Abstract
Food production influences a population’s dietary habits and vice versa, and both are directly linked to planetary and human health. Currently, the food production system is aimed at high animal production and ultra-processed foods, leading to high pollution, water contamination, and high production of greenhouse gases, thus impairing the environmental equilibrium. Concurrently, high consumption of animal protein and ultra-processed foods is associated with the development of non-communicable diseases, including kidney diseases and worse outcomes. Changes are urgently needed to promote both human and planetary health. In this chapter, we have highlighted the vital role of food intake in kidney health and discussed the future challenges in terms of nutrition, which may involve the use of artificial food and new perspectives for cellular agriculture.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
With estimates of the global population reaching a plateau at nine billion in 2050, a significant increase in food production over the next three decades is imperative. Concurrently, enormous quantities of food must be produced to protect the environment and create resistance to climate change.
In addition, dietary habits are strongly linked to health status. High intake of ultra-processed food (UPF) and processed meat with food termed as “ready-to-go-food” or “fast food” causes damage to both human and planetary health. People are at high risk of developing non-communicable diseases (NCDs), such as type II diabetes mellitus, obesity, hypertension, and kidney diseases, when the intake of unhealthy food is high. An unhealthy diet is closely related to kidney health, and the concept of food as medicine should be used to prevent or mitigate poor health [1]. Thus, the future of food production should also favor people’s access to dietary patterns that improve the overall health and quality of life.
In this chapter, we have discussed some aspects related to dietary patterns, nephrotoxins from the diet, and agricultural production in terms of kidney diseases. We have also discussed the current practices and future trends of food production, especially artificial food, mainly the most studied cultured meat. Finally, we have examined how the future of nutrition and food production can better promote both human and planetary health.
7.2 The Present
7.2.1 Dietary Patterns and Kidney Diseases
In nutritional epidemiology, dietary pattern analysis has emerged as an approach to investigate the relationship between the effects of the overall diet and synergistic effects of nutrients resulting in cumulative effects on health and disease instead of evaluating individual nutrients or foods [2].
From 1960 to 2015, agricultural production was more than tripled, with significant expansion in the use of water, land, and other natural resources. In the same period, there was remarkable industrialization of food, and the consumption of processed, packaged, and prepared food has increased worldwide [3]. Although these technologies have advantages such as increasing shelf life, microbiological safety, and increased access due to lower cost, they negatively impact diet quality.
The Global Burden of Disease Study 2017 reported that unhealthy diets might cause most of the burden of chronic, NCDs, such as hypertension, cardiovascular disease, cancer, diabetes mellitus, and chronic kidney disease (CKD) [4].
Approximately 10% of the world’s population lives with CKD, and its main risk factors are hypertension and diabetes mellitus [5], which are related to unhealthy Western diets [6], characterized by high consumption of UPF, salt, and sugar. This dietary pattern is well known for its pro-inflammatory properties. Several researchers have shown an association between this diet and a decline in renal function [7, 8]. In contrast, healthy dietary patterns, characterized by higher intake of fruit and vegetables, fish, legumes, cereals, whole grains, and fiber and lower intake of red meat, salt, and refined sugars, are associated with nephroprotective outcomes [9, 10]. A meta-analysis including 630,108 adults who were followed up for 10.4 ± 7.4 years has shown that healthy dietary patterns are associated with a lower incidence of CKD [9]. The DASH diet (low intake of red meat, processed food, sodium, and fat and high intake of nuts, fruits, legumes, vegetables, and whole grains) is associated with a low incidence or prevalence of CKD. This association has been shown in prospective studies such as the Atherosclerosis Risk in Communities study [11], Tehran Lipid and Glucose Study [12], and Korean National Health and Nutrition Examination Survey [13]. In addition, a healthy dietary pattern is associated with a lower mortality risk in patients with CKD [14].
Nephrolithiasis or kidney stones is another very prevalent kidney disease. A review of epidemiological data from seven countries found a prevalence rate of 1.7%–14.8%, which seems to be rising [15]. The etiology of kidney stones is multifactorial and involves the interaction of environmental and genetic factors. The current dietary guidelines recommend increasing fluid intake, maintaining a balanced calcium intake, and similar to CKD, reducing dietary intake of sodium and animal proteins and increasing intake of fruits and fiber [16, 17].
