Abstract
An overview of Centers for Medicare & Medicaid Services (CMS) alternative payment models and their quality metrics is provided. Review of applicable quality metrics and gates shows where concurrent review may be most effective. We briefly summarize our successful experience with quality metrics for the CMS Comprehensive Care for Joint Replacement program, as well as with Employers Centers of Excellence Network programs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- CMS
- Comprehensive Care for Joint Replacement
- bundle payments
- bundle quality metrics
- Employers Centers of Excellence Network
- commercial payer
- center of excellence
Increasingly, payer organizations are shifting the focus from payments for specific medical services to payment for episodes or bundles of care. This shift is intended to motivate provider organizations to adjust their care models for greater value generation. Value is defined as achievement of an outcome of care at a certain cost. For example, the Centers for Medicare & Medicaid Services (CMS) Comprehensive Care for Joint Replacement (CJR) program defines its incentives to hospitals by their ability to achieve certain cost targets based on a tier of quality measure performance. While there are other bundle payment arrangements, in this chapter, we focus on CMS bundles and the Employers Centers of Excellence Network (ECEN).
1 CMS Bundled Payment Programs
Cost pressure on federal payment systems from an aging population and escalating healthcare costs has led to the development of alternate payment models (APMs). Bundled payment care initiatives (BPCIs) and accountable care organizations (ACOs) are forms of APMs. BPCIs have been applied to total joint replacement, hip fracture, spine procedures, congestive heart failure, urinary tract infection, stroke, percutaneous coronary intervention, coronary artery bypass, chronic obstructive pulmonary disease, and other major conditions [1]. Participation is generally by choice, and hospitals must participate for 3 years with a possible extension period. Cost is bunded for each care episode, and participating organizations are eligible for payment or recoupment based on cost performance against a target price; payment is modified by quality gates.
In contrast, ACOs measure quality outcomes annually and require improved outcomes year over year for ACOs to be eligible for reconciliation payments [2]. ACOs follow several principles. They are provider-led organizations with strong primary care; an ACO is accountable for quality outcomes and per capita costs; payments are linked to improvement in quality and reduced costs; and ACOs have reliable measures of performance to support improvement and instill care team’s confidence. A common APM is a bundled reimbursement model such as the voluntary Bundled Payments for Care Improvement (BPCI) and the mandatory CJR initiatives. Implementation of these bundled payment models has generally resulted in cost savings and quality improvements [3]. Successful provider organizations have found ways to reduce the number and severity of poor-quality outcomes within their at-risk populations. Comorbid conditions such as diabetes and cardiac, cerebrovascular, and pulmonary diseases contribute to poor postoperative outcomes, so tight care coordination is necessary, both to avoid surgical complications and exacerbations and sequelae of comorbidities.
2 The Comprehensive Care for Joint Replacement Model [4]
With the aging of the US population and improvements in survival to advanced age, total joint replacement procedures are projected to increase steadily. In response, CMS has transitioned to APMs in many health service areas. This CMS innovation aims to support better and more efficient care for beneficiaries undergoing hip and knee replacement surgery. These procedures are the most common inpatient surgeries for Medicare beneficiaries. Payment is bundled and quality measured for a 90-day episode of care related to hip and knee replacements (MS-DRG 469 – major joint replacement or reattachment of lower extremity with major complications or comorbidities, or MS-DRG 470 – major joint replacement or reattachment of lower extremity without major complications or comorbidities). Hospitals, physician groups, and post-acute care providers are financially incentivized to collaborate. This is meant to improve the quality and care coordination starting with the hospitalization for surgery through 90 days postdischarge. Quality improvement was to be driven through care standardization because of known substantial variation, for example, in the rate of infections and implant failures, as well as overall cost. This payment model began on April 1, 2016; on January 1, 2021, more than 400 hospitals in 67 geographic areas of the United States were participating in the CJR model. Initially set to run for 5 years, the CJR program was recently extended for 3 years and now includes total joint replacement performed in an outpatient setting. Payments are made based on a participating hospital’s ability to achieve its target price for the episode of care, determined by regional pricing benchmarks and adjusted by a 3% discount. The latter is further adjusted at reconciliation based on composite quality score [5].
