Abstract
Complex bone injuries often impact several types of tissue and experience healing complications due to injury severity, infection, instability, or other comorbidities such as diabetes. The intricacies and poor functional outcomes of these injuries merit the consideration of regenerative medicine in concert with rehabilitation strategies to improve healing. The field of regenerative rehabilitation is emerging with promising technologies, since bone is a dynamic tissue that is highly sensitive to mechanical stimulus and its regeneration is accomplished by a cascade of biological processes that are strongly influenced by local mechanical loading (Carter et al., Clin Orthop Relat Res (1976–2007) 355:S41, 1998; Kenwright and Goodship, Clin Orthop Relat Res 241:36–47, 1989). Enabling technologies to investigate these injuries include regenerative strategies such as protein or cell delivery to augment the endogenous biological environment and promote healing; implantable sensors and wireless technologies to longitudinally quantify the in vivo mechanical environment of the defect in a real-time, patient-specific manner; as well as computational models of tissue differentiation and healing to provide predictive mechanical boundary conditions that optimize healing. Ultimately, integration of these emerging innovations with advancements in understanding the fundamental biological principles of mechanotransduction may enable optimizing personalized feedback-controlled rehabilitation strategies that promote functional restoration of complex bone injuries.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction and Current Clinical Practice
This chapter will discuss the intersection of regenerative medicine and rehabilitative strategies to address complex bone injuries that often experience healing complications due to injury severity, infection, instability, or other comorbidities such as type I and II diabetes. These injuries are intricate and prone to poor functional outcomes, which merits the consideration of bone regeneration in concert with rehabilitation strategies to improve healing. Regenerative medicine concentrates on regrowing or replacing injured, diseased, or defective tissues, while the purpose of rehabilitation is to facilitate functional recovery after an injury, illness, or disease. The process of bone healing involves regeneration of bone tissue that continually responds to the biological and mechanical environment. Therefore, the field of regenerative rehabilitation can provide potential therapeutic strategies for complex injuries, because rehabilitation can provide a beneficial mechanical environment while regenerative medicine promotes a beneficial biologic environment to optimize functional healing. The following sections will contextualize the intersection of regenerative medicine and rehabilitation strategies for complex bone injuries to ultimately identify some of the current best practices, limitations, and areas for continued investigation. This chapter is organized into emerging technologies and translatable knowledge gained from multivariate computational models, implantable orthopedic sensors, and preclinical studies that combine regenerative and rehabilitation strategies.
8.1.1 Pathophysiology of Complex Bone Injuries
Complex bone injuries often leave patients devastated with high complication rates and poor functional restoration due to diminished coordination between the cellular activity within the healing niche and the surrounding tissue (Fig. 8.1). In fact, 5–10% of the 12 million annual fractures in the United States do not heal in a timely fashion or lack restoration of function entirely (Klosterhoff et al. 2017a). Large or complex bone injuries often stem from accident or combat traumas, tumor resection surgeries, or congenital defects (Uhrig et al. 2013). Open fractures can be classified using the Gustilo-Anderson classification which includes type I, II, or III where type III can be further described as grade A, B, or C (Egol et al. 2010). The Gustilo-Anderson classification design ranks injury severity on factors such as wound size, level of contamination, and damage to soft tissue and bone (Egol et al. 2010). Injuries are ranked more severe for increasing injury types, so type IIIC is the most severe with a wound size greater than 10 cm in length, high level of contamination, severe loss of soft tissue and bone coverage, plus vascular damage that requires repair (Egol et al. 2010). In preclinical research, large bone injuries can also be described as critical-size defects, which do not heal despite surgical stabilization. Bone healing can result in union, delayed union, or nonunion. Following injury, bone union is achieved when the bone is healed and strong enough to resume normal activity, delayed union is when the bone takes longer than usual to heal but the function is eventually restored, and nonunion is when the bone does not bridge and mechanical function is not restored following a severe injury.
Factors that contribute to bone nonunion or healing complications following complex bone injuries. Created with BioRender.com
In preclinical research, complex bone injuries that result in nonunion can be modeled by inducing a critical-size bone defect in animal subjects (Boerckel et al. 2011). To examine the functional ability of the regenerated bone tissue, defects are made in a weight-bearing bone and ex vivo mechanical tests are performed to quantify functional restoration (Boerckel et al. 2012). Radiography and microcomputed tomography may also be performed to longitudinally examine the defect throughout healing. These injury models provide crucial preclinical platforms to evaluate potential regenerative strategies in vivo to address clinically observed complications associated with delayed or nonunion bone healing.
8.1.1.1 Stages of Bone Healing
Following injury, bone healing consists of distinct, yet overlapping stages, including the early inflammatory stage, the repair stage, and the late remodeling stage (Kalfas 2001). Within a few hours of injury, the early inflammatory stage is initiated with hematoma formation to trigger infiltration of inflammatory cells and fibroblasts. The infiltration of these cells results in the formation of granulation tissue, ingrowth of vascular tissue, and migration of mesenchymal cells. Nonunion or poor healing complications can arise during this early stage if the inflammatory response is altered by the use of anti-inflammatory or cytotoxic medications (Kalfas 2001).
Next, the repair stage consists of fibroblasts building a stroma to support continual vascular ingrowth and infiltration of osteoprogenitor cells. As vascular ingrowth progresses, mesenchymal stem cells (MSCs) can differentiate directly into osteoblasts to form bone via intramembranous ossification or into chondrocytes to promote the formation of cartilage which serves as a template to be completely replaced by bone via endochondral ossification. The transition from cartilage to bone tissue begins with the differentiation of cartilage-producing chondrocytes into terminally differentiated hypertrophic chondrocytes which is associated with the subsequent invasion of blood vessels. Then MSCs from the periosteum (the enveloping connective tissue for cartilage) or vascular pericytes differentiate into osteoblasts and begin to form woven bone in the mineralized callus that is later remodeled into mature lamellar bone. The newly formed callus and the surrounding blood supply is sensitive to mechanical stimulus and thus requires adequate protection and stability in the form of external fixation via brace or internal fixation via a plate or nail (Elliott et al. 2016; McKibbin 1978). Stabilizing the defect at this stage is crucial to preserve the newly formed tissue because instability can prevent ossification of the callus and result in nonunion or poor healing (Elliott et al. 2016; Kalfas 2001).
