Abstract
Calcific tendinopathy of the shoulder implicates calcification and degeneration of the rotator cuff tendon nearby its insertion point on the greater tuberosity. The objective of this chapter is to review recent literature assessing the clinical results of nonoperative and operative management for calcific tendinopathy of the shoulder. Conservative treatment, extracorporeal shock wave therapy (ESWT), ultrasound-guided percutaneous irrigation of calcific tendinopathy (US-PICT), and surgical intervention will be analyzed. Conservative treatment, ESWT, US-PICT, and operative management have all been identified to be beneficial in the management of symptomatic calcific tendinopathy. Conservative treatment is very efficacious for most patients and should be the first line of management. In patients who fail conservative treatment, ESWT or US-PICT is frequently efficacious and should be the next step in management. Surgery should be reserved for patients who have failed these other modalities of treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
3.1 Introduction
Rotator cuff calcific tendinitis (RCCT) is a frequent pathologic condition affecting the rotator cuff, principally happening in women in their forties [1,2,3]. Commonly, patients complain of a low-degree subacute shoulder pain augmenting during the night [3]. Plain radiography and ultrasound (US) are the imaging tests of choice [4], permitting easy identification of focal calcium depositions in the RC tendons, mainly in the supraspinatus (80%) and less commonly in the infraspinatus and subscapularis tendons (15% and 5% of all cases, respectively) [2].
Conversely, magnetic resonance imaging (MRI) is not usually indicated in this setting due to the well-known limitations of this imaging technique in the assessment of RCCT, even though it is considered the crucial imaging test to exclude other pathologic conditions of the shoulder [5,6,7]. RCCT is a self-limiting condition that can be completely asymptomatic in chronic stage and not in need of management. Nevertheless, in some cases, it can represent a painful and disabling condition, especially when considering the acute stage [3]. Discomfort intensity affects the selected management: conservative (rehabilitation medicine and oral anti-inflammatory medication) if pain is mild or more invasive (shock waves, surgery, and imaging-guided irrigation) when symptoms are more severe. Shock wave lithotripsy was shown to be not always resolving [8], and, at present, there is no standard of care for RCCT [1, 9].
Over the last years, US-guided percutaneous irrigation of calcific tendinopathy (US-PICT) has become more and more universally utilized [10] because of its minimal invasiveness compared to surgery and its radical impact on calcifications in comparison to shock waves, since mineralized deposits are disaggregated and removed outside the tendon [11, 12]. Moreover, it has been previously reported how US-PICT makes easier rapid shoulder function recovery and pain alleviation [13]. The technique is usually carried out with 16- to 21-gauge needles under local anesthesia. It is shown that even interventional or minor surgical techniques may be associated with a significant psychological burden in patients, possibly producing discomfort and anxiety [14].
The purpose of this chapter is to analyze recent literature evaluating the clinical outcomes of nonoperative and operative treatment for calcific tendinopathy of the shoulder.
3.2 Pathogenesis
In 2020 Cho et al. identified differentially expressed genes associated with extracellular matrix degradation and inflammatory regulation in calcific tendinopathy utilizing RNA sequencing [15]. They identified 202 differentially expressed genes (DEGs) between calcific and adjacent normal tendon tissues of rotator cuff using RNA sequencing-based transcriptome analysis. The DEGs were highly enriched in extracellular matrix (ECM) degradation and inflammation-related processes. Further, matrix metalloproteinase 9 (MMP9) and matrix metalloproteinase 13 (MMP13), two of the enzymes associated with ECM degradation, were encountered to be highly upregulated 25.85- and 19.40-fold, respectively, in the calcific tendon tissues compared to the adjacent normal tendon tissues. Histopathological analyses indicated collagen degradation and macrophage infiltration at the sites of calcific deposit in the rotator cuff tendon. This study could help to better understand the pathogenesis associated with calcific tendinopathy [15].