Reducing healthy diet intake (food rich in dietary fiber, bioactive compounds, minerals, and vitamins) leads to loss of antioxidants and anti-inflammatory properties of food [1]. In addition, as diet is the primary modulator of the gut microbiota, unhealthy diets promote gut dysbiosis, which has been linked to inflammation and cardiovascular disease in patients with CKD [18, 19].
Taken together, changes in food system production provoked an impaired quality pattern of diets, leading to high consumption of processed food and UPF, including high saturated fats, sugar, salt, additives, and pesticides. In addition to the influence of dietary patterns on kidney health, an unhealthy diet can affect kidney disease.
Food additives are widely used in the food industry to improve safety, shelf-life, taste, texture, and appearance. Here, we have focused on two widely consumed elements present in many processed foods—sodium and phosphate. Excessive sodium and phosphate intake is associated with a high risk of hypertension and kidney diseases. It is also directly and indirectly associated with cardiovascular events [20].
Despite existing dietary guidelines, sodium intake is usually higher than the recommended value (1.5–2.3 g/day) in populations worldwide [21, 22]. In 2010, the average world consumption was 3.95 g Na/day, equivalent to 10 g of salt daily. The world’s largest sodium consumers are in Asia, Eastern Europe, and tropical Latin America, where the daily average exceeds 4 g Na/day. This is exemplified in countries such as China (4.8 g), Thailand (5.3 g), Turkey (4.1 g), and Brazil (4.1 g) [23].
High sodium intake has also been observed in CKD populations [24, 25]. However, there is good evidence supporting the positive effects of decreasing sodium intake on surrogate markers of cardiovascular events (blood pressure) and progression of kidney disease (albuminuria) [26, 27]. Positive effects are also found for kidney stone prevention using dietary approaches that include low sodium intake. This results in a reduced incidence of kidney stones [28] as sodium intake is directly associated with urinary calcium excretion.
In low- and middle-income countries, most of the sodium consumed comes from salt added during cooking or from sauces. In most high-income countries, however, sodium intake can be reduced by a gradual and sustained reduction in the amount of sodium added in processed food since it is the main sodium source of their diet [29]. Therefore, high-income countries that invested in public campaigns to decrease added salt and implemented a gradual and sustained reduction in the amount of salt added to food by the food industry have shown positive results in reducing sodium consumption [29, 30].
Phosphate additives are also present in various food products. However, due to the high consumption of processed food in the last century, there are concerns regarding whether chronic high consumption of phosphate may be toxic and impact kidney health [31].
The recommended dietary allowance (RDA) of phosphate for adults is 700 mg/day [32], which is easily achieved by a varied diet. However, phosphate consumption can exceed this amount by two or more times in individuals and populations who consume a significant quantity of industrialized food items. Estimation of phosphate consumption by dietary recalls is challenging and largely underestimated, especially in population consuming high amounts of processed food. Such estimations are difficult since phosphate content is not available in industrialized food item labels. In addition to increasing the total intake, the bioavailability of inorganic phosphate from additives is higher than that of organic phosphate present in natural sources [17].
High phosphate intake (from red meat and processed food) appears to be associated with kidney damage, although the exact biochemical mechanism has not been fully elucidated [33]. However, it is well documented that high phosphate plasma levels are associated with a higher risk of overall mortality in patients with CKD [34, 35].
7.2.2 Nephrotoxins from Diet and Agricultural Production
Nephrotoxins present in consumed water, food, and the environment may also play a role in kidney diseases. This concern was raised due to the current epidemic of CKD of non-traditional cause (CKDnt) leading to kidney failure mainly in young male agricultural workers without traditional risk factors, mainly in Central America and Asian countries such as Sri Lanka [36, 37].
Although the etiology has not been fully elucidated in any region [38], the research has focused on consumption of contaminated water as the primary risk factor in Asian hotspots. The possible contaminants include heavy metals, glyphosate, and other agrochemicals [39, 40]. However, contamination of food has been poorly investigated. Some studies have found hazardous amounts of lead and cadmium in a typical diet of a region; however, these contaminants were not found in other studies [41,42,43].
