3) at least two cases of LBC before the age of 50. Genetic testing is also recommended for patients with any of the following personal histories: (1) DGC before the age of 50; (2) DGC at any age in individuals of Maori ethnicity; (3) DGC at any age in individuals with personal or family history of cleft lip or cleft palate; (4) DGC and LBC, both diagnosed before the age of 70; (5) bilateral LBC diagnosed before the age of 70; and (6) gastric in situ signet ring cells and/or pagetoid spread of signet ring cells in individuals before the age of 50 [13••]. The above criteria for genetic testing have been relaxed compared to prior iterations, mainly via changes to age cutoffs. Genetic testing should begin with analysis of CDH1; CTNNA1 analysis should be considered if no CDH1 pathogenic variant is identified [13••].
Approximately 20–50% of families meeting 2010 IGCLC clinical criteria were found to have germline mutations in CDH1 [12, 14]. For carriers of pathogenic germline variants in CDH1, cumulative incidence of gastric cancer by age 80 is often reported to be as high as 70% in men and 56% in women [14]. However, these figures were derived from families who were preselected with HDGC clinical criteria and were thus highly enriched in gastric cancer. Using data from patients who underwent multigene panel testing but had not been pre-selected by HDGC clinical criteria, our group and Roberts et al. both found significantly lower cumulative incidence of gastric cancer by age 80: 37–42% for men and 24–33% for women [15••, 16]. Therefore, for unselected CDH1 mutation carriers, penetrance is much lower. This is highly reminiscent of the data on Lynch syndrome, which were initially determined in mutation carriers that were pre-selected with the highly stringent Amsterdam criteria. Eventually, when penetrance was evaluated only based on mutation carrier status and without clinical pre-selection, cumulative incidence was found to be much lower. Recent data have raised the possibility that mutations in specific CDH1 gene regions could confer different risks, which could be extremely useful to assist in risk stratification [17]. Further studies should shed more light into this issue. The risk of gastric cancer in those with pathogenic CTNNA1 mutations is not well defined. In a study of 33 CTNNA1 mutation carriers identified by multigene panel testing, 12% had DGC, and 21% had either a personal or family history of gastric cancer [18].
In light of the high incidence of DGC and associated poor prognosis, as well as the traditionally poor data on screening, patients who meet clinical criteria and carry a known pathogenic CDH1 variant are generally advised to undergo prophylactic total gastrectomy with Roux-en-Y reconstruction. Since this surgery can have major effects on quality of life, the international consortium guidelines stress the importance of a multidisciplinary approach and careful decision-making. They recommend considering gastrectomy in early adulthood, generally between ages 20 and 30 [13••]. Using a Markov model of HDGC progression associated with pathogenic variants in CDH1, Laszkowska et al. found that quality-adjusted life-years (QALYs) would be optimized if prophylactic gastrectomy was done at age 39 for men and age 30 for women [19]. While their calculations were based only on data from CDH1 families pre-selected with clinical criteria, in our study of un-selected CDH1 mutation carriers, we found the cumulative risk of gastric cancer to be relatively low until age 40 (2.8% and 1.3% for women and men, respectively) before nearly doubling with each successive decade [15••]. In any case, acknowledging that HDGC is not a homogeneous syndrome, the guidelines do suggest taking into account family phenotype, especially age at cancer diagnosis in probands, when deciding when to proceed with prophylactic gastrectomy. Annual breast MRI is recommended for women with CDH1 pathogenic variants starting at age 30. Alternatively, bilateral risk-reducing mastectomy can be considered [13••].