3.3 Imaging
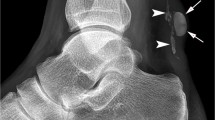
RCCT has a typical imaging presentation: in most cases, calcific deposits appear as a dense opacity around the humeral head on conventional radiography (Fig. 3.1), as hyperechoic foci with or without acoustic shadow at ultrasound and as a signal void at magnetic resonance imaging (Fig. 3.2) [16]. Nonetheless, we have to take into account the possible unusual presentations of RCCT and the key imaging features to correctly differentiate RCCT from other RC conditions, such as calcific enthesopathy or RC tears. Other presentations of RCCT to be considered are intrabursal, intraosseous, and intramuscular migration of calcific deposits that may mimic infectious processes or malignancies. While intrabursal and intraosseous migration are quite common, intramuscular migration is an unusual evolution of RCCT. It is important also to know atypical regions affected by calcific tendinopathy as biceps brachii, pectoralis major, and deltoid tendons [16].
An important question is to know whether MRI of the shoulder is ever appropriate in assessing patients with calcific tendinopathy of the rotator cuff. According to Beckmann et al., a shoulder MRI might be carried out for preoperative planning prior to surgical removal of calcium deposits, but even in this patient population, the prevalence of full-thickness rotator cuff tear is low [17].
In 2021, Laucis et al. compared the prevalence of rotator cuff (RC) tears on shoulder ultrasounds of patients with RC calcific tendinopathy (CaT) to that of a control group without CaT [18]. RC tears were diagnosed in 38% (19/50) of the control group (16 full-thickness) as compared to 22% (11/50) with CaT (6 full-thickness). The fewer full-thickness tears in the CaT group (12%, 6 of 50) compared to that in the control group (32%, 16 of 50) was statistically significant (P = 0.016, odds ratio 0.29). Only 7 of the 11 tears in the CaT group were in a calcium-containing tendon (3 full-thickness). The fewer calcium-containing tendon tears compared to tears in the control group was also statistically significant (P = 0.006, odds ratio 0.27). Moreover, the fewer full-thickness calcium-containing tendon tears (6%, 3/50) compared to full-thickness tears in the control group (32%, 16/50) were yet more statistically significant (P = 0.001, odds ratio 0.14). In patients with shoulder pain and CaT, Laucis et al. observed a decreased number of RC tears and especially calcium containing tendon tears, as compared to similar demographic patients with shoulder pain but without CaT [18].
In 2019, Beckman et al. compared the incidence of rotator cuff tears in the setting of calcific tendinopathy on MRI (a case controlled comparison) [19]. They found that patients presenting with indeterminate shoulder pain and rotator cuff calcific tendinopathy were not at augmented risk for having a rotator cuff tear compared with similar demographic patients without calcific tendinopathy presenting with shoulder pain. It appeared that calcific tendinopathy and rotator cuff tears likely arise from different pathological processes [19].
3.4 Treatment
According to Beckmann et al., in most cases, calcific tendinopathy is a self-limited process, typically resolving within a few weeks or months [17]. During this period, conservative treatment with nonsteroidal anti-inflammatory drugs, rehabilitation medicine, warm compresses, and possibly a corticosteroid injection into the subacromial bursa can be administered for symptomatic pain alleviation. Around 10% of patients with calcific tendinopathy will have protracted symptoms that are refractory to conservative treatment. Even in this population of patients with calcific tendinopathy and failed conservative treatment, the prevalence of full-thickness tear remains low. Extracorporeal shockwave therapy and ultrasound-guided needle techniques are efficacious in alleviating pain and resolving the calcium deposits in chronic calcific tendinopathy of the rotator cuff that has failed initial conservative management These treatments are minimally invasive and involve mostly minor complications of soreness, local bruising/ swelling, and subcutaneous hemorrhage, which happen in 10% of patients treated with ultrasound-guided needle techniques and 7%–19% of patients treated with extracorporeal shockwave therapy. Surgical removal of the calcium deposits of calcific tendinopathy is also efficacious in diminishing pain and ameliorating function by utilizing either arthroscopic or open techniques. Nonetheless, surgery is expensive and requires exposure to anesthesia and a longer recovery period compared with other less invasive treatments. For these reasons, surgery should be indicated in patients who have protracted, activity-limiting pain and have failed initial conservative and minimally invasive treatments. In this select population of patients with chronic calcific tendinopathy and prolonged refractory pain being considered for surgical removal of the calcifications, shoulder MRI may be warranted for preoperative planning [17].
