Abstract
Recent advances in the field of peptide therapeutics have led to the design and synthesis of many promising peptides. However, research and development to provide safe, stable, efficacious, and patient compliant formulation plays a vital role in bringing peptide therapeutics to market. The conventional parenteral route has made scientific advances to overcome multiple barriers, leading to the approval of many peptide-based products via parenteral route of administration in recent years. In parallel, oral, pulmonary, transdermal, and other delivery routes have been extensively investigated to deliver peptides with improved patient compliance. This includes the use of novel strategies for developing delivery systems that can offer various advantages over conventional dosage forms. This chapter focuses on fundamentals, formulations, and recent advances for successful peptide delivery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Peptides
- Pharmaceutical market
- Formulation development
- Delivery systems
- Parenteral
- Oral
- Pulmonary
- Transdermal
- Controlled release parenteral
- Carrier systems
5.1 Introduction
Peptides and polypeptides are small-sized compounds (fewer than 50 amino acids) and a separate category of drugs positioned between small organic molecules and large proteins (Lau and Dunn 2018). Peptides offer several advantages such as better efficiency, specificity, and selectivity as compared to small molecules and are more economical and less immunogenic as compared to large proteins (D’Hondt et al. 2014). Peptides of natural and synthetic origin have been involved in various biological roles such as hormones, enzyme substrate, antibiotics, regulators, and inhibitors (Tesauro et al. 2019). Recent years have witnessed the authorization of over 25 peptides and oligonucleotide drugs (Al Musaimi et al. 2021). In 2020, the US Food and Drug Administration (FDA) had approved 53 new drug entities, 6 of which fall in the peptides and oligonucleotides category. This number is almost 10% of the total drug authorizations and reflects the consolidation of peptides in the market. Although peptides cover a wide spectrum of therapeutic areas, three major areas for peptide development include metabolic disease, cardiovascular disease, and oncology (Lau and Dunn 2018). These numbers reflect the potential interest in peptides (D’Hondt et al. 2014). The rise in scientific publications in the last decade related to peptide research indicates increased interest in this area of research which aligns with the current trend of marketed peptide therapeutics. However, the physical and chemical instability, enzymatic breakdown, and short half-life are the major barriers to the use of peptides (Sachdeva et al. 2016). Various routes and newer delivery systems have thus been explored for therapeutic peptide delivery. While the most preferred and traditional parenteral route of administration overcomes some of these challenges, other routes of administration namely oral, pulmonary, transdermal are widely researched and investigated for safe and efficient delivery of peptide therapeutics (Fig. 5.1). This chapter focuses on different routes of administration for peptide therapeutics, formulation development, examples of marketed formulations, and recent advances in the field of peptide delivery such as new drug delivery systems and technologies investigated.
5.2 Peptide Therapeutics Administered via Parenteral Route
In the past few decades, tremendous advances have been made in bringing peptide therapeutics to the market. Despite efforts put into other routes of administration, the parenteral route remains the primary and most promising route for the administration of peptides. However, their delivery can be challenging due to factors such as susceptibility to denaturation, degradation by enzymes, and short half-life, ultimately leading to poor bioavailability (Banga 2005; Agarwal and Rupenthal 2013). Parenteral route of drug administration refers to injection directly into the body, which bypasses the skin and mucous membranes, and common routes of parenteral administration are intramuscular, subcutaneous, and intravenous.
The intramuscular route refers to the administration of medication deep into the muscles. Most of the vaccines, like flu shots, are administered via the intramuscular route. Interferon alfa-2b to treat hairy cell leukemia, malignant melanoma is commonly administered via the intramuscular route. Plenaxis (abarelix), a product by Praecis Pharmaceuticals, which is an injectable gonadotropin-releasing hormone antagonist, approved by the FDA in 2003 is administered via intramuscular route (https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021567s026lbl.pdf).
The subcutaneous route refers to the administration of drug using a short needle into the tissue layers between the skin and the muscle. Absorption from the subcutaneous route is usually slower than intravenous route. This route also permits self-administration, thus freeing up the healthcare practitioners’ time for other issues beyond administration (Banga 2005; Ibeanu et al. 2020). Insulin, the first polypeptide to be administered therapeutically, is given via the subcutaneous route. Adipose tissue peptide, leptin to treat obesity, octreotide to treat acromegaly, and peptide neurotrophic factors such as nerve growth factor (NGF) used in the therapy of neurodegenerative disorders are some examples of peptides or polypeptides commonly administered via the subcutaneous routes. Imcivree™ (Setmelanotide), a product by Molina Healthcare for use as anti-obesity medication and delivered via subcutaneous route, was approved by the FDA in 2020.
The intravenous route facilitates the administration of drug directly into the systemic circulation. A number of approved and under clinical trial peptides via intravenous routes have increased exponentially in recent years (Asfour 2021). For example, Parsabiv (Etelcalcetide) is a product currently owned by Amgen and Ono Pharmaceuticals and was approved by FDA in 2017 for chronic idiopathic hyperparathyroidism and is administered via the intravenous route. Another recently FDA-approved product via intravenous route is Polivy® (polatuzumab vedotin-piiq), a product by Genentech Inc., indicated to treat relapsed or refractory diffuse large B-cell lymphoma. Padcev® (enfortumab vedotin-ejfv) was also approved by FDA in 2019 for adult patients with locally advanced or metastatic urothelial cancer and is administered via the intravenous route.
