Abstract
Endoscopic screening and surveillance of Barrett’s esophagus (BE) are limited to the small volume of tissue sampled by random biopsies, leaving a large area of metaplasia that may contain unidentified dysplasia. Technologies to better assess the mucosa and direct further examination or to better diagnose the severity of disease represent an evolution of the endoscopic surveillance of BE. Wide-area transepithelial sampling of the esophagus with computer-assisted three-dimensional analysis (WATS3D) and endoscopic microscopy including confocal laser endomicroscopy (CLE) or optical coherence tomography (OTC) may improve the ability to diagnose and manage patients with BE. In this chapter, we will review these emerging technologies, their application, and the clinical evidence behind their use.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Gastroesophageal reflux disease (GERD) is an increasingly common diagnosis worldwide, displaying commonality in populations with increased rates of obesity. Within the United States (US), approximately 20% of the population suffers from GERD [1]. GERD is a significant risk factor for the development of Barrett’s esophagus (BE). BE is characterized by the metaplastic change of esophageal mucosa from stratified squamous epithelium to columnar epithelium (columnar-lined esophagus or goblet-cell metaplasia). The incidence of BE in the US is between 5–6% and is a known risk factor for the development of esophageal adenocarcinoma [2]. Advanced esophageal adenocarcinoma has a poor prognosis, making the early detection, proper surveillance of disease progression, and (if indicated) eradication of BE essential components of the endoscopic management of metaplasia.
The most commonly used endoscopic detection strategy, the “Seattle Protocol, “ requires the endoscopist to perform four quadrant forceps biopsies (FB) every 1–2 cm along the length of the columnar-lined portions of the esophagus, with separate biopsies of any other suspicious areas such as masses, nodules, or areas of ulceration [3]. This random sampling is performed in an attempt to identify any areas of dysplasia in an early and curable stage. A prospective study demonstrated that after the institution of a rigorous surveillance and sampling protocol for BE, there was an increase in the number of identified cases of dysplasia and invasive cancer [4]. Unfortunately, several studies have shown that as the length of the segment of BE increases, adherence to the protocol guidelines and the subsequent rate of dysplasia detection both decrease [5, 6].
Endoscopic methods of BE screening and surveillance with higher rates of detection are becoming more widely available. Wide-area transepithelial sampling of the esophagus with computer-assisted three-dimensional analysis (WATS3D, CDx Diagnostics, Suffern, NY) provides more effective tissue sampling. Endoscopic microscopy (EM) utilizing confocal laser endomicroscopy (CLE) or optical coherence tomography (OCT) allow direct visual identification of dysplasia without the need for direct tissue sampling. These methods hold promise to permit the detection of dysplasia within BE sooner than could be detected by random biopsy samples, thereby altering the subsequent management strategy to one of BE eradication or resection.
Wide-Area Transepithelial Sampling
WATS3D has emerged as an adjunctive therapy to current methods, assisting in the early detection and surveillance of BE. WATS3D has recently been endorsed by the Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy [7]. The Society of American Gastrointestinal and Endoscopic Surgeons Technology and Value Assessment Committee concluded that WATS3D is “a safe and effective adjunct to forceps biopsies (FB) in the evaluation of Barrett’s Esophagus, Low-Grade Dysplasia (LGD), and High-Grade Dysplasia (HGD).” [7, 8].
Technology Overview
WATS3D is used as an adjunctive method to the Seattle protocol in the identification and surveillance of patients with BE. The system is comprised of an abrasive brush that is passed through the working channel of the endoscope (Fig. 15.1). This brush is passed along the esophageal mucosa and rotated circumferentially, obtaining transepithelial specimens over a broad area of the esophagus in contact with the device (Fig. 15.2). The brush is capable of obtaining deep samples down to the lamina propria. The WATS3D sampling adds an average of 4.5 min to the total procedure time [9].
The brush is removed, and the samples are plated, stained, and examined at the CDx Diagnostics Laboratory. A computational analysis consisting of a neural network and a high-speed scanning system is capable of identifying abnormal cells. The proprietary system allows three-dimensional viewing of the tissue fragments (Fig. 15.2). Suspicious cells are flagged by the system to then be reviewed by pathologists using the 3D system, as well as conventional microscopy, using published and commonly accepted pathologic criteria used to evaluate specimens for BE (Fig. 15.3). Indications for WATS3D include patients who are undergoing endoscopy for evaluation of reflux, peptic ulcer disease, and screening or surveillance for BE. WATS3D is not recommended as a substitute for the Seattle protocol but should be performed as an adjunctive measure for diagnosis and detection.