If proper stability is maintained, the callus ossifies to form woven bone across the defect region. At this point, the defect will enter the remodeling stage where the shape, structure, and mechanical strength of the bone is restored. Remodeling occurs over a longer period of time (months to years) and is facilitated by mechanical stress, which activates osteogenic cells to promote bone formation in regions where bone is needed and resorption where bone is not needed (Kalfas 2001). Mechanical stimulation is necessary to promote bone modeling and remodeling during later stages of bone healing, but too much too early, can impair healing (Kenwright and Goodship 1989; Klosterhoff et al. 2017a).
8.1.1.2 Role of Skeletal Muscle
Several studies have found skeletal muscle to be a key player in functional bone regeneration following complex bone injury (Elliott et al. 2016; Uhrig et al. 2013). Before injury, muscle and functional weight-bearing, provide the mechanical stimulus necessary to trigger bone modeling and remodeling, as well as proper morphogenesis, maintenance, and repair of other tissue types (Guder et al. 2020). Beyond biomechanical stimuli, muscle is also a critical source for vascularization, progenitor cells, and osteogenic myokines to support bone repair after injury (Uhrig et al. 2013). In vivo research that utilized a preclinical model of segmental bone and volumetric muscle loss injury further established the relationship between bone and muscle tissue because injury to both tissues resulted in compromised bone healing (Willett et al. 2013). They found that a concomitant muscle injury decreased bone healing by approximately 50% compared to segmental bone injury alone for the same treatment (Willett et al. 2013). Muscle cells also help bone healing by secreting several osteogenic factors such as insulin-like growth factor (IGF-1), fibroblast growth factor (FGF-2), and transforming growth factor (TGT-β) (Ruehle et al. 2019). Additionally, muscle progenitor cells were shown to differentiate into osteogenic cell lineages when tracked in an open bone fracture and found incorporated into regenerated bone (Willett et al. 2013). The relationship between muscle and bone tissue is particularly relevant to regenerative rehabilitation because activation of muscle during rehabilitation can help guide bone regeneration and healing outcomes. Further, regenerative rehabilitation strategies can emulate the relationship between muscle and bone by modulating the mechanobiology via internal and external fixation devices that play a major role in determining the mechanical environment and subsequent pattern of healing (Kenwright and Goodship 1989).
8.1.1.3 Role of Vasculature
Vasculature is another key aspect of bone healing. In fact, vascular integrity is a key clinical indicator of injury severity, since revascularization is a critical early step for functional bone healing and is needed to stimulate bone repair (Boerckel et al. 2011; Klosterhoff et al. 2017a). However, little is known about the process of revascularization in the context of loading-induced bone regeneration. To address this gap in knowledge, a preclinical in vivo study done by Boerckel et al. quantified the effects of early and delayed functional loading on new vascular growth using their large bone defect model (Boerckel et al. 2011). The defects were stabilized with compliant internal fixation plates that were unlocked to allow ambulatory load transfer either at the time of implantation or after 4 weeks of the stiff (locked) internal fixation plate. They found that early mechanical loading inhibited vascular invasion into the defect and reduced bone formation compared to the stiff plate controls. In contrast, the delayed loading significantly enhanced bone formation and stimulated vascular remodeling (Boerckel et al. 2011). Their results demonstrate that neovascular networks are mechanosensitive and biomechanical stimulations have the capacity to modulate postnatal vascular growth and remodeling.
To expand the exploration of mechanobiology for vascular and bone tissue healing, Klosterhoff et al. engineered an implantable strain sensor platform to longitudinally measure strain across the defect stabilized with internal fixation plates in real-time and throughout rehabilitation. This in vivo study found an initial increase in deformation magnitude and a subsequent increase in bone formation for the compliant fixator that permitted load-sharing (Klosterhoff et al. 2020). Further load-shielding from the stiff fixation plate increased the number of relatively small vessels in the defect, while the load-sharing from the compliant fixation plate had a similar vessel number and size as the naïve contralateral femur (Klosterhoff et al. 2020). Therefore, although the increased strain magnitudes from the compliant plates impaired angiogenesis, the loading still supported sufficient tissue revascularization to enhance bone repair. Their work revealed distinct magnitude-dependent mechanobiological thresholds that differentially impair either bone of neovascular growth when exceeded.
To further analyze vasculature in the context of mechanical loading, an in vitro study by Ruehle et al. studied the effect of two load initiation times, three strain magnitudes, and two modes of compressive deformation on microvascular network growth within microvascular fragment-containing gels. They found that immediate loading inhibited angiogenesis and expression of vascular-related genes, while delayed loading enhanced microvascular network formation and upstream mechanotransduction signaling pathways. From this, they demonstrated that the magnitude, mode, and initiation time of the extracellular matrix (ECM) loading were all critical regulatory parameters for angiogenesis. Vasculature is a potential target for regenerative rehabilitation strategies because the blood supply is crucial for tissue regeneration and preclinical studies found vascular tissue to respond to varying magnitudes of mechanical stimulation (Boerckel et al. 2011; Klosterhoff et al. 2020; Ruehle et al. 2020). The knowledge gained from these studies provides the potential to enhance revascularization during tissue regeneration to optimize regenerative rehabilitation strategies for complex bone injuries.