2.1 Quality Measures for the CMS CJR Program
CMS publishes hospitals’ quality outcomes from the CJR program on the Web [6]. Two quality measures included in the CJR model are complications and patient experience. The total hip and knee arthroplasty (THA/TKA) complication measure is endorsed by the National Quality Forum (NQF) as measure #1550. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey measure (NQF #0166) relates to patient experience. The THA/TKA complication measure includes only elective THA/TKA patients. It excludes fractures which are, however, included in the CJR model. This measure represents a risk-standardized complication rate for 90 days following THA/TKA surgery. The components of this measure include acute myocardial infarction (AMI), deep vein thrombosis (DVT), pulmonary embolism (PE), pneumonia , bleeding, and others (see Chapter “Risk-Adjusted Complications”). Case selection for concurrent review should take into account how bundled payment programs like CJR measure care quality. Many of the conditions measured also represent AHRQ PSIs or may be captured with other metrics addressing complications. Organizations participating in bundled programs should assess whether their existing process for concurrent review adequately captures this group of patients.
Key Concept
CMS alternative payment methods require certain quality and patient safety outcomes to be met for hospitals to realize the maximum payment for bundled care such as for total hip and knee replacement.
The patient experience measure for the CJR model uses the HCAHPS linear mean rollup (HLMR) score. The HLMR score describes performance in the publicly reported HCAHPS measures, excluding the pain management domain. The HLMR is the average of the mean scores of the HCAHPS measures, using a weight of 100% for each of the six composite HCAHPS measures and a weight of 50% for the cleanliness, quietness, overall hospital rating, and recommend-the-hospital measures.
The CJR model incentivizes the submission of THA/TKA patient-reported outcomes for eligible elective primary THA/TKA procedures but does not require these data for reconciliation payment eligibility. CJR participants who successfully submit patient-reported outcomes data can increase their financial opportunity; they receive points toward their composite quality score ranging from 0 to 20 points (10 for performance in complications, 8 for patient experience, and 2 for additional data reporting such as patient-reported metrics). Provider organizations are sorted into four quality categories along this spectrum: barely acceptable, acceptable, good, and excellent. Based on where organizations fall along this quality spectrum, their reconciliation payment (or repayment responsibility amount based on cost performance) will be reduced by a lesser or greater percentage. There is also a quality gate for organizations to be eligible for any reconciliation payments, meaning hospitals or groups that perform below a minimally acceptable quality standard are ineligible for incentive or reconciliation payments.
2.2 Experience with CJR at the Ochsner Health
Our experience with quality improvement through care standardization for major joint replacement began several years before CMS mandated CJR program participation in the New Orleans metropolitan statistical area. Through a collaboration of leaders from orthopedic surgery, anesthesia, perioperative pain management, case management, nursing, and physical therapy, the Ochsner Perioperative Surgical Home (PSH) model was initiated in 2014. Sustained success with this model of care pathway and algorithm set our total joint replacement program apart from others regionally and allowed for our program to become designated as a national center of excellence (COE).
The PSH model of care is a proven method of delivering perioperative value-based care. Clinical pathways and other care algorithms standardize care, while internal clinical benchmarking leads to continuous feedback and improvement [7]. PSH programs improve postoperative recovery and decrease hospital utilization by reducing hospital length of stay, utilization of opioids, and discharge to nonhome locations of care [8]. Through a collaborative approach, the PSH allows for programmatic, multidisciplinary participation in the periprocedural care for total joint patient populations [9]. A multidisciplinary team engages with the patient from the time of surgical decision to 90 days postoperatively. Care is given through standardized evidence-based protocols. Care pathways built into the electronic medical record (EMR) require documentation of adherence to each pathway step. Weekly reports are generated and team-reviewed for improvement opportunity.
