Abstract
The introduction of bulk-fill resin composite restorations can be regarded as one of the most significant advances in restorative dentistry. Thanks to their physical and setting characteristics, restoration of deep cavities is now simpler and more efficient with the use of bulk-fill restoratives as they eliminate the need for incremental placement of composite material and thereby reduce the risk of void inclusion within the final restoration. Consequently, bulk filling strategies have received significant interest, which has fuelled further research and development. The past few years have witnessed significant advances in the chemistry of bulk-fill materials and application techniques that have culminated in the emergence of commercially available materials with promising potential for long-term clinical success. This chapter highlights the already achieved progress in bulk-fill resin composite materials and explores potential improvements that may lead to predictable in vivo performance of such materials in the following aspects:
-
Self-adhesive properties.
-
Ion releasing, bioactive, and cariostatic properties.
-
Self-healing or self-sealing properties.
-
Aesthetic properties.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
10.1 Self-Adhesive Resin-Based Bulk-Fill Materials
Adhesive bonding of conventional direct resin composite restorations is a complex, technique sensitive, and time-consuming process. It requires application and curing of the adhesive resin layer prior to the placement of the resin composite. Self-adhesive restoratives would negate the need for tooth surface conditioning, adhesive bonding, and mechanical retentive features, where indicated. Self-adhesive materials are highly desired by clinicians owing to their efficiency and use for treating challenging situations such as uncooperative patients, cases where prolonged moisture control is unfeasible, or patients who cannot tolerate lengthy dental treatment due to chronic medical conditions.
The global trend of amalgam phasedown has driven significant research and development on self-adhering bulk-fill amalgam substitutes. Resin modified glass ionomer (RMGI) based restoratives are amongst the most widely used and tested materials. This group of materials exhibits the advantages of bulk-fill restoratives in addition to their cariostatic activity due to the fluoride release. However, reduced bonding to tooth structure [1], lack of strength [2] as well as their diminished wear resistance [2, 3], and moisture sensitivity [4] are among the major drawbacks of these materials.
Conventional resin composites are inherently unable to bond to tooth structure and thereby an adhesive system should be used with such restorations [5]. That being said, several strategies have been implemented to produce self-adhering resin composites in order to simplify restorative treatments. One of the earliest strategies was to modify the viscosity controller monomers or the so-called reactive diluents. The modification involves addition of acidic moieties to the reactive diluents in order to promote adhesion to tooth structure. This group of materials bonds to tooth structure primarily via the interaction of phosphate functional groups with calcium ions within hydroxyapatite crystals and secondarily through micromechanical interlocking between the polymerized monomer and collagen fibres of dentin.
10.1.1 Self-Adhesive Resin Composites with Acidic Resin Matrix
One of the earliest commercially available self-adhering flowable composites (Vertise Flow; Kerr, CA, USA) contained a phosphoric-acid ester methacrylate and glycerol-phosphate dimethacrylate (GPDMA) as acidic functional monomers [1]. The phosphate functional group had an acidic phosphate group for etching tooth structure and two methacrylate groups for co-polymerization with other methacrylate monomers [6]. Despite the lower nano-leakage exhibited by such self-adhering flowable composites compared to conventional counterparts [5], its’ retention and bond strength to dentin and interfacial adaptation to enamel and dentin have been sub-optimal as indicated by in vitro [6, 7] and clinical [8] studies. Fusio Liquid Dentin (Pentron, Orange, CA, USA), another commercially available self-adhering flowable resin composite that chemically bonds to tooth structure using 4-methacryloxyethyl trimellitic acid (4-META) which is able to partially demineralise dentin and to form ionic bonds between its carboxylate groups and calcium ions [9]. The latter material was associated with low bond strength [9, 10] and poor clinical performance [11]. One experimental self-adhesive, micro-hybrid resin composite material (code: Exp.564, 3 M Oral Care, Seefeld, Germany) was investigated [12]. The two-paste material utilized the well-known phosphoric acid-6-methacryloxy-hexylesters (15–25% wt) adhesive monomer [12]. Preliminary micro-tensile bond strength data suggested optimal bonding to dentin though less promising results were observed with enamel. Furthermore, interfacial analysis using transmission electron microscopy revealed a tight interface formed between the experimental material and bur-cut enamel and dentin with limited evidence of micro-tag formation and superficial demineralisation [12].
10.1.2 Modified Polyacid Systems (MOPOS)
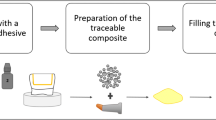
Recently, a new self-adhesive bulk-fill resin composite was commercially introduced as Surefil One (SF-I; Dentsply Sirona, Germany). The self-adhesive properties of this material are obtained via modification of the structural monomer rather than the reactive diluent. The key component of this material is the patented modified polyacid system (MOPOS). The modification involves the use of polyacids, similar to those used in glass ionomer (GI) as a backbone. The high number of carboxylate groups within the polyacid backbone allows adhesion with enamel and dentin via ionic bonds with calcium ions within the tooth structure. Furthermore, acidic groups can bond the structural monomer to the glass fillers. The formation of an ionic bond between the carboxylate groups and calcium ions requires an aqueous environment, hence the addition of water to the formula of SF-I. The presence of water necessitates the use of hydrolytically stable, polymerizable groups (methacrylamide) that can be crosslinked with the reactive diluent. Furthermore, cross-linker molecules and reactive diluent need to be water-soluble and hydrolytically stable. In SF-I, a medium viscosity cross-linker with two polymerizable groups (BADEP) is used. A low viscosity reactive diluent, the acrylic acid, which also can adhere to tooth structure and reactive fillers via ionic bonds is also used in SF-I. Barium glass fillers of conventional resin composites cannot be used in SF-I owing to the presence of water in the formula. The low refractive index filler system used in SF-I contains aluminium-phosphor-strontium-sodium-fluorosilicate glass, highly dispersed silicon dioxide and ytterbium fluoride. Silanization of the fillers allows strong adhesion to the resin matrix within the system. The material is available in light-cure or self-cure modes. The light polymerization initiator system is comprised of camphorquinone along with two different reducing agents. To fulfil the bulk-fill objective, a redox initiator (potassium persulphate) is used to initiate radical polymerization reaction in order to mediate the chemical or dark cure process of SF-I. Figure 10.1: Graphical illustration of various components of the SF-I and their interaction among each other and with tooth structure.