8.1.1.4 Impact of Immune Dysregulation
Healing complications after complex bone injuries can also stem from a dysregulated immune response. Past work has characterized a detrimental dysregulated immune response which consists of chronic immunosuppression and immune paralysis. Trauma-induced immune dysregulation occurs in multiple stages, including an initial systemic inflammatory response syndrome (SIRS) and a compensatory anti-inflammatory response syndrome (CARS), each with unique cytokine profiles (Lord et al. 2014). The prolonged exposure to high levels of inflammatory factors and reactive oxygen species generated during SIRS is damaging to the surrounding tissues, so the CARS compensatory response immediately follows SIRS (Rosenthal and Moore 2016). In physiological healing, the SIRS and CARS responses resolve themselves within a couple of weeks; however, failure to restore homeostasis can lead to a destructive catabolic phase, otherwise known as systemic immune dysregulation and immune suppression (SIDIS) (Vantucci et al. 2018). Patients with symptoms of SIDIS are prone to complications and greater healthcare cost (Lord et al. 2014). A recent study using a preclinical model of orthopedic trauma demonstrated that distinct systemic immune profiles correlate with this long-term immune dysregulation and impaired bone regeneration (Ruehle et al. 2020). Some of the primary cellular mediators include T regulatory cells (Tregs) and myeloid-derived suppressor cells (MDSCs). These mediators contribute to the secretion of inflammatory cytokines and activation of other immune cells. Their work further supports the relationship between early systemic immune responses to trauma and local bone regeneration, with the potential to help predict poor functional outcomes and provide novel targets for immunotherapeutic interventions.
8.1.1.5 Conclusion
Overall, complex bone injuries are prone to nonunion or healing complications because of several factors including limited cellular communication and instability due to a large defect size, injury to neighboring vascular and muscular tissue, dysregulation of the systemic immune response, infection, or other comorbidities such as disease (Fig. 8.1). The restoration of bone tissue is crucial for functional recovery after complex injuries, but recent literature has found that restoring the vascular and muscular tissue, as well as controlling the immune response can help optimize necessary bone regeneration (Cheng et al. 2019; Ruehle et al. 2020). Research has also motivated the emerging field of mechanobiology because of the observed cellular response to mechanical stimulation throughout all stages of healing (Boerckel et al. 2011; Carter et al. 1998; Guldberg et al. 1997; Kalfas 2001; Klosterhoff et al. 2017a; Olesen et al. 2015). Therefore, modulating the mechanobiology of the healing niche via internal factors such as fixation stiffness or external factors such as rehabilitation has the potential to help address complex bone injuries that would otherwise face nonunion or healing complications. Additionally, the field of regenerative rehabilitation is emerging with promising strategies for complex bone injuries because the bone is a dynamic tissue that is highly sensitive to mechanical stimulus and its regeneration is accomplished by a cascade of biological processes that are strongly influenced by local tissue mechanical loading (Carter et al. 1998; Kenwright and Goodship 1989).
8.1.2 Clinical Treatment Strategies
8.1.2.1 Grafting: Masquelet Technique
There is currently no accepted medical standard to treat complex bone injuries, though the most common include debridement of necrotic tissue, prevention of infection, muscle flap coverage, bone grafting, and amputation as the last resort (Masquelet 2003; Nauth et al. 2011; Yazar et al. 2004). Within the realm of bone grafting, clinicians utilize allografts, autografts, as well as ceramic and polymeric bone graft substitutes. Allografts use bone from a deceased donor, so this practice is challenged with limited graft material as well as lower osteoinductive and osteogenic properties due to the sterilization process. Autografts use bone from the patient, so challenges include limited graft materials and surgical complications such as donor site morbidity. At the same time, ceramic or polymeric grafts have limited bioactivity, so they often rely on osteogenic cells or bone material to accompany the graft. Complications for this strategy include insufficient bioactivity or rejection of synthetic material altogether. The interplay between muscle and bone tissue has also motivated the clinical use of muscle flaps to help revascularize bone and promote healing of large range fractures. However, muscle flaps exhibit complications such as infection, partial or total flap loss, seroma or hematoma, necrosis, and wound dehiscence (Deramo and Rose 2020).
Historically, clinicians have tried using grafts in surgical treatments such as the Masquelet technique (Fig. 8.2) which uses a temporary cement spacer followed by staged bone grafting to manage posttraumatic bone defects (Wong et al. 2014). This strategy involves a two-stage surgical technique; the first operation includes debridement of necrotic bone, skeletal stabilization, and the insertion of polymethylmethacrylate (PMMA) cement spacer to envelope the bone ends (Olesen et al. 2015). Then after several weeks, the second operation involves the removal of the spacer without disrupting the induced biomembrane and filling the defect with bone graft (Deramo and Rose 2020). For this strategy, the cement spacer is vital for increasing stability, fighting infection, hindering fibrous ingrowth into the defect, and inducing a membrane that harbors and secretes growth factors such as vascular and osteoinductive factors to promote regeneration (Deramo and Rose 2020; Vantucci et al. 2018). Patients who underwent the Masquelet technique experienced pain-free weight-bearing after an average recovery time of 9 months (Deramo and Rose 2020). However, major differences were seen in consolidation time between patients and the correlation between consolidation time and bone defect size (Deramo and Rose 2020). Therefore, the healing timeframe for this technique is unpredictable (Aronson 1994; Deramo and Rose 2020).