In order to improve stability, prolong delivery, and decrease clearance of biologics after intravenous administration, chemical modifications such as PEGylation, hyperglycosylation, mannosylation, stapled peptides, and colloidal carriers (liposomes, microspheres, and nanoparticles) are widely explored strategies. PEGylation can be used as a strategy to alter properties such as molecular weight, solubility, and steric hindrance. Thus, it leads to improved stability and pharmacokinetic activity of peptides. Oncaspar® (pegaspargase) is an FDA-approved product with L-asparaginase (Lasparagine amidohydrolase) covalently conjugated to monomethoxypolyethylene glycol (mPEG). It is indicated as a component of a multiagent chemotherapeutic regimen and is administered via the intravenous route. Hyperglycosylation refers to a co- or post-translational enzymatic process that conjugates proteins, lipids, or other organic molecules with polysaccharides to form a glycoconjugate. This technique has been explored for peptide delivery via intravenous route and offers advantages such as prolonged systemic circulation and reduced immunogenicity (Patel et al. 2014). Mannosylation refers to mannose receptor-targeted delivery of proteins and peptides by conjugation with mannose to achieve improved pharmacokinetic and pharmacological properties (Patel et al. 2014). Other technologies such as staples peptides have been developed to bypass the intrinsic problems related to peptides and to enhance their pharmacological performance. Stapled peptides are short peptides that are constrained in their alpha helical conformation by a synthetic brace, also called “staples.” They allow targeting the peptides inside the cells with high selectivity and efficiency (Moiola et al. 2019). ALRN-6924 is a stabilized cell-permeating peptide designed by Aileron Therapeutics, Inc. to disrupt the interaction between the p53 tumor suppressor protein and its predominant endogenous inhibitors. As of July 2020, ALRN-6924 is in Phase 2a clinical trial study that evaluates the antitumor effects in patients with advanced solid tumors or lymphomas (Kim and Jacobsen 2020). These technologies may thus play a pivotal role in the future of peptide therapeutics in the pharmaceutical field. Several delivery issues exist for peptide products, such as instability during storage and processing, instability in biological fluids, and poor intracellular delivery (Swaminathan and Ehrhardt 2012). Carrier systems such as liposomes, microspheres, and nanoparticles are some of the approaches to overcome these challenges in peptide delivery by conventional intravenous therapy. Liposomes are vesicles composed of one or more phospholipid bilayers with an aqueous internal cavity. Liposomes can encapsulate hydrophilic as well lipophilic components and hence have multiple applications as drug delivery systems. They can be formulated to be of different sizes, compositions, charge, and lamellarity (Bulbake et al. 2017). Microspheres can be used as depot systems for controlled and localized delivery of therapeutic peptides. Microspheres-based delivery systems are commonly fabricated by three methods: polymerization, emulsion-solvent extraction evaporation, and extrusion (Ramteke et al. 2012). There have been recent advances in the use of polymeric microspheres for the delivery of single-shot vaccines, plasmid DNA, and therapeutic peptides (Ramteke et al. 2012). Nanoparticles are microscopic particles with at least one dimension smaller than 100 nm. Nanoparticulate delivery systems have gained attention in delivering pharmaceutical actives in recent years.
Various products based on these controlled release technologies have been approved by FDA for parenteral administration of peptides. Lupron Depot® (TAP Pharmaceuticals) is a biodegradable, biocompatible polymeric microspheres-based product indicated for targeted and localized delivery of leuprolide acetate (a synthetic nonapeptide) to treat the symptoms of advanced prostate cancer, endometriosis, and uterine leiomyomata. Signifor Lar® (Novartis) is another product approved by the FDA in 2014 for pasireotide pamoate in PLGA microspheres for intravenous administration to treat acromegaly and Cushing’s disease. Bydureon Bcise® (Exenatide) is an extended-release injectable suspension from AstraZeneca indicated to improve blood sugar control in adults with type 2 diabetes.
5.3 Peptide Therapeutics Administered via Oral Route
Peptides are typically administered through the parenteral route because of their poor bioavailability orally. While each route has its advantages and disadvantages, the oral route of administration is often the most preferred route of drug administration due to factors such as noninvasive, painless delivery, lower manufacturing cost, and high patient compliance (Drucker 2020). Glucagon-like peptide-1 (GLP-1) is an intestinal hormone that exerts profound effects in the regulation of glycemia, stimulating glucose-dependent insulin secretion, and various other pathways (Lim and Brubaker 2006). The FDA recently approved Rybelsus (Semaglutide) oral tablets to improve blood sugar control in adult patients with type 2 diabetes. This is the first GLP-1 product approved for oral use and is a landmark in peptide delivery by oral administration (Drucker 2020; Fda 2019). Research has been done for delivering other peptides such as calcitonin, insulin, human growth hormone, parathyroid hormone, and many other peptide therapeutics via the oral route (Liu and Dinh 2011). Trulance™ (Plecanatide), developed by Synergy Pharmaceuticals, is another peptide product that received FDA and global approval in 2017 for chronic idiopathic constipation and is administered via oral route (Al-Salama and Syed 2017).
Orally administered peptides follow the same route as ingested food and hence undergo extensive degradation and metabolism and have to cross other barriers before being absorbed into the bloodstream from the small intestine. Barriers in oral peptide delivery include enzymatic barriers of the digestive system, mucus and epithelial barriers of the intestine, paracellular transport, efflux pumps, and interindividual variability (Drucker 2020; Patel et al. 2014).
The gastric acid present in the stomach destabilizes and exposes the peptide bonds for enzymatic degradation in the small intestine. Various proteolytic enzymes such as pepsin, trypsin, and aminopeptidases in the stomach and small intestine promote the digestion of peptides to amino acids, thus complicating the delivery of peptides via oral route (Dan et al. 2020; Brown et al. 2020). Various factors such as molecular weight, structural flexibility, hydrophilicity, and a number of enzyme susceptible groups affect the extent of proteolysis in the peptide therapeutics. Primarily, the function of the gut epithelium is recognition and exclusion of any foreign substances such as viruses, bacteria, and other pathogens which makes the lining of the gastrointestinal tract poses an even greater challenge for the delivery of peptides (Dan et al. 2020). The gut epithelium consists of a single layer of columnar epithelial cells supported by the lamina propria and the muscularis mucosae layers. The mucus secreted by these intestinal goblet cells, which cover the mucosal surfaces, comprises water and mucins, which are high molecular weight and heavily glycosylated proteins. This mucus membrane effectively traps larger macromolecules and blocks their access to the underlying epithelial cells and thus another barrier to peptide absorption (Drucker 2020; Dan et al. 2020).
Paracellular transport refers to the movement of molecules through spaces between epithelial cells regulated by tight junctions by passive diffusion. The size and charge of peptides generally exclude them from paracellular transport. On the other hand, the transcellular pathway has a large surface area of the brush border membrane available for absorption. Hence, most oral drugs are absorbed passively via the transcellular pathway (Dan et al. 2020). Efflux pumps pose another significant barrier to peptide absorption (Bruno et al. 2013). These are proteins of the ATP-binding cassettes superfamily and present on mature epithelial cells and play a role in multidrug resistance in humans. These efflux pumps can pump the peptide back to the lumen of the gastrointestinal tract (Bruno et al. 2013). Interindividual variability refers to the differences in the physiology of the gastrointestinal tract between individuals, including factors like the extent of mucus, enzyme production and expression, gastrointestinal motility, and gastric emptying time (Drucker 2020). Lastly, even after the peptide drug is absorbed, the first-pass metabolism in the gut and liver extensively reduces the fraction of the drug that reaches the systemic circulation (Bruno et al. 2013).
Multiple strategies have been pursued to overcome the barriers in the oral delivery of peptides. Zizzari et al. (2021) and Liu et al. (2011) have reviewed and highlighted many promising attempts to improve the oral bioavailability of peptides. Multiple oral delivery products of insulin, calcitonin, and parathyroid hormone which are in clinical development and are based on various strategies to enhance oral bioavailability of peptides have been described in these reviews (Liu and Dinh 2011; Dan et al. 2020; Zizzari et al. 2021).