The evidence pertaining to the bonding effectiveness of SF-I to tooth structure is limited. Shear bond strength of SF-I to enamel was comparable to that obtained with a conventional resin composite bonded using a universal self-etch adhesive [13]. SF-I also exhibited similar bond strength to dentin when compared to a light cured RMGI or hybrid glass restorative materials. The bond strength of such materials was, however, significantly lower when compared to a conventional resin composite bonded with a universal, self-etch adhesive [13]. Nonetheless, shear bond strength values of SF-I (21–26 MPa) may be within clinically acceptable values and similar to materials with favourable long-term clinical success. Furthermore, the bond strength of SF-I to dentin was similar when the material is applied to moist or desiccated dentin indicating that using such material may reduce the incidence of post-operative sensitivity associated with excessive drying of dentin and may be more forgiving in cases where optimum moisture control cannot be achieved [14]. Additionally, finishing of cavity preparation appeared to be critical to the bond strength of SF-I as the shear bond strength to dentin was significantly reduced when SF-I was applied to dentin covered with a thick smear layer [14]. The effectiveness of bonding of SF-I to dentin has been demonstrated in both flat dentin (low c-factor) and class I cavity preparations (high c-factor). The light-cured SF-I exhibited significantly higher immediate and post-fatigue microtensile bond strength to flat dentin when compared to a reference RMGI material. In high c-factor configurations, self-cured SF-I exhibited microtensile bond strength comparable to a bonded restoration placed using a self-etch adhesive, resin-based bulk-fill restorative material [1]. With regard to material wear, SF-I exhibited less localized and generalized wear when compared to GI, RMGI, and bioactive RMGI materials [3]. SF-I also exhibited mechanical performance close to that for some commercially available micro-filled (Heliomolar; Ivoclar Vivadent, Germany) and nano-filled resin composites (CeramX mono+; Dentsply Sirona, Germany). Processing the material in either self-cure or light-cure mode led to superior mechanical performance over a GI based material (Fuji II LC; GC, Japan) but significantly inferior when compared to a conventional, nano-cluster filled resin composite (Filtek Supreme; 3 M Oral Care, USA) [15]. Furthermore, SF-I exhibited stable fracture behaviour and comparable marginal quality as compared to resin composite bonded with self-etch adhesive when used as bulk MOD restorations in molar teeth especially when used in light-cured modus [2].
Self-adhering bulk-fill restoratives would be a significant asset in clinical practice. However, they should be thoroughly verified in vitro and tested for long-term durability in vivo. Table 10.1 summarizes the composition and literature pertaining the performance of some commercially available self-adhesive resin-containing bulk-fill materials.
10.2 Ion Release, Bioactive, and Antibacterial Properties of Resin-Based Bulk-Fill Materials
The widespread popularity of GI-based materials is largely attributed to their fluoride ion release and uptake. GI-based materials exhibit anticariogenic properties owing to the bacteriostatic effect of fluoride ions and the increased resistance of hard tissues containing fluoride to acid dissolution [16]. Several materials have recently been developed in order to preserve the simplicity of application, ion release and cariostatic properties whilst mitigating the shortcomings associated with GI-based materials such as poor aesthetics and reduced mechanical properties. Furthermore, the adoption of the biomimetic approach in various disciplines in dentistry has fuelled the development of bioactive restoratives. The objective of such bioactive restoratives is to overcome the drawbacks associated with amalgam alternatives, namely marginal gap and microleakage.
10.2.1 Resin Composites with Alkaline Fillers
Bioactive materials can be defined as materials that can affect a biological process, namely remineralisation of dental hard tissues, as a result of the interaction with the surrounding environment. In restorative materials, the bioactive glass filler system is the reactive component and responsible for releasing, upon degradation at neutral pH, calcium, and phosphate ions leading to the formation of an apatite-like phase to fill the marginal gap [17]. Ion release is also associated with pH buffering in acidic environment especially if the bioactive filler contains an alkaline component. Activa bioactive restorative (AB; Pulpdent, USA) is a heavily marketed resin-containing, bioactive bulk-fill restorative. AB was claimed to exhibit self-adhesive properties owing to the ionic interaction between phosphate acid groups within the so-called ionic resin matrix and calcium ions within the tooth structure. Furthermore, the manufacturer asserts that the bioactive glass filler system promotes mineral apatite formation and remineralisation at the restoration-tooth interface. However, several in vitro studies have cast doubt on AB’s performance. The self-adhesiveness of AB was deemed nonexistent in one study [18], others reported a significantly lower bond strength to enamel and dentin as compared to conventional resin composites and other self-adhering restoratives [13, 14, 19]. Furthermore, AB exhibited lower wear resistance when compared to conventional resin composites [2]. Clinical data regarding the performance of AB is mixed, one study demonstrated poor treatment outcomes (annual failure rate = 24.1%) and the primary cause of failure was loss of retention followed by post-operative symptoms and secondary caries [20]. In contrast, another study reported comparable, short-term clinical performance of AB and a nanohybrid resin composite [21]. Regarding the bioactivity, one study demonstrated lack of glass degradation and apatite formation with AB under different experimental conditions [22]. Another study revealed that AB underscores a conventional RMGI based bulk-fill restorative in terms of fluoride release [23]. Rigorous in vitro verification of the performance of AB is warranted in order to determine the clinical benefits and the scope of indications for such material in clinical practice.