In Latin America, heat stress and dehydration are the most frequently studied causative risk factors of kidney disease [44,45,46]. However, a recent longitudinal study conducted in Mexico that assessed kidney functioning of migrant and seasonal farmworkers pre- and post-harvest found a significant decrease in kidney function that was more pronounced in those who worked in the conventional field than in those who worked in the organic field. Thus, the authors suggest that pesticide exposure should be considered in combination with heat stress and dehydration [47].
Cases of acute kidney injury, mainly in Brazil and China, have been linked to Haff disease, a type of human rhabdomyolysis characterized by the sudden onset of unexplained muscular rigidity and an elevated serum creatine kinase level within 24 h after consuming cooked aquatic products [48].
Toxins from tropical plants, such as Djenkol beans [49], star fruit (Averrhoa carambola) [50], poisonous mushrooms (Amanita phalloides) [51], and cotton seed oil (gossypol), can also cause acute kidney injury [52].
7.3 The Future
7.3.1 Food Production and Introduction of Artificial Food
Food systems can nurture human health and support environmental sustainability; however, they are currently causing adverse effects. It has been estimated that more than 820 million people have insufficient food and many more consume low-quality diets that cause micronutrient deficiencies and contribute substantially to diet-related NCDs [53]. The currently expanding food production and economic growth have resulted in a huge economic burden on the natural environment. “Almost one-half of the forests that once covered the Earth are now gone. Groundwater sources are being depleted rapidly. Biodiversity has been deeply eroded. Every year, the burning of fossil fuels emits billion of tons of greenhouse gases into the atmosphere, which are responsible for global warming and climate change” [3].
The world’s growing population and increasing human welfare will necessitate a 30%–70% increase in food production over the next three decades. Concurrently, large quantities of food must be produced to protect the environment and create resistance to climate change. However, it is unclear whether we can sustainably feed a global population of 11 billion in 2100. This question has been extensively explored in FAO’s report—The future of food and agriculture: Trends and challenges, 2017. The consensus view is that current systems are likely capable of producing enough food, but to do so in an inclusive and sustainable manner will require major transformations involving international agencies, local governments, scientists, agricultural and food industries, consumers, and others [3].
The food industry successfully introduced different artificial foods and ingredients in the last century to substitute natural sources, including sweeteners, colorings, and flavorings. Foods from non-meat sources (soybeans or wheat), such as seitans and tofu, have existed for many centuries, whereas cellular agriculture has been introduced in the last decade. Artificial meat production may be a more sustainable alternative for producing high-protein sources using technologies such as genetic modification and cloning. Although in vitro meat culturing techniques have been explored, they are presently under discussion.
Approximately 70% of all agricultural land is used for livestock production, and artificial meat products may help reduce greenhouse gas emissions compared to conventional meat production [54]. The other benefits include those regarding animal welfare issues, food safety, public health, and the need to face the increasing worldwide population and associated protein demand [53]. In 2020, this novel product was approved for sale in Singapore, and only the future will tell whether it will meet complex consumer demands [55].
The National Aeronautics and Space Administration designed artificial meat from myoblasts in suspension culture in 2002. In 2014, Dr. Mark Post developed cultured meat [56], and Maastricht University produced the first cultured beef burger. Cellular agriculture is also linked to the production of starch and cellulose, such as amylose and amylopectin, hyaluronic acid, chitosan, soy protein, and bread-derived scaffolds [57].
Studies have shown how to construct steak-like meat using several sources of bovine cells such as adipose-derived stem cells, pluripotent stem cells, and satellite and muscle stem cells. With cell fiber synthesis from tendon-gel-integrated bioprinting, a bioreactor is used to increase cell number [58, 59]. The popularization of this meat produced in vitro, also called cultured meat or clean meat, is growing rapidly; however, the cost of production is still high. Another problem is the low acceptance of cultured meat. A systematic review (including 91 articles on consumer acceptance of different sources of proteins) showed that in addition to uptake of insects, the acceptance of cultured meat is also low [60]. Negative acceptance is related to neophobia [61].