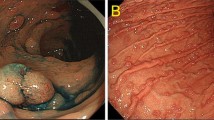
Annual upper endoscopy is recommended for CDH1 mutation carriers who are not interested in prophylactic gastrectomy or wish to delay it, as well as for CTNNA1 mutation carriers [13••]. During the procedure, the stomach should be adequately inflated in order to check for poor distensibility, which can be a sign of linitis plastica, diffuse infiltration of the gastric wall with signet ring cells. In contrast, tiny foci of signet ring cells generally cannot be recognized macroscopically, so wide sampling of gastric mucosa is needed to maximize the likelihood of diagnosis. The Cambridge protocol prescribes biopsy of all visible lesions/pale areas, as well as random biopsies [12, 13••]. The most recent IGCLC guidelines recommend a total of 28–30 random biopsies with increased sampling of the gastric body (3–5 cardia, 5 of the fundus, 10 of the body, 5 of the antrum) [13••]. Unfortunately, endoscopic surveillance has usually been found to be insensitive for detecting DGC/signet ring carcinoma cells (SRCC). Older case series of HDGC patients undergoing prophylactic gastrectomy found the sensitivity of pre-operative endoscopy to be as low as 7–16% [4, 20]. However, a more recent study utilizing the Cambridge protocol plus narrow band imaging identified SRCC in 69% of gastrectomy-confirmed cases [21]. Studies on other independent series should help clarify this issue.
While recommendations are clear for those with both HDGC clinical criteria and CDH1 mutations, optimal management is less clear for those with one but not the other. The IGCLC now terms those who meet clinical criteria but lack pathogenic variants in CDH1 or CTNNA1 “HDGC-like” and recommends that they be considered for yearly endoscopic surveillance starting at age 40, or 10 years prior to the earliest gastric cancer case in the family [13••]. However, recent studies call into question the utility of annual endoscopy in these patients. Mi et al. found SRCC in 61% of CDH1 mutation carriers, compared to only 9.7% of HDGC-like non-carriers [22]. Another study found SRCC in 6% of non-carriers with median follow-up of 46 months [23]. Perhaps in response to these studies, the most recent IGCLC guidelines state that surveillance intervals may be prolonged at the discretion of the endoscopist after 2 years, taking into account prior endoscopic findings and the patient’s family history [13••].. The opposite situation, that of CDH1 or CTNNA1 mutation in someone without a family history of DGC, is becoming increasingly common with the proliferation of multigene panel genetic testing. In our study of CDH1 mutation carriers identified by multigene panel testing, only 46% met HDGC clinical criteria, though all had a personal or family history of cancer [15••]. Among these patients, cancer risks were lower, but still very significant. Another recent study comparing CDH1 carriers with family histories of DGC to those without found similar rates (60% vs. 50%) of SRCC on EGD and/or gastrectomy [24]. Thus, while risks may be different, given the limited usefulness of gastric cancer screening, gastrectomy should still be a strong consideration, though acknowledging that the risk of developing actual DGC in this population is not completely understood and the clinical significance of SRCC is far from clear.
Gastric adenocarcinoma and proximal polyposis of the stomach
Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS) is a rare autosomal dominant gastric cancer syndrome first described by Worthley et al. in 2012. They reported three families from North America and Australia with multiple family members having fundic gland polyposis (sparing the antrum and lesser curvature) and intestinal-type adenocarcinoma [25]. The syndrome has subsequently been identified in European and Asian families, as well [26, 27]. Diagnostic criteria proposed in the initial description are as follows: (1) gastric polyps restricted to the body and fundus with no evidence of colorectal or duodenal polyposis; (2) > 100 polyps carpeting the proximal stomach in the index case or > 30 polyps in a first-degree relative of another case; (3) predominantly fundic gland polyp (FGP) histology, with some having regions of dysplasia (or a family member with either dysplastic FGPs or gastric adenocarcinoma); (4) autosomal dominant pattern of inheritance; and (5) exclusion of other heritable gastric polyposis syndromes and PPI use [25].
On a genetic level, GAPPS has been associated with specific point mutations in the promoter 1B region of APC, the tumor suppressor gene that is defective in familial adenomatous polyposis (FAP) and attenuated FAP [28••]. The implicated point mutations (c.-191 T > C, c.-192A > G, and c.-195A > C) reduce binding of the transcription factor Yin Yang 1 (YY1) and, as a result, decrease transcription of the APC protein. Transcription of APC is generally preserved in the colonic mucosa via promoter 1A, preventing development of the extensive colonic polyposis seen in FAP and attenuated FAP. However, promoter 1A is almost universally methylated (i.e., silenced) in both gastric cancer and normal mucosa [29].
