Abstract
Diagnosis and classification are two essential points for correct patient management. Correct classification allows proper treatment and alerts of the risk of leprosy reaction and nerve damage. The Ridley–Jopling classification recognizes the complex pathogenesis of leprosy and is based on a spectrum that extends from tuberculoid leprosy (TT), through borderline tuberculoid (BT), mid-borderline (BB), borderline lepromatous (BL), to the poorly resistant lepromatous leprosy (LL). The World Health Organization (WHO) classification, for therapeutic purposes, divides patients into paucibacillary (PB) and multibacillary (MB) on the basis of the number of skin lesions. PB cases have up to five skin lesions in total, whereas MB cases have six or more skin lesions. The two systems are complementary rather than exclusive.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Diagnosis and classification are two essential points for correct patient management. Correct classification allows proper treatment and alerts of the risk of leprosy reaction and nerve damage. A generic diagnosis of “leprosy” must be avoided.
1 Classifications of Leprosy Before Ridley and Jopling
Leprosy classification has been a matter of debate for many years. The first classifications were based only upon clinical parameters, generating confusion and controversies. Moreover, different countries and schools applied different classifications, making communication between leprologists at international meetings almost impossible.
Since the beginning of the twentieth century, there has been the need for a unitary international classification; different systems were proposed at international meetings in Manila (1931), Cairo (1938), Rio de Janeiro (1946), and Havana (1948), until the Madrid Congress held in 1953, where a classification based on four main disease groups was formulated [1]:
-
Lepromatous leprosy (L) (macular, nodular, diffuse infiltrate, pure neuritic).
-
Tuberculoid leprosy (T) (minor, major, and reactional).
-
Indeterminate leprosy (I) (macular, pure neuritic).
-
Borderline or dimorphous leprosy.
2 Ridley–Jopling Classification
In 1962 and 1966, Ridley and Jopling (R&J) [2, 3] proposed a new classification based not only on the clinical features but also on histopathology, the degree of cell-mediated immune response (CMI) against M. leprae, and bacterial load [4]. This classification recognizes the complex pathogenesis of leprosy and is based on a five-group spectrum (Fig. 6.1) that extends from tuberculoid leprosy (TT) with heightened CMI (hyperergic pole; Chap. 5), through borderline tuberculoid (BT), mid-borderline (BB), borderline lepromatous (BL), to the poorly resistant (anergic) lepromatous type (LL) characterized by increased humoral immunity. TT and LL patients are immunologically stable (meaning that they do not usually shift to another type), while borderline patients (BT, BB, and BL) are immunologically unstable (i.e., they may abruptly shift from one form to another).
Indeterminate leprosy (I) does not fall into this spectrum because there is lack of correlation between the clinico- and histopathological features. Indeterminate leprosy represents an early stage of the disease in which the degree of CMI is still not clear. Patients with indeterminate leprosy either can heal or might develop leprosy and move on borderline part of the spectrum [1].
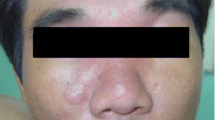
In each of the five forms of the spectrum, the clinicobacteriological and histopathological parameters have to agree with each other (Table 26.1). Along the leprosy spectrum, between the two polar forms, there is a graduation of the clinical manifestations (Table 26.2). Of course, not all patients may fit neatly into one of the five forms. As Ridley himself noted, “The spectrum is uninterrupted and there may be patients with an intermediate position among two groups” [4, 5]. Patients with TT leprosy have a high degree of CMI, having one or two skin lesions with monolateral distribution, with no or few bacilli and epithelioid granuloma on histopathology (Chap. 12). Moving in the spectrum toward the lepromatous pole, the CMI decreases progressively; BT patients have few lesions, asymmetrically distributed, with no or few bacilli and epithelioid granulomas on histopathology. In BB patients, the lesions become symmetric, there are some bacilli, and granulomas show both epithelioid and macrophage features. CMI progressively decreases, so that BL and LL show many symmetrically distributed lesions (see Chap. 12) with many bacilli and macrophage granuloma on histopathology.
BT and BL are the most frequent forms of presentation of leprosy. TT is uncommon, as it can also heal spontaneously. The BB form is rare because it is immunologically highly unstable and BB patients frequently shift to BT or BL. LL shows different prevalence among continents, probably due to genetic factors: in South America it represents more than 20% of cases, in Asia 5–20%, and in sub-Saharan Africa less than 5%.
The Ridley–Jopling classification was proposed over 40 years ago, and it has never been standardized. Moreover, discrepancies between clinical pictures and histopathological features have been described (Chap. 12). The Ridley–Jopling spectral concept cannot explain single variations encountered in leprosy, which represent however only a minority of cases. Interestingly, the spectral concept based on CMI has been expanded to explain the divergent manifestation seen in other diseases such as leishmaniasis, tuberculosis, and even lupus erythematosus.
3 The WHO Classifications
In 1982, the WHO introduced the multidrug therapy (MDT) with two different treatment schemes correlated to the result of the slit-skin smear examination. Patients were classified as paucibacillary (PB) if the bacterial index (BI) was 2+ or as multibacillary (MB) if the BI was C2+ [6].
In 1988, all cases with positive slit-skin smear at any site were grouped as MB and all cases with negative slit-skin smear as PB [7].