3.4.1 Ultrasound-Guided Percutaneous Irrigation of Rotator Cuff Calcific Tendinopathy (US-PICT)
In 2020, Albano et al. assessed patients’ experience of US-PICT. They found that US-PICT was a mildly painful, comfortable, and well-tolerated technique, regardless of any previous treatments. Patients’ satisfaction was correlated with clinical benefit and full explanation of the technique and its complications [20].
3.4.1.1 US-Guided Percutaneous Irrigation of Calcific Tendinopathy of the Rotator Cuff in Patients with or Without Previous External Shockwave Therapy
In 2021, Lanza et al. compared the outcome of US-PICT of the rotator cuff in patients with or without previous external shockwave therapy (ESWT) [21]. They found that US-PICT of the rotator cuff was an efficacious technique to diminish shoulder pain and augment mobility in patients with calcific tendinopathy, both in short- and long-run time intervals. Previous unsuccessful ESWT did not affect the result of US-PICT.
3.4.1.2 Efficacy of Ultrasound-Guided Percutaneous Treatment of the Rotator Cuff Calcific Tendinopathy with Double Needle Technique
According to Saba et al., US-PICT with double needle was a dependable and reproducible procedure for treatment of the RCCT and their clinical symptoms, when conservative treatment was insufficient [22]. Only patients with calcification at least 5 mm in size with and with acute pain and functional limitation were selected. All patients had a shoulder radiograph to compare it with posttreatment. The patient was placed supine and disinfected profusely. Then percutaneous local anesthesia (Lidocaine 10 mg/mL) was carried out utilizing 25-gauge (G) needle, along the path chosen for the treatment and for both needles. Then, two 18 G needles were introduced into the calcification, with the first needle that must be inserted in a deep position. With a 20 mL syringe prefilled with saline and lidocaine (the irrigation of the calcification could be painful), pressure was applied to one of the two needles. It is possible to insert a 20 G needle into each needle to remove calcium that may obstruct needle tips. During the technique, the needle can also be moved to other areas to be treated, depending on the size and shape of the calcification. The duration of the treatment depended on the size and the hardness of the calcification. After the destruction of the calcification, the fragments pushed by the physiological solution were able to exit by from the other needle positioned inside the calcification creating a washing circuit. Finally, infiltration into the subacromial-subdeltoid bursa (SASD) with cortisone (Betamethasone dipropionate 1 mL) was performed [22].
3.4.1.3 US-PICT: Redefining Predictors of Treatment Outcome
In 2020, Vassalou et al., tried to identify prognostic factors affecting the clinical result in patients treated with rotator cuff US-PICT, by assessing the grade of calcium removal, the size and consistency of calcific deposits, and baseline level of shoulder pain and functionality [23]. The conclusion was that large calcifications and low-grade pain at baseline are correlated with short- and long-run pain amelioration. The grade of calcium removal did not impact pain or functional improvement beyond 1 week. Augmented calcification size, cystic appearance, and low-grade baseline pain predicted complete pain recovery at 1 year [23].
3.4.2 External Shock Wave Therapy (ESWT)
3.4.2.1 Focused, Radial, and Combined ESWT
A study with level 1 evidence (randomized control study) compared the clinical, functional, and ultrasonographic results of focused, radial, and combined ESWT in the management of calcific shoulder tendinopathy [24]. In the three studied groups, there was a significant amelioration in shoulder pain, active range of motion (ROM), and shoulder function by shoulder disability questionnaire (SDQ) at 1 week after the end of treatment and after 3 months follow-up. Furthermore, there was a significant sonographic reduction in calcification size in the three groups. At the end of the study, the best improvement as regards a decrease of calcification size was obtained in group III when compared with group I and group II. This study demonstrated clinical, functional, and sonographic improvement in all groups. The best therapy in calcific shoulder tendinopathy seemed to be combined focused and radial ESWT compared to interventions alone [24].
3.4.2.2 Effectiveness of Focused Shockwave Therapy Versus Radial Shockwave Therapy for Noncalcific Rotator Cuff Tendinopathies: A Randomized Clinical Trial
A randomized clinical trial, registered with ChiCTR1900022932, compared the effectiveness of focused shockwave therapy (F-SWT) versus radial shockwave therapy (R-SWT) for the treatment of noncalcific rotator cuff tendinopathies [25]. The conclusion was that both F-SWT and R-SWT were efficacious in patients with noncalcific rotator cuff tendinopathy. F-SWT proved to be significantly superior to R-SWT at long-run follow-up (more than 24 weeks).