Due to the small number of identified cases to date, much remains to be learned about the natural history of GAPPS. Absolute risk of gastric cancer is not well defined, but has been estimated at 25% in a recent case series [30]. Gastric polyposis was found in a patient as young as 10, and the earliest associated gastric cancer was reported at age 23 [25, 26]. Other malignancies reported in families with GAPPS include leukemia and cancers of the skin, thyroid, brain, prostate, lung, and colon [31]. McDuffie et al. found higher rates of adenomatous colonic polyps in patients with GAPPS compared to their unaffected relatives, suggesting possible colon involvement in this syndrome [32].
There are currently no guidelines for management of GAPPS. Those at risk should be tested for germline mutations in promoter 1B of APC, and those carrying such a mutation should get endoscopic screening followed by surveillance. Unfortunately, there have been multiple cases of patient developing invasive gastric adenocarcinoma and even metastatic disease while under endoscopic surveillance. Prophylactic gastrectomy should therefore be strongly considered in GAPPS patients found to have dysplasia on gastric biopsy or whose number or location of polyps make adequate sampling difficult [31].
Lynch syndrome
First described as hereditary nonpolyposis colorectal cancer in 1966, Lynch syndrome (LS) is one of the most common hereditary cancer syndromes, affecting up to 1 in 300 people [33]. LS carries the greatest risk for colorectal and uterine cancers for which lifetime incidences can be as high as 61% and 57%, respectively. It also predisposes to cancers of the stomach, ovaries, hepatobiliary tract, upper urinary tract, pancreas, and small bowel [34]. Inherited in autosomal dominant manner, LS is caused by a germline mutation in one of several mismatch repair genes (MLH1, MSH2, MSH6, and PMS2) or deletion of the cell adhesion molecule gene EPCAM, which in turn leads to loss of expression of MSH2 [35].
Cumulative incidence of gastric cancer in LS has been described to be from less than 1% to almost 10% [36,37,38]. Following 3119 LS patients for a total of 24,475 years, Moller et al. found cumulative incidence of gastric cancer by age 75 to be 7–8% in those with pathogenic MLH1 or MSH2 mutations [39]. For MSH6 mutation carriers, cumulative risk has been described between ≤ 1 and 7.9% [40,41,42]. A study of 284 LS families found no increased risk in those with PMS2 mutations [43]. A recent cross-sectional study of 3828 LS carriers found male sex, older age, MLH1 and MSH2 mutations, and number of first-degree relatives with gastric cancer each to be independently associated with personal history of gastric cancer [44]. Risk of gastric cancer is significantly higher among LS patients who come from areas with high baseline risk, such as East Asia. In Korea, where gastric cancer makes up nearly a quarter of all cancer diagnoses, carrying a mutation in MLH1, MSH2, or MSH6 doubles one’s lifetime risk [45]. Recent studies have estimated the cumulative incidence of gastric cancer by age 70 among Japanese LS carriers to be 20–50% for men and 12.5–25% for women, compared with 4.4% and 1.7% in Japanese male and female non-carriers, respectively [46, 47].
The cornerstone of screening and surveillance in LS is colonoscopy every 1–2 years [48]. Recommendations for gastric cancer screening are less firm. The National Comprehensive Cancer Network (NCCN) recommends consideration of baseline upper endoscopy with random biopsy of the proximal and distal stomach at age 40, followed by surveillance EGD every 3–5 years in patients with the following risk factors: male sex, older age, MLH1 or MSH2 pathogenic variants, first-degree relative with gastric cancer, Asian ethnicity, coming from country with high background incidence of gastric cancer, chronic autoimmune gastritis, gastric intestinal metaplasia, and gastric adenomas [49]. The American College of Gastroenterology (ACG) and United States Multi-Society Task Force (USMSTF) both recommend consideration of baseline EGD at age 30–35, followed by surveillance every 2–3 years (ACG) or 3–5 years (USMSTF), depending on individual risk factors. All groups recommend consideration of H. pylori testing and treatment, if detected [48, 50, 51].
