Abstract
This chapter covers the role of interventional radiology, high intensity focused ultrasound, and other modalities that may enhance success of primary management of placenta accreta spectrum.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
In this chapter, we provide an overview about therapies that may offer benefit in conjunction with cesarean hysterectomy, which is the most common and definitive treatment of the placenta accreta spectrum (PAS). We also discuss techniques used as adjunctive therapies with conservative and uterine sparing management, which may be applied perioperatively. Specifically, we discuss the interventional modalities that focus on preventing maternal hemorrhage. This includes vascular embolization, prophylactic arterial balloon occlusion, and use of the antifibrinolytic agent tranexamic acid. We also briefly discuss the controversy surrounding methotrexate and why its use is not recommended, and the investigational technique of high-intensity focused ultrasound (HIFU).
Surgical Control of Bleeding
There are several different techniques that have been described for bleeding control in cases of PAS which include intra-arterial embolization, intra-arterial balloon occlusion, arterial ligation, intrauterine tamponade, and the use of uterine compression sutures.
Uterine Artery Embolization
Uterine artery embolization (UAE) is a procedure most commonly used to treat symptomatic fibroids [1]. Other indications include postpartum hemorrhage, inoperable gynecologic tumors, and occlusion of uterine vascular malformations [2]. The procedure is contraindicated in the setting of suspected gynecologic malignancies, ongoing gynecologic infection, and ongoing pregnancy [3]. In the case of life-threatening hemorrhage, UAE may be performed regardless of the clinical scenario, when the benefits outweigh the risks [4]. The procedure is performed by interventional radiologists. The embolic materials most commonly used for uterine or vaginal hemorrhage are Gelfoam slurry, pledgets, coils, or n-butyl-2-cyanoacrylate, whereas particles such as tris-acryl gelatin microspheres or polyvinyl alcohol are used for embolization of fibroids. The procedure is performed by first gaining vascular access via the common femoral or the radial artery, and passing a guidewire to the intended target. Angiogram is performed to map the arterial tree and to locate the uterine arteries. The ipsilateral anterior oblique view allows for optimal visualization of the uterine artery. A 4- or 5-Fr catheter or a larger lumen microcatheter is placed at the transverse portion of the uterine artery, distal to the cervicovaginal branches, to prevent unintentional embolization of other arteries [5]. The goal of treatment is to slow blood flow within the uterine artery and thus decrease uterine perfusion pressure, rather than to cause complete occlusion of the artery. The most common complications of uterine artery embolization are amenorrhea and persistent vaginal discharge [6]. However, given the indication for UAE in the case of PAS, when hysterectomy is planned and performed, these complications become less significant.
Arterial embolization as a treatment for postpartum hemorrhage in cases of PAS is supported by evidence-based data [7]. It can be used as an adjunctive therapy with conservative management or with hysterectomy. In a systematic review of 177 pregnant patients who had pelvic arterial embolization in the setting of conservative management, secondary hysterectomy was avoided in 90% of patients [8]. It has been available as a highly successful treatment modality for postpartum hemorrhage for years [7]. However, arterial embolization for PAS differs significantly from cases of postpartum hemorrhage due to uterine atony. The chaotic periuterine hypervascularization between the bladder and lower uterine segment in PAS is predominantly venous in nature; therefore, arterial embolization does not directly occlude these vessels. Additionally, periuterine fibrosis makes surgical dissection challenging, no matter where the vessels are located. Bugling placental tissue may increase the difficulty in mapping or easily accessing target arteries. Other arteries that may be involved in the uteroplacental vasculature are the ovarian, pudendal, obturator, sacral, and inferior epigastric arteries. Embolizing these aberrant vessels could inadvertently cause ischemic events in organs such as the bladder or bowel [9].
Most reports focus on using arterial embolization in conjunction with conservative management. In one retrospective study, median estimated blood loss (EBL), transfusion requirements, and length of intensive care unit (ICU) stay were compared between a UAE group that underwent UAE following delivery and prior to hysterectomy and a control group who received only cesarean hysterectomy. There was a significant difference in EBL (P = 0.04), 1500 (range 500–2000) vs 2000 (range 1000–4500), respectively. There was not a significant difference in length of ICU stay or transfusion requirements. In a subgroup analysis, women with placenta increta had a significant decrease in length of ICU stay (P = 0.04) and transfusion requirements (P = 0.009). Thus, the authors concluded that for placenta increta, UAE following cesarean delivery and prior to hysterectomy appears to be safe and effective in decreasing blood loss, transfusion requirements, and length of ICU stay compared with cesarean hysterectomy alone [10]. Other studies have described UAE prior to cesarean delivery; however, this poses the risks of exposing the fetus to radiation, and decreasing oxygen supply to the fetus, causing the surgeons to rush in attempts to decrease time from embolization to delivery [11, 12].