3.4.3 Platelet-Rich Plasma (PRP)
In 2019, Kim et al. studied the effect of PRP on the degenerative rotator cuff tendinopathy according to the compositions [26]. They found that TGF-β1 and IL-1β among cellular components of PRP were related to clinical efficacy for RC tendinopathy, and concentration of IL-1β above 5.19 pg/mL and TGF-β1 above 61.79 μg/mL in PRP had better clinical results for RC tendinopathy than the exercise group. Patients were in supine position with their arms placed on the superior aspect of the iliac wing with the palm up and the elbow flexed. Kim et al. found the long head of biceps in the intertubercular groove transversely via ultrasound. After lining the probe along the long axis of biceps tendon, the probe was moved to the supraspinatus tendon in a parallel position. After finding the hypoechoic lesion, 2 mL of PRP solution was injected to the hypoechoic lesion of degenerative supraspinatus via 22-gauge syringe with peppering technique. Peppering technique was utilized to avoid tendon morphology disruption by injecting PRP into the tendon. The remaining 1 mL of PRP solution was used in analyzing the compositions of PRP [26].
3.4.4 Needle Aspiration
In 2020, Oudelaar et al. tried to identify prognostic factors for the effectiveness of needle aspiration of calcific deposits (NACD) for RCCT [27]. They found that a good initial response after NACD was associated with better results at 12 months. Patients with a longer duration of symptoms before NACD and patients who needed multiple procedures showed inferior results in terms of pain reduction and amelioration of quality of life. Smaller-size calcific deposits were associated with a less favorable result of shoulder function and quality of life scores and might therefore be less susceptible for NACD [27].
3.4.5 Dextrose Prolotherapy
In 2020, Catapano et al. systematically reviewed and assessed the efficacy and complication profile of prolotherapy using hyperosmolar dextrose solution injection for rotator cuff tendinopathy [28]. They found that prolotherapy with hyperosmolar dextrose solution was a potentially efficacious adjuvant intervention to rehabilitation medicine for patients with rotator cuff tendinopathy ranging from tendinosis to partial-thickness and small full-thickness tears. However, Catapano et al. stated that further studies were necessary to determine effects in subpopulations as well as optimal technique including dextrose concentration, volume, and location [28].
3.4.6 Sodium Thiosulfate
A study (clinical trial registration number NCT02538939) reported in 2020 assessed the tolerance and the feasibility of sodium thiosulfate (STS) lavage of calcific tendinopathy [29]. Overall, STS was well tolerated with no side effect occurring during the technique and the follow-up. Nonetheless, no significant effect on calcium disappearance could be shown compared with what is expected without STS. Darrieutort-Laffite et al. stated that new studies utilizing larger volume and repeated injections of STS were needed.
3.4.7 Surgical Treatment
Surgery should be reserved for patients who have protracted, activity-limiting pain and have failed initial conservative and minimally invasive treatments. In this select population of patients with chronic calcific tendinopathy and prolonged refractory pain being considered for surgical removal of the calcifications, shoulder MRI may be warranted for preoperative planning [30].
Surgical treatment is commonly considered if symptoms persist for more than 6 months after the start of nonoperative treatment [31]. Surgical intervention is undertaken in roughly 10% of patients, who have failed nonoperative treatment [32]. Operative management can be pursued via an arthroscopic or open approach. The open approach has been used historically but has a limited role with evolutions in arthroscopic techniques and training [31].
In the arthroscopic approach, calcium deposits are identified as a bulge within the tendon often with increased vascular patterns [33]. The tendon is commonly incised in a longitudinal manner to avoid rotator cuff tears and retraction and with the assistance of a cannula to minimize distribution of small calcification deposits [34, 35]. Effective needling of the calcification is confirmed when a snowstorm-like effect is seen in the space [34]. Additional shoulder pathologies can be addressed at the same time arthroscopically.