Chemical modifications of peptide drugs can alter their physiological properties and improve enzyme stability and membrane permeation and minimize immunogenicity (Liu and Dinh 2011; Shaji and Varkey 2012). Such modifications include alteration of amino acid side chains, alteration of carbohydrate moieties in glycoproteins, and conjugation to fatty acid and other lipophilic moieties to increase hydrophobicity and introduction of protective groups to prevent degradation (Dan et al. 2020). For example, the addition of alpha-lipoic acid and palmitoyl derivative moiety to insulin resulted in protection against digestion by trypsin (Hashimoto et al. 1989). Another example of structural modification is the modification by deaminating and substituting a protective group in vasopressin to produce desmopressin (Dan et al. 2020). Desmopressin (1-desamino-8-D-arginine vasopressin; DDAVP) developed by Ferring Pharmaceuticals is a synthetic analog of human hormone vasopressin. Desmopressin has greatly simplified the management of diabetes insipidus by offering ease of administration, safety, and tolerability (Kim et al. 2004).
Formulation additives can enhance peptide drug gastrointestinal absorption (Liu and Dinh 2011). The use of enzyme inhibitors resists degradation by enzymes in the gastrointestinal tract, while absorption enhancers improve membrane permeability. Protease inhibitors inhibit the enzymatic activity of the protease enzyme. The choice of protease inhibitors should depend on the amino acids in the peptide therapeutics since these inhibitors are sequence specific (Brown et al. 2020). Another approach to inhibit the enzymes is to alter the pH to inactivate the local digestive enzymes. For example, digestive enzymes such as trypsin, chymotrypsin, and elastase can be inactivated by a sufficient amount of pH lowering buffer that can lower the local pH of the intestine to below 4.5 (Liu and Dinh 2011; Shaji and Patole 2008). Absorption enhancers are components of the formulation that disrupt the intestinal barrier and aid the peptides in crossing the biological membrane and reaching systemic circulation (Shaji and Patole 2008). Numerous compounds such as surfactants, bile salts, chelating agents, fatty acids, alkanoylcholines, mucoadhesive polymers, acyl carnitine, lectins, and chitosans are used as absorption enhancers for peptide therapeutics (Bruno et al. 2013; Zizzari et al. 2021; Shaji and Patole 2008; Aungst 2000). Some chelating agents such as ethylenediaminetetraacetic acid (EDTA) and ethylene glycol tetraacetic acid (EGTA) can sequester metal ions to enhance the paracellular transport of peptides (Brown et al. 2020).
Strategies such as PEGylation and various formulation vehicles such as liposomes, nanoparticles, and microspheres discussed earlier for parenteral delivery have multiple applications in the oral delivery of peptides as well (Bruno et al. 2013; Fasano 1998; Cao et al. 2019). However, the renewal of the mucus layer due to periodic turnover every 4–6 hours can lead to the rapid clearing of entrapped particulate system. For example, BioOral system (BioSante Pharmaceuticals) is based on calcium phosphate-based nanotechnology (CAP) for facilitating vaccine delivery. CAP was observed as a safer adjuvant to improve the efficacy of vaccines as compared to other approved adjuvants (BioSante 2004; Dan et al. 2020). Insulin was formulated CAP-PEG-insulin-casein (CAPIC), to improve the oral bioavailability by protecting insulin against the low pH in stomach where casein encapsulates the insulin-PEG formulation and acts as an enteric coating. The use of CAP in cancer, infectious disease, autoimmune disease vaccines, malaria vaccine, and anthrax vaccine is investigated (BioSante 2004).
Hydrophilic mucoadhesive polymers (polyacrylates, cellulose, and chitosan) and thiolated polymers have also been used as peptide carrier systems (Bruno et al. 2013). Nanoemulsions are another type of carrier system specifically for oral peptide delivery. They are typically oil-in-water (o/w) or water-in-oil (w/o) emulsions with mean droplet diameters ranging from 50 to 1000 nm (Bruno et al. 2013). Another type of formulation in development are self-emulsifying drug delivery systems (SEDDS) that are composed of surfactants, lipids, and co-solvents. These systems have gained focus in recent years to improve oral delivery of peptides owing to their mechanism of forming emulsions and microemulsions when dispersed in GI fluids (Zizzari et al. 2021). Sandimmune/Neoral® (Cyclosporin A) by Novartis Pharma AG is an FDA-approved marketed SEDDS-based product to prevent transplant rejection and treat patients with severe rheumatoid arthritis (Zizzari et al. 2021).
Hydrogels have high water content and a cross-linked network of hydrophilic polymer yet insoluble in water and can also be tailored for site-specific sustained oral drug delivery (Bindu Sri et al. 2012; Peppas et al. 2004). Hydrogels are biocompatible and have a high drug loading. Poly (methyl methacrylic acid), alginates, and chitosans are commonly used polymers for formulating hydrogels (Brown et al. 2020). Mucoadhesive polymeric systems are another approach for delivering peptides. These delivery systems adhere to the mucin layer and increase residence time at drug absorption site, thus decreasing drug clearance rate from the absorption site (Shaji and Patole 2008). Examples of mucoadhesive polymers include semi-natural polymers such as xanthan gum, polyvinyl pyrrolidone, polyvinyl alcohol, and synthetic polymers such as polyacrylic acid-based polymers and cellulose derivatives (Shaji and Patole 2008). In conclusion, despite being extremely challenging, oral delivery of peptides evolved with newer technologies. It can be an alternate and a more patient-compliant route of peptide therapeutics administration.
5.4 Peptide Therapeutics Administered via Pulmonary Route
In recent years, pulmonary route due to its unique and versatile features (Smith 1997) including (1) large surface area of the respiratory tract and lungs allowing simultaneous exposure of drug, (2) increased blood flow with thinner alveolar epithelium, (3) lesser metabolic activity, and (4) no hepatic metabolism has become an alternate route for delivery of therapeutic peptides via noninvasive route. As opposed to the oral route of delivery, pulmonary route has shown better bioavailability for peptide therapeutics with providing both local and systemic effects. However, delivery of peptides via respiratory tract has its challenges (Kwok et al. 2011). Mucociliary clearance is the primary challenge as it is the mechanism by which foreign particles get restricted from entering the body. Besides, the geometry and morphology of the airway and the presence of pulmonary peptidases are the other challenges for absorption of peptides (Smith 1997; Banga 2011). With a better understanding of these challenges, various approaches have been tried to deliver therapeutic peptides with better efficiency and reproducibility while maintaining their stability. One major technology for pulmonary delivery of peptides is the use of aerosols that is via inhalation (Shoyele and Slowey 2006). Nebulizers, metered-dose inhalers (MDI), and dry powder inhalers (DPI) are the most popular inhaled formulations in the market. The drug inhaled from aerosol gets deposited by gravitational sedimentation, inertial impaction, and diffusion (Shoyele and Slowey 2006). The aerodynamic behavior of particles, breathing patterns, and airway anatomy affects the distribution and absorption of drugs in the lungs (Liang et al. 2020). Although aerosols are most popular for pulmonary delivery of peptides, newer formulation approaches such as liposomes and microparticulate systems have been investigated recently for controlled and targeted delivery of peptides (Wan et al. 2012).