Introducing the PSH model resulted in significant total cost savings, decreased hospital length of stay, and fewer readmissions within 30 days of discharge. Some of the components of PSH approach are not new. A randomized prospective study [10] demonstrated that a pathway-controlled physical therapy regimen led to enhanced recovery and reduction of adverse events in the post-acute phase when compared to a non-pathway regimen. In addition to standardizing physical therapy, the PSH model achieves superior outcomes through preoperative patient optimization and comorbidity management, standardized pain and anesthesia regimens, enhanced postoperative monitoring, standardized discharge orders, and increased coordination of care between hospital and community health providers.
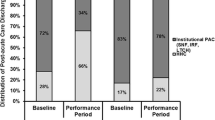
The PSH model of care was begun without fully integrating all its pathways into the EMR. Neither did EMR reporting capability exist initially. Even without these features, our teams were able to achieve remarkable (20–50%) improvements in cost, length of stay, home health discharge, and skilled nursing facility (SNF) utilization. PSH implementation reduced 30-day readmission rates from 4.3% to 1.9%. EMR integration did not significantly affect readmission rate [11, 12]. However, adding EMR integration to the PSH model further reduced certain costs and increased home discharge while decreasing reliance on SNF care [11]. EMR integration further increased home health discharge and decreased SNF discharge (Fig. 37.1). Our participation in the CMS CJR program has been successful. Our organization has been eligible for reconciliation payments year over year. For the most recent composite CJR quality scores, we achieved a ten of ten points level of performance [6].
3 Employers Center of Excellence Network
As employers experience significant health costs for their employees, they look to increase the value they realize for their investment. Such value derives from the avoidance of unnecessary healthcare utilization, with care outcomes that are unchanged or better than care received outside of the COE network. An example of such value generated is that COE patients avoided surgery 20% of the time after referral. When surgery was performed in the COE setting, COE care teams were able to avoid SNF-based post-acute care utilization [13]. Our own experience supports the ability of a care coordination and perioperative population management program to reduce such post-acute care utilization after total joint replacement [12]. Reports of provider organizations’ bundled arrangement experience with private payers exist [14]. The arrangements generally resulted in lower costs due to reduced utilization and improved quality from reductions in complications and readmissions.
Employers look for provider organizations that are an optimal fit with their culture and care philosophy for their employees. They seek highly reliable organizations to help solve for utilization, standardization, and cost of care while achieving the best possible patient experience and care outcomes. Employers find COE partners through convenors (also referred to as third-party administrators) such as the Health Design Plus. These third-party organizations conduct a thorough assessment on behalf of their employer’s clients. They look closely at publicly available cost and quality information about the organization and surgeons; a site visit is part of the due diligence to determine whether they recommend pursuing a COE partnership. A hospital cannot unilaterally apply to be an employer COE; if the hospital meets the criteria the employer sets, the third-party administrator invites the hospital to apply. Organizations desiring to establish employer COE partnerships need to be aware of the significant resources required for participation. Principally, such resources are necessary to assure success in what is essentially an arrangement where the provider organization takes risk for an episode of surgical or interventional care. An initial investment is required to apply for and stand up the program. The most resource-intensive ongoing activities under such programs are care navigation, care review, financial systems, continuous learning, and data analytics/reporting. For example, our financial systems needed rebuilding to allow service provision without authorization and billing. Our relationship as a Walmart’s COE has required the dedication of three patient and access navigators.
From the medical perspective, organizations should have experience in well-functioning processes and programs to coordinate perioperative care that can assure process reliability, harm avoidance, and avoidance of unnecessary utilization . This generally incudes a preoperative optimization process, care pathways hardwired into the EMR, and algorithms for tailored application of higher-level resources based on patient data (e.g., a surgical home program). Our group practice model organization facilitates the provision of cross-disciplinary services such as radiology, anesthesia, surgeons’ fees, and hospital charges that can all be furnished by the same provider entity, as well as patient-centered services such as hotel accommodation, outpatient therapy, durable medical equipment, and transportation.