There have been sparse prospective randomized trials studying the effect of arthroscopic treatment on patient-reported results in patients with calcific tendinopathy of the shoulder. In a study by Sabeti et al. [36], the efficacy of arthroscopic treatment in 20 patients at 9 months after treatment was assessed. Constant and visual analog scale (VAS) pain scores significantly improved (p < 0.01). In a different study, Clement et al. [37] assessed the efficacy of arthroscopic treatment alone and arthroscopic treatment with subacromial decompression in 80 patients at 12 months after treatment. There was a statistically significant improvement in Constant and VAS pain scores for both groups (p < 0.001) but no statistical difference between them (p > 0.05).
Rompe et al. [38] and Rebuzzi et al. [39] investigated ESWT compared to arthroscopy for the treatment of calcific tendinopathy and found similar improvements between the two treatment methods. While arthroscopic treatment can provide patients relief, it is only recommended after failure of all other treatments given its invasiveness compared to ESWT and US-PICT. Controversy remains regarding the optimal methods for surgical management of calcific tendinitis. There is debate about removing all deposits versus leaving some deposits or whether or not the created tendon defect should be repaired.
In a study by Ark et al. [34], the authors concluded that complete removal of the deposits is not necessary after 12 of 14 patients obtained significant pain relief with residual calcium deposits evident on postoperative radiographs. Repair of the defects created from removal of the deposits was not performed. Alternatively, Jerosch et al. [40] suggested that complete removal of the deposits is necessary, but repair of defects afterward is not. In another study by Porcellini et al. [41], 63 patients who underwent arthroscopic debridement by one surgeon were analyzed. It was deemed that complete removal of the deposits and repair of the defects was appropriate. The authors stated that repair of the defects decreased the chance of further propagation of the tear and aids inpatient rehabilitation.
3.5 Comparative Studies
3.5.1 Operative Versus Nonoperative Management
According to Bechay et al., conservative treatment, ESWT, US-PICT, and operative management have all been found to be beneficial in the treatment of symptomatic calcific tendinopathy. Conservative management is very effective for most patients and should be the first line of treatment. In patients who fail conservative management, ESWT or US-PICT is often effective and should be the next step in treatment. Surgery should be reserved for patients who have failed these other modalities of treatment [30].
3.5.2 Radial ESWT Versus Ultrasound Therapy
Dedes et al. investigated the intensity of pain, the functionality of the upper limbs, and the quality of life of patients with rotator cuff tendinopathy by using two different therapeutic modalities, shockwave and ultrasound, whose results were evaluated pretreatment and posttreatment as well as after a 4-week follow-up [42]. The pain intensity was diminished, and both the functionality and quality of life were ameliorated after shockwave therapy posttreatment (p < 0.001) and at a 4-week follow-up (p < 0.001) compared with those found after the treatment. Similar improvements in all three parameters were also found after ultrasound treatment, but the results were not as pronounced as in the shockwave group. In conclusion, both radial shockwave and ultrasound therapies were found to be effective in the treatment of rotator cuff tendinopathy, the statistical analysis showing that radial shockwave therapy was superior to the ultrasound therapy posttreatment and at the 4-week follow-up [42].
3.5.3 Comparing Ultrasound-Guided Needling Combined with a Subacromial Corticosteroid Versus High-Energy ESWT
In a randomized controlled trial (level II of evidence), Louwerens et al. compared clinical and radiographic results after treatment with standardized high-energy ESWT and ultrasound-guided needling (UGN) in patients with symptomatic calcific tendinitis of the rotator cuff who were nonresponsive to conservative treatment [43]. Both techniques were successful in improving function and pain, with high satisfaction rates after 1-year follow-up. However, UGN was more effective in eliminating the calcific deposit, and the amount of additional treatments was greater in the ESWT group.