Nebulizers are commonly used to deliver a large volume of dose for inhalation in the form of droplets. Depending on the mechanism of generation of droplets, nebulizers can be classified as (1) jet nebulizer which uses compressed air to produce droplets or (2) ultrasonic nebulizer in which a piezoelectric crystal below the liquid reservoir generates ultrasonic waves and leads to the creation of aerosol droplets. The creation of an air-water interface and repeated stress can lead to physical instability in jet nebulizers, whereas thermal stress can be an issue in the case of ultrasonic nebulizers (Banga 2005). Advances in nebulizer technologies led to the development of devices such as AERx (Aradigm, Hayward, CA) and Respimat (Boehringer, Germany), which are based on mechanical extrusion of liquid from unit dose, and more recent AeroDose (Aerogen Inc., Mountain View, CA) based on vibrating mesh technology which all are investigated for pulmonary delivery of peptides (Schuster et al. 1997; Perera et al. 2002; Cryan 2005). However, the only marketed formulation administered via jet nebulizer is Pulmozyme® containing dornase alfa to treat cystic fibrosis (Cryan 2005).
As the name suggests, MDIs are formulations containing the active substance and other excipients dissolved or suspended in a propellent system which, upon actuation, delivers a measured dose of drug in the form of aerosol spray. Advantages of MDI include their low cost, portability, dose reproducibility, and disposability (Shoyele and Slowey 2006). Propellants such as hydrofluroalkanes (HFA) have replaced chlorofluorocarbons (Banga 2005). HFA-based MDI was investigated to deliver a high dose of cyclosporine using ethanol as co-solvent (Myrdal et al. 2004). In MDI, the inert propellant vapor atmosphere and sealed container protect the active from oxidative degradation and microbiological contamination, but the stability of peptides in these propellants remains a challenge (Banga 2005; Shoyele and Slowey 2006). Thus, many MDIs are formulated as a suspension. There is reported use of nonionic soluble surfactants to create a uniform suspension using freeze-dried protein and surfactant particles to formulate MDIs (Kwok et al. 2011). Synthetic nonapeptide leuprolide acetate is reported to be formulated as MDI both as solution and suspensions (Adjei and Gupta 1994). Studies conducted with human subjects with these formulations showed a three–four fold increase in plasma concentration from suspension as compared to a solution.
DPI is a system inhaled as a cloud of fine particles, and they do not contain propellant (Shoyele and Slowey 2006). These can be single or multiple doses where the drug is preloaded or loaded in the form of hard capsule (e.g., Spinhaler from Fisons Pharmaceuticals, Rochester, NY) or foil blister discs (e.g., Diskhaler from GSK, RTP, NC). Thus, they are easy to operate and inexpensive and have an advantage over nebulizers and MDI for administration of peptides (Banga 2005). Newer devices such as Spiros (Dura Pharmaceuticals, San Diego, CA) and Nektar T-326/ TOBI®Podhaler (now owned by Novartis AG) use powder inhaler system which generates aerosol independent of inspiratory rate and volume, enhancing the efficiency of DPI for drug delivery (Cryan 2005). However, formulating a peptide as DPI faces other challenges, including powder flowability, dispersibility, and stability (Banga 2005). One of the advances made into overcoming these challenges is drying the protein to an amorphous glassy state which inhibits denaturation. While this technology takes care of biochemical stability, the hygroscopic nature of dried particles can lead to physical instability (Kwok et al. 2011). Other ways of producing dry powders of peptides include milling, spray drying, spray freeze-drying, and supercritical fluid (Cryan 2005). Caveolin scaffolding domain peptide was investigated recently for treating pulmonary fibrosis as DPI using excipient free jet milling (Zhang et al. 2020). Cetrorelix acetate (decapeptide) was also reported to be formulated as DPI to study the role of particle engineering in detail (Zijlstra et al. 2004). Previously marketed inhalable insulin Exubera by Pfizer was the first-in-class product manufactured using spray drying and was administered as DPI with low-dose powder filing technology. However, it was withdrawn from the market due to several other factors, including its price, low sales, bulky device, and lack of insurance reimbursement (Banga 2005).
Like parenteral and oral routes, other strategies researched for pulmonary delivery of peptides include liposomes and microparticulate system (Wan et al. 2012). Due to their ability to encapsulate peptides, reduced local irritation, and toxicity with possible sustained release, liposomes are widely explored (Cryan 2005). They can be formulated as a liquid to be used with a nebulizer or in the form of dry powder for DPI. As mentioned earlier, essential parameters for formulation include selection and composition of lipids used and their ratio, charge, and size, which can be modulated to control drug release. Pulmonary insulin delivery has been previously investigated via liposomal carriers where insulin absorption and retention was increased using liposomes (Liu et al. 1993). Other peptides investigated for liposomal pulmonary delivery include cyclosporine, interleukin-2, and enzyme catalase (Cryan 2005). Microspheres and large porous particles are different microparticulate delivery systems explored for pulmonary delivery of peptides due to their ability to be formulated as powder and better stability. Polylactic acid (PLA), polylactic-co-glycolic acid (PLGA), chitosan, dextran, and gelatin are some of the polymers used to fabricate the microparticles. Large porous particles have an aerodynamic diameter of less than 5 μm owing to their low density and hence can be used for deep lung delivery (Banga 2005).
Factors to be considered while developing a peptide-based formulation for pulmonary delivery include pH of the formulation, buffering agents used, solubility, osmolarity, and special excipients such as absorption enhancers, protease inhibitors, and surfactants (Kwok et al. 2011). All these factors affect the conformation, stability, and absorption of peptides from the lungs. Absorption enhancers such as oleic acid, polyoxyethylene oleyl ether, bile acids, bile salts, fatty acids, and surfactants are reported to enhance absorption of peptides (Banga 2005). The use of protease inhibitors is investigated mainly for delivery of proteins rather than peptides. In a study conducted using rat lung homogenate, bacitracin showed highest effectiveness among the various protease inhibitors (sodium glycocholate, soybean trypsin inhibitor, aprotinin, and bacitracin) tested for delivery of insulin (Shin et al. 1994). In another study, pulmonary transport of polypeptide arginine vasopressin was enhanced with use of protease inhibitors (Hiroshi et al. 1994). Another critical factor that needs to be considered for the formulation is the immunogenicity of the excipients used, where certain absorption enhancers and enzyme inhibitors can lead to immunogenic response (Kwok et al. 2011). Liposomes discussed earlier can help to encapsulate peptides, thus avoiding clearance triggered by the immunogenic response. The safety of excipients used in the formulation is of concern as only phosphatidylcholine is approved for inhalation as of now, whereas safety of other absorption enhancers remains to be tested (Cryan 2005).