According to Djisalov et al. (2021), cultured meat is also beneficial because there is no treatment with hormones or antibiotics. In addition, it reduces food-borne illnesses and diseases such as avian and swine influenza [62]. In addition, the composition and flavor can be modulated by controlling fat, mineral, and vitamin content and can be customized according to different nutritional requirements [57, 63]. Another interesting point is that “designer meat” can be produced using nanotechnology-based methods to improve the nutritional value, flavor, and bioavailability of nutrients [64].
The organoleptic properties and regulations regarding production, labeling, and marketing deserve more discussion. Furthermore, more studies on the risks regarding food safety, ethical perspectives, and health are needed. The nutritional equivalence between traditional and cultured meat is debatable. However, the next step in food production involves artificial food production, and studies showing the pros and cons of their use are needed urgently.
It is important to note that many biochemical metabolisms, such as conversion of glycogen to lactate in the post-mortem of the anima and muscle contraction by actin and myosin using calcium, do not exist in cultured meat. More research is needed to determine whether these differences interfere with the nutritional composition of cultured meat [64].
Regarding nutritional composition, protein is the most important nutrient in red meat and cultured meat is made with the best protein source, such as muscle cells or cytoskeletal proteins [63].
Concerning the dietary protein recommendation for patients with CKD, it is important to recommend a low protein diet to patients with CKD on pre-dialysis treatment [17]. Cultured meat is a good source of protein, and therefore, studies evaluating the effects of cultured meat on these patients need to be conducted.
7.3.2 Future of Nutrition for Kidney Health
Healthy dietary patterns, usually characterized by higher intake of vegetables, fruits, legumes, nuts, whole grains, fish, and low-fat dairy and lower intake of red and processed meats, sodium, and sugar, have been associated with CKD prevention, progression, and mortality [9, 14, 65]. Healthy dietary patterns reduce the risk of albuminuria and CKD [9]. Thus, based on current knowledge, nutrition experts recommend a plant-dominant low-protein diet for conservative management of CKD [66]. The best scenario seems to be the one that promotes and supports universal access to a healthy dietary pattern based on organic foods, more fruits and vegetables, and less red meat and processed foods. In addition, personalized nutrition is a promising approach at an individual level, which manages and integrates heterogeneous and patient-specific molecular, clinical, and anamnestic data to achieve individual well-being [67].
High red meat intake is linked to many cardiovascular diseases, cancer, and kidney diseases, in addition to high greenhouse gas emissions. Therefore, reducing its consumption is urgently required. Cultured meat intake could reduce the risk of these chronic diseases and reduce food-borne illness and nutrition deficiency, thus making it a promising candidate for a sustainable diet [68]. Artificial food can reduce significantly greenhouse gas emissions, water use, and energy consumption [69]. However, controlling nutritional composition is very important and is unclear, mainly regarding micronutrients such as vitamin B12 and iron. Another discussion is regarding cell multiplications as some dysregulation can occur and lead to adverse effects on human health [70, 71].
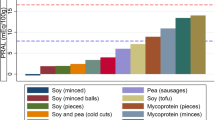
Overall, this chapter reinforced the findings of previous studies that an unhealthy diet is harmful to human and planetary health and included the negative consequences for patients with kidney diseases. Therefore, these changes should be urgently proposed and implemented. This chapter discussed the introduction of artificial food, cellular agriculture, and cultured food as an alternative strategy to replace the unhealthy diet (Fig. 7.1).
Future of nutrition for kidney health. The food production system and high red meat and ultra-processed food intake lead to alteration in the environment equilibrium and increased risk of non-communicable diseases, including kidney diseases. Therefore, discussions and actions for the future of nutrition are urgently necessary. (Image created with Biorender)
In terms of technical issues, methods to increase the production of cultured food are being optimized, but industrial-scale production is not yet possible. However, this research is in the infancy stage in the health field, and many gaps in knowledge exist. These gaps cannot be resolved if there are adverse effects on human health, and no study has been performed in patients with kidney diseases. In addition, it is unclear whether cultured meat will be a food option in the future, and whether this food is good for human health.