Clinical example of a complex musculoskeletal injury that required revision surgery due to lack of bone healing after initial treatment. Courtesy of Dr. Philipp Leucht from NYU Langone. Created with BioRender.com
8.1.2.2 Mechanical Loading: Distraction Osteogenesis
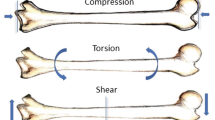
To avoid surgical intervention, scientists and clinicians have also utilized mechanical loading to promote bone union because interfragmentary movement, determined by the applied load and stability, has a strong impact on bone healing (Claes and Heigele 1999). This was evident in the study by Claes and Heigele that relates tissue formation in a fracture gap to local stress and strain (1999). Claes and Heigele found that varying levels of stress and strain along existing calcified surfaces in the fracture callus controlled whether the callus tissue differentiated into cortical bone, connective tissue, or fibrous cartilage (Claes and Heigele 1999). They knew mechanical loading influenced the healing process, but in vivo studies to determine the stress and strain of the cells in a fracture callus were not possible. To overcome this limitation, they employed the finite element method (FEM) to estimate the local stress and strain at the cellular level in callus tissue. This method allowed them to quantify the relationship between the ossification pattern and the loading treatment for the first time. They found the critical values that guided cell differentiation into either an osteoblast or a chondrocyte to further direct either intramembranous differentiation or endochondral ossification. However, the FEM poses limitations because it depends on set parameters that only correlate to simple oblique fractures and their study only described bone healing as three distinct stages (Wong et al. 2014). Future work that examines the cellular mechanisms of bone healing may help explain the pathology of delayed or nonunion defects. Longitudinal analysis of fixation techniques is also needed to understand how the healing progresses in response to loading. The amount of interfragmentary movement to optimize healing and avoid nonunion complications remains unknown, but work continues to highlight the potential for mechanical loading to control and promote bone regeneration.
Utilizing mechanical loading, surgeons have tried distraction osteogenesis to address large bone defects. This strategy includes an initial osteotomy followed by gradual distraction to induce the integration of cells, growth factors, and extracellular matrix to form bone (Compton et al. 2015). Bone formation using distraction osteogenesis relies on control of mechanical tension by altering the rate and rhythm of distraction to influence cell proliferation, angiogenesis, and genetic expression within the distraction gap (Olesen et al. 2015). The exact mechanism in which strain stimulates bone formation remains unclear, but research suggests that slow and steady traction can metabolically activate living tissue through mechanotransduction, which stimulates proliferation and biosynthetic cellular function (Ai-Aql et al. 2008). Similarly, other investigations have found molecular signaling cascades to play an important role in strain-induced bone regeneration (Olesen et al. 2015). After, initial success, this technique was modified to shorten the consolidation time. From this, the rate of distraction was seen as an important clinical consideration because high-speed distraction exhibited painful neuropathy and soft tissue complications, while slow distraction diminished the osteogenic potential (Olesen et al. 2015). Although this technique has seen promising results, robust investigations are still underway because of the delicate physiological balance required for all stages of healing. Such investigations involve applying systemic and local factors that may improve healing, as well as other mechanical loading strategies to promote regeneration. Distraction osteogenesis also illuminates the need for personalized medicine because the healthy population may require faster distraction rates than the elderly or ill to maintain osteogenesis.
8.1.3 Current Clinical Rehabilitation Practices and Limitations
Rehabilitation is a critical component of the healing process—in terms of both tissue repair and functional recovery—and is commonly prescribed to patients after regenerative or reparative intervention for complex bone injuries in the lower extremities. Key factors that influence the rehabilitation regimen include the severity, type, and location of the injury along with the fixation method. Typically, clinicians prescribe relatively conservative regimens that begin with non-weight-bearing for up to 12 weeks before progressing to the next stages of active rehabilitation for severe injuries. Once patients are permitted to use their injured limb, rehabilitation incorporates a variety of loading, strengthening, and pain management strategies.
Clinical rehabilitation can start with non-loading practices for a recommended length of time, and varies based on injury severity, type, and fixation method. The major methods of fixation include internal and external fixation. External fixation methods are commonly used for traumatic injuries that often result in open fractures and severe damage to the surrounding soft tissue (Hoyt et al. 2015). Since external fixation can shield the injured region from excessive axial loading, immediate weight-bearing can be permitted as long as the patient is not experiencing unusual pain (Bacon et al. 2008; Joslin et al. 2008; Kershaw et al. 1993; Taljanovic et al. 2003) However, for more severe injuries, patients are often prescribed a 6-week non-weight-bearing period following surgery because the open reduction and internal fixation (ORIF) method often used for these more severe fractures is most effective when the injured region is completely stable (Joslin et al. 2008; Kershaw et al. 1993; Mitkovic et al. 2002; Sato et al. 1999; Zlowodzki et al. 2007). If the internal fixation is coupled with intramedullary fixation, immediate weight-bearing may be permitted, again providing the patient is free of pain (Arazi et al. 2001; Lin et al. 2014; Brumback et al. 1999). Many of these regimens are based on the severity of the bone injury and guidelines often do not account for the severity of soft tissue injury or volumetric muscle loss which can accompany complex injuries. Research implementing rehabilitation for the treatment of volumetric muscle loss has shown significant challenges in restoring function and general guidelines do not currently exist (Greising et al. 2020).
The most common form of rehabilitation following the non-loading period for complex bone injuries is progressive touchdown weight-bearing (Hoyt et al. 2015; Hurkmans et al. 2007). This process begins with toe-touch weight-bearing, during which only the toes of the injured limb should touch the ground. This is followed by partial weight-bearing, where the clinician may prescribe 10%, 25%, or 50% weight-bearing following injury. The percentage increases on a patient-by-patient basis until the patient is able to place full weight on the injured limb (Inverarity 2020). Patients may be provided scales or body weight supports to control forces in the lower limb. One of the major issues with restricted weight-bearing is poor patient compliance; even when patients attempt to follow the clinician’s recommendations, they frequently exceed the weight permitted. Alternatively, other techniques such as hydrotherapy and lower body positive pressure (LBPP), which allow for better control of the pressure on the injury, may be used (Stucky et al. 2018).
In addition to direct loading on the bone, rehabilitation regimens also focus on muscle strengthening and pain management. Serious leg injuries, especially those which require several weeks of non-loading, lead to significant muscle loss. Studies have found that patients prescribed with muscle strengthening exercises improve strength, balance, mobility, and function (Latham et al. 2014). Exercises include standing from a chair, walking up steps, and other functional-based exercises. Pain following injury is typically managed through analgesia and the use of peripheral nerve blocks, which have been shown to aid in functional use of the limb and reduce falls (Ilfeld et al. 2010; Long et al. 2006). Rehabilitation regimens have been shown to help patients with pain management and as a result reduce the doses of analgesia prescribed (Cheville et al. 2018). Such rehabilitation strategies often incorporate stretching and strengthening with the goal of restoring basic functions and activities (Osterweis et al. 1987).