Clinical Evidence
Multiple published studies have examined the clinical validity of WATS3D as an adjunct to the Seattle protocol. Johanson et al. reported their results of a multicenter prospective trial of patients who were undergoing screening for BE and esophageal dysplasia [10]. Of the 1266 patients who were enrolled, 363 were diagnosed with BE after FB, with an additional 146 cases identified after adding WATS3D. This increase in BE diagnosis of 11.5% of all patients tested resulted in a number needed to test for each additional BE diagnosis of 8.7. Within the subset of patients with a history of GERD without a previous diagnosis of BE, adding WATS3D to FB identified an additional 105 patients with BE increasing the detection rate by 70.5%. Finally, with FB alone, dysplasia was diagnosed in 16 cases, with 14 additional cases identified by adding WATS3D, increasing the detection rate by 87.5%.
Anandasabapathy et al. reported their results of a multi-institution trial examining the detection of dysplasia during surveillance of patients with BE using computer-assisted brush biopsy analysis [11]. After enrolling 151 patients from 4 institutions, they identified 117 patients (77.5%) with specimens adequate for interpretation. The overall yield of FB for detection of dysplasia was 25.2% (n = 38). Brush biopsy added an additional 16 cases, increasing the yield of detection by 42%. This resulted in a number needed to test to detect one additional case of dysplasia of 9.4 (95% CI: 6.4–17.7).
Gross et al. reported the results of their multicenter prospective trial of patients with known BE undergoing surveillance and patients screened for suspected BE at 25 community-based practices utilizing WATS3D adjunctively with FB [12]. Among the 4203 patients enrolled, FB diagnosed 594 with BE, with an additional 493 patients identified by adding WATS3D, an increase of overall detection of BE of 83%. Low-grade dysplasia was identified in 26 patients using FB alone, with 23 additional cases identified with the addition of WATS3D, increasing the identification of low-grade dysplasia by 88.5%.
Vennalaganti et al. reported their results of a multi-institutional randomized trial of 160 BE patients undergoing surveillance [9]. The primary endpoint was the detection of high-grade dysplasia or esophageal adenocarcinoma (HGD/EA) using WATS3D followed by FB compared to FB followed by WATS3D. Forceps biopsy sampling alone yielded seven cases (4.4%) of HGD/EA, while the addition of WATS3D yielded an additional 23 cases (an absolute increase of 14.4%).
Smith et al. reported the results of their multicenter prospective trial examining WATS3D as an adjunct to both targeted and random FB in patients undergoing BE screening or surveillance. Twelve thousand eight hundred ninety-nine patients were enrolled, and FB identified 88 cases of esophageal dysplasia (0.68%). WATS3D identified an additional 213 cases missed by FB, representing an absolute increase of 1.65% and a remarkable 242% overall increase in detection. Forceps biopsy identified 1684 cases of BE, while WATS3D identified an additional 2570 cases, increasing the overall detection of BE by 153%. The number needed to test with WATS3D in order to identify an additional case of BE was 5. The order in which FB and WATS3D were performed did not affect the results.
Given the sampling error inherent to FB-based surveillance protocols, the need for adjunctive sampling and screening methods seems evident. Only 4% of the examined esophagus is biopsied using the Seattle protocol, leaving potential areas of dysplasia unsampled [13]. As we pointed out earlier, patients with longer segments of BE tend to undergo inadequate sampling. Alarmingly, these are the very patients who are at the highest risk of having dysplasia within their BE.
Despite these apparent advantages, there are questions that remain. It is unclear which patients would benefit most from screening or surveillance with WATS3D or if all patients with suspected BE should undergo testing. Some authors worry that the addition of WATS3D may result in false positives and overdiagnosis [14]. Whether this is true or not is speculation and warrants further study.
Importantly, the reported morbidity is acceptably low, with no significant morbidity or mortality reported in the literature [8]. Issues of insurance coverage for WATS3D also remain; while FB is a universally afforded benefit, WATS3D analysis may not be reimbursed.
Endoscopic Microscopy
Endoscopic microscopy is the name given to a variety of tools and techniques that permit the assessment of tissue architecture at a level of resolution similar to standard histopathological analysis. Compared to standard white light endoscopy (WLE), EM permits a more in-depth analysis of the esophageal mucosa by providing a real-time in vivo histologic assessment of the whole epithelial thickness without the need for physical tissue removal via biopsy.
Confocal Laser Endomicroscopy
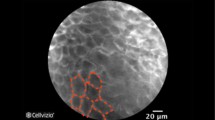
Confocal Laser Endomicroscopy (CLE) is an advanced imaging technique used to evaluate BE. It can magnify esophageal mucosa up to 1000 times and acquire images 250 micrometers below the tissue surface. The technology is based on the technique of illuminating the tissue with a low-power laser and detecting fluorescent light that is reflected from the target tissue. Intravenous or topically-applied agents are required to assist with the fluorescence. CLE can either be performed with a specialized scope, where the microscope is placed on the tip of the scope or probe-based, where the microscope is passed through the working channel of a standard endoscope (Figs. 15.4 and 15.5).