Internal Iliac Artery Ligation
Direct ligation of the internal iliac artery has been described, specifically several retrospective studies studying outcomes in women who had this procedure performed at the time of delivery. However, in one study, with the strength of having a comparative group (patients who did not undergo internal iliac artery ligation), the authors’ conclusion could not corroborate a reduction in blood loss. In this study, patients with PAS who did and did not receive intraoperative internal iliac artery ligation were analyzed for blood loss and length of hospitalization. Among 23 cases, there was neither a significant difference in blood loss nor length of hospital stay [13]. Notably, patients who did not have cesarean hysterectomy for management were excluded from this study. A subsequent randomized controlled trial confirmed the lack of difference of estimated intraoperative blood loss in patients with PAS who underwent cesarean hysterectomy between groups who had internal iliac artery ligation and those who did not. Additionally, the group who underwent internal iliac artery ligation had significantly longer operative time [14].
Although internal iliac artery ligation is conventionally accepted as an effective means to control blood loss intraoperatively, with studies showing up to 49% reduction in pelvic blood flow and 85% reduction in pulse pressure, cesarean hysterectomy in the context of PAS presents additional challenges [13, 15]. The time needed to achieve adequate hemostasis, presence of collateral vessels, and excess blood flow from other vessels (external iliac, inferior epigastric, inferior mesenteric arteries) and potential occlusion of the operative field by lateral placental extension are all contributory factors [13]. Additionally, experience in identification of the internal iliac artery and appropriate ligation is necessary to avoid ligation and occlusion of more proximal vessels.
Endovascular Balloon Occlusion of the Pelvic Circulation
Endovascular balloon occlusion of the pelvic circulation is another strategy that has been increasingly attempted as an adjunct intraoperative strategy [7]. The procedure can be done in several ways, including occlusion of the internal iliac arteries (PBOIIA), common iliac arteries (PBOCIA), abdominal aorta (PBOAA), and uterine arteries (PBOUA). It can be performed in conjunction with or in lieu of UAE. Of these, aortic balloon occlusion has been shown to be associated most consistently with the reduced blood loss. Conversely, balloon occlusion of the internal iliac and common iliac arteries has been shown to result in higher lower-limb complications such as claudication and thrombosis [16].
One systematic review found a statistically significant difference in blood loss for cesarean section and cesarean hysterectomy in pregnancies complicated by PAS (−310 mL, P = 0.020) with use of PBOIIA compared to no endovascular intervention [16]. Additionally, the authors found reduced amount of packed red blood cells transfused in all patients who underwent endovascular occlusion compared to those who did not during delivery (−1.54 units of packed red blood cells, P = 0.001). Operative time and length of hospital stay were not significantly different. There were, however, significant complications that arose from endovascular balloon occlusion including bladder injury, ureteral injury, disseminated intravascular coagulopathy (DIC), vesicovaginal and vesicouterine fistula formation, rebleeding requiring further intervention, lower limb claudication, arterial thrombosis, balloon rupture, access vessel pseudoaneurysm, and groin hematoma [16]. Based on this systematic review and another small randomized controlled trial, the International Society for Placenta Accreta Spectrum (IS-PAS) does not recommend routine use of prophylactic pelvic arterial balloon catheters (Grade B recommendation) [7].
Uterine Compression Sutures
Uterine compression sutures include methods such as B-Lynch, Hayman, Pereira, Cho, and other techniques [17,18,19,20,21]. Several studies have reported the use of compression sutures in conjunction with uterine artery ligation, intrauterine balloon tamponade, and focal resection for uterine preservation in PAS cases [22,23,24,25,26,27,28]. In a large case series, 26 women had bilateral uterine artery ligation performed, followed by placement of a B-Lynch suture—compression achieved by suturing the anterior and posterior uterine walls together [23]. B-Lynch suture is well described as a treatment for uterine atony. The ligation was first performed with a simple stitch, using 1.0 chromic suture. B-Lynch was then performed, followed by double-layer closure of the hysterotomy. Although this technique was effective in preserving fertility in cases of atony and bleeding from placental remnants, the limitations and drawbacks were noted. Placenta accreta spectrum and DIC were proposed as reasons for failure of the B-Lynch procedure. Although bleeding from atony was well controlled by the B-Lynch suture, there likely needs to be additional steps to control bleeding from the placental bed [23]. It is difficult to comment about the use compression sutures independently, as it was used in conjunction with arterial ligation or other measures in most of the studies described above.