Preclinical studies have shown that early loading improved healing outcomes in both bone growth and bone strength compared to those with extended periods of non-loading after injury. However, current rehabilitation strategies still prescribe extended periods of non-loading after injury. Section 8.2.3 will further detail the results of preclinical trials regarding the effects of early loading on tissue regeneration and functional restoration.
8.2 Effects of Mechanical Environment on Vascular Growth, Tissue Differentiation, and Bone Regeneration
The notion that bone adapts to mechanical stress during rehabilitation via remodeling processes is often attributed to Julius Wolff in the late nineteenth century. Wolff observed that trabeculae of fractured bone remodeled over time due to changes in bone shape or mechanical stresses (Brand 2010; Wolff 1892). Mechanosensitivity has since been demonstrated in numerous physiological processes in most tissues and throughout the organ to intracellular levels. Near the turn of the century, researchers began formalizing approaches to predict patterns of tissue differentiation, mineralization, osteogenesis, chondrogenesis, and vascular growth based on mechanical loading environments. These approaches are beginning to guide patient and etiology-specific rehabilitation and regenerative strategies. In this section, we review computational methods, wireless strain sensor developments, and preclinical models that have advanced our understanding of tissue adaptation in response to mechanobiological stimuli in fracture healing and remodeling. These approaches may guide regenerative and rehabilitation strategies by encouraging proper tissue differentiation and ultimate union after fracture in long bones.
8.2.1 Computational Models of Tissue Differentiation and Healing
Nearly a century after Wolff’s law was established, researchers still disagreed on how stress mechanistically controlled bone morphology. Experimental models have delineated links between strain and patterns of tissue differentiation during healing, though these pathways are more complex in vivo. This section overviews computational approaches to incorporate mechanical and biological regulators of osteogenesis, chondrogenesis, and angiogenesis into computational models. We first review seminal computational advances in simulating tissue differentiation and healing in response to fracture mechanical environments, and then we demonstrate their capability of probing and designing regenerative rehabilitation protocols.
8.2.1.1 Approaches to Modeling Osteogenesis, Chondrogenesis, and Angiogenesis
Computational models of osteogenesis and tissue differentiation first attempted to predict long bone mineral distribution and tissue density in response to mechanical loading. Some of the initial research needed to support these computational aims focused on developing material models to explain bone in the context of fracture healing. A robust theory relating stress to bone orientation and density presented by Fyhrie and Carter proposed that cancellous bone is an anisotropic material that simultaneously maximizes structural integrity and minimizes bone density (Fyhrie and Carter 1986). In addition to developing material models, they also developed a fundamental approach to simulate the effects of cyclic load histories without explicitly modeling each individual load, a task that may have been computationally cumbersome at the time (Carter et al. 1987). Once the material model and approach to simulating cyclic load history were formalized, they were applied in one of the first computational models that predicted a physiological distribution of bone mineral density in response to mechanical loads. Importantly, the authors noted that the degree of tissue stress stimulus determined the degree of bone resorption or apposition (Beaupré et al. 1990). Further studies found that physiological bone density patterns can be predicted in numerous bones as long as the simulated load histories are comprehensive and reflective of multiple activities of daily living (Levenston et al. 1993).
While investigating the effects of a micromotion implant in canine condyles, Prendergast et al. developed a theory of a mechanoregulatory pathway. Their theory stated that biophysical stimuli determine the trajectory of cells during tissue differentiation (Huiskes et al. 1997). The differentiated interface tissue took on either a bony, fibro-cartilaginous, or fibrous phenotype depending on the distortional strain and relative fluid velocity (Huiskes et al. 1997). Subsequent models studied the adaptation of segmental defects to mechanical loads (Beaupré et al. 1990; Fyhrie and Carter 1986). They created FE models of the callus, medullary tissue, and diaphyseal bone at the defect and applied simplified loading histories of compression or tension to six models with unique initial boundary conditions representing different mechanobiological environments. Notably, a single modeling approach was able to predict experimental tissue differentiation patterns of fracture healing and distraction osteogenesis. This model of tissue differentiation was refined and applied numerous times in different contexts (Fig. 8.3). Claes et al. found that low magnitude strains encourage intramembranous healing while high magnitude strains and pressures lead to connective and fibrous tissue differentiation (Claes and Heigele 1999). Loboa et al. focused on the continuous change of material properties, allowing their material parameters to continuously adapt to local mechanical stimuli, rather than at fixed time points. Proteoglycan synthesis, collagen fibrillogenesis, crosslinking, and material moduli were regulated by fluid pressure and tensile strain. Further, materials were allowed to adapt into any phenotype unlike prior models which assumed differentiation into one of a few predefined phenotypes (Loboa et al. 2003; Wren et al. 2000). Indeed, these modeling approaches were a promising platform to study mechanoregulation of tissue differentiation during fracture healing; however, a few studies demonstrated that mechanoregulation alone was insufficient to account for biological factors and subject variation (Beaupré et al. 1990; Stevens et al. 1999). Thus, models around the turn of the century began to incorporate both mechanical and biological variables to better predict bone adaptation to mechanical stimuli.