Alkasite, a recently introduced tooth-coloured restorative material which is comprised of alkaline fillers embedded in a resin matrix. Cention N (CN; Ivoclar Vivadent, Germany) is a commercially available alkasite processed by hand mixing powder and liquid. Its application requires the use of an adhesive bond in non-retentive cavity preparations hence it is not considered a self-adhering material. The currently-available evidence suggests that using adhesive bonding with CN results in less microleakage [24] and improves bond strength to dentin acting as an intermediary reliever of polymerisation stresses [1]. The material is primarily self-cured and utilizes thiocarbamide, hydroperoxide and copper salt as chemical initiators. Light curing of CN is optional but effective to accelerate the setting of the surface layer (4 mm) of the material. The photoinitiator system is comprised of a dibenzoyel germanium derivative (Ivocerin) and an acyl phosphine oxide. Ivocerin exhibits a higher photocuring reactivity and light-absorption in the 400–450 nm wavelength range as compared to camphoroquinone [1, 25]. CN contains four different dimethacrylate based monomers and urethane dimethacrylate is the main component of the monomeric matrix. The monomer matrix comprises approximately 12–40 (wt%) of the set material. The powder contains the inorganic fillers (particle size: 0.1–35 μm, 78.4 wt%) including barium aluminium silicate glass filler, ytterbium trifluoride, an isofiller, calcium barium aluminium fluorosilicate, and calcium fluorsilicate. The last two fillers are primarily responsible for the ion release exhibited by this material. Calcium fluorsilicate, the alkaline filler comprises 24.6 (wt%) of the set material and is responsible for calcium, hydroxyl, and fluoride ion release [26]. Hydroxyl ions released from CN can play an important role in neutralizing acidic conditions generated by cariogenic flora or acidic foods and drinks. Further, hydroxyl ions may lead to higher plaque pH thus reducing the demineralisation potential of biofilm in the vicinity of the restoration [27]. CN releases calcium and fluoride ions and forms an apatite-like phase upon immersion in artificial saliva (pH = 7.0) [22]. An in vitro study revealed that CN (self-cured) has the highest fluoride ion release and alkalizing potential in acidic pH as compared to CN (light-cured) and a GI-based material [28]. Furthermore, CN was associated with higher fluoride ion release and recharge capacity when compared to other GI-based materials [29, 30]. CN was also associated with significantly smaller demineralised areas in enamel and dentin following an artificial caries challenge as compared to a conventional resin composite material [31]. Despite having a rougher surface following finishing procedure, CN exhibited lower S. mutans adhesion as compared to a smoother resin composite counterpart [32]. In the light of the presented evidence, CN meets the criteria of a bioactive material and can potentially reduce microleakage and might be of a significant clinical benefit owing to the anticariogenic potential. However, several aspects regarding the bioactivity of CN are yet to be thoroughly investigated especially the effects of using an adhesive resin with the material on the ion release and uptake potential.
CN exhibited a higher degree of conversion compared to a hybrid resin composite restorative [33]. Furthermore, it exhibited comparable dentin shear bond strength to a nano-hybrid [34] and a flowable bulk-fill [35] resin composites when all used materials bonded to dentin using etch-rinse-bond. Moreover, CN exhibited significantly higher microtensile bond strength to dentin when compared to a RMGI material [1]. CN demonstrates superior mechanical, aesthetic, and marginal sealing properties when compared to conventional GI and RMGI restoratives [33, 36]. When compared to hybrid resin composite restorative, CN demonstrated lower microleakage and inferior flexural strength [36]. The high ion release of CN may indicate increased susceptibility of the filler system to acid attack and hydrolysis which in turn, may reduce wear resistance [22]. Thus, it might be prudent to veneer CN with a conventional resin composite restorative in load bearing areas. Alternatively, additional light curing of the occlusal surface restored with CN may significantly reduce material wear as demonstrated in one in vitro study [37].
10.2.2 Resin Composites with Fluoride-Containing Filler Systems
Incorporation of fluoride containing filler systems in resin composites has long been done in order to exploit the anticariogenic potential of the former. However, a limited number of such resin composite restoratives can be used for bulk-fill application (increment thickness ≥4 mm). Tetric EvoCeram Bulk Fill (TEC; Ivoclar Vivadent, Germany) is one example on fluoride releasing bulk-fill resin composites. The proprietary filler system in TEC is largely responsible for the low polymerisation shrinkage associated with such a material. Ytterbium trifluoride is the filler component responsible for the fluoride release in TEC. Despite lower fluoride ion release compared to conventional GI materials [38], TEC exhibited significantly less demineralisation around restoration margins when compared to a non-fluoride releasing resin composite [39].