Adenomatous polyposis syndromes: Familial adenomatous polyposis, attenuated FAP, and MUTYH-associated polyposis
Familial adenomatous polyposis (FAP) is a rare autosomal dominant polyposis syndrome characterized by the development hundreds to thousands of colorectal adenomas. Cumulative incidence of colorectal cancer (CRC) in FAP is 95% by age 50. Attenuated FAP is a less severe form; patients typically develop 0–100 colon adenomas with 70% lifetime risk of CRC. Both of these syndromes are caused by germline mutations in APC, a tumor suppressor gene in the Wnt signaling pathway [34]. Patients with FAP are also at risk for various extracolonic malignancies, most notably cancers of the duodenum and thyroid. While gastric fundic gland polyps are found in 50% of cases, gastric adenomas and cancer are much less common [52]. First identified in 2002, MUTYH-associated polyposis (MAP) is an autosomal recessive polyposis syndrome with a clinical phenotype that closely resembles that of attenuated FAP. MAP is caused by loss of function MUTYH, a gene involved in base excision repair and programmed cell death [35].
In western countries, patients with FAP have not generally been considered to be at increased risk of gastric cancer; cumulative incidence is close to 1% in both FAP patients and the general population. In contrast, in Japan and Korea, those with FAP appear to be 7–10 times more likely to develop gastric cancer than their compatriots [53]. Nevertheless, in a recent review of FAP patients enrolled in the Cleveland Clinic registry between 1979 and 2016, 10/767 (1.3%) developed gastric cancer. Remarkably, 9/10 cases were diagnosed between 2012 and 2016, hinting at a recent rise in incidence [54]. A case-control study using the same patients identified carpeting of gastric polyps, solitary polyps > 20 mm, polypoid mounds, pyloric gland adenomas, and polyps with high-grade dysplasia as possible markers of increased risk [55]. The risk of gastric cancer in patients with MAP is not well defined.
Given the very high rate of colon cancer in these syndromes, guidelines recommend frequent colonoscopies and early consideration of prophylactic colectomy. Recommendations for upper endoscopy are driven primarily by the risk of duodenal and periampullary cancer. In FAP and attenuated FAP, baseline upper endoscopy should be done around age 20–25; baseline upper endoscopy should be considered at age 30–35 for patients with MAP. Frequency of repeat endoscopy typically depends on burden of duodenal polyps or Spigelman stage. Regarding the risk of gastric cancer specifically, the NCCN recommends consideration of specialized surveillance or surgery for lesions with high-risk histologic features, such as tubular adenomas, polyps with high-grade dysplasia, and pyloric gland adenomas. Gastrectomy should be considered for high-risk lesions that cannot be removed endoscopically [48].
Hamartomatous polyposis syndromes
Peutz-Jeghers syndrome (PJS), juvenile polyposis syndrome (JPS), and PTEN hamartoma tumor syndrome (PHTS) comprise the hereditary hamartomatous polyposis syndromes. These rare syndromes, each with a prevalence of about 1 in 100,000, are characterized by the development of hamartomas (disorganized overgrowth of normal-appearing cells) primarily in the gastrointestinal (GI) tract [34]. Each syndrome has an autosomal dominant pattern of inheritance, although approximately a quarter of cases result from de novo mutations and thus have no significant family history. PJS is caused by mutations in the STK11 tumor suppressor gene and manifests clinically with mucocutaneous hyperpigmentation (most often involving the lips, buccal mucosa, and finger/toe tips) and multiple GI polyps, which can cause intussusception, bowel obstruction, or bleeding [56]. A clinical diagnosis of JPS can be made upon finding five or more juvenile polyps in the colon, juvenile polyps in other parts of the GI tract, or any number of juvenile polyps in a someone with a family history of juvenile polyps [51]. Approximately half of cases are associated with mutations in the SMAD4 and BMPR1A tumor suppressor genes. Juvenile polyps have a tendency to bleed, and, as a result, patients often have iron deficiency anemia. PHTS is caused by germline mutations in the PTEN tumor suppressor gene and encompasses Cowden, Bannayan-Riley-Ruvalcaba, and Proteus and Proteus-like syndromes. More than 90% of patients have papules on the face (hamartomas of the hair follicle root sheath), and 75% have macrocephaly. The most common polyps in PHTS are hyperplastic colon polyps, but patients can also develop adenomas, juvenile polyps, lipomas, and ganglioneuromas [34].