5.5 Peptide Therapeutics Administered via Transdermal Route
Topical/transdermaldelivery of peptides has gained attention due to its advantages, which include (1) large surface area, (2) bypassing hepatic metabolism and minimizing enzymatic degradation, (3) ease of administration leading to better patient compliance, and (4) controlled and sustained delivery (Herwadkar and Banga 2011). Thus, transdermal route is one of the routes explored as an alternative to parenteral administration, especially for peptides. Stratum corneum, the outermost layer of skin, is a major barrier to diffusion of drugs. An ideal drug administered via skin passively is a moderately lipophilic (log P ~ 1–3) molecule with molecular weight <500 Da (Banga 2005). On the other hand, peptides are hydrophilic macromolecules, making passive delivery via the skin a challenge (Schuetz et al. 2005). Apart from permeation across skin, proteolytic enzymes in the skin are an enzymatic barrier to delivering peptides.
To overcome these challenges, various physical and chemical enhancement techniques are employed to enhance delivery of peptides into and across skin (Banga 2005). The physical enhancement techniques researched so far include microneedles, iontophoresis, electroporation, sonophoresis, laser ablation, thermal and radiofrequency ablation, jet injectors, and their combination. On the other hand, chemical enhancement technique uses various chemicals to alter permeation of molecules across skin.
Microneedles (MN) are micron-sized needles that create hydrophilic microchannels in the skin by offering a needle-free, pain-free mode of administration (Herwadkar and Banga 2011). This disruption of stratum corneum thus bypasses the major barrier for transdermal delivery enabling delivery of hydrophilic macromolecules such as peptides. Material of fabrication for microneedles, microneedle length, number of microneedles per unit area, microneedle structure/geometry, and type of application are among the critical factors determining successful delivery (Kirkby et al. 2020). Transdermal delivery of insulin via MN and the effect of MN lengths on delivery have been investigated (Zhou et al. 2010). Transdermal delivery of four hydrophilic peptides having different molecular weights was investigated using solid MN across porcine ear skin, and microneedles enhanced delivery of all four peptides (Zhang et al. 2014). Delivery of peptide salmon calcitonin via coated microneedles was found to be similar to subcutaneous administration in hairless rat models (Banga 2005). The ability to deliver hydrophobic autoantigen peptides has been demonstrated recently using coated microneedles (Zhao et al. 2017). Another study used dissolving MN to deliver monoclonal IgG (Mönkäre et al. 2015) and interferon-α-2b (Chen et al. 2016). Swelling hydrogel-forming microneedles are among the new type of microneedles investigated for delivery of insulin and protein-based drug bevacizumab (Courtenay et al. 2018). With many examples investigated so far, MN is a promising approach for delivery of peptides; however, its commercialization will depend on developments in large-scale manufacturing to ensure safety, stability, and regulatory compliance.
Iontophoresis is another technique that uses a physiologically acceptable amount of current to deliver molecules into and across skin. As opposed to other techniques, iontophoresis works on the drug rather than on skin layers, with electro-osmosis and electro-repulsion being the two driving forces to deliver molecules (Banga 2005; Bakshi et al. 2020). Factors that need to be considered for iontophoretic delivery of peptides include physicochemical properties of peptide (isoelectric point, charge at physiological pH), type, amount, and duration of current applied. Peptides with a high charge-to-mass ratio can be delivered more efficiently. Due to skin pH between 4 and 7, peptides with isoelectric point below 4 and above 7.4 are better suited for transdermal delivery (Herwadkar and Banga 2011). The effect of pH on delivery of peptide leuprolide was investigated, where a pH of 7.4 was found to be optimal for delivery (Kochhar and Imanidis 2004). In another study, iontophoresis enabled delivery of leuprolide in vivo in humans to achieve a response similar to subcutaneous injection (Meyer et al. 1990). Iontophoretic delivery of various peptides, including cyclosporine, angiotensin, octreotide, arginine vasopressin, nafarelin, luteinizing hormone-releasing hormone (LHRH), and thyrotropin-releasing hormone, has been investigated (Schuetz et al. 2005). While mild symptoms including redness and erythema associated with iontophoresis are well-tolerated, success of the available marketed iontophoretic device will determine development of iontophoretic delivery of peptides in the near future.
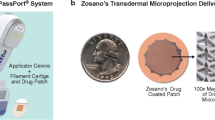
Laser ablation, thermal microporation, and radiofrequency-assisted ablation are different ablation technologies explored for drug delivery, including peptides (Benson and Namjoshi 2008). Laser ablation involves using a high laser beam that leads to water evaporation on the skin surface, thereby creating microchannels. These have been investigated for delivery of various macromolecules. For example, Nelson et al. observed a 2.1-fold increase in delivery of peptide INF-γ using an erbium-YSGG laser across porcine skin (Nelson et al. 1991). As the name suggests, thermal ablation uses heat for a short amount of time to create micropores. Delivery of interferon-α-2b using thermal ablation across hairless rats was found to be comparable to subcutaneous injection (Badkar et al. 2007). The use of the Passport™ system using thermal ablation to deliver insulin has also been reported (Benson and Namjoshi 2008). Similar to thermal ablation, radio frequency-assisted thermal ablation uses radiofrequency generated energy for ablation. The ViaDor™ system developed by Trans Pharma uses this technique to deliver drugs into and across skin which is tested for human growth hormone (Levin et al. 2005). For all the ablation technologies, safety and patient compliance remain to be tested for successful delivery system.
Other technologies to deliver peptides via transdermal route include jet injectors, electroporation, sonophoresis, and chemical enhancers. A jet injector is a velocity-based technology that uses a high velocity (>100 m/s) jet to penetrate skin. There are different jet injectors developed for liquid and powder formulations (Schuetz et al. 2005). Some of the jet injectors developed include Vitajet™, Medi-jector®, and Zomajet®, which are investigated for delivery of insulin, human growth hormone, and erythropoietin (Benson and Namjoshi 2008). Other dry powder formulation injector uses finer particles of drug in supersonic flow to penetrate the skin. Successful delivery of salmon calcitonin in vivo in rabbits was reported using PowderJect® device, which was further tested for insulin delivery in rats (Benson and Namjoshi 2008). The maximum dose that can be delivered using the jet injectors and stability of formulations are some of the barriers that limit the application of this technology for peptide delivery.
Electroporation uses high voltage pulses (60–1000 V) for a short duration (μ to ms) to create pores in lipid bilayer (Herwadkar and Banga 2011). Physiological properties of drug and formulation and the electrical parameters such as pulse rate, duration, and voltage affect peptide delivery. Peptide vaccine has been investigated for delivery using electroporation in mice (Zhao et al. 2006). Electroporation-assisted delivery of luteinizing hormone-releasing hormone has been reported in vitro across porcine skin in combination with iontophoresis, where increased delivery was observed with an increase in number of pulses of electroporation (Riviere et al. 1995). A combination of electroporation and iontophoresis was also used for delivery of salmon calcitonin (Chang et al. 2000) and human parathyroid hormone (Medi and Singh 2003). The nature of micropores (reversibility) and concern about damage to skin limit application of electroporation for peptide delivery.