Reproduction of the mechanoregulatory model proposed by Carter et al. (1998) created with BioRender.com. Mechanoregulatory models typically predict differentiation based on state variables such as stress, strain, and fluid velocity. Further, the distribution of tissue types can change over time to reflect the dynamic nature of healing
In addition to mechanical activity, in vivo bone healing outcomes can be influenced by oxygen, growth factor, and metabolite transport and production. Investigators of previous studies began introducing cell-based modeling approaches which simulate differentiation of cell populations rather than only tissue types in response to mechanobiological stimuli. These cells transformed the tissue around them through reactions representing bone apposition and resorption (Beaupré et al. 1990; Hernandez 2000). Ament and colleagues adapted the models of Carter et al. (1998) by introducing a fuzzy logic controller to determine tissue differentiation and composition (Ament and Hofer 2000). Previous models had only allowed tissues to differentiate into a single phenotype; fuzzy set theory however allowed various degrees of membership to multiple tissue types depending on mechanical and biological stimuli (Zadeh 1965). A subsequent study used fuzzy logic, which included local vascularity as a biological variable to predict trabecular bone fracture healing and remodeling as distinct events (Shefelbine et al. 2005). At this time, most models had only represented the influence of biological variables in an abstract manner rather than evaluating the transport of oxygen, growth factors, or metabolites. Bailón-Plaza and van der Meulen were perhaps the first to develop a bioregulatory model that simulated the transport, production, and inductive role of growth factors in the context of tissue differentiation during fracture healing (Bailón-Plaza and van der Meulen 2001). In their model, mesenchyme was allowed to take on chondrocyte, osteoblast, and osteocyte lineages as well as undergo mitosis and produce matrix and other cellular products in response to BMP-2, BMP-4, and TGF-β1. In a follow-up study, a combined mechanobioregulatory modeling approach was used to simulate growth across a fracture while varying the onset and magnitude of loading (Bailón-Plaza and van der Meulen 2003). In both experimental and computational studies, delayed onset of loading led to low-stiffness tissue properties and nonunion or poor healing. Simulations indicated that by the time of load onset, the concentration of osteoblasts had greatly declined, leading to insufficient endochondral ossification. Early, moderate loads however were associated with stiff gap tissue and successful bridging. Bailón-Plaza et al.’s approach and observations became common in successive studies that demonstrated the ability of experimentally based computer simulations to guide regenerative rehabilitation therapies. However, these models still took simplified approaches to represent transport wherein cells, biophysical species, and growth factors were assumed to move only via diffusion.
Geris and colleagues acknowledged that the simplifications of previous models had limited the models’ ability to study compromised healing cases. To address this, they extended the bioregulatory models of Bailón-Plaza et al. by simulating endothelial cells that migrated from preexisting vasculature (Geris et al. 2008). Endothelial cell movement was guided by both a random component and an angiogenic factor gradient. Osteoblasts and hypertrophic chondrocytes generated the angiogenic factor, attracting endothelial cells to the callus after the formation of the initial fibrous and cartilaginous tissue in the soft callus. The model was sensitive to the production and consumption of the angiogenic factor—overproduction or saturation of the angiogenic factor did not permit gradient formation, resulting in poor healing. Further, reduced production of angiogenic factor led to slow healing and nonunion. The mechanoregulatory mechanism was reintroduced in a later study where Geris et al. demonstrated that overload-induced nonunion could only be predicted when both angiogenesis and osteogenesis were governed by mechanoregulatory and bioregulatory mechanisms (Geris et al. 2010). A similar approach included mechanoregulatory elements to study osteogenesis and angiogenesis in the bone-implant interface (Checa and Prendergast 2009). Notably, they predicted dendritic growth of new vasculature similar to angiogenesis, as well as decreased angiogenesis and osteogenesis when high shear loads were introduced between the implant and bone. The basic concepts developed thus far built a basis that at first reproduced experimental results of healing and nonhealing based on mechanical and biological stimuli. More recently, these results have been applied to patient-specific and etiology-specific cases to guide regenerative rehabilitation strategies for the clinic.
8.2.1.2 Applied Models of Angiogenesis and Osteogenesis
With the knowledge that interfragmentary movement strongly relates to bone adaptation and healing outcomes (Claes and Heigele 1999), investigators began to study how fracture stabilization protocols in both the operating room and rehabilitation clinic influence interfragmentary movement and long-term fracture healing. Prior simulations of healing relied on idealized fracture site geometry and loading conditions which may smooth over local hotspots of stress and strain introduced by irregular fracture geometries. One of the first patient-specific models of interfragmentary movement was performed while a patient was simultaneously recovering with a stabilized fracture (Gardner et al. 2000). The patient’s fracture geometry and gait-cycle loads during recovery were used as inputs. The patient experienced delayed healing, which based on predicted distributions of strain throughout the callus, the authors believe may stem from insufficient interfragmentary support by the fixation device during the early course of healing. In addition to patient-specific studies, some began to evaluate fixation procedures themselves. One group found that significant non-axial movement can occur during axial dynamization depending on fixator joint location and the ability for joints to slide (Liu et al. 2005).
In addition to studying fixator design, recent interest has emerged pertaining to when fixator dynamization or removal can begin. Byrne et al. modeled a fixation device which was automatically removed once the callus had reached a threshold stiffness in an approach that may be useful for patient-specific preoperative treatment planning (Byrne et al. 2011). Alierta et al. studied the effects of combined compressive and shear loads during healing across a fixated fracture, which had scarcely been studied experimentally at that time (Alierta et al. 2014). Further, they studied the effect of fixation on comminuted fractures (in this case an oblique fracture with three fragments) and found that comminuted fractures may require stiffer fixation than simple transverse fractures. Wilson et al., modeled inverse dynamization—a recently proposed fixation strategy where some interfragmentary movement is initially allowed in order to promote a large callus to form, at which point, dynamization is restricted (Wilson et al. 2017). They found that inverse dynamization led to quicker callus formation but ultimately did not provide significant additional stiffness to the fracture during healing. A similar study by Ganadhiepan et al. investigated dynamization with the treatment of Ilizarov circular fixators (Ganadhiepan et al. 2019). They found that early dynamic physiological loads may encourage advective transport and improve secondary healing. Simultaneously, their simulations predicted changes in cell population distributions and matrix deposition associated with different fixator material properties. While much attention has been given to external fixators, simulations are also used to study internal stabilization methods. For example, Mehboob and colleagues used simulations to select composite materials for intramedullary rods that best supported callus formation and healing in transverse or oblique fractures at multiple locations along the length of the femur (Mehboob and Chang 2018). Indeed, simulations have enabled a deeper understanding of how fixation techniques and fracture etiology alter the mechanical environment and biological adaptation.