Patients with hamartomatous polyposis syndromes are at increased risk of developing various cancers, although precise risks are difficult to estimate owing to the rarity of these syndromes. Those with PJS appear to be at greatest risk for breast, GI, and gynecologic malignancies [48]. The cumulative incidence of gastric cancer, specifically, was found to be 29% in a meta-analysis of 210 PJS patients [57]. Among patients with JPS, cancers of the stomach and colon are most common. A recent analysis of 171 Japanese patients with JPS found 73% lifetime risk of gastric cancer [58]. Previous studies of JPS patients from western countries have estimated lifetime risk of gastric cancer at 20–30% [48, 59]. This likely reflects risk for SMAD4 and BMPR1A mutation carriers, as recent data points to absence of gastric polyps and cancer in JPS when there are no mutations in these two genes (MacFarland et al., under review). Those with PHTS are at greatest risk of developing breast cancer (81% by age 70 in women) and thyroid cancer (21% by age 70) [60]. To date, these patients have not been shown to suffer from higher rates of gastric cancer [61].
Management of the hamartomatous polyposis syndromes involves frequent surveilling of the organs at risk for cancer. For those with PJS, the NCCN recommends EGD every 2–3 years, starting in the late teens [48]. Citing the risk of developing early complications from hamartomatous polyps, the ACG guidelines are more proactive, calling for first upper endoscopy at age 8; if polyps are found on the initial exam, EGD should be repeated every 3 years; if none are found, next EGD should be done at age 18 and be repeated every 3 years thereafter [51]. For JPS, the NCCN guidelines recommend first upper endoscopy around age 15, repeated annually if polyps are found and every 2–3 years if none are found. For families without an identified genetic pathogenic variant, they recommend consideration of upper endoscopy every 5 years starting at age 20 and every 10 years starting at age 40 in patients in whom no polyps are found [48]. The ACG guidelines recommend starting gastric cancer surveillance at age 12 with repeat upper endoscopy every 1–3 years depending on polyp burden [51]. Gastric polyps can typically be managed endoscopically, but surgery may be necessary if anemia develops. According to expert opinion, upper endoscopy should be considered at age 15 in PHTS and repeated every 2–3 years [51].
Conclusion
Gastric cancer is a major cause of cancer death worldwide. Currently, 1–3% of cases can be linked to specific hereditary cancer syndromes. As our knowledge of genetics expands, these syndromes are increasingly being defined by specific pathogenic variants, as opposed to various combinations of personal and family histories. Management strategies are currently limited by incomplete understanding of precise risks associated with some syndromes and clinical significance of some pathologic findings, such as SRCC in patients with CDH1 mutations, but lack significant family history. As we learn more, we will be able to optimize recommendations for endoscopic screening and prophylactic gastrectomy, minimizing incidence of gastric cancer while also avoiding unnecessary costly and sometimes morbid procedures.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–48.
Ajani JA, Lee J, Sano T, Janjigian YY, Fan D, Song S. Gastric adenocarcinoma. Nat Rev Dis Primers. 2017;3:17036.
Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomark Prev. 2014;23:700–13.
Chen Y, Kingham K, Ford JM, Rosing J, van Dam J, Jeffrey RB, et al. A prospective study of total gastrectomy for CDH1-positive hereditary diffuse gastric cancer. Ann Surg Oncol. 2011;18:2594–8.
Oliveira C, Pinheiro H, Figueiredo J, Seruca R, Carneiro F. Familial gastric cancer: genetic susceptibility, pathology, and implications for management. Lancet Oncol. 2015;16:e60–70.
van der Post RS, Vogelaar IP, Carneiro F, Guilford P, Huntsman D, Hoogerbrugge N, et al. Hereditary diffuse gastric cancer: updated clinical guidelines with an emphasis on germline CDH1 mutation carriers. J Med Genet. 2015;52:361–74.
Gall TM, Frampton AE. Gene of the month: E-cadherin (CDH1). J Clin Pathol. 2013;66:928–32.
Majewski IJ, Kluijt I, Cats A, Scerri TS, de Jong D, Kluin RJC, et al. An α-E-catenin (CTNNA1) mutation in hereditary diffuse gastric cancer. J Pathol. 2013;229:621–9.