Use of Tranexamic Acid
The WOMAN trial was a large, multicenter, double-blinded, placebo-controlled randomized controlled trial that compared tranexamic acid (TXA) to placebo to prevent death from all causes of peripartum bleeding [29]. 20,021 gravidae were included in the primary analysis, and there were 483 maternal deaths, in which 72% of these deaths were attributed to bleeding. The study concluded that the risk ratio due to bleeding for patients who received 1 gram of TXA within 3 h of delivery was 0.78 (P = 0.03). In the WOMAN trial, if bleeding continued after 30 min of first administration of TXA or stopped and restarted within 24 h, 1 gram of TXA was re-dosed [29]. The risk reduction with regard to all causes of mortality was not statistically significant. Importantly, the risk of thromboembolic events did not differ between the groups, nor did the rate of sepsis [29]. The CRASH-2 trial, a study of trauma patients, came to the same conclusion; however, this study demonstrated reduction in all-cause mortality [30]. While neither of these studies was specific to treatment of the PAS, given that PAS results in increased blood loss compared to cesarean or vaginal delivery absent PAS, and that massive transfusion is often required, it is plausible that early administration of TXA is reasonable when anticipating massive transfusion. One international PAS database study analyzed factors associated with severe postpartum hemorrhage defined as either estimated blood loss >3500 mL or ≥ 5500 mL (the 75th and 95th percentiles for the cohort). Neither prophylactic nor therapeutic tranexamic acid use correlated with a difference in blood loss; however, the authors concluded that the lack of difference with therapeutic use was due to the indication for ongoing bleeding rather than lack of efficacy [31]. This relatively inexpensive, low-risk intervention still may be considered in patients with PAS and future, well-designed trials are needed [7].
With regard to uterotonic agents and procoagulant agents, there is not enough data validating their use directly related to PAS. Therefore, IS-PAS recommends using uterotonic agents in compliance with local policies. Hemostatic agents and procoagulant agents should be used at the discretion of the surgeon (class D evidence) [7].
Investigational Therapies
High-Intensity Focused Ultrasound
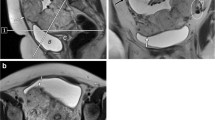
High-intensity focused ultrasound (HIFU) is another modality that has been proposed for the management of PAS. HIFU is a noninvasive treatment that results in thermal damage directly to a targeted area without an effect on the surrounding tissue. It has been used historically in the management of solid tumors [32] and more recently has been used for treatment of uterine leiomyomas, cesarean scar pregnancies, and adenomyosis [33, 34]. A recently published systematic review of four articles highlighted its potential application to PAS as an adjunct to conservative management [35].
One study included patients who had vaginal deliveries with retained PAS only [36], whereas the three remaining studies included patients who had either cesarean delivery or vaginal delivery [37,38,39]. The studies had strict inclusion criteria, which included exclusion of patients with active postpartum hemorrhage, extensive abdominal scarring, and genital infection. Additionally, all studies included combined treatment with uterine curettage or hysteroscopic resection, and methotrexate in selected cases. For the one study in which only vaginal deliveries were included, inclusion criteria included patients with (1) stable vital signs without active bleeding or infection, (2) normal liver and renal function, (3) hemoglobin greater than 7, (4) residual placenta area greater than or equal to 3 cm by 3 cm but covering less than half the uterine cavity, (5) desire to preserve fertility and breastfeed, (6) declining surgery and chemical therapy, and (7) no prior conservative approach before HIFU therapy [36]. Generally, the procedure is safe, with a low incidence of complications (less than 1%), and highly effective for women who strongly desire uterine preservation. However, the limitations of this procedure are noticeable.