For many people, cultured meat is still science fiction, and it can also be seen as an unnatural food. Finally, considering that unhealthy food consumption needs to change urgently in patients with kidney diseases, we need more educational programs to encourage healthy and sustainable diet consumption.
References
Mafra D, Borges NA, Lindholm B, et al. Food as medicine: targeting the uraemic phenotype in chronic kidney disease. Nat Rev Nephrol. 2021;17:153–71. https://doi.org/10.1038/s41581-020-00345-8.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9. https://doi.org/10.1097/00041433-200202000-00002.
FAO. The future of food and agriculture: trends and challenges. Rome: FAO; 2017.
Afshin A, Sur PJ, Fay KA, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2019;393:1958–72. https://doi.org/10.1016/S0140-6736(19)30041-8.
Bello AK, Levin A, Lunney M, Osman MA, Ye F, Ashuntantang GB-FE, Benghanem Gharbi M, Ghnaimat M, Harden P, Jha V, Kalantar-Zadeh KKR, Kerr P, Ossareh S, Perl J, Rondeau E, Solá L, Tesar V, Tchokhonelidze ITK, et al. Global kidney health atlas: a report by the International Society of Nephrology on the global burden of end-stage kidney disease and capacity for kidney replacement therapy and conservative care across world countries and regions. Brussels, Belgium; 2019.
Medina-Remón A, Kirwan R, Lamuela-Raventós RM, Estruch R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit Rev Food Sci Nutr. 2018;58:262–96. https://doi.org/10.1080/10408398.2016.1158690.
Martínez Leo EE, Peñafiel AM, Hernández Escalante VM, Cabrera Araujo ZM. Ultra-processed diet, systemic oxidative stress, and breach of immunologic tolerance. Nutrition. 2021;91–92:111419. https://doi.org/10.1016/j.nut.2021.111419.
Rey-García J, Donat-Vargas C, Sandoval-Insausti H, et al. Ultra-processed food consumption is associated with renal function decline in older adults: a prospective cohort study. Nutrients. 2021;13:1–13. https://doi.org/10.3390/nu13020428.
Bach KE, Kelly JT, Palmer SC, et al. Healthy dietary patterns and incidence of CKD. Clin J Am Soc Nephrol. 2019;14:1441–9. https://doi.org/10.2215/CJN.00530119.
Quintela BCSF, Carioca AAF, de Oliveira JGR, et al. Dietary patterns and chronic kidney disease outcomes: a systematic review. Nephrol Ther. 2021;26:603–12. https://doi.org/10.1111/nep.13883.
Rebholz CM, Crews DC, Grams ME, et al. DASH (dietary approaches to stop hypertension) diet and risk of subsequent kidney disease. Am J Kidney Dis. 2016;68:853–61. https://doi.org/10.1053/j.ajkd.2016.05.019.
Asghari G, Yuzbashian E, Mirmiran P, Azizi F. The association between dietary approaches to stop hypertension and incidence of chronic kidney disease in adults: the Tehran lipid and glucose study. Nephrol Dial Transplant. 2017;32:ii224–30. https://doi.org/10.1093/ndt/gfw273.
Lee HS, Lee KB, Hyun YY, et al. DASH dietary pattern and chronic kidney disease in elderly Korean adults. Eur J Clin Nutr. 2017;71:755–61. https://doi.org/10.1038/ejcn.2016.240.
Kelly JT, Palmer SC, Wai SN, et al. Healthy dietary patterns and risk of mortality and ESRD in CKD: a meta-analysis of cohort studies. Clin J Am Soc Nephrol. 2017;12:272–9. https://doi.org/10.2215/CJN.06190616.
Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. 2010;12:e86–96.
Skolarikos A, Straub M, Knoll T, et al. Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. Eur Urol. 2015;67:750–63. https://doi.org/10.1016/j.eururo.2014.10.029.
Ikizler TA, Burrowes JD, Byham-Gray LD, et al. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am J Kidney Dis. 2020;76:S1–S107. https://doi.org/10.1053/j.ajkd.2020.05.006.