The probe-based system (Cellvizio, Mauna Kea Technologies, Paris, France) is the only system currently available for use in the US. It consists of a microprobe that is advanced through the working channel of most commercially available endoscopes. This probe is reusable if properly sterilized between uses. The probe has a fixed focal length and is available for different settings, including upper endoscopy, lower endoscopy, endoscopic retrograde cholangiopancreatography (ERCP), and a probe that can be passed through a 19 g needle used during endoscopic ultrasound (EUS) used for the evaluation of pancreatic lesions [15].
In a meta-analysis examining the use of CLE for the detection of cancer in patients with BE, Wu et al. reported pooled data from 709 patients [16]. They found the per-patient sensitivity for CLE in the detection of neoplasia was 89% with a specificity of 75%. Canto et al. reported their results of a prospective, randomized control trial of 192 patients undergoing BE surveillance with either high definition WLE with random biopsies or high definition WLE with CLE with targeted biopsies [17]. They found that including CLE led to a lower number of biopsies with a higher diagnostic yield for cancer detection (34% vs. 7%; P < 0.001). However, other randomized trials had conflicting results showing no clinical benefit to using CLE compared to high definition WLE [18].
Optical Coherence Tomography
Optical coherence tomography (OCT) is a technology capable of obtaining cross-sectional images of tissue with resolution equivalent to a low-powered microscope. The methodology of OCT can be thought of as an ‘optical ultrasound’; reflections of light that penetrate the tissue surface are used to create images. With standard WLE imaging, the light that hits the tissue and diffusely scatters is used to create the image. OCT is based on interferometry, a process by which light from a source is divided into two beams and directed toward the tissue and toward a moveable reference mirror. This permits the optical path length of the light beams to be measured. Photons of light that are reflected from the tissue are used to generate an image, while photons of light that have scattered before detection are rejected. As the signal is processed, OCT can build cross-sectional two-dimensional and three-dimensional images by rejecting background noise (scattered light) and accepting only light signals reflected from the sub-surface tissue layers.
In the first prospective study with the technology, using ultra-high definition OCT, 121 patients were examined for the following criteria when screening for BE: lack of normal esophageal morphology, inhomogeneous tissue contrast, and presence of submucosal glands [19]. The authors found that when two of the three diagnostic criteria were met, the sensitivity for detecting BE was 97%, and the specificity was 92% when compared to histology. One of the drawbacks of OTC is the high interobserver variability due to the subjective nature of the interpretation of the data. Furthermore, obtaining and interpreting the data from OTC can be time-consuming and may not be ideal for screening or surveillance purposes due to the time needed to perform the test. One prospective study comparing WLE and OTC reported that using OCT imaging added an average of 12 min (range 3–20 min) to the study [20].
Conclusions
BE is a known risk factor for the development of esophageal adenocarcinoma, which holds a poor prognosis in its advanced stages. The current endoscopic diagnosis and protocolled surveillance of BE are limited by the small amount of tissue sampled and may leave behind undiagnosed dysplasia. The addition of WATS3D as an adjunct to the Seattle protocol increases the diagnosis of BE, low and high-grade dysplasia, and esophageal adenocarcinoma without significant increases in time spent during the procedure or morbidity. Emerging EM and other real-time imaging modalities that obviate the need for tissue sampling are evolving and may represent a more efficient and directed form of assessment and diagnosis.
Acknowledgments
Dr. Caitlin Houghton at the University of Southern California for providing images of WATS3D for this manuscript.
References
Patti MG. An evidence-based approach to the treatment of gastroesophageal reflux disease. JAMA Surg. 2016;151(1):73–8.
Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371(9):836–45.
Levine DS, Haggitt RC, Blount PL, Rabinovitch PS, Rusch VW, Reid BJ. An endoscopic biopsy protocol can differentiate high-grade dysplasia from early adenocarcinoma in Barrett’s esophagus. Gastroenterology. 1993;105(1):40–50.
Fitzgerald RC, Saeed IT, Khoo D, Farthing MJ, Burnham WR. Rigorous surveillance protocol increases detection of curable cancers associated with Barrett’s esophagus. Dig Dis Sci. 2001;46(9):1892–8.