Other fluoride containing fillers may include the GI type filler (Fluoro-Alumino-Silicate) and CaF2 nanoparticles [40]. CaF2 nanoparticles are synthesized via spray-drying and capable of releasing high concentrations of fluoride ions [40]. Experimental resin composites containing CaF2 exhibited high release of calcium and fluoride ions as well as potent biofilm inhibition as indicated by the low production of lactic acid, and the decreased colony forming unit [41]. The virtue of using CaF2 nanoparticles is the fact that antibacterial properties and fluoride release occurs at low fillers concentrations (20–30% by mass). This indicates that the bioactivity of such compound can be exploited whilst allowing for incorporation of other strengthening or reinforcing fillers to be used to configure resin composites with optimum mechanical properties. Therefore, incorporating CaF2 nanoparticles could revolutionize bulk-fill resin composites to produce highly bioactive, caries resistant and yet durable bulk-fill restoratives. Table 10.2: Summary of chemical composition and literature pertaining to some commercially available bioactive, ion-releasing bulk-fill resin-based composites.
10.2.3 Resin Composites with Novel/Experimental Filler Systems
Amorphous calcium phosphate (ACP) nanoparticles have demonstrated promising potential for long-lasting calcium and phosphate ion release. One study reported the use of UDMA and triethylene glycol divinylbenzyl ether (TEG-DVBE), 3% dimethylaminohexadecyl methacrylate (DMAHDM), and 20% ACP nanoparticles to produce an antibacterial and bioactive low-shrinkage resin composite [42]. DMAHDM possess strong antibacterial activity, TEG-DVBE exhibits lower susceptibility to enzymatic and hydrolytic degradation, UDMA is a high molecular weight structural monomer that higher exhibits high stability toward salivary hydrolysis, greater flexibility, and cross-linking density which confer improved mechanical properties and low polymerisation shrinkage [42]. The ACP experimental resin composite achieved substantial long-term (3 months) antibacterial activity as indicated by the significant reduction of S. mutans biofilm colony-forming units and lactic acid production. Furthermore, high resistance to S. mutans biofilm acidic attack was observed with the experimental ACP resin composite as indicated by the significantly higher dentin hardness in the vicinity of dentin-composite interface as compared to a conventional resin composite restorative. The ACP experimental resin composite exhibited significantly lower polymerization shrinkage stress and similar mechanical properties as compared to a conventional resin composite restorative [42]. However, the study did not specify as to whether this experimental material can be used for bulk fill or incremental application.
Other bioactive materials have been explored as potential fillers for resin composite materials. Calcium sodium phosphosilicate (Bioglass 45S5) and Portland cement have been investigated as modifiers for commercially available bulk-fill restoratives. Bioglass 45S5 (20 wt%) did not adversely affect the degree of conversion or hardness of the investigated bulk-fill restoratives. Portland cement was, however, found to have a deleterious effect on the polymerisation of the studied materials as a result of the significant drop in materials’ light transmittance [43]. Niobium-containing bioactive glasses have also promising potential in the development of remineralising resin composites as they do not seem to adversely affect the degree of monomer conversion [44]. They are also associated with high mineral deposition and pulp fibroblasts viability [44]. Such findings were obtained from an in vitro study that utilized the niobium bioactive glass as filler for an adhesive resin. Further studies are required to verify the performance of bulk-fill resin composites doped with such bioactive filler.
The significant progress in biomaterial’s research in bone regeneration may inspire futuristic ideas for bioactive and biocompatible bulk-fill resin composites. Currently, the utility of polymer composites has a predominant role as scaffolds in bone tissue engineering [45]. Chitosan (CS) is a bioactive polymer that exhibits high biocompatibility and antibacterial activity. It can be produced by deacetylation of chitin; a highly abundant natural polysaccharides [45, 46]. CS can be combined with hydroxyapatite, calcium phosphate, resinous materials, or ceramic particles to form strong, and yet bioactive composites [45, 46]. The controlled biodegradability and solubility in acidic environment of CS can be pivotal to achieve cariostatic properties. CS based composites are yet to be implemented in bulk-fill dental restoratives. Despite the promising properties, the impact of biodegradability on biomechanical reliability and durability of such material warrants meticulous consideration.
Carbon nanotubes (CnTs) are allotropes of carbon with a cylindrical nanostructure and constructed with length-to-diameter ratio of up to 28,000,000:1 [45]. CnTs containing composites have attracted great attention as biocompatible coatings for load-bearing orthopaedic implants [45]. CnTs enhance strength and fracture toughness of the composite materials as they exhibit high surface area, low density and exceptionally high strength and stiffness. Besides CnTs’ function as a reinforcing phase to various composites, their role as carrier for bioactive ceramic materials is of a great importance. Incorporation of CnTs based composites in bulk-fill materials may lead to the development of strong and bioactive restoratives that can be effectively used for cusp replacement direct restorations in high load bearing areas. However, application of CnTs in dental resin composites is largely challenged by the difficulty to disperse CnTs within any matrix phase besides challenging production of pure forms of CnTs [45]. Absolute gap free margins seem to be far from achievable with the currently available resin composite restorations and secondary caries remains one of the leading causes for failure [47]. This is primarily related to polymerization shrinkage and placement techniques. Hence, developing material that possess bioactive, antibacterial and low polymerisation shrinkage seems to be the way forward to reduce recurrent caries and improve a restorations’ longevity. Such materials can potentially improve restorations’ longevity at several levels including; smaller marginal gap, lower bacterial colonization or the marginal gap, reduced demineralisation as a result of decreasing acidogenic potential of the bacterial biofilm and buffering capacity of the bioactive fillers, decreased enzymatic degradation of resin composite components and collagen fibres of dentin, and increasing the remineralisation capacity of de novo or remnants carious/demineralised lesions. Furthermore, such bioactive bulk-fill composites may have a great potential to be used as biocompatible bone cements for artificial implants. They might be a biomechanically superior alternative to conventional poly methyl methacrylate cement with a more controlled setting reaction.