Mafra D, Borges N, Alvarenga L, et al. Dietary components that may influence the disturbed gut microbiota in chronic kidney disease. Nutrients. 2019;11:496. https://doi.org/10.3390/nu11030496.
Snelson M, Tan SM, Clarke RE, et al. Processed foods drive intestinal barrier permeability and microvascular diseases. Sci Adv. 2021;7:eabe:4841. https://doi.org/10.1126/sciadv.abe4841.
He FJ, Mac Gregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52:363–82. https://doi.org/10.1016/j.pcad.2009.12.006.
World Health Organization. Sodium intake for adults and children. Geneva: World Health Organization; 2012. p. 56.
Stallings VA, Harrison M, Oria M. Dietary reference intakes for sodium and potassium. Washington, DC: The National Academies Press; 2019.
Powles J, Fahimi S, Micha R, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733. https://doi.org/10.1136/bmjopen-2013-003733.
Nerbass FB, Pecoits-Filho R, McIntyre NJ, et al. High sodium intake is associated with important risk factors in a large cohort of chronic kidney disease patients. Eur J Clin Nutr. 2014;69:786–90. https://doi.org/10.1038/ejcn.2014.215.
De Vico RB, Baggio Nerbass F, Chaud Hallvass AE, et al. Development and validation of equations to estimate 24 h urinary sodium excretion from urine samples of patients with chronic kidney disease. Nephron. 2019;143:255–63. https://doi.org/10.1159/000502013.
Nerbass FB, Calice-Silva V, Pecoits-Filho R. Sodium intake and blood pressure in patients with chronic kidney disease: a salty relationship. Blood Purif. 2018;901:166–72. https://doi.org/10.1159/000485154.
McMahon EJ, Campbell KL, Bauer JD, Mudge DW. Altered dietary salt intake for people with chronic kidney disease. Cochrane Database Syst Rev. 2015;2:CD010070. https://doi.org/10.1002/14651858.CD010070.pub2.
Taylor EN, Fung TT, Curhan GC. DASH-style diet associates with reduced risk for kidney stones. J Am Soc Nephrol. 2009;20:2253–9. https://doi.org/10.1681/ASN.2009030276.
He FJ, Mac Gregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–84. https://doi.org/10.1038/jhh.2008.144.
Millett C, Laverty AA, Stylianou N, et al. Impacts of a national strategy to reduce population salt intake in England: serial cross sectional study. PLoS One. 2012;7:e29836. https://doi.org/10.1371/journal.pone.0029836.
Rubio-Aliaga I. Phosphate and kidney healthy aging. Kidney Blood Press Res. 2020;45:802–11. https://doi.org/10.1159/000509831.
Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academies Press; 2007.
Duayer IF, Duque EJ, Fujihara CK, et al. The protein-independent role of phosphate in the progression of chronic kidney disease. Toxins. 2021;13:503. https://doi.org/10.3390/toxins13070503.
Eddington H, Hoefield R, Sinha S, et al. Serum phosphate and mortality in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:2251–7. https://doi.org/10.2215/CJN.00810110.
Kestenbaum B, Sampson JN, Rudser KD, et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol. 2005;16:520–8. https://doi.org/10.1681/ASN.2004070602.
Lanerolle RD, Nanayakkara S, Sheriffdeen AH, Sheriff R. Demographic characteristics of end stage renal disease in Sri Lanka. J Ceylon Coll Physicians. 2000;33:124–6.
Trabanino RG, Aguilar R, Silva CR, et al. End-stage renal disease among patients in a referral hospital in El Salvador. Rev Panam Salud Publica. 2002;12:202–6.
Redmon JH, Levine KE, Lebov J, et al. A comparative review: chronic kidney disease of unknown etiology (CKDu) research conducted in Latin America versus Asia. Environ Res. 2021;192:110270. https://doi.org/10.1016/j.envres.2020.110270.
Kulathunga MRDL, Ayanka Wijayawardena MA, Naidu R, Wijeratne AW. Chronic kidney disease of unknown aetiology in Sri Lanka and the exposure to environmental chemicals: a review of literature. Environ Geochem Health. 2019;41:2329–38. https://doi.org/10.1007/s10653-019-00264-z.