Patients often travel from far away, including from other states. After discharge, they are housed in a hospital-affiliated hotel. They receive physical therapy in the hotel. If they have a minor medical or postsurgical issue, they can be seen in the hotel room for their convenience. Organizationally and administratively, COE programs require health system executive support, alignment of transportation, care management, appointment navigation, hospitality, medical equipment procurement, outpatient therapy (e.g., physical therapy services delivered in the hotel), concierge services, medical informatics, information technology, and finance teams.
3.1 Quality Metrics Monitored in ECEN Programs
The quality indicators monitored and reported by employer networks generally encompass a 30-day period after the procedure. They include 30-day mortality and readmissions, PE, DVT, surgical site infection (SSI), surgical site bleeding, wound dehiscence, and unplanned return to operating room (ROR) [15]. Hospital length of stay is also reported as part of the ECEN quality dashboard, as is AMI, pneumonia, or sepsis within 7 days, unplanned medical management after discharge, and completion of total joint-related patient questionnaires documenting functional outcomes.
Key Concept
To be chosen as a national center of excellence by major employers, hospitals must meet network care philosophy, volume, and quality criteria. Quality metrics include complications and process metrics. Systems for reporting and concurrent review need to be set up or adjusted to account for these requirements.
3.2 Experience with ECEN at the Ochsner Health
Adoption of the PSH at our hospitals, with systemwide adoption of hardwired care pathways in the EMR, set the stage for successful entry into the ECEN. To date, surgical patients referred to Ochsner as part of the ECEN designation include those considered for hip replacement, knee replacement, spine surgery, and bariatric surgery.
Our experience is most comprehensive with joint replacement surgery. Among the 11 health systems for which quality data were most recently available, Ochsner had complication rates of PE, DVT, SSI, wound dehiscence, and ROR, which were below the group means of the participating centers. Readmission rates were near the mean but improved substantially year over year.
Our journey toward a bariatric ECEN contract arrangement entailed a multistep process. We were initially approached with a high-level data request to assess our group’s fit for the network program. The information requested comprised of our bariatric center’s volumes, accreditation status, and patient outcomes. Patient outcome data sought by ECEN surrogates included readmission rates, length of stay, and infection rates. Once these data were found acceptable, we were able to move to the next step which involved a more formal application and telephone interview. The full application included more detailed information about the Ochsner bariatric program and our institution. In particular, detail was sought regarding safety culture and performance within the hospital and within the division of bariatrics. The application also included questions about our EMR and its adaptability to facilitate the network program for bariatric referral. Our application acceptance prompted an onsite visit. Once full approval to proceed was obtained, program details were worked out, including data sharing and payment arrangements. Moving forward, we have planned yearly safety and quality evaluations using data from our previous year. This process compares our data to that of the other participating centers. Our continued participation in the program is dependent on these quality outcomes, which include minimum case activity for the facility and each surgeon.
4 Summary and Future Considerations
Population management has become a strategic priority at the Ochsner Health. The group practice model, aided by health system information technology and care coordination resources, has been able to support a substantial entry into perioperative population management. Our experience has been that perioperative patient engagement through preoperative classes for patients and family, reinforcement during preoperative visits, and intentionally timed postoperative contacts have all contributed materially to improved outcomes, patient experience, and efficiency of care. A system for accurate medical record documentation and quality metric reporting, augmented by our concurrent review process, is key to successful participation in bundled care arrangements. Our COE patients’ feedback has been overwhelmingly positive. While substantial resources needed to be invested to support them, the program’s high-touch, encouraging outcomes have continued to energize our care teams.
Targeted access to electronic platforms for patient engagement will be critical to the success of perioperative population management [16]. Accordingly, we have initiated the use of such platforms (e.g., Epic Care Companion, telemedicine pre- and postoperative visits facilitated through the Ochsner Health patient portal). We envision continuing to expand their use. Personnel, such as unit-based providers and care navigators, are being aligned to encourage patients to sign on to and adopt their use prior to and during hospitalization.