10.3 Self-Healing or Crack-Sealing Properties
Bulk fracture or chipping of resin composite restorations are among the leading reasons for restoration repair or replacement [48]. In the oral environment, polymerisation shrinkage, fluctuation of temperature, and repetitive occlusal loading especially in the stress bearing areas may lead to the accumulation of cracks within the restorations. This matter is further complicated in extensive restorations or in the presence of excessive occlusal loading as a result of parafunctional habits. Once a crack propagates to a critical size/length, fracture of the restoration becomes inevitable. Thus, it is paramount to engineer restorative materials to inhibit crack growth and propagation. One of the strategies to fulfil such objective is to integrate a self-healing or a crack-sealing mechanism within the restorative material.
10.3.1 Urea-Based Capsular Shell Systems
A widely investigated self-healing mechanism is based on releasing reactive molecules from micro- or nano-capsules in response to a mechanical stimulus [49]. Such reactive molecules can repair crack damage and recover the mechanical performance of a resin matrix polymer. A recent systematic review identified ten studies and two patents describing self-healing microcapsule-based resin composite restoratives [49]. Poly urea-formaldehyde (UF), melamine-modified UF, and polyoxymethylene urea were all reported as capsular shell material whilst poly UF being the most commonly utilized. In this group of microcapsules, the healing agents used were DCPD, TEGDMA-DHEPT, TMPET, UDMA, Bis-GMA, and MBDMA amine. One study reported using melamine-modified UF with DCPD monomer and no catalyst whilst all other studies reported the use of a catalyst system such as Grubb’s catalyst or benzoyl peroxide [50]. Rupture of microcapsules as a result of crack formation releases the healing monomeric molecules which become in contact with a catalyst that is dispersed within the resin composite matrix. Consequently, a polymerisation reaction leads to the formation of a reparative polymer in the vicinity of the mechanical stimulus that eventually obturate flaws created by propagating cracks.
10.3.2 Silanized Silica Microcapsule Systems
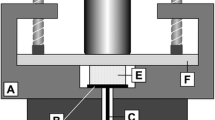
Silanized silica microcapsules have been advocated as an alternative to urea-based counterparts. Silica microcapsules exhibit a lower tendency to rupture owing to the significantly higher shell thickness as compared to poly UF counterparts (160–230 nm vs. 4–8 μm) [49]. However, silanization of the silica microcapsule increases the bond strength to the resin matrix and facilitates microcapsule rupture upon exposure to a propagating crack as well as improves the overall mechanical properties of the self-healing resin composite [49]. Silanized silica microcapsules containing an aqueous solution of polyacrylic acid is another self-healing system that can be used in resin composites [51]. Once ruptured as a result of a propagating crack, polyacrylic acid reacts with amorphous calcium phosphate and strontium fluoroaluminosilicate (healing fillers) within the resin composite to produce reparative GI molecules with an ionic crosslinking network [51] (Fig. 10.2).
10.3.3 Potentials and Limitations of the Current Self-Healing Systems
Implementation of self-healing mechanisms is an optimum utilization of biomimetic approach to overcome a significant problem encountered with resin composite restoratives. Microcapsules loaded with various healing substances resulted in 25–80% recovery of the original fracture toughness in several experimental resin composite restoratives [49]. A significant potential is present for incorporating such technology in bulk-fill resin composites. It has been reported that microcapsules with different healing substances were able to recover the mechanical properties of various bulk, self-adhering polymeric materials with various setting mechanisms [52]. However, the exploitation of such strategy may encounter a multitude of problems related to the technicality of the production and dispersion of microcapsules within a resin composite material. Further, the instability of the catalyst compounds used in self-healing systems when subjected to high temperatures created by light curing may compromise their performance [49]. One major concern with the use of microcapsule technology is the remnant spaces created by the explosion of the microcapsules and their effects on mechanical reliability and surface roughness [49]. Concerns regarding the biocompatibility of the self-healing systems do also exist. DCPD monomer is no longer used in dental materials owing to the high cytotoxicity [53]. Local or systemic toxicity as a result of monomeric healing substance or formaldehyde elution can be of a significant concern [49]. Further research is required to ensure biosafety and efficient delivery of the healing agents in resin composite restoratives (Table 10.3).
10.4 Aesthetic Properties
Achieving an optimum aesthetic result with direct resin composites requires meticulous placement of multiple layers with different opacities/values. In principle, this contradicts the concept of bulk filling and negates many of its advantages. Furthermore, the current bulk-fill restoratives cover basic monochromatic shades and enamel, dentine, body, translucent, and opaque shades are yet to be made available. Rather than using pigments to obtain different shades, structurally coloured resin composites utilize filler systems with refractive index similar to that for the cured resin matrix [54, 55]. This, in turn, results in sufficient light diffusivity to produce the so-called chameleon effect [55]. In one commercially available conventional resin composite (OmniChroma, Tokuyama Dental Corp., Japan), the uniformly sized supra-nano spherical zirconia and silica fillers (260 nm) reflects light in the red-to-yellow spectrum [56]. Similarly, light reflected from adjacent tooth structure is within the same spectrum. The combined light reflection from tooth structure and restoration besides the diffusion of light from the restoration into the nearby tooth structure may lead to enhanced colour matching [57]. This in turn has led to development of universal shade restoratives that could cover a wide range of classical shades.