Gunarathna S, Gunawardana B, Jayaweera M, et al. Glyphosate and AMPA of agricultural soil, surface water, groundwater and sediments in areas prevalent with chronic kidney disease of unknown etiology, Sri Lanka. J Environ Sci Health Pt B. 2018;53:729–37. https://doi.org/10.1080/03601234.2018.1480157.
Ananda Jayalal TB, Jayaruwan Bandara TWMA, Mahawithanage STC, et al. A quantitative analysis of chronic exposure of selected heavy metals in a model diet in a CKD hotspot in Sri Lanka. BMC Nephrol. 2019;20:1–14. https://doi.org/10.1186/s12882-019-1371-5.
S Herath HMA, Kawakami T, Nagasawa S, et al. Arsenic, cadmium, lead, and chromium in well water, rice, and human urine in Sri Lanka in relation to chronic kidney disease of unknown etiology. J Water Health. 2018;16:212–22. https://doi.org/10.2166/wh.2018.070.
Levine KE, Redmon JH, Elledge MF, et al. Quest to identify geochemical risk factors associated with chronic kidney disease of unknown etiology (CKDu) in an endemic region of Sri Lanka—a multimedia laboratory analysis of biological, food, and environmental samples. Environ Monit Assess. 2016;188:548. https://doi.org/10.1007/s10661-016-5524-8.
Wesseling C, Aragón A, González M, et al. Heat stress, hydration and uric acid: a cross-sectional study in workers of three occupations in a hotspot of mesoamerican nephropathy in Nicaragua. BMJ Open. 2016;6:e011034. https://doi.org/10.1136/bmjopen-2016-011034.
Glaser J, Lemery J, Rajagopalan B, et al. Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. 2016;11:1472–83. https://doi.org/10.2215/CJN.13841215.
Laws RL, Brooks DR, Amador JJ, et al. Changes in kidney function among nicaraguan sugarcane workers. Int J Occup Environ Health. 2015;21(3):241–50. https://doi.org/10.1179/2049396714Y.0000000102.
López-Gálvez N, Wagoner R, Canales RA, et al. Longitudinal assessment of kidney function in migrant farm workers. Environ Res. 2021;202:111686. https://doi.org/10.1016/j.envres.2021.111686.
PEI P, LI XY, LU SS, et al. The emergence, epidemiology, and etiology of haff disease. Biomed Environ Sci. 2019;32:769–78. https://doi.org/10.3967/bes2019.096.
Reimann HA, Sukaton RU. Djenkol bean poinsoning (DJENKOLISM): a cause of hematuria and anuria. Am J Med Sci. 1956;232:172–4. https://doi.org/10.1097/00000441-195608000-00006.
Lee K-G. Star fruit intoxication with acute kidney injury. Clin Med. 2012;12:494.1–94. https://doi.org/10.7861/clinmedicine.12-5-494.
McClain JL, Hause DW, Clark MA. Amanita phalloides mushroom poisoning: a cluster of four fatalities. J Forensic Sci. 1989;34:83–7.
Gao H, Yang ZS, Jin SX. Primary observations on distal renal tubule acidosis in 177 cases caused by gossypol intoxication. Zhonghua Nei Ke Za Zhi. 1985;24:419–21, 447.
Willett W, Rockström J, Loken B, et al. The lancet commissions food in the Anthropocene: the EAT–lancet commission on healthy diets from sustainable food systems. Lancet. 2019;393(10191):2590. https://doi.org/10.1016/S0140-6736(18)31788-4.
Bonny SPF, Gardner GE, Pethick DW, Hocquette J. What is artificial meat and what does it mean for the future of the meat industry? J Integr Agric. 2015;14:255–63. https://doi.org/10.1016/S2095-3119(14)60888-1.
Liu J, Hocquette É, Ellies-Oury MP, Chriki S, Hocquette JF. Chinese consumers’ attitudes and potential acceptance toward artificial meat. Foods. 2021;10(2):353. https://doi.org/10.3390/foods10020353.