References
Srinivasan D, Desai NR. The impact of the transition from volume to value on heart failure care: implications of novel payment models and quality improvement initiatives. J Card Fail. 2017;23:615–20.
Moy HP, Giardino AP, Varacallo M. Accountable Care Organization. 2021 Feb 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. Accountable Care Organization - StatPearls - NCBI Bookshelf (nih.gov).
Piccinin MA, Sayeed Z, Kozlowski R, Bobba V, Knesek D, Frush T. Bundle payment for musculoskeletal care: current evidence (part 1). Orthop Clin North Am. 2018;49:135–46.
Centers for Medicare & Medicaid Services: Comprehensive Care for Joint Replacement Model. https://innovation.cms.gov/innovation-models/cjr (2021). Accessed 11 Jun 2021.
Federal Register: Medicare program: Comprehensive Care for Joint Replacement Model Three-Year Extension and Changes to episode definition and pricing. https://www.federalregister.gov/documents/2020/02/24/2020-03434/medicare-program-comprehensive-care-for-joint-replacement-model-three-year-extension-and-changes-to (2021). Accessed 11 Jun 2021.
Centers for Medicare & Medicaid Services: Hospital Compare. data.medicare.gov/data/hospital-compare (2021). Accessed 11 Jun 2021.
Guo EW, Sayeed Z, Padela MT, Qazi M, Zekaj M, Schaefer P, Darwiche HF. Improving total joint replacement with continuous quality improvement methods and tools. Orthop Clin North Am. 2018;49:397–403.
Cline KM, Clement V, Rock-Klotz J, Kash BA, Steel C, Miller TR. Improving the cost, quality, and safety of perioperative care: a systematic review of the literature on implementation of the perioperative surgical home. J Clin Anesth. 2020;63:109760.
Vetter TR. Perioperative surgical home models. Anesthesiol Clin. 2018;36:677–87.
den Hertog GK, Timm J, Mühlbauer B, Zebrowski S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: a randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch Orthop Trauma Surg. 2012;132:1153–63.
Sumarriva G, Wong M, Thomas L, Kolodychuk N, Ochsner JL, Chimento GF. Perioperative surgical home model with or without electronic medical record integration results in positive clinical and financial outcomes. 2018 AAHKS annual meeting, Dallas, TX, November 1–4, 2018.
Schubert A, Patterson M, Sumrall WD, Broussard D, Dias D, Aboalfaraj A, Thomas L, Bergeron B, Brandon B, Shum L, Ravipati L, Chimento G. Perioperative population management for primary hip arthroplasty reduces hospital and postacute care utilization while maintaining or improving care quality. J Clin Anesth. 2021;68:1–11.
Chauffe A. How we became a Walmart Center of Excellence. Presented at the Academic Orthopedic Consortium (Orthopedic Administrator’s Organization), 2019.
Piccinin MA, Sayeed Z, Kozlowski R, Bobba V, Knesek D, Frush T. Bundle payment for musculoskeletal care: current evidence (part 2). Orthop Clin North Am. 2018;49:147–56.
2019 Annual ECEN joint quality data review. Contigohealth Updated 12–2-2020.
Campbell K, Louie P, Levine B, Gililland J. Using patient engagement platforms in the postoperative management of patients. Curr Rev Musculoskelet Med. 2020;13:479–84.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Chimento, G.F., Chauffe, A., Wooldridge, J., Oravetz, P. (2022). Quality Metrics for CMS Care Bundles and Commercial Center of Excellence Status. In: Schubert, A., Kemmerly, S.A. (eds) Optimizing Widely Reported Hospital Quality and Safety Grades. Springer, Cham. https://doi.org/10.1007/978-3-031-04141-9_37
Download citation
DOI: https://doi.org/10.1007/978-3-031-04141-9_37
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-04140-2
Online ISBN: 978-3-031-04141-9
eBook Packages: MedicineMedicine (R0)