3.5.4 Comparison of Radial Extracorporeal Shockwave Therapy and Traditional Rehabilitation Medicine
A study investigated the efficacy of radial extracorporeal shockwave therapy (rESWT) in alleviating pain and ameliorating ROM and functionality besides conventional rehabilitation methods in the treatment of RCCT [44]. Duymaz and Sindel studied 80 patients (35 males, 45 females; mean age 53.3 years; range, 40–70 years) with chronic RCCT. Patients were randomly divided into two groups: rESWT group (n = 40) treated with conventional physiotherapy and rESWT and control group (n = 40) treated only with a conventional rehabilitation program. The traditional rehabilitation medicine program included ultrasound, transcutaneous electrical nerve stimulation, shoulder joint ROM and stretching exercises, and ice applications. All patients received a total of 20 treatments, 5 days a week for 4 weeks. rESWT was applied once a week for 4 weeks in total. Before and after treatment, all patients were assessed for age, height, weight, body mass index (BMI), pain intensity with a visual analog scale, shoulder ROM, and functional disability status with the shortened version of the Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH). Mean BMI value of the participants was 26.1 kg/m2. Although all parameters of the patients in both groups improved significantly, patients in the rESWT group had a statistically significant improvement in pain, ROM, and QuickDASH scores (p < 0.001, p < 0.001, and p < 0.001, respectively). The conclusion was that rESWT was an effective and noninvasive method of reducing pain and increasing ROM and functional status without the need for surgery [44].
3.6 Conclusions
In most cases, calcific tendinopathy is a self-limited process, typically resolving within a few weeks or months. During this period, conservative treatment with nonsteroidal anti-inflammatory drugs, rehabilitation medicine, warm compresses, and possibly a corticosteroid injection into the subacromial bursa can be administered for symptomatic pain alleviation. About 10% of patients with calcific tendinopathy will have protracted symptoms that are refractory to conservative treatment. Even in this population of patients with calcific tendinopathy and failed conservative management, the prevalence of full-thickness tear remains low. Extracorporeal shockwave therapy and ultrasound-guided needle techniques are efficacious in alleviating pain and resolving the calcium deposits in chronic calcific tendinopathy of the rotator cuff that has failed initial conservative treatment. These treatments are minimally invasive and involve mostly minor complications of soreness, local bruising/ swelling, and subcutaneous hemorrhage, which occur in 10% of patients treated with ultrasound-guided needle techniques and 7%–19% of patients treated with extracorporeal shockwave therapy. Surgical removal of the calcium deposits of calcific tendinopathy is also efficacious in decreasing pain and improving function by using either arthroscopic or open techniques. However, surgery comes at greater cost, exposure to anesthesia and a longer recovery period compared with other less-invasive treatments. For these reasons, surgery should be reserved for patients who have protracted, activity-limiting pain and have failed initial conservative and minimally invasive treatments.
References
Chianca V, Albano D, Messina M, Midiri F, Mauri G, Aliprandi A, et al. Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta Biomed. 2018;89(Suppl 1):186–96.
Uhthoff HK, Sarkar K. Calcifying tendinitis. Baillière's. Clin Rheumatol. 1989;3:567–81.
Mole D, Gonzalvez M, Roche O, Scarlat M. Introduction to calcifying tendinitis. In: Gazielly DF, Gleyze P, Thomas T, editors. The cuff. Paris: Elsevier; 1997. p. 141–3.
Sconfienza LM, Albano D, Allen G, Bazzocchi A, Bignotti B, Chianca V, et al. Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur Radiol. 2018;28:5338–51.
Albano D, Chianca V, Zappia M, Russo R, Romano S, Sconfienza LM, et al. Imaging of usual and unusual complication of rotator cuff repair. J Comput Assist Tomogr. 2019;43:359–66.
Bellelli A, Silvestri E, Barile A, Albano D, Aliprandi A, Caudana R, et al. Position paper on magnetic resonance imaging protocols in the musculoskeletal system (excluding the spine) by the Italian College of Musculoskeletal Radiology. Radiol Med. 2019;124:522–38.
Albano D, Messina C, Sconfienza LM. Posterior shoulder instability: what to look for. Magn Reson Imaging Clin N Ame. 2020;28:211–21.
Hurt G, Baker CL Jr. Calcific tendinitis of the shoulder. Orthop Clin N Am. 2003;34:567–75.
Hsu CJ, Wang DY, Tseng KF, Fong YC, Hsu HC, Jim YF. Extracorporeal shock wave therapy for calcifying tendinitis of the shoulder. J Shoulder Elb Surg. 2008;17:55–9.
Silvestri E, Barile A, Albano D, Messina C, Orlandi D, Corazza A, et al. Interventional therapeutic procedures in the musculoskeletal system: an Italian survey by the Italian College of Musculoskeletal Radiology. Radiol Med. 2018;123:314–21.
