Abstract
Leprosy is a chronic disease with varied manifestations. Its varied course, prognosis, and complications require a distinct classification. A uniform classification helps in communication at field level with appropriate diagnosis and management of disease. But at the research level, the perception is different. Here we have described currently available different classifications of leprosy to meet the expectations of both primary healthcare workers and researchers.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
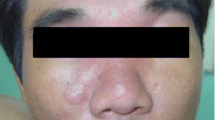
Leprosy can present with cutaneous lesions and/or neural symptoms. The wide variations in disease presentation and its course, prognosis, and complications force one to consider these variants as a distinct entity and need to classify the disease. But a single classification can’t meet all the criteria at all levels. Hence, a uniform classification by WHO helps in easy communication among field workers and early diagnosis and treatment of leprosy. The comparison of clinical, histological, bacteriological, and immunological parameters by Ridley-Jopling helps the researchers to understand the finer aspects of the disease.
Classification of Leprosy
Classification of leprosy is important because it decides the line of treatment and stage and prognosis of the disease.
Criteria Deciding Classifications
-
1.
Bacteriological criteria: measures the density of organism in lesions and estimated by slit skin smear technique or in biopsy specimens.
-
2.
Immunological criteria: deficiency of cell-mediated immunity against M. leprae is measured by lepromin testing. Patients are classified as lepromin positive (good immunity) and lepromin negative (poor immunity).
-
3.
Histological criteria: it reflects the actual process going on inside the body in the form of tissue reactions. It is the most definitive criteria for defining different entities.
-
4.
Clinical criteria: Easiest to apply as clinical features can be identified and applied easily.
Types
Madrid classification, Indian, New IAL, Ridley-Jopling, WHO classification
Ridley-Jopling Classification [1, 2]
Defined five groups on the basis of clinical, bacteriological, histological, and immunological features (Table 1.1). It is very useful in research purposes, but not feasible in primary health centers and field levels. This classification does not include indeterminate type and pure neuritic type of leprosy.
-
1.
Tuberculoid leprosy (TT)
-
2.
Borderline tuberculoid (BT)
-
3.
Borderline borderline (BB)
-
4.
Borderline lepromatous (BL)
-
5.
Lepromatous leprosy (LL)
Indian Classification [4]
It includes six groups that have maculo-anesthetic (MA) and pure neuritic as separate categories. The main drawback was the classification was not entirely clinical and its usefulness at all levels of leprosy workers was doubtful. But it adds the pure neuritic leprosy cases which were not in Ridley-Jopling classification.
The types are as follows:
-
Lepromatous (L)
-
Tuberculoid (T)
-
Maculo-anesthetic (MA)
-
Polyneuritic (P)
-
Borderline (B)
-
Indeterminate (I)
New IAL Classification [5]
A modification of Indian classification has been adopted by IAL where maculo-anesthetic (MA) leprosy was merged with tuberculoid (T) leprosy.
-
Lepromatous (L)
-
Tuberculoid (T)
-
Polyneuritic (P)
-
Borderline (B)
-
Indeterminate (I)
WHO Classification (1988)
It was the most important classification of the disease for any treating leprologist. The patients were categorized depending upon whether slit skin smears demonstrate any bacilli or not.
Paucibacillary leprosy (PB): Only smear-negative cases and include indeterminate (I), tuberculoid (T), and borderline tuberculoid (BT) cases under Ridley-Jopling.
Multibacillary leprosy (MB): All smear-positive cases and mid-borderline (BB), borderline lepromatous (BL), and lepromatous (LL) types under Ridley-Jopling classification.
WHO Classification (1998) [6]
Application of slit skin smear universally to maintain their quality in control programs was the biggest challenge. Hence, in 1998, the WHO categorized PB and MB leprosy depending upon the number of skin lesions to overcome the operational problem of slit skin smear.
-
Paucibacillary single lesion leprosy (SLPB)
-
Paucibacillary leprosy (PB) (two to five skin lesions)
-
Multibacillary leprosy (MB) (six or more skin lesions and all smear-positive cases)
Current WHO Classification
For field workers, the WHO has classified leprosy based on number of skin lesions for treatment purposes (Table 1.2). The sensitivity and specificity of this operational classification tested using slit skin smear and biopsy results as the gold standard were found to be 63% and 85%, respectively. 8th WHO expert excludes SLPB [7].
Classification Under NLEP, India (2009) [8]
This classification is currently used in India for treatment purposes. It considers the number of nerve involvement along with skin lesion count while categorizing PB and MB leprosy (Table 1.3). The main advantage includes early diagnosis of pure neuritic leprosy that constitutes around 4–5 percent of all leprosy cases in our country.
Conclusion
Not a single classification can only meet the expectations at all levels of leprosy workers. Currently, the WHO classification, based on skin/nerve lesion count, is simple and practical to follow for treatment purposes worldwide. Ridley-Jopling classification remains the most useful one for academic and research purposes.
Abbreviations
- AFB:
-
Acid fast bacilli
- MB:
-
Multibacillary
- NLEP:
-
National Leprosy Eradication Programme
- PB:
-
Paucibacillary
- SSS:
-
Slit skin smear
- WHO:
-
World Health Organization
References
Ridley DS, Jopling WH. A classification of leprosy for research purposes. Lepr Rev. 1962;33:119–28.
Ridley DS, Jopling WH. Classification of leprosy according to immunity. A five group system. Int J Lepr. 1966;34(3):255–73.
Kundu SK. Features of Ridley-Jopling classification and its application in the clinical field. Int J Lepr Other Mycobact Dis. 1979;47:64–5.
All India Leprosy Workers Conference. Classification of leprosy adopted by the Indian association of leprologists. Lepr India. 1955, 1955;(27):93–5.
Clinical, Histopathological. Immunological features of the five type classification approved by the Indian Association of Leprologists. Lepr India. 1982;54:22–32.
WHO. Expert committee on leprosy. 6th report. Geneva: World Health Organization; 1988. Tech Rep Ser 768.
World Health Organization. WHO expert committee on leprosy. 8th report. Geneva: WHO; 2012; No. 968.
World Health Organization, Leprosy Elimination Group. Guide to eliminate leprosy as a public health problem; WHO/CDS/CPE/2000.14. 2000. http//whqlibdoc.who.int/hq/2000/WHO_CDS_CPE_CEE_2000.14.pdf.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Padhi, T., Sahu, K., Pradhan, S. (2022). Clinical Classification of Leprosy. In: Pradhan, S., Kumar, P. (eds) Clinical Cases in Leprosy. Clinical Cases in Dermatology. Springer, Cham. https://doi.org/10.1007/978-3-031-08220-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-08220-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08219-1
Online ISBN: 978-3-031-08220-7
eBook Packages: MedicineMedicine (R0)