Vogelaar IP, van der Post RS, van Krieken JHJ, et al. Unraveling genetic predisposition to familial or early onset gastric cancer using germline whole-exome sequencing. Eur J Hum Genet. 2017;25:1246–52.
Stiekema J, Cats A, Kuijpers A, van Coevorden F, Boot H, Jansen EPM, et al. Surgical treatment results of intestinal and diffuse type gastric cancer. Implications for a differentiated therapeutic approach? Eur J Surg Oncol. 2013;39:686–93.
Caldas C, Carneiro F, Lynch HT, Yokota J, Wiesner GL, Powell SM, et al. Familial gastric cancer: overview and guidelines for management. J Med Genet. 1999;36:873–80.
Fitzgerald RC, Hardwick R, Huntsman D, Carneiro F, Guilford P, Blair V, et al. Hereditary diffuse gastric cancer: updated consensus guidelines for clinical management and directions for future research. J Med Genet. 2010;47:436–44.
•• Blair VR, McLeod M, Carneiro F, et al. Hereditary diffuse gastric cancer: updated clinical practice guidelines. Lancet Oncol. 2020;21:e386–97 This is the most recent version of the international gastric Cancer linkage Consortium's clinical guidelines for hereditary diffuse gastric cancer (HDGC). It defines clinical crtieria for this genetic cancer syndrome and provides recommendations for management.
Hansford S, Kaurah P, Li-Chang H, Woo M, Senz J, Pinheiro H, et al. Hereditary diffuse gastric cancer syndrome: CDH1 mutations and beyond. JAMA Oncol. 2015;1:23–32.
•• Xicola RM, Li S, Rodriguez N, et al. Clinical features and cancer risk in families with pathogenic CDH1 variants irrespective of clinical criteria. J Med Genet. 2019;56:838–43 This paper, along with Roberts et al. (next reference), identifed patients with CDH1 pathogenic variants who did not meet clinical criteria for HDGC. Including these patients in penetrance analysis, gastric cancer penetrance was shown to be significanlty lower than previously estimated.
Roberts ME, Ranola JMO, Marshall ML, Susswein LR, Graceffo S, Bohnert K, et al. Comparison of CDH1 penetrance estimates in clinically ascertained families vs families ascertained for multiple gastric cancers. JAMA Oncol. 2019;5:1325–31.
Lo W, Zhu B, Sabesan A, Wu HH, Powers A, Sorber RA, et al. Associations of CDH1 germline variant location and cancer phenotype in families with hereditary diffuse gastric cancer (HDGC). J Med Genet. 2019;56:370–9.
Clark DF, Michalski ST, Tondon R, Nehoray B, Ebrahimzadeh J, Hughes SK, et al. Loss-of-function variants in CTNNA1 detected on multigene panel testing in individuals with gastric or breast cancer. Genet Med. 2020;22:840–6.
Laszkowska M, Silver ER, Schrope B, et al. Optimal timing of total gastrectomy to prevent diffuse gastric cancer in individuals with pathogenic variants in CDH1. Clin Gastroenterol Hepatol. 2020;18:822–829.e4.
Hebbard PC, Macmillan A, Huntsman D, et al. Prophylactic total gastrectomy (PTG) for hereditary diffuse gastric cancer (HDGC): the Newfoundland experience with 23 patients. Ann Surg Oncol. 2009;16:1890–5.
van Dieren JM, Kodach LL, den Hartog P, et al. Gastroscopic surveillance with targeted biopsies compared with random biopsies in CDH1 mutation carriers. Endoscopy 2020.
Mi EZ, Mi EZ, di Pietro M, O’Donovan M, Hardwick RH, Richardson S, et al. Comparative study of endoscopic surveillance in hereditary diffuse gastric cancer according to CDH1 mutation status. Gastrointest Endosc. 2018;87:408–18.
van der Post RS, van Dieren J, Grelack A, et al. Outcomes of screening gastroscopy in first-degree relatives of patients fulfilling hereditary diffuse gastric cancer criteria. Gastrointest Endosc. 2018;87:397–404.e2.
Jacobs MF, Dust H, Koeppe E, Wong S, Mulholland M, Choi EY, et al. Outcomes of endoscopic surveillance in individuals with genetic predisposition to hereditary diffuse gastric cancer. Gastroenterology. 2019;157:87–96.