Bulk-fill restoratives may benefit from such advances in colour chemistry where anterior teeth can be restored in bulk whilst produce an aesthetically appealing outcome. In human teeth, fluorescent emission by ambient UV light occurs primarily in dentine which is related to its organic content [58]. The bluish-white fluorescence of human teeth is the result of a broad emission band with a diffuse peak at 410–420 nm when subjected to near UV excitation [59]. Fluorescence is a key determinant of aesthetic outcome and shade match [60]. Ideal restorative materials should exhibit fluorescence similar to that of natural teeth [59, 60]. Aesthetic performance and shade match was negatively affected with restorative materials that exhibited less intense fluorescence than natural teeth [61]. Rare earth metals have been used in dental resin composites and ceramics to act as lumiphores [59]. However, they reportedly failed to yield fluorescence comparable to that of tooth structure [59]. Semiconductor nanoparticles or the so-called quantum dots may exhibit more potential in manipulation of resin composite’s fluorescence. The highly luminescent, core-shell, Cadmium Selenide-Zinc Sulphide (CdSe/ZnS) composite quantum dots were able to modify the fluorescence of a conventional resin composite material to match that of natural teeth [62]. Such an approach can be of great potential to improve shade matching of bulk-fill restoratives via optimizing fluorescence intensity. However, concerns remain regarding long term performance should this approach be utilized. Several factors within the oral environment such as temperature fluctuation, enzymatic activity, moisture, and oxidation reactions may reduce quantum yield and thereby fluorescence intensity.
10.5 How to Choose from the Ever-Growing Bulk-Fill Restoratives Available to Practitioners
Clinicians have the duty to select the restorative material that meets the functional and aesthetic demands of the patient at the least biological cost and which provides the best available favourable prognosis. The vast and progressively increasing variety of dental materials in the market alongside the increased marketing activities has rendered material selection a difficult task for clinicians. Clinicians should use/update their working knowledge to scrutinize various aspects related to the properties and performance of each material. Being aware of the specifications, advantages, disadvantages, and grades of a particular dental material as well as the clinical demands of the patient is key for optimum material selection.
“The field of dental materials has grown significantly, but the time available for teaching and studying this subject has not”, a statement made in one of the most famous dental materials textbooks more than a decade ago [63]. As of yet, no notable changes to the undergraduate dental curricula could be observed to accommodate the growth of this field. Thus, at the end of this book, we propose a succinct and structured strategy to help the clinicians make a balanced and evidence-based decision to select a particular restorative material.
10.5.1 Choosing Materials in the Same Category
It is always useful to compare a new material to reference counterparts or previous generations of the same material with long-term and documented optimum clinical performance. Independent and long-term clinical studies with a low risk of bias provide optimum evidence and guidance for clinicians in this context. However, with emerging, new materials such studies are scarce. Thus, it is prudent to resort to independent in vitro studies and short-term clinical trials. The findings of such studies should be scrutinized and compared to reference materials in order to make an informed decision on how well this material may perform in a clinical environment.
10.5.2 Using Marketing Data
There are several examples where extensively marketed dental materials failed to convey any advantage when rigorously tested in clinical trials. It is widely accepted that manufacturer-funded studies will very likely report less complication rates and more positive research findings. Of course, such findings can be trusted once confirmed by studies conducted by independent researchers and published in journals with a strict policy to deal with conflict of interest among researchers. Findings from studies comparing materials from the same category manufactured by different competitors can also be utilized effectively to help with material selection.
10.5.3 Moving Beyond P-Values
Leaving aside the controversy among statisticians regarding the validity of the statistical significance as a tool, clinicians should critically appraise research findings and their validity/relevance to clinical practice. In this context, clinicians should understand that materials with significantly superior performance over a competitor counterpart or previous generation may only provide an extra 0.2 mm of clinical attachment gain, 4% reduction in polymerisation shrinkage, or 15 s shorter procedure time, which are all barely measurable and of no clinical significance.
It is also paramount that clinicians assess whether the used methodology adequately answers the research question. In this context, clinicians differentiate between success and survival reported in clinical studies and the implications of the difference between the two outcomes on clinical decision making. In the case of in vitro studies, the burden is larger as deeper knowledge is required to extrapolate clinically relevant data. For instance, cyclic fatigue studies of restored natural teeth are more relevant to the clinical situation compared to static experimental designs utilizing disc- or beam-shaped specimens.
10.5.4 Operator’s Clinical Experience and Expertise
The three pillars that comprise evidence-based dentistry are patient’s needs, scientific evidence, and clinician’s expertise. Whilst clinicians must endeavour to choose materials based on sound research data, they also must ensure that they master the handling of such material. Hands-on training are key to optimize clinical techniques utilizing new dental materials prior to using them for patients.
10.6 Summary
This chapter has explored the progress already achieved with bulk-fill resin composite materials but also potential improvements to this group of materials, that might lead to improved clinical outcomes have been explored in depth. The following conclusions can be drawn:
-
1.
Self-adhering bulk materials would be a significant asset in clinical practice; however, significant research is needed to further develop these materials.
-
2.
Bioactive or bio reactive, ion release, and antimicrobial properties are desirable characteristics for all materials but in this context for bulk-fill resin composite materials. There is much to do, however, to develop these technologies not least to demonstrate the clinical benefit.
-
3.