Sonophoresis, as the name suggests, uses ultrasonic perturbation to drive molecules into and across skin. It employs piezoelectric crystal, which produces acoustic waves. The resulting acoustic cavitation is believed to play a major role in enhancing drug delivery (Dragicevic and Maibach 2017). The ultrasonic frequency, duration of application, intensity, and pulse length are the parameters that need to be optimized for achieving target delivery. A low frequency is preferred for permeation enhancement. A study was conducted to deliver cyclosporin A using sonophoresis alone and in combination with electroporation and chemical enhancers. It was observed that the skin delivery of cyclosporin was enhanced with sonophoresis alone and in combination with chemical enhancers as compared to passive diffusion. However, a significant enhancement in systemic delivery was observed only when electroporation was combined with sonophoresis and chemical enhancers (Liu et al. 2006). For sonophoresis-assisted delivery of insulin, the effect of intensity, duration, and threshold energy to increase permeation has been tested in several studies (Dragicevic and Maibach 2017). Other peptides and proteins explored for delivery using this technology include vasopressin, interferon- γ, and erythropoietin. Although various devices such as SonoDerm™ Technology and Sonoprep® were developed, heavy and oversized instrumentation and flexibility limit the use of sonophoresis in transdermal delivery (Benson and Namjoshi 2008).
The use of chemical enhancers is another strategy traditionally used to deliver small molecules, and it is also utilized to deliver peptides transdermally. These chemicals, when applied, change the permeability of skin either by increasing solubility of drug or chemical enhancer in lipid layer or by disrupting the barrier of skin. Polyalcohols, esters, fatty acids, pyrrolidones, sulfoxides, amines, amides, surfactants, and phospholipids are various chemical enhancers that can be used to enhance transdermal delivery of peptides (Herwadkar and Banga 2011). For example, ethanol alone and combined with cineole is reported to enhance the delivery of thyrotropin-releasing hormone analog (M-TRH) across human epidermal membrane (Magnusson and Runn 1999). Another strategy is the use of synthetic peptides to be administrated along with large protein molecules. For example, a short synthetic peptide was found to enhance permeation of insulin and human growth hormone (Chen et al. 2006). Although chemical enhancers are well known for enhancement, their use for enhancing delivery of hydrophilic molecules such as peptides is limited.
Formulation approaches for transdermal delivery of peptides include encapsulation technologies, use of protease inhibitors, and prodrug/chemical modification. The encapsulation technology uses a carrier system to deliver peptide transdermally, whereas use of protease inhibitors is the same as mentioned earlier. In the prodrug approach, hydrophilic peptide molecules are modified by conjugating it with lipid moiety or by derivatization, enabling delivery via skin. For example, a 2.5–5-fold increase in delivery of INF-α was observed when converted to acyl derivative for in vitro permeation across human skin (Foldvari et al. 1999). Similarly, delivery of insulin and thyrotropin hormone was also tested with fatty acid derivative (Herwadkar and Banga 2011). As this approach leads to creation of a new chemical entity, additional testing might be required from a regulatory perspective. Other novel and emerging technologies yet to be explored for transdermal delivery of peptides are photochemical waves, heat-assisted drug delivery, microscissioning, and ionic liquids (Schuetz et al. 2005).
5.6 Peptide Therapeutics Administered via Other Routes
Other routes for administration of peptides include nasal, rectal, vaginal, and buccal routes. The nasal route for peptide administration offers advantages such as rapid absorption, bypassing presystemic clearance, and ease of administration. Two approaches are commonly used for nasal delivery of peptides, namely, use of absorption enhancers to modify the permeability of the nasal membrane and use of mucoadhesive systems to decrease mucociliary clearance, and thereby increase the contact time at the site of absorption (Jitendra et al. 2011). Another potential route for administering peptide therapeutics is via the rectum. The lower part of the rectum is connected directly to systemic circulation, which also offers an opportunity to enter directly into the systemic circulation. In addition, it has many lymphatic vessels and thus can be a target to the lymphatic system route (Sanders 1990). Vaginal route can also be a favorable alternative for systemic drug delivery due to rich blood supply and large surface area of the vagina. Research has been conducted to deliver peptides such as calcitonin, human growth hormone, oxytocin, and insulin via the vaginal route (Jitendra et al. 2011). However, factors such as cultural sensitivity, personal hygiene, local irritation, and gender specificity can limit the vaginal route of administration of peptide therapeutics (Jitendra et al. 2011). Finally, the buccal route of administration is known to be an alternative to the conventional oral route, wherein the formulation can stick to the buccal mucosa and maintain a prolonged contact due to the mucoadhesive polymers. The formulation for delivery via buccal route also contains additives such as penetration enhancers to improve peptide permeation across buccal mucosa and enzyme inhibitors to protect the peptides from mucosal enzymes (Jitendra et al. 2011).
5.7 Summary
-
Parenteral Route: Primary and most promising with choice of IV/IM/SC administration but faces challenges including stability, short half-life, and poor bioavailability for peptide delivery. Various formulation approaches including chemical modifications and colloidal carriers have been explored for successful delivery with products in market.
-
Oral Route: Noninvasive and highly patient compliant route of administration. However, enzymatic degradation in GI tract along with other factors leads to poor bioavailability of peptides. Chemical modification and use of enzyme inhibitors and absorption enhancers along with several other approaches such as mucoadhesive and carrier systems have been utilized for therapeutic peptide delivery.
-
Pulmonary Route: A noninvasive route providing both local and systemic effects, with improved bioavailability compared to oral administration. Morphology and geometry of airway, mucociliary clearance, and immunogenicity limits peptide delivery. Various microparticulate systems and liposomes have been explored with strategic use of absorption enhancers and protease inhibitors for enhanced peptide delivery via aerosolized systems.
-
Transdermal Route: Another noninvasive route which can provide sustained and controlled delivery. However, permeation of hydrophilic peptides across skin is a major challenge. Various physical enhancement techniques such as microneedles, iontophoresis, and sonophoresis, encapsulation technologies, and chemical modifications have been explored for therapeutic peptide delivery.
-
Future Aspects: Extensive research and technological advances in various routes of administration have shown promising results, and this may broaden the reach of peptide therapeutics in the future.
References
Adjei A, Gupta P. Pulmonary delivery of therapeutic peptides and proteins. J Control Release. 1994;29:361–73.
Agarwal P, Rupenthal ID. Injectable implants for the sustained release of protein and peptide drugs. Drug Discov Today. 2013;18:337–49.
Al Musaimi O, Al Shaer D, Albericio F, de la Torre BG. 2020 FDA TIDES (peptides and oligonucleotides) harvest. Pharmaceuticals. 2021;14:1–14.
Al-Salama ZT, Syed YY. Plecanatide: first global approval. Drugs. 2017;77:593–8.