Worthley DL, Phillips KD, Wayte N, Schrader KA, Healey S, Kaurah P, et al. Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS): a new autosomal dominant syndrome. Gut. 2012;61:774–9.
Repak R, Kohoutova D, Podhola M, Rejchrt S, Minarik M, Benesova L, et al. The first European family with gastric adenocarcinoma and proximal polyposis of the stomach: case report and review of the literature. Gastrointest Endosc. 2016;84:718–25.
Mitsui Y, Yokoyama R, Fujimoto S, Kagemoto K, Kitamura S, Okamoto K, et al. First report of an Asian family with gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS) revealed with the germline mutation of the APC exon 1B promoter region. Gastric Cancer. 2018;21:1058–63.
•• Li J, Woods SL, Healey S, et al. Point mutations in exon 1B of APC reveal gastric adenocarcinoma and proximal polyposis of the stomach as a familial adenomatous polyposis variant. Am J Hum Genet. 2016;98:830–42 This paper identified the genetic basis of gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS), a newly discovered hereditary gastric cancer risk syndrome.
Tsuchiya T, Tamura G, Sato K, Endoh Y, Sakata K, Jin Z, et al. Distinct methylation patterns of two APC gene promoters in normal and cancerous gastric epithelia. Oncogene. 2000;19:3642–6.
Foretová L, Navrátilová M, Svoboda M, Grell P, Nemec L, Sirotek L, et al. GAPPS - gastric adenocarcinoma and proximal polyposis of the stomach syndrome in 8 families tested at Masaryk Memorial Cancer Institute - prevention and prophylactic gastrectomies. Klin Onkol. 2019;32:109–17.
Rudloff U. Gastric adenocarcinoma and proximal polyposis of the stomach: diagnosis and clinical perspectives. Clin Exp Gastroenterol. 2018;11:447–59.
McDuffie LA, Sabesan A, Allgäeuer M, et al. β-Catenin activation in fundic gland polyps, gastric cancer and colonic polyps in families afflicted by 'gastric adenocarcinoma and proximal polyposis of the stomach' (GAPPS). J Clin Pathol. 2016;69:826–33.
Boland CR, Shike M. Report from the Jerusalem workshop on Lynch syndrome-hereditary nonpolyposis colorectal cancer. Gastroenterology. 2010;138:2197.e1–7.
Samadder NJ, Baffy N, Giridhar KV, Couch FJ, Riegert-Johnson D. Hereditary cancer syndromes-a primer on diagnosis and management, part 2: gastrointestinal cancer syndromes. Mayo Clin Proc. 2019;94:1099–116.
Ma H, Brosens LAA, Offerhaus GJA, Giardiello FM, de Leng WWJ, Montgomery EA. Pathology and genetics of hereditary colorectal cancer. Pathology. 2018;50:49–59.
Engel C, Loeffler M, Steinke V, Rahner N, Holinski-Feder E, Dietmaier W, et al. Risks of less common cancers in proven mutation carriers with lynch syndrome. J Clin Oncol. 2012;30:4409–15.
Capelle LG, Van Grieken NC, Lingsma HF, et al. Risk and epidemiological time trends of gastric cancer in Lynch syndrome carriers in the Netherlands. Gastroenterology. 2010;138:487–92.
Watson P, Vasen HFA, Mecklin JP, Bernstein I, Aarnio M, Järvinen HJ, et al. The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. Int J Cancer. 2008;123:444–9.
Møller P, Seppälä TT, Bernstein I, Holinski-Feder E, Sala P, Gareth Evans D, et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the prospective Lynch syndrome database. Gut. 2018;67:1306–16.
Bonadona V, Bonaïti B, Olschwang S, Grandjouan S, Huiart L, Longy M, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. Jama. 2011;305:2304–10.
Dominguez-Valentin M, Joost P, Therkildsen C, Jonsson M, Rambech E, Nilbert M. Frequent mismatch-repair defects link prostate cancer to Lynch syndrome. BMC Urol. 2016;16:15.