Choudhury D, Singh S, Seah JSH, et al. Commercialization of plant-based meat alternatives. Trends Plant Sci. 2020;25:1055–8. https://doi.org/10.1016/j.tplants.2020.08.006.
Djisalov M, Knežić T, Podunavac I, et al. Cultivating multidisciplinarity: manufacturing and sensing challenges in cultured meat production. Biology (Basel). 2021;10:204. https://doi.org/10.3390/biology10030204.
Kang D-H, Louis F, Liu H, et al. Engineered whole cut meat-like tissue by the assembly of cell fibers using tendon-gel integrated bioprinting. Nat Commun. 2021;12:5059. https://doi.org/10.1038/s41467-021-25236-9.
Park S, Jung S, Heo J, et al. Chitosan/cellulose-based porous nanofilm delivering c-phycocyanin: a novel platform for the production of cost-effective cultured meat. ACS Appl Mater Interfaces. 2021;13:32193–204. https://doi.org/10.1021/acsami.1c07385.
Onwezen MC, Bouwman EP, Reinders MJ, Dagevos H. A systematic review on consumer acceptance of alternative proteins: pulses, algae, insects, plant-based meat alternatives, and cultured meat. Appetite. 2021;159:105058. https://doi.org/10.1016/j.appet.2020.105058.
Wilks M, Phillips CJC, Fielding K, Hornsey MJ. Testing potential psychological predictors of attitudes towards cultured meat. Appetite. 2019;136:137–45. https://doi.org/10.1016/j.appet.2019.01.027.
Mavaro I, De Felice E, Palladino A, et al. Anatomical templates for tissue (re)generation and beyond. Biotechnol Bioeng. 2020;117:3938–51. https://doi.org/10.1002/bit.27533.
Balasubramanian B, Liu W, Pushparaj K, Park S. The epic of in vitro meat production—a fiction into reality. Foods. 2021;10:1395. https://doi.org/10.3390/foods10061395.
Abinash V, Rahul T, Antoniraj MG, Moses JA, Anandharamakrishnan C. Food, medical, and environmental applications of polysaccharides. In: Nanotechnology approaches for food fortification. Amsterdam: Elsevier; 2021. p. 161–86.
Cai Q, Dekker LH, Vinke PC, et al. Diet quality and incident chronic kidney disease in the general population: the lifelines cohort study. Clin Nutr. 2021;40(9):5099–105. https://doi.org/10.1016/j.clnu.2021.07.033.
Kalantar-Zadeh K, Joshi S, Schlueter R, et al. Plant-dominant low-protein diet for conservative management of chronic kidney disease. Nutrients. 2020;12:1931. https://doi.org/10.3390/nu12071931.
Simmons LA, Dinan MA, Robinson TJ, Snyderman R. Personalized medicine is more than genomic medicine: confusion over terminology impedes progress towards personalized healthcare. Pers Med. 2012;9:85–91. https://doi.org/10.2217/pme.11.86.
Rubio NR, Xiang N, Kaplan DL. Plant-based and cell-based approaches to meat production. Nat Commun. 2020;11:6276. https://doi.org/10.1038/s41467-020-20061-y.
Tuomisto HL, Teixeira de Mattos MJ. Environmental impacts of cultured meat production. Environ Sci Technol. 2011;45:6117–23. https://doi.org/10.1021/es200130u.
Chriki S, Hocquette J-F. The myth of cultured meat: a review. Front Nutr. 2020;7:7. https://doi.org/10.3389/fnut.2020.00007.
Hocquette J-F. Is in vitro meat the solution for the future? Meat Sci. 2016;120:167–76. https://doi.org/10.1016/j.meatsci.2016.04.036.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Nerbass, F.B., Mafra, D. (2022). Artificial Food and the Future of Nutrition for Kidney Health. In: Bezerra da Silva Junior, G., Nangaku, M. (eds) Innovations in Nephrology. Springer, Cham. https://doi.org/10.1007/978-3-031-11570-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-11570-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-11569-1
Online ISBN: 978-3-031-11570-7
eBook Packages: MedicineMedicine (R0)