Asfour MH. Advanced trends in protein and peptide drug delivery: a special emphasis on aquasomes and microneedles techniques. Drug Deliv Transl Res. 2021;11:1–23.
Aungst BJ. Intestinal permeation enhancers. J Pharm Sci. 2000;89:P429–42.
Badkar AV, Smith AM, Eppstein JA, Banga AK. Transdermal delivery of interferon alpha-2b using microporation and iontophoresis in hairless rats. Pharm Res. 2007;24:1389–95.
Bakshi P, Vora D, Hemmady K, Banga AK. Iontophoretic skin delivery systems: success and failures. Int J Pharm. 2020;586:119584.
Banga AK. Therapeutic peptides and proteins formulation, processing, and delivery systems. Boca Raton: CRC Press; 2005.
Banga AK. Transdermal and intradermal delivery of therapeutic agents: application of physical technologies, vol. 38. Boca Raton: CRC Press; 2011. p. 1–282.
Benson HAE, Namjoshi S. Proteins and peptides: strategies for delivery to and across the skin. J Pharm Sci. 2008;97:3591–610.
Bindu Sri M, Ashok V, Arkendu C. As a review on hydrogels as drug delivery in the pharmaceutical field. Int J Pharm Chem Sci. 2012;1:642–61.
BioSante. CAP nanotechnology product development – new product. February 5, 2004.
Brown TD, Whitehead KA, Mitragotri S. Materials for oral delivery of proteins and peptides. Nat Rev Mater. 2020;5:127–48.
Bruno BJ, Miller GD, Lim CS. Basics and recent advances in peptide and protein drug delivery. Ther Deliv. 2013;4:1443–67.
Bulbake U, Doppalapudi S, Kommineni N, Khan W. Liposomal formulations in clinical use: an updated review. Pharmaceutics. 2017;9:1–33.
Cao SJ, Xu S, Wang HM, Ling Y, Dong J, Xia RD, Sun XH. Nanoparticles: oral delivery for protein and peptide drugs. AAPS PharmSciTech. 2019;20:1–11.
Chang SL, Hofmann GA, Zhang L, Deftos LJ, Banga AK. The effect of electroporation on iontophoretic transdermal delivery of calcium regulating hormones. J Control Release. 2000;66:127–33.
Chen Y, Shen Y, Guo X, Zhang C, Yang W, Ma M, Liu S, Zhang M, Wen LP. Transdermal protein delivery by a coadministered peptide identified via phage display. Nat Biotechnol. 2006;24:455–60.
Chen J, Qiu Y, Zhang S, Gao Y. Dissolving microneedle-based intradermal delivery of interferon-ɑ-2b. Drug Dev Ind Pharm. 2016;42:890–6.
Courtenay AJ, McCrudden MTC, McAvoy KJ, McCarthy HO, Donnelly RF. Microneedle-mediated transdermal delivery of bevacizumab. Mol Pharm. 2018;15:3545–56.
Cryan SA. Carrier-based strategies for targeting protein and peptide drugs to the lungs. AAPS J. 2005;7:E20–41.
D’Hondt M, Bracke N, Taevernier L, Gevaert B, Verbeke F, Wynendaele E, De Spiegeleer B. Related impurities in peptide medicines. J Pharm Biomed Anal. 2014;101:2–30.
Dan N, Samanta K, Almoazen H. An update on pharmaceutical strategies for Oral delivery of therapeutic peptides and proteins in adults and pediatrics. Children. 2020;7:307.
Dragicevic N, Maibach HI. Percutaneous penetration enhancers physical methods in penetration enhancement. Berlin Heidelberg: Springer; 2017;1:1–508.
Drucker DJ. Advances in oral peptide therapeutics. Nat Rev Drug Discov. 2020;19:277–89.
Fasano A. Innovative strategies for the oral delivery of drugs and peptides. Trends Biotechnol. 1998;16:152–7.
FDA. FDA approves first oral GLP-1 treatment for type 2 diabetes inquiries. FDA News Release. 2–4;2019.
Foldvari M, Baca-Estrada ME, He Z, Hu J, Attah-Poku S, King M. Dermal and transdermal delivery of protein pharmaceuticals: lipid-based delivery systems for interferon alpha. Biotechnol Appl Biochem. 1999;30:129–37.
Hashimoto M, Takada K, Kiso Y, Muranishi S. Synthesis of palmitoyl derivatives of insulin and their biological activities. Pharm Res. 1989;6:171–6.
Herwadkar, Anushree, and Ajay K. Banga. 2011. Transdermal delivery of peptides and proteins (Elsevier).
Hiroshi Y, Morimoto K, Lee VHL, Kwang-Jin K. Effect of protease inhibitors on vasopressin transport across rat alveolar epithelial cell monolayers. Pharm Res. 1994;11:1617–22.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021567s026lbl.pdf.
Ibeanu N, Egbu R, Onyekuru L, Javaheri H, Khaw PT, Williams GR, Brocchini S, Awwad S. Injectables and depots to prolong drug action of proteins and peptides. Pharmaceutics. 2020;12:1–42.
Jitendra PK, Sharma SB, Banik A. Noninvasive routes of proteins and peptides drug delivery. Indian J Pharm Sci. 2011;73:367–75.
Kim A, Jacobsen E. Anaplastic large cell lymphoma. In: Novel therapeutics for rare lymphomas. Cham: Springer; 2020.
Kim RJ, Malattia C, Allen M, Moshang T Jr, Maghnie M. Vasopressin and desmopressin in central diabetes insipidus: adverse effects and clinical considerations. Pediatr Endocrinol Rev. 2004;2:115–23.
Kirkby M, Hutton ARJ, Donnelly RF. Microneedle mediated transdermal delivery of protein, peptide and antibody based therapeutics: current status and future considerations. Pharm Res. 2020;37:1–18.
Kochhar C, Imanidis G. In vitro transdermal iontophoretic delivery of leuprolide under constant current application. J Control Release. 2004;98:25–35.
Kwok L, Chi P, Chan HK. Pulmonary delivery of peptides and proteins. Elsevier; Amsterdam, 2011.
Lau JL, Dunn MK. Therapeutic peptides: historical perspectives, current development trends, and future directions. Bioorg Med Chem. 2018;26:2700–7.
Levin G, Gershonowitz A, Sacks H, Stern M, Sherman A, Rudaev S, Zivin I, Phillip M. Transdermal delivery of human growth hormone through RF-microchannels. Pharm Res. 2005;22:550–5.
Liang W, Pan HW, Vllasaliu D, Lam JKW. Pulmonary delivery of biological drugs. Pharmaceutics. 2020;12:1–28.
Lim GE, Brubaker PL. Glucagon-like peptide 1 secretion by the L-cell: the view from within. Diabetes. 2006;55:S70–7.
Liu P, Dinh S. Oral delivery of protein/peptide therapeutics. In: Oral bioavailability: basic principles, advanced concepts, and applications. Hoboken: Wiley; 2011. p. 371–80.