Whilst self-healing and crack sealing properties are valid areas for further research there are concerns about the biosafety and the efficient delivery of these materials and again the clinical benefits need to be demonstrated in suitably designed and powered clinical trials.
-
4.
Traditionally bulk-fill materials have performed poorly with respect to achieving a good aesthetic outcome. There are interesting, proposed developments to improve the aesthetics of this group of materials but further development and clinical evaluation is required.
References
Yao C, et al. Structural/chemical characterization and bond strength of a new self-adhesive bulk-fill restorative. J Adhes Dent. 2020;22(1):85–97.
Frankenberger R, et al. Amalgam alternatives critically evaluated: effect of long-term thermomechanical loading on marginal quality, wear, and fracture behavior. J Adhes Dent. 2020;22(1):107–16.
Latta MA, et al. In vitro wear resistance of self-adhesive restorative materials. J Adhes Dent. 2020;22(1):59–64.
Cho E, Kopel H, White SN. Moisture susceptibility of resin-modified glass-ionomer materials. Quintessence Int. 1995;26(5):351–8.
Bonsor SJ. Resin-based composite materials: a science update. Dent Update. 2019;46(4):304–12.
Rangappa A, et al. Comparative evaluation of bond strength of self-adhering flowable composites to the dentin prepared with different burs: an in vitro study. J Conserv Dent. 2018;21(6):618–21.
Mine A, et al. Limited interaction of a self-adhesive flowable composite with dentin/enamel characterized by TEM. Dent Mater. 2017;33(2):209–17.
Maj A, et al. A comparative clinical study of the self-adhering flowable composite resin vertise flow and the traditional flowable composite resin premise flowable. Coatings. 2020;10(8):800.
Peterson J, et al. Bonding performance of self-adhesive flowable composites to enamel, dentin and a nano-hybrid composite. Odontology. 2018;106(2):171–80.
Poitevin A, et al. Bonding effectiveness of self-adhesive composites to dentin and enamel. Dent Mater. 2013;29(2):221–30.
Celik EU, Aka B, Yilmaz F. Six-month clinical evaluation of a self-adhesive flowable composite in noncarious cervical lesions. J Adhes Dent. 2015;17(4):361–8.
Hanabusa M, et al. TEM interfacial characterization of an experimental self-adhesive filling material bonded to enamel/dentin. Dent Mater. 2011;27(8):818–24.
Latta MA, et al. Enamel and dentin bond durability of self-adhesive restorative materials. J Adhes Dent. 2020;22(1):99–105.
Latta MA, Radniecki SM. Bond strength of self-adhesive restorative materials affected by smear layer thickness but not dentin desiccation. J Adhes Dent. 2020;22(1):79–84.
Lohbauer U, Belli R. The mechanical performance of a novel self-adhesive restorative material. J Adhes Dent. 2020;22(1):47–58.
Larsen M, Bruun C. Caries chemistry and fluoride-mechanisms of action. In: Textbook of clinical cariology. Copenhagen, Denmark: Munksgaard; 1994. p. 231–54.
Jun S-K, Lee J-H, Lee H-H. The biomineralization of a bioactive glass-incorporated light-curable pulp capping material using human dental pulp stem cells. Biomed Res Int. 2017;2017:2495282.
Benetti AR, et al. Adhesion and marginal adaptation of a claimed bioactive, restorative material. Biomater Investig Dent. 2019;6(1):90–8.
Alkhudhairy FI, Z.H. Ahmad comparison of shear bond strength and microleakage of various bulk-fill bioactive dentin substitutes: an in vitro study. J Contemp Dent Pract. 2016;17:997–1002.
van Dijken JW, Pallesen U, Benetti A. A randomized controlled evaluation of posterior resin restorations of an altered resin modified glass-ionomer cement with claimed bioactivity. Dent Mater. 2019;35(2):335–43.
Bhadra D, et al. A 1-year comparative evaluation of clinical performance of nanohybrid composite with Activa™ bioactive composite in class II carious lesion: a randomized control study. J Conserv Dent. 2019;22(1):92–6.
Tiskaya M, et al. Characterization of the bioactivity of two commercial composites. Dent Mater. 2019;35(12):1757–68.
Garoushi S, Vallittu PK, Lassila L. Characterization of fluoride releasing restorative dental materials. Dent Mater J. 2018;37(2):293–300. advpub
Mazumdar P, Das A, Das U. Comparative evaluation of microleakage of three different direct restorative materials (silver amalgam, glass ionomer cement, Cention N), in class II restorations using stereomicroscope: an in vitro study. Indian J Dent Res. 2019;30(2):277–81.
Moszner N, et al. Benzoyl germanium derivatives as novel visible light photo initiators for dental materials. Dent Mater. 2008;24(7):901–7.
Todd J. Scientific documentation: Cention N. Schaan, Liechtenstein: Ivoclar-Vivadent Press; 2016. p. 1–58.
Persson A, Lingstrom P, van Dijken JW. Effect of a hydroxyl ion-releasing composite resin on plaque acidogenicity. Caries Res. 2005;39(3):201–6.
Gupta N, et al. Comparison of fluoride ion release and alkalizing potential of a new bulk-fill alkasite. J Conserv Dent. 2019;22(3):296–9.
Rai S, Kumari RA, Meena N. Comparative assessment of fluoride release and recharge through newer fluoride releasing posterior restorative materials: an in vitro study. J Conserv Dent. 2019;22(6):544.
Ruengrungsom C, et al. Evaluation of F, Ca, and P release and microhardness of eleven ion-leaching restorative materials and the recharge efficacy using a new Ca/P containing fluoride varnish. J Dent. 2020;102:103474.