8.2.2 Implantable Sensors for In Vivo Load Monitoring
The healing outcomes from orthopedic injuries that require the use of temporary or permanent implants depend on the surgical technique, rehabilitation approach, patient’s health, and physical activities, as well as the mechanical environments at the implant sites (O’Connor and Kiourti 2017). Today, assessments of the mechanical environment at a musculoskeletal injury site are still typically done using mechanical loading/measurement instruments and/or numerical simulations based on assumed boundary conditions (Klosterhoff et al. 2017a). These methods may be inaccurate in many instances because they are usually performed under ideal and controlled conditions with assumptions that may not capture the actual mechanical loading experienced during the patient’s physical activities. Direct measurement of the mechanical loading outside of a laboratory or clinical setting would provide a better assessment of how mechanical forces can promote or impair functional healing of an orthopedic injury (Klosterhoff et al. 2017a).
In 1960s, researchers started to integrate sensors to orthopedic implants through percutaneous wires, so measurements could communicate to external data processing electronics for monitoring in vivo mechanical forces in the shoulder, spine, hip, and knee implants (Karipott et al. 2018a). These sensors were mostly used as investigative tools to study the healing process and shed light on the physical environment in the musculoskeletal system (Karipott et al. 2018a). Since then, rapid innovations in electronics, computing, battery, and wireless communications have significantly increased the integration of sensors into orthopedic implants. Modern wireless sensors, which are smaller, safer, and more convenient to use, have been incorporated into various orthopedic implants to further improve their performance. These sensor-integrated orthopedic implants can allow efficient measurement of clinical data that was not possible before, providing new therapeutic and diagnostic capabilities to enable personalized medicine, which leads to better treatment outcomes for orthopedic injuries (Ledet et al. 2018). Specifically, sensor-integrated orthopedic implants generate useful information characterizing the environment inside the body, giving an opportunity to tailor treatment regimens, trigger transition in care, and detect adverse events earlier (Ledet et al. 2018). They also minimize complications, reduce recovery time, and decrease readmission and revision procedures (Ledet et al. 2018). Moreover, the use of sensors in orthopedic implants gives a greater understanding of the healing processes, tissue-implant interactions, and biomechanics of the injury hence providing knowledge for the development of improved implants and surgical techniques.
8.2.2.1 Sensor and Wireless Technologies
Stress and strain are critical parameters in orthopedic care, providing useful information on the healing conditions after an injury. These parameters can be used to determine the effectiveness of the treatment and predict patient outcomes. While many sensors are available, strain gauges are still the dominant technology for measuring stress and strain (Karipott et al. 2018a). In fact, strain gauges continue to be used in orthopedic implants since the 1960s due to their robustness, sensitivity to applied strain, and convenience to integrate on or within the implants (Ledet et al. 2018).
Strain gauges, as shown in Fig. 8.4a, are electronic components that vary their electrical resistance in response to applied mechanical strains. A Wheatstone bridge circuit, illustrated in Fig. 8.4b, is typically implemented to change an input resistance of a strain gauge to a voltage output that can then be processed to a digital output. Typically, strain gauges are a thin layer of electrically conducting pattern deposited onto a polymeric backing substrate (Ledet et al. 2018). A strain gauge is usually directly attached to the surface of an implant. The deformation of the implant alters the dimension of the strain gauge, creating a proportional change in the gauge resistance. The resistance change is then converted to a digital voltage output as a record of change in strain (Ledet et al. 2018).
Traditional strain gauge sensors require transcutaneous wired connections to supply power and collect in vivo data from patients or test subjects. For example, Sato and coworkers developed a piezoresistive strain gauge pressure sensor that was percutaneously wired to external electronics to measure intradiscal pressure (Sato et al. 1999). Another group developed a similar strain gauge embedded inside a femoral head prosthesis via percutaneous wires to monitor forces on a hip implant (Rydell 1966). In addition, Burny and coworkers have also demonstrated the application of strain gauges for orthopedic monitoring (Burny et al. 2000) by integrating resistive strain gauges into a modified nail plate implant to perform in vitro and in vivo evaluations on the effectiveness and safety of the implant system (Burny et al. 2000).
Wired sensors, while able to provide continuous and high-resolution measurements on orthopedic conditions, are limited to laboratory and/or clinical settings and have an increased risk of infection to the test subjects. Advancements in telemetry systems have allowed for the development of sensors that can wirelessly communicate and transfer data without wires (Nelson et al. 2020), which alleviates these issues. As depicted in Fig. 8.5, a telemetry system commonly consists of two components: a transmitter that is implanted along with the strain gauge (or other types of strain/pressure sensors) and a receiver that is typically connected to a signal processor such as a computer or a handheld electronic recording/displaying device. An example of a wireless orthopedic sensor was developed by Ledet and coworkers for direct in vivo measurements of spinal loads on the lumbar spine of baboons (Ledet et al. 2012). Other strain gauge implants include those developed by Rohlman and coworkers to study loads on the vertebral body (Rohlmann et al. 2014), and the calcium phosphate ceramic-coated strain gauges by Szivek and coworkers (Szivek et al. 2005) that exhibited improved osteointegration.