In all included studies, a HIFU system was used for the procedure. This included an ultrasound transducer with a generator (to produce the therapeutic energy), a diagnostic ultrasound imaging device, a movement system controlled by a computer to drive the transducer, a specialized treatment bed, and a degassed water circulation unit. The procedure was performed with the patient lying in the prone position, allowing the lower abdomen to be in contact with degassed water. The location, size, and shape of the residual placenta, along with adjacent organs, were then mapped out with assistance of the ultrasound-based computer system. The residual placental tissue was divided into slices of 5 mm in width, and each slice was ablated in 5-second bursts, from deepest to most superficial point of infiltration. Ultrasound scans were performed before and after the treatment, to ensure that the target area was captured [36].
The number of patients with PAS who may be eligible for HIFU is severely limited by the requisite strict selection criteria—patients with PAS may have significant adhesive disease, and are at greater risk for significant hemorrhage, and definitive management should not be delayed. Patients who are hemodynamically stable with active bleeding are generally eligible for endovascular occlusion procedures; however, this is not the case for HIFU. There is a need for more evidence-based data to further understand the role of HIFU in PAS prior to widespread adoption.
Methotrexate
Methotrexate therapy has been suggested as an adjuvant therapy for the conservative management of placenta accreta spectrum and is highly controversial [40]. In a systematic review which studied conservative management strategies, there were 17 patients who received methotrexate. Six percent of these patients required a delayed hysterectomy despite treatment. There were no deaths reported in the methotrexate group in this study [41]; however, the route of administration of methotrexate was not specified. In a retrospective study performed in China, 54 women with confirmed placenta increta who desired conservative management received either systemic methotrexate intravenously or local multipoint injection under ultrasound guidance. The treatment was considered successful if hysterectomy was avoided. In the systemic group, which included 21 patients, 4 underwent hysterectomy for uncontrollable postpartum hemorrhage and infection. In the local administration group, which included 33 patients, 8 patients needed dilation and curettage as placenta was not delivered spontaneously. However, there were no instances of hysterectomy in this subgroup. There were no maternal deaths in the study [42]. In a larger French multicenter study, there were 167 patients included who were treated with conservative management including methotrexate. There was one maternal death attributed to methotrexate therapy, when it was injected into the umbilical cord [43].
Methotrexate works by disrupting the folic acid pathway in rapidly dividing cells such as first and second trimester trophoblasts. Trophoblasts’ division is limited and does not appear to contribute significantly to placental growth in the later stages of pregnancy; therefore, there is no biologic plausibility for the mechanism of action of methotrexate, and it likely does not reduce the volume of the placenta [44]. Methotrexate is immunosuppressive, which can be harmful in the case of PAS, as patients are already at higher risk of morbidity due to longer operative time—the risk for infection and sepsis may be therefore be exacerbated with methotrexate therapy. Methotrexate can cause pancytopenia, nephrotoxicity, and toxic accumulation when injected intra-umbilically [41]. Based on these risks, the IS-PAS consensus guidelines strongly recommend against using methotrexate [7].
Conclusions
Many adjunctive treatments may be used singly or in combination in addition to the gold standard treatment for PAS—hysterectomy. These strategies can also be used in conjunction with conservative management. Emerging strategies need further investigation and may provide a wider array of novel options for PAS management.
References
Ravina J, Ciraru-Vigneron N, Bouret J, Herbreteau D, Houdart E, Aymard A, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995;346(8976):671–2.
Vedantham S, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: an underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol. 1997;176(4):938–48.
Momah-Ukeh I, Ertreo M. Uterine artery embolization. Essential interventional radiology review. Springer; 2022. p. 567–77.
Pelage J-P, Le Dref O, Mateo J, Soyer P, Jacob D, Kardache M, et al. Life-threatening primary postpartum hemorrhage: treatment with emergency selective arterial embolization. Radiology. 1998;208(2):359–62.
Salazar GM, Petrozza JC, Walker TG. Transcatheter endovascular techniques for management of obstetrical and gynecologic emergencies. Tech Vasc Interv Radiol. 2009;12(2):139–47.
Varghese K, Adhyapak S. Therapeutic Embolization. Springer; 2017.
Collins SL, Alemdar B, van Beekhuizen HJ, Bertholdt C, Braun T, Calda P, et al. Evidence-based guidelines for the management of abnormally invasive placenta: recommendations from the International Society for Abnormally Invasive Placenta. Am J Obstet Gynecol. 2019;220(6):511–26.
Mei J, Wang Y, Zou B, Hou Y, Ma T, Chen M, et al. Systematic review of uterus-preserving treatment modalities for abnormally invasive placenta. J Obstet Gynaecol. 2015;35(8):777–82.