In 1998, the WHO repealed the use of slit-skin smear examination for the classification and recommended a new classification based only on the number of the lesions, with patients having up to five lesions in total being PB and those with six or more skin lesions being MB. If skin smear is done and is positive, the patient is classified as MB irrespective of the skin lesions. This lesion counting system is currently published in the WHO Guidelines for the diagnosis, treatment and prevention of leprosy (2018) [8, 9]. According to the WHO, “The diagnosis of leprosy remains based on the presence of at least one of three cardinal signs: (1) definite loss of sensation in a pale (hypopigmented) or reddish skin patch; (2) thickened or enlarged peripheral nerve with loss of sensation and/or weakness of the muscles supplied by that nerve; or (3) presence of acid-fast bacilli in a slit-skin smear.”
3.1 The Issue of the Two Classification Systems
Treatment schedules are determined by classification. Both the R&J and WHO classifications are well established but also have shortcomings.
With the lesion counting system, classifying and treating patients has become simpler. The WHO system is appropriate and has had great success, especially in highly endemic, low-resource settings. It is easy to use and teach, and general healthcare workers can easily allocate patients to the appropriate treatment regimen. Moreover, some countries such as Brazil apply a modified WHO classification [10, 11].
Nevertheless, this system has some weakness. Assessing skin lesions might not always be easy. It depends on the amount of skin examined, the quality of the light, and of course the expertise of the leprosy workers, who still have to recognize the wide range of manifestations of leprosy. Moreover, the number and appearance of skin lesions may change over time; for example, during reaction, lesions may become more evident. In early BL/LL cases, skin lesions are often few and difficult to see or even invisible. Furthermore, the size of the lesion also matters but is not considered in the WHO classification [12].
As demonstrated in various studies, underestimation of the number of lesions and misclassification (particularly for MB patients) may happen, leaving patients at risk of under- or overtreatment [13]. For example, MB patients presenting few lesions will be incorrectly classified as PB and will receive insufficient chemotherapy, becoming exposed to the possibility of drug resistance and relapses. Of course determination of bacterial load in skin smears considerably improves the reliability of the classification, but this service is often not available in areas where leprosy is most common. Most importantly, contrary to the R&J classification, the WHO system does not identify the categories of patients at high risk for leprosy reaction and in need of accurate follow-up.
The classification influences also research and epidemiological studies. The PB category comprises patients with I, TT, and part of BT leprosy. In fact, the line dividing PB from MB cases crosses the BT form. The MB category is equally heterogeneous and comprises part of BT, BB, BL, and LL patients, rendering comparison among studies performed with the two systems impossible. Moreover, due to the changes in the WHO classification in the last 25 years, it is hard to compare works done 20 years ago with those done more recently. Also, data among countries and even within a country itself are at risk of misclassification [9, 13].
We completely agree with Lockwood et al. that the two classifications, R&J and WHO, should be seen as being complementary rather than exclusive [9]. The WHO classification is useful for allocating patients to treatment groups and should be used in peripheral centers where skin smears and histopathology are not available. The R&J classification has to be used in referral centers and in the research context, because it permits better understanding of disease pathology, prognosis, and risk factors for complications, and provides standardization and comparability of studies over time and location [14, 15].
References
Ridley DS. Pathogenesis of leprosy and related diseases. London: Wright; 1988.
Ridley DS, Jopling WH. A classification of leprosy for research purposes. Lepr Rev. 1962;33:119–28.
Ridley DS, Jopling WH. Classification of leprosy according to immunity—a five-group system. Int J Lepr Other Mycobact Dis. 1966;34:255–73.
Ridley DS. Nature of the leprosy spectrum. In: Ridley DS, editor. Pathogenesis of leprosy and related diseases. London: Wright; 1988. p. 93–105.
Noto S, Clapasson A, Nunzi E. Classification of leprosy: the mystery of “reactional tuberculoid”. G Ital Dermatol Venereal. 2007;142:294–5.
WHO. Chemotherapy of leprosy for control programmes. Technical report series 675. Geneva: World Health Organization; 1982.
WHO. A guide to leprosy control. 2nd ed. Geneva: WHO; 1988.
WHO. Enhanced global strategy for further reducing the disease burden due to leprosy (2011–2015). Operational guidelines (Updated); 2009
Lockwood DN, Sarno E, Smith WC. Classifying leprosy patients–searching for the perfect solution? Lepr Rev. 2007;78:317–20.
Guia para o controle da hanseniase. Brasilia: Ministério da Saúde; 2002. http://bvsms. saude.gov.br/bvs/publicacoes/guia_de_hanseniase.pdf.
Talhari S. Diagnosis, classification and prognosis. Int J Leprosy. 1996;64(Suppl):s13–4.
Parkash O. Classification of leprosy into multibacillary and paucibacillary groups: an analysis. FEMS Immunol Med Microbiol. 2009;55:1–5.
Buhrer-Sekula S, Visschedijk J, Grossi MAF, et al. The ML flow test as a point of care test for leprosy control programmes: potential effects on classification of leprosy patients. Lepr Rev. 2007;78:271–9.
WHO. Guidelines for the diagnosis, treatment and prevention of leprosy; 2018.
Alemu Belachew W, Naafs B. Position statement: leprosy: diagnosis, treatment and follow-up. J Eur Acad Dermatol Venereol. 2019;33(7):1205–13.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Massone, C., Brunasso, A.M.G. (2022). Classification of Leprosy. In: Nunzi, E., Massone, C., Portaels, F. (eds) Leprosy and Buruli Ulcer. Springer, Cham. https://doi.org/10.1007/978-3-030-89704-8_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-89704-8_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-89703-1
Online ISBN: 978-3-030-89704-8
eBook Packages: MedicineMedicine (R0)