Abrams JA, Kapel RC, Lindberg GM, et al. Adherence to biopsy guidelines for Barrett’s esophagus surveillance in the community setting in the United States. Clin Gastroenterol Hepatol. 2009;7(7):736–42. quiz 10
Curvers WL, Peters FP, Elzer B, et al. Quality of Barrett’s surveillance in the Netherlands: a standardized review of endoscopy and pathology reports. Eur J Gastroenterol Hepatol. 2008;20(7):601–7.
Qumseya B, Sultan S, et al. ASGE guideline on screening and surveillance of Barrett’s esophagus. Gastrointest Endosc. 2019;90(3):335–59 e2.
Docimo S Jr, Al-Mansour M, Tsuda S. SAGES TAVAC safety and efficacy analysis WATS(3D) (CDx diagnostics, Suffern, NY). Surg Endosc. 2020;34(9):3743–7.
Vennalaganti PR, Kaul V, Wang KK, et al. Increased detection of Barrett’s esophagus-associated neoplasia using wide-area trans-epithelial sampling: a multicenter, prospective, randomized trial. Gastrointest Endosc. 2018;87(2):348–55.
Johanson JF, Frakes J, Eisen D, Endo CCG. Computer-assisted analysis of abrasive transepithelial brush biopsies increases the effectiveness of esophageal screening: a multicenter prospective clinical trial by the EndoCDx collaborative group. Dig Dis Sci. 2011;56(3):767–72.
Anandasabapathy S, Sontag S, Graham DY, et al. Computer-assisted brush-biopsy analysis for the detection of dysplasia in a high-risk Barrett’s esophagus surveillance population. Dig Dis Sci. 2011;56(3):761–6.
Gross SA, Smith MS, Kaul V, Group USCWDS. Increased detection of Barrett’s esophagus and esophageal dysplasia with adjunctive use of wide-area transepithelial sample with three-dimensional computer-assisted analysis (WATS). United Eur Gastroenterol J. 2018;6(4):529–35.
Harrison R, Perry I, Haddadin W, et al. Detection of intestinal metaplasia in Barrett’s esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am J Gastroenterol. 2007;102(6):1154–61.
Canto MI, Montgomery E. Wide-area transepithelial sampling with 3-dimensional cytology: does it detect more dysplasia or yield more hype? Gastrointest Endosc. 2018;87(2):356–9.
Al-Mansour MR, Caycedo-Marulanda A, Davis BR, et al. SAGES TAVAC safety and efficacy analysis confocal laser endomicroscopy. Surg Endosc. 2021;35(5):2091–103.
Wu J, Pan YM, Wang TT, Hu B. Confocal laser endomicroscopy for detection of neoplasia in Barrett’s esophagus: a meta-analysis. Dis Esophagus. 2014;27(3):248–54.
Canto MI, Anandasabapathy S, Brugge W, et al. In vivo endomicroscopy improves detection of Barrett’s esophagus-related neoplasia: a multicenter international randomized controlled trial (with video). Gastrointest Endosc. 2014;79(2):211–21.
Wallace MB, Crook JE, Saunders M, et al. Multicenter, randomized, controlled trial of confocal laser endomicroscopy assessment of residual metaplasia after mucosal ablation or resection of GI neoplasia in Barrett’s esophagus. Gastrointest Endosc. 2012;76(3):539–47 e1.
Poneros JM, Brand S, Bouma BE, Tearney GJ, Compton CC, Nishioka NS. Diagnosis of specialized intestinal metaplasia by optical coherence tomography. Gastroenterology. 2001;120(1):7–12.
Isenberg G, Sivak MV Jr, Chak A, et al. Accuracy of endoscopic optical coherence tomography in the detection of dysplasia in Barrett’s esophagus: a prospective, double-blinded study. Gastrointest Endosc. 2005;62(6):825–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
JSW recieves consulting fees from Boston Scientific. EMP receives honoraria from Becton Dickinson, Medtronic, Ovesco, Cook Biotech, Boston Scientific, Actuated Biomedical, Baxter, Wells Fargo, CMR Surgical, and royalties from Up-To-Date and Springer.
Rights and permissions
Copyright information
© 2023 SAGES
About this chapter
Cite this chapter
Winder, J.S., Pauli, E.M. (2023). Barrett’s Esophagus Surveillance: WATS, Real-Time Endoscopic Microscopy. In: Kroh, M., Docimo Jr., S., El Djouzi, S., Shada, A., Reavis, K.M. (eds) The SAGES Manual Operating Through the Endoscope. Springer, Cham. https://doi.org/10.1007/978-3-031-21044-0_15
Download citation
DOI: https://doi.org/10.1007/978-3-031-21044-0_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-21043-3
Online ISBN: 978-3-031-21044-0
eBook Packages: MedicineMedicine (R0)