Messina C, Sconfienza LM. Ultrasound-guided percutaneous irrigation of calcific tendinopathy. Semin Musculoskelet Radiol. 2016;20:409–13.
Albano D, Vicentin I, Messina C, Sconfienza LM. Post-surgical Achilles calcific tendinopathy treated with ultrasound guided percutaneous irrigation. Skelet Radiol. 2020;49:1475–80.
Serafini G, Sconfienza LM, Lacelli L, Silvestri E, Aliprandi A, Sardanelli F. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle US guided percutaneous treatment–nonrandomized controlled trial. Radiology. 2009;252:157–64.
Verstraelen FU, Fievez E, Janssen L, Morrenhof W. Surgery for calcifying tendinitis of the shoulder: a systematic review. World J Orthop. 2017;8:424–30.
Cho N, Lee SG, Kim JO, Kim YA, Kim EM, Park C, et al. Identification of differentially expressed genes associated with extracellular matrix degradation and inflammatory regulation in calcific tendinopathy using RNA sequencing. Calcif Tissue Int. 2020;107:489–98.
Albano D, Coppola A, Gitto S, Rapisarda S, Messina C, Sconfienza LM. Imaging of calcific tendinopathy around the shoulder: usual and unusual presentations and common pitfalls. Radiol Med. 2021;126:608–19.
Beckmann NM. Editorial commentary: is magnetic resonance imaging of the shoulder ever appropriate in evaluating patients with calcific tendinopathy of the rotator cuff? Arthroscopy. 2020;36:991–2.
Laucis NC, Rosen KA, Thodge A, Leschied JR, Klochko CL, Soliman SB. Sonographic evaluation of the association between calcific tendinopathy and rotator cuff tear: a case-controlled comparison. Clin Rheumatol. 2021;40:2897–905.
Beckman NM, Tran MQ, Cai C. Incidence of rotator cuff tears in the setting of calcific tendinopathy on MRI: a case controlled comparison. Skelet Radiol. 2019;48:245–50.
Albano D, Gambino A, Messina C, Chianca V, Gitto S, Faenza S, et al. Ultrasound-guided percutaneous irrigation of rotator cuff calcific tendinopathy (US-PICT): patient experience. BioMed Res Intl. 2020:3086395.
Lanza E, Piccoli F, Intrieri C, Muglia R, Politi LS, Borroni M, et al. US-guided percutaneous irrigation of calcific tendinopathy of the rotator cuff in patients with or without previous external shockwave therapy. Radiol Med. 2021;126:117–23.
Saba L, De Filippo M, Saba F, Fellini F, Marcy PY, Dagan R, et al. Efficacy of ultrasound-guided percutaneous treatment of the rotator cuff calcific tendinopathy with double needle technique. J Orthop. 2020;20:195–7.
Vassalou EE, Klontzas ME, Plagou AP, Karantanas AH. Ultrasound-guided percutaneous irrigation of calcific tendinopathy: redefining predictors of treatment outcome. Eur Radiol. 2021;31:2634–43.
Al-Kahir MAB, El Khouly RM, Khodair SA, Elsergany MAAS, Hussein MI, Mowafi MEE. Focused, radial and combined shock wave therapy in treatment of calcific shoulder tendinopathy. Phys Sportsmed. 2021;49:480–7.
Li C, Li Z, Shi L, Wang P, Gao F, Sun W. Effectiveness of focused shockwave therapy versus radial shockwave therapy for noncalcific rotator cuff tendinopathies: a randomized clinical trial. Biomed Res Int. 2021;2021:6687094.
Kim SJ, Yeo SM, Noh SJ, Ha CW, Lee BC, Lee HS, et al. Effect of platelet-rich plasma on the degenerative rotator cuff tendinopathy according to the compositions. J Orthop Surg Res. 2019;14:408.
Oudelaar BW, Veld RHI, Schepers-Bok R, Ooms EM, Nelissen RGHH, Vochteloo AJH. Prognostic factors for the outcome of needle aspiration of calcific deposits for rotator cuff calcific tendinitis. Eur Radiol. 2020;30:4082–90.