Although wireless sensors possess clear advantages over wired sensors in terms of safety and convenience, a limitation of their usage in orthopedic implants is the power requirement at the implanted part of the sensor system. They are also bulky due to the size of the battery. Therefore, wireless sensors typically have a limited operation lifetime and require a carefully planned power budget. To extend the performance period of wireless sensors, some sensor-integrated implants employ batteries that can be charged remotely, or use an energy harvesting system that can generate power from mechanical forces (Nelson et al. 2020). For example, Santos and coworkers generated energy needed by a hip implantable sensor by utilizing the motion around it (Soares dos Santos et al. 2013). Another approach to prolong operation time is to reduce the power consumption rate. Integrated circuit technology has enabled the fabrication of implantable sensors (Soares dos Santos et al. 2013) featuring power-saving circuit designs such as the bulk-driven technique, the floating gates, and the subthreshold design (Borchani et al. 2016).
Besides batteries, some sensors are powered by an external device through wireless energy coupling and communicate through electromagnetic fields or acoustic waves. These sensors have been used to measure various parameters in hip prostheses, as well as loads in the knee and spine. The most common wirelessly powered systems are inductively coupled systems, which receive power through electromagnetic energy (Ledet et al. 2018). For example, Graichen and coworkers developed a system that consisted of six strain gauges and a telemetry system that utilized radio frequency (RF) to inductively power the electronics and transmit data (Graichen et al. 2007). It was implemented on three patients with shoulder endoprostheses to monitor in vivo load (Graichen et al. 2007).
Another type of battery-free sensor is comprised of only energy-passive elements such as magnetic materials or passive electronic components (capacitors, inductors, and resistors) forming a combined sensing unit and wireless transceiver. They have no active circuitry and do not require an internal power source, making them small, robust, reliable, and ideal for long-term, in vivo monitoring. One example of passive sensors is the magnetoelastic sensor, made of magnetostrictive materials that can convert magnetic energy to mechanical energy and vice versa. When under the excitation of a magnetic AC field, the sensor undergoes a mechanical resonance, generating a secondary magnetic flux that can be remotely captured (Pacella et al. 2014). These sensors, which are wireless, battery-free, and sensitive to stress/strain, are used to measure forces at bone fixation plates or medical sutures (DeRouin et al. 2016; Oess et al. 2009). They are easily integrated into existing implants because of their simple designs and have demonstrated application to monitor cell adhesion on an implant and bone tissue integration to implant (Vlaisavljevich et al. 2013). Another passive sensor is the inductive-capacitive sensor which consists of an electrical resistor, inductor, and capacitor (RLC) that exhibit an electrical resonance when interrogated with an RF wave. By sensitizing the RLC element to stress/strain, these sensors have been used to monitor pulling force and deformation at orthopedic implants (Karipott et al. 2018b). Karipott and coworkers also developed a wireless RLC-based sensor that was inductively powered to detect infection at an orthopedic implant site by analyzing the change in temperature, measured through the shift in resonance frequency due to the temperature-induced variation in the resistor value (Karipott et al. 2018b). Although these battery-free wireless sensors have a much longer operational life compared to their battery-powered counterparts, they need to be passively powered to function thus preventing them from applications where continuous, uninterrupted monitoring is needed (Karipott et al. 2018b). Moreover, metallic orthopedic implants may limit the ability to use electromagnetic energy, and result in signal distortion, loss of energy, and performance reduction (Karipott et al. 2018b).
With these technologies, sensors have been incorporated into orthopedic implants to monitor physical parameters (force, loading, pressure, strain, etc.) in bones at the knees, hips, shoulders, etc., to study healing outcomes and monitor conditions of implants after surgery. Most of these sensors are based on strain gauges and rely on wireless transmission protocols (with custom communication schemes or standard protocols such as Bluetooth). For example, Klosterhoff and coworkers developed a bone fixation device for rats with an embedded wireless strain gauge sensor to quantify the mechanical environment experienced by healing tissues during physical activities (Klosterhoff et al. 2020). A digital transceiver based on Bluetooth low energy (BLE) was used for remote-controlled circuit calibration (Klosterhoff et al. 2020). Although Klosterhoff’s sensor was limited as an investigational tool to study changes in mechanobiological cues in vivo for an extended period following surgery, other sensors are already in the process or at the early stage of clinical adoption (Bergmann et al. 2007; Karipott et al. 2018a; Ledet et al. 2005), and a few of them are commercially employed to assist orthopedic surgeries (Gustke et al. 2017).
In conclusion, implantable sensors have become a key component in orthopedic regenerative medicine. These sensors, when integrated within existing orthopedic implants, have allowed new understandings of the mechanics of bone and tissue regeneration, leading to the development of better implants and treatment procedures. While implantable sensors will continue to play an increasing role in orthopedic care, they still face challenges in terms of their efficacy, cost, and biocompatibility for long-term monitoring. Furthermore, the lack of standardization in implantable sensors still causes confusion and miscommunications between sensor developers and physicians (Clausen and Glott 2014), slowing down the development process. Section 8.3.2 provides further discussions on the future of implantable sensors for orthopedic regenerative medicine, including new technologies, specific challenges, and innovative solutions to overcome the barrier to successful clinical translation.
8.2.3 Preclinical Regenerative Rehabilitation Studies
Revascularization is a primary limiting factor in tissue regeneration and in vitro work has shown that endothelial cells and vascular networks are mechanosensitive thus supporting mechanical loading as a potential strategy to address vascular limitations and help tissue regeneration (Kannan et al. 2005; Koike et al. 2004). To explore this potential, Boerckel et al. analyzed the effects of functional loading on neovascular growth and subsequent tissue regeneration in large bone defects (2011). Their preclinical study utilized the rat segmental bone defect model stabilized with a compliant plate that was either unlocked at the time of implantation (early) or 4 weeks after surgery (delayed). Microcomputed tomography and histology analysis found robust angiogenesis and collateral vessel formation after the initial vascular response to bone injury. However, early loading significantly inhibited vascular invasion into the defect by 66% and reduced bone formation by 75% compared to the stiff plate controls (Boerckel et al. 2011). In contrast, delayed loading enhanced bone formation by 20% and stimulated vascular remodeling by increasing the number of large vessels while decreasing the number of small vessels (Boerckel et al