Donly KJ, Liu JA. Dentin and enamel demineralization inhibition at restoration margins of vitremer, Z 100 and Cention N. Am J Dent. 2018;31(3):166–8.
Park C, et al. Surface roughness and microbial adhesion after finishing of Alkasite restorative material. J Korean Acad Pediatr Dent. 2020;47(2):188–95.
Panpisut P, Toneluck A. Monomer conversion, dimensional stability, biaxial flexural strength, and fluoride release of resin-based restorative material containing alkaline fillers. Dent Mater J. 2020;39(4):608–15. advpub
Naz F, et al. Comparative evaluation of mechanical and physical properties of a new bulk-fill alkasite with conventional restorative materials. Saudi Dent J. 2020;33(7):666–73.
Awad MM, et al. Evaluation of the bond strength and cytotoxicity of alkasite restorative material. Appl Sci. 2020;10(18):6175.
Sujith R, et al. Comparative evaluation of mechanical and microleakage properties of Cention-N, composite, and glass ionomer cement restorative materials. J Contemp Dent Pract. 2020;21(6):691–5.
Roulet J-F, et al. In vitro wear of dual-cured bulkfill composites and flowable bulkfill composites. J Esthet Restor Dent. 2020;32(5):512–20.
Naoum S, et al. Fluoride release, recharge and mechanical property stability of various fluoride-containing resin composites. Oper Dent. 2011;36(4):422–32.
Leon-Pineda C, Donly K. Inhibition of demineralization at restoration margins of Z100 and tetric EvoCeram bulk fill in dentin and enamel. Bioengineering. 2019;6(2):36.
Xu H, et al. Novel CaF2 nanocomposite with high strength and fluoride ion release. J Dent Res. 2010;89(7):739–45.
Mitwalli H, et al. Novel CaF2 nanocomposites with antibacterial function and fluoride and calcium ion release to inhibit oral biofilm and protect teeth. J Funct Biomater. 2020;11(3):56.
Bhadila G, et al. Bioactive low-shrinkage-stress nanocomposite suppresses S. mutans biofilm and preserves tooth dentin hardness. Acta Biomater. 2020;114:146–57.
Dieckmann P, et al. Light transmittance and polymerization of bulk-fill composite materials doped with bioactive micro-fillers. Materials (Basel). 2019;12(24):4087.
Balbinot GDS, et al. Niobium containing bioactive glasses as remineralizing filler for adhesive resins. Dent Mater. 2020;36(2):221–8.
Venkatesan J, Kim SK. Chitosan composites for bone tissue engineering—an overview. Mar Drugs. 2010;8(8):2252–66.
Muxika A, et al. Chitosan as a bioactive polymer: processing, properties and applications. Int J Biol Macromol. 2017;105(Pt 2):1358–68.
Demarco FF, et al. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28(1):87–101.
Opdam NJM, et al. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater. 2007;23(1):2–8.
Althaqafi KA, Satterthwaite J, Silikas N. A review and current state of autonomic self-healing microcapsules-based dental resin composites. Dent Mater. 2020;36(3):329–42.
Then S, Neon GS, Abu Kasim NH. Performance of melamine modified urea–formaldehyde microcapsules in a dental host material. J Appl Polym Sci. 2011;122(4):2557–62.
Huyang G, Debertin AE, Sun J. Design and development of self-healing dental composites. Mater Des. 2016;94:295–302.
Blaiszik BJ, et al. Microcapsules filled with reactive solutions for self-healing materials. Polymer. 2009;50(4):990–7.
Bevan C, et al. Subchronic toxicity study of dicyclopentadiene vapor in rats. Toxicol Ind Health. 1992;8(6):353–67.
Ota M, et al. Influence of refractive index on optical parameters of experimental resin composites. Acta Odontol Scand. 2012;70(5):362–7.
Oivanen M, et al. The effect of refractive index of fillers and polymer matrix on translucency and color matching of dental resin composite. Biomater Investig Dent. 2021;8(1):48–53.
Tokuyama. Omnichroma: technical report; 2021. p. 4–9.
Tsubone M, et al. Color shifting at the border of resin composite restorations in human tooth cavity. Dent Mater. 2012;28(8):811–7.
Lee YK. Fluorescence properties of human teeth and dental calculus for clinical applications. J Biomed Opt. 2015;20(4):040901.
Monsénégo G, Burdairon G, Clerjaud B. Fluorescence of dental porcelain. J Prosthet Dent. 1993;69(1):106–13.
Volpato CAM, Pereira MRC, Silva FS. Fluorescence of natural teeth and restorative materials, methods for analysis and quantification: a literature review. J Esthet Restor Dent. 2018;30(5):397–407.
Lee YK, Lu H, Powers JM. Influence of fluorescent and opalescent properties of resin composites on the masking effect. J Biomed Mater Res B Appl Biomater. 2006;76(1):26–32.
Alves LP, et al. Core-shell quantum dots tailor the fluorescence of dental resin composites. J Dent. 2010;38(2):149–52.
O'Brien WJ. Dental materials and their selection. Batavia, IL: Quintessence; 2008.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jum’ah, A.A., Brunton, P.A. (2023). Bulk-Fill Resin Composites: Recent Advances and Future Perspectives. In: Sabbagh, J., McConnell, R. (eds) Bulk Fill Resin Composites in Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-031-16388-3_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-16388-3_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-16387-6
Online ISBN: 978-3-031-16388-3
eBook Packages: MedicineMedicine (R0)