Pan Y, Zhou X, Yang Z, Cui S, De W, Sun L. Retrospective cohort study of prophylactic intraoperative uterine artery embolization for abnormally invasive placenta. Int J Gynecol Obstet. 2017;137(1):45–50.
Wang M, Ballah D, Wade A, Taylor AG, Rizzuto G, Li B, et al. Uterine artery embolization following cesarean delivery but prior to hysterectomy in the management of patients with invasive placenta. J Vasc Interv Radiol. 2019;30(5):687–91.
Niola R, Giurazza F, Nazzaro G, Silvestre M, Nasti G, Di Pasquale MA, et al. Uterine artery embolization before delivery to prevent postpartum hemorrhage. J Vasc Interv Radiol. 2016;27(3):376–82.
Matsubara S. Re: uterine artery embolization before delivery to prevent postpartum hemorrhage. J Vasc Interv Radiol. 2016;27(7):1101–2.
Iwata A, Murayama Y, Itakura A, Baba K, Seki H, Takeda S. Limitations of internal iliac artery ligation for the reduction of intraoperative hemorrhage during cesarean hysterectomy in cases of placenta previa accreta. J Obstet Gynaecol Res. 2010;36(2):254–9.
Hussein AM, Dakhly DMR, Raslan AN, Kamel A, Abdel Hafeez A, Moussa M, et al. The role of prophylactic internal iliac artery ligation in abnormally invasive placenta undergoing caesarean hysterectomy: a randomized control trial. J Matern Fetal Neonatal Med. 2019;32(20):3386–92.
Camuzcuoglu H, Toy H, Vural M, Yildiz F, Aydın H. Internal iliac artery ligation for severe postpartum hemorrhage and severe hemorrhage after postpartum hysterectomy. J Obstet Gynaecol Res. 2010;36(3):538–43.
Shahin Y, Pang CL. Endovascular interventional modalities for haemorrhage control in abnormal placental implantation deliveries: a systematic review and meta-analysis. Eur Radiol. 2018;28(7):2713–26.
B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ. The B-Lynch surgical technique for the control of massive postpartum haemorrhage: an alternative to hysterectomy? Five cases reported. BJOG Int J Obstet Gynaecol. 1997;104(3):372–5.
Pereira A, Nunes F, Pedroso S, Saraiva J, Retto H, Meirinho M. Compressive uterine sutures to treat postpartum bleeding secondary to uterine atony. Obstet Gynecol. 2005;106(3):569–72.
Hayman R, Arulkumaran S, Steer P. Uterine compression sutures: surgical management of postpartum hemorrhage. Obstet Gynecol. 2002;99(3):502–6.
Cho JH, Jun HS, Lee CN. Hemostatic suturing technique for uterine bleeding during cesarean delivery, vol. 96. Elsevier; 2000. p. 129.
Takahashi H, Baba Y, Usui R, Suzuki H, Horie K, Yano H, et al. Matsubara–Yano suture: a simple uterine compression suture for postpartum hemorrhage during cesarean section. Arch Gynecol Obstet. 2019;299(1):113–21.
Shazly SAE, Badee AY, Ali MK. The use of multiple 8 compression suturing as a novel procedure to preserve fertility in patients with placenta accreta: case series. Aust N Z J Obstet Gynaecol. 2012;52(4):395–9.
Shahin AY, Farghaly TA, Mohamed SA, Shokry M, Abd-El-Aal D-EM, Youssef MA. Bilateral uterine artery ligation plus B-Lynch procedure for atonic postpartum hemorrhage with placenta accreta. Int J Gynecol Obstet. 2010;108(3):187–90.
Mohamed MA, Mohammed AH. Parallel vertical compression sutures to control bleeding in cases of placenta previa and accreta. J Matern Fetal Neonatal Med. 2019;32(4):641–5.
Zhu L, Lu J, Huang W, Zhao J, Li M, Zhuang H, et al. A modified suture technique for the treatment of patients with pernicious placenta previa and placenta accreta spectrum: a case series. Ann Trans Med. 2021;9(14):1140.
ElNoury MAH, Webster SN, Abdelhalim DA. ElNoury–Webster bundle: a preemptive surgical approach with a modified lower B-Lynch compression suture to manage morbidly low or adherent placenta. J Matern Fetal Neonatal Med. 2021:1–4.