Karimi M, von Salomé J, Aravidis C, Silander G, Askmalm MS, Henriksson I, et al. A retrospective study of extracolonic, non-endometrial cancer in Swedish Lynch syndrome families. Hered Cancer Clin Pract. 2018;16:16.
Ten Broeke SW, van der Klift HM, Tops CMJ, et al. Cancer risks for PMS2-associated Lynch syndrome. J Clin Oncol. 2018;36:2961–8.
Kim J, Braun D, Ukaegbu C, et al. Clinical factors associated with gastric cancer in individuals with Lynch syndrome. Clin Gastroenterol Hepatol. 2020;18:830–837.e1.
Park YJ, Shin KH, Park JG. Risk of gastric cancer in hereditary nonpolyposis colorectal cancer in Korea. Clin Cancer Res. 2000;6:2994–8.
Ikenoue T, Arai M, Ishioka C, et al. Importance of gastric cancer for the diagnosis and surveillance of Japanese Lynch syndrome patients. J Hum Genet. 2019;64:1187–94.
Saita C, Yamaguchi T, Horiguchi SI, Yamada R, Takao M, Iijima T, et al. Tumor development in Japanese patients with Lynch syndrome. PLoS One. 2018;13:e0195572.
Gupta S, Provenzale D, Llor X, Halverson AL, Grady W, Chung DC, et al. NCCN guidelines insights: genetic/familial high-risk assessment: colorectal, version 2.2019. J Natl Compr Cancer Netw. 2019;17:1032–41.
National Comprehensive Cancer Network. Genetic/familial high-risk assessment: colorectal (Version 1.2020).
Giardiello FM, Allen JI, Axilbund JE, Boland RC, Burke CA, Burt RW, et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US multi-society task force on colorectal cancer. Am J Gastroenterol. 2014;109:1159–79.
Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW, et al. ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223–62 quiz 263.
Jasperson KW, Tuohy TM, Neklason DW, Burt RW. Hereditary and familial colon cancer. Gastroenterology. 2010;138:2044–58.
Walton SJ, Frayling IM, Clark SK, Latchford A. Gastric tumours in FAP. Familial Cancer. 2017;16:363–9.
Mankaney G, Leone P, Cruise M, LaGuardia L, O’Malley M, Bhatt A, et al. Gastric cancer in FAP: a concerning rise in incidence. Familial Cancer. 2017;16:371–6.
Leone PJ, Mankaney G, Sarvapelli S, Abushamma S, Lopez R, Cruise M, et al. Endoscopic and histologic features associated with gastric cancer in familial adenomatous polyposis. Gastrointest Endosc. 2019;89:961–8.
Schreibman IR, Baker M, Amos C, McGarrity TJ. The hamartomatous polyposis syndromes: a clinical and molecular review. Am J Gastroenterol. 2005;100:476–90.
Giardiello FM, Brensinger JD, Tersmette AC, Goodman SN, Petersen GM, Booker SV, et al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000;119:1447–53.
Ishida H, Ishibashi K, Iwama T. Malignant tumors associated with juvenile polyposis syndrome in Japan. Surg Today. 2018;48:253–63.
Howe JR, Mitros FA, Summers RW. The risk of gastrointestinal carcinoma in familial juvenile polyposis. Ann Surg Oncol. 1998;5:751–6.
Riegert-Johnson DL, Gleeson FC, Roberts M, Tholen K, Youngborg L, Bullock M, et al. Cancer and Lhermitte-Duclos disease are common in Cowden syndrome patients. Hered Cancer Clin Pract. 2010;8:6.
Heald B, Mester J, Rybicki L, Orloff MS, Burke CA, Eng C. Frequent gastrointestinal polyps and colorectal adenocarcinomas in a prospective series of PTEN mutation carriers. Gastroenterology. 2010;139:1927–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no potential conflicts of interest to disclose that are relevant to the manuscript. BAL receives grant support from the National Institutes of Health T32 DK007017. XL research is partially funded by R01-CA242914.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Genetics in Gastroenterology Practice
Rights and permissions
About this article
Cite this article
Lerner, B.A., Llor, X. Genetic Gastric Cancer Risk Syndromes. Curr Treat Options Gastro 18, 604–615 (2020). https://doi.org/10.1007/s11938-020-00312-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-020-00312-z