Catapano M, Zhang K, Mittal M, Sangha H, Onishi K, de Sa D. Effectiveness of dextrose prolotherapy for rotator cuff tendinopathy: a systematic review. PM R. 2020;12:288–300.
Darrieurtort-Laffite C, Bertrand-Vasseur A, Garraud T, Planche L, Le Goff B. Tolerance and effect of sodium thiosulfate in calcific tendinitis of the rotator cuff. Clin Rheumatol. 2020;39:561–9.
Bechay J, Lawrence C, Namdari S. Calcific tendinopathy of the rotator cuff: a review of operative versus nonoperative management. Phys Sportsmed. 2020;48:241–6.
Sansone V, Maiorano E, Galluzzo A, Pascale V. Calcific tendinopathy of the shoulder: clinical perspectives into the mechanisms, pathogenesis, and treatment. Orthop Res Rev. 2018;10:63–72.
Lam F, Bhatia D, van Rooyen K, et al. Modern management of calcifying tendinitis of the shoulder. Curr Orthop. 2006;20:446–52.
ElShewy MT. Calcific tendinitis of the rotator cuff. World J Orthop. 2016;7(1):55.
Ark JW, Flock TJ, Flatow EL, Bigliani LU. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy. 1992;8:183–8.
Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521–7.
Sabeti M, Schmidt M, Ziai P, Graf A, Nemecek E, Schueller-Weidekamm. C the intraoperative use of ultrasound facilitates significantly the arthroscopic debridement of calcific rotator cuff tendinitis. Arch Orthop Trauma Surg. 2014;134:651–6.
Clement N, Watts A, Phillips C, McBirnie JM. Short-term outcome after arthroscopic bursectomy debridement of rotator cuff calcific tendonopathy with and without subacromial decompression: a prospective randomized controlled trial. Arthroscopy. 2015;31:1680–7.
Rompe JD, Zoellner J, Nafe B. Shock wave therapy versus conventional surgery in the treatment of calcifying tendonitis of the shoulder. Clin Orthop Relat Res. 2001;387:72–82.
Rebuzzi E, Coletti N, Schiavetti S, Giusto F. Arthroscopy surgery versus shock wave therapy for chronic calcifying tendinitis of the shoulder. J Orthop Traumatol. 2008;9:179–85.
Jerosch J, Strauss JM, Schmiel S. Arthroscopic treatment of calcific tendonitis of the shoulder. Rev Cuba Ortop y Traumatol. 2017;31:118–30.
Porcellini G, Paladini P, Campi F, Paganelli M. Arthroscopic treatment of calcifying tendinitis of the shoulder : clinical and ultrasonographic follow-up findings at two to five years. J Shoulder Elb Surg. 2004;13:503–8.
Dedes V, Tzirogiannis K, Polikandrioti M, Dede AM, Nikolaidis C, Mitseas A, et al. Comparison of radial extracorporeal shockwave therapy versus ultrasound therapy in the treatment of rotator cuff tendinopathy. Folia Med. 2019;61:612–9.
Louwerens JKG, Sierevelt IN, Kramer ET, Boonstra R, van dem Bekerom MPJ, van Royen BJ, et al. Comparing ultrasound-guided needling combined with a subacromial corticosteroid injection versus high-energy extracorporeal shockwave therapy for calcific tendinitis of the rotator cuff: a randomized controlled trial. Arthroscopy. 2020:36:1823-33e1.
Duymaz T, Sindel D. Comparison of radial extracorporeal shock wave therapy and traditional physiotherapy in rotator cuff calcific tendinitis treatment. Arch Rheumatol. 2019;34:281–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rodríguez-Merchán, E.C., De la Corte-Rodríguez, H., Encinas-Ullán, C.A., Gómez-Cardero, P. (2022). Calcific Tendinopathy of the Rotator Cuff in Adults: Operative Versus Nonoperative Management. In: Rodríguez-Merchán, E.C., Moreno-Garcìa, A. (eds) Controversies in Orthopedic Surgery of The Upper Limb . Springer, Cham. https://doi.org/10.1007/978-3-031-04907-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-04907-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-04906-4
Online ISBN: 978-3-031-04907-1
eBook Packages: MedicineMedicine (R0)