Ratiu AC, Crisan DC. A prospective evaluation and management of different types of placenta praevia using parallel vertical compression suture to preserve uterus. Medicine. 2018;97(46):e13253.
Shih JC, Liu KL, Kang J, Yang JH, Lin MW, Yu CU. ‘Nausicaa’ compression suture: a simple and effective alternative to hysterectomy in placenta accreta spectrum and other causes of severe postpartum haemorrhage. BJOG Int J Obstet Gynaecol. 2019;126(3):412–7.
Shakur H, Roberts I, Fawole B, Chaudhri R, El-Sheikh M, Akintan A, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105–16.
Shakur H, Roberts I, Bautista R, Caballero J, Coats T, Dewan Y, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376(9734):23.
Schwickert A, van Beekhuizen HJ, Bertholdt C, Fox KA, Kayem G, Morel O, et al. Association of peripartum management and high maternal blood loss at cesarean delivery for placenta accreta spectrum (PAS): a multinational database study. Acta Obstet Gynecol Scand. 2021;100:29–40.
Orsi F, Arnone P, Chen W, Zhang L. High intensity focused ultrasound ablation: a new therapeutic option for solid tumors. J Cancer Res Ther. 2010;6(4):414.
Jeng C-J, Ou K-Y, Long C-Y, Chuang L, Ker C-R. 500 cases of high-intensity focused ultrasound (HIFU) ablated uterine fibroids and adenomyosis. Taiwanese J Obstet Gynecol. 2020;59(6):865–71.
Hong Y, Guo Q, Pu Y, Lu D, Hu M. Outcome of high-intensity focused ultrasound and uterine artery embolization in the treatment and management of cesarean scar pregnancy: A retrospective study. Medicine. 2017;96(30):e7687.
Abd Elazeem HAS, Saad MM, Ahmed IA, Sayed EG, AlMahdy AM, Atef F, et al. High-intensity focused ultrasound in management of placenta accreta spectrum: A systematic review. Int J Gynecol Obstet. 2020;151(3):325–32.
Bai Y, Luo X, Li Q, Yin N, Fu X, Zhang H, et al. High-intensity focused ultrasound treatment of placenta accreta after vaginal delivery: a preliminary study. Ultrasound Obstet Gynecol. 2016;47(4):492–8.
Ye M, Yin Z, Xue M, Deng X. High-intensity focused ultrasound combined with hysteroscopic resection for the treatment of placenta accreta. BJOG Int J Obstet Gynaecol. 2017;124:71–7.
Jiang X, Tang Q, Yang B, Ye F, Cai L, Wang X, et al. High-intensity focused ultrasound combined procedures treatment of retained placenta accreta with marked vascularity after abortion or delivery. Int J Hyperth. 2019;36(1):420–6.
Liu Y, Zhang WW, He M, Gong C, Xie B, Wen X, et al. Adverse effect analysis of high-intensity focused ultrasound in the treatment of benign uterine diseases. Int J Hyperth. 2018;35(1):56–61.
Arulkumaran S, Ng C, Ingemarsson I, Ratnam S. Medical treatment of placenta accreta with methotrexate. Acta Obstet Gynecol Scand. 1986;65(3):285–6.
Steins Bisschop CN, Schaap TP, Vogelvang TE, Scholten PC. Invasive placentation and uterus preserving treatment modalities: a systematic review. Arch Gynecol Obstet. 2011;284(2):491–502.
Zhang C, Li H, Zuo C, Wang X. Retrospective analysis: conservative treatment of placenta increta with methotrexate. J Obstet Gynaecol Res. 2018;44(5):907–13.
Sentilhes L, Ambroselli C, Kayem G, Provansal M, Fernandez H, Perrotin F, et al. Maternal outcome after conservative treatment of placenta accreta. Obstet Gynecol. 2010;115(3):526–34.
Khan M, Sachdeva P, Arora R, Bhasin S. Conservative management of morbidly adherant placenta–a case report and review of literature. Placenta. 2013;34(10):963–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Shah, S.C., Fox, K.A., Nassr, A.A. (2023). Adjunctive Treatment of Placenta Accreta Spectrum. In: Shazly, S.A., Nassr, A.A. (eds) Placenta Accreta Spectrum. Springer, Cham. https://doi.org/10.1007/978-3-031-10347-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-10347-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-10346-9
Online ISBN: 978-3-031-10347-6
eBook Packages: MedicineMedicine (R0)