Liu FY, Shao Z, Kildsig DO, Mitra AK. Pulmonary delivery of free and liposomal insulin. Pharm Res. 1993;10(2):228–32.
Liu H, Li S, Pan W, Wang Y, Han F, Yao H. Investigation into the potential of low-frequency ultrasound facilitated topical delivery of Cyclosporin A. Int J Pharm. 2006;326:32–8.
Magnusson BM, Runn P. Effect of penetration enhancers on the permeation of the thyrotropin releasing hormone analogue pGlu-3-methyl-His-Pro amide through human epidermis. Int J Pharm. 1999;178:149–59.
Medi BM, Singh J. Electronically facilitated transdermal delivery of human parathyroid hormone (1-34). Int J Pharm. 2003;263:25–33.
Meyer BR, Kreis W, Eschbach J, O'Mara V, Rosen S, Sibalis D. Transdermal versus subcutaneous leuprolide: a comparison of acute pharmacodynamic effect. Clin Pharmacol Ther. 1990;48:340–5.
Moiola M, Memeo MG, Quadrelli P. Stapled peptides-a useful improvement for peptide-based drugs. Molecules. 2019;24:3654
Mönkäre J, Reza Nejadnik M, Baccouche K, Romeijn S, Jiskoot W, Bouwstra JA. IgG-loaded hyaluronan-based dissolving microneedles for intradermal protein delivery. J Control Release. 2015;218:53–62.
Myrdal PB, Karlage KL, Stein SW, Brown BA, Haynes A. Optimized dose delivery of the peptide cyclosporine using hydrofluoroalkane-based metered dose inhalers. J Pharm Sci. 2004;93:1054–61.
Nelson JS, McCullough JL, Wright GTC, Liaw LH, Wh JSL. Mid-infrared laser ablation of stratum corneum enhances in vitro percutaneous transport of drugs. J Invest Dermatol. 1991;97:874–9.
Patel A, Cholkar K, Mitra AK. Recent developments in protein and peptide parenteral delivery approaches. Ther Deliv. 2014;5:337–65.
Peppas NA, Wood KM, Blanchette JO. Hydrogels for oral delivery of therapeutic proteins. Expert Opin Biol Ther. 2004;4:881–7.
Perera AD, Kapitza C, Nosek L, Fishman RS, David a Shapiro, Tim Heise, and Lutz Heinemann. Absorption and metabolic effect of inhaled insulin. Diabetes Care. 2002;25:2276–81.
Ramteke KH, Jadhav VB, Dhole SN. Microspheres: as carrieres used for novel drug delivery system. IOSRPHR. 2012;2:44–8.
Riviere JE, Monteiro-Riviere NA, Rogers RA, Bommannan D, Tamada JA, Potts RO. Pulsatile transdermal delivery of LHRH using electroporation: drug delivery and skin toxicology. J Control Release. 1995;36:229–33.
Sachdeva S, Lobo S, Tarun G. What is the future of noninvasive routes for protein- and peptide-based drugs? Ther Deliv. 2016;7:355–7.
Sanders LM. Drug delivery systems and routes of administration of peptide and protein drugs. Eur J Drug Metab Pharmacokinet. 1990;15:95–102.
Schuetz YB, Naik A, Guy RH, Kalia YN. Emerging strategies for the transdermal delivery of peptide and protein drugs. Expert Opin Drug Deliv. 2005;2:533–48.
Schuster J, Rubsamen R, Lloyd P, Lloyd J. The AER(x)(TM) aerosol delivery system. Pharm Res. 1997;14:354–7.
Shaji J, Patole V. Protein and peptide drug delivery: Oral approaches. Indian J Pharm Sci. 2008;70:269–77.
Shaji J, Varkey D. Recent advances in physical approaches for transdermal penetration enhancement. Curr Drug Ther. 2012;7:184–97.
Shin Y-S, Mori T, Okita M, Gemma T, Kai C, Mikami T. NII-electronic library service. Chem Pharm Bull. 1994;17:1460–2.
Shoyele SA, Slowey A. Prospects of formulating proteins/peptides as aerosols for pulmonary drug delivery. Int J Pharm. 2006;314:1–8.
Smith PL. Peptide delivery via the pulmonary route: a valid approach to local and systemic delivery. J Control Release. 1997;46:99–106.
Swaminathan J, Ehrhardt C. Liposomal delivery of proteins and peptides. Expert Opin Drug Deliv. 2012;9:1489–503.
Tesauro D, Accardo A, Diaferia C, Milano V, Guillon J, Ronga L, Rossi F. Peptide-based drug-delivery systems in biotechnological applications: recent advances and perspectives. Molecules. 2019;24:1–27.
Wan F, Møller EH, Yang M, Jørgensen L. Formulation technologies to overcome unfavorable properties of peptides and proteins for pulmonary delivery. Drug Discov Today Technol. 2012;9:e141–e46.
Zhang S, Qiu Y, Gao Y. Enhanced delivery of hydrophilic peptides in vitro by transdermal microneedle pretreatment. Acta Pharm Sin B. 2014;4:100–4.
Zhang Y, Mackenzie B, Koleng JJ, Maier E, Warnken ZN, Williams RO. Development of an excipient-free peptide dry powder inhalation for the treatment of pulmonary fibrosis. Mol Pharm. 2020;17:632–44.
Zhao YL, Murthy SN, Manjili MH, Guan LJ, Sen A, Hui SW. Induction of cytotoxic T-lymphocytes by electroporation-enhanced needle-free skin immunization. Vaccine. 2006;24:1282–90.
Zhao X, Coulman SA, Hanna SJ, Susan Wong F, Dayan CM, Birchall JC. Formulation of hydrophobic peptides for skin delivery via coated microneedles. J Control Release. 2017;265:2–13.
Zhou CP, Liu YL, Wang HL, Zhang PX, Zhang JL. Transdermal delivery of insulin using microneedle rollers in vivo. Int J Pharm. 2010;392:127–33.
Zijlstra GS, Hinrichs WLJ, de Boer AH, Frijlink HW. The role of particle engineering in relation to formulation and de-agglomeration principle in the development of a dry powder formulation for inhalation of cetrorelix. Eur J Pharm Sci. 2004;23:139–49.
Zizzari AT, Pliatsika D, Gall FM, Fischer T, Riedl R. New perspectives in oral peptide delivery. Drug Discov Today. 2021;26:1097–105.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vora, D., Dandekar, A.A., Banga, A.K. (2022). Therapeutic Peptide Delivery: Fundamentals, Formulations, and Recent Advances. In: Jois, S.D. (eds) Peptide Therapeutics. AAPS Advances in the Pharmaceutical Sciences Series, vol 47. Springer, Cham. https://doi.org/10.1007/978-3-031-04544-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-04544-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-04543-1
Online ISBN: 978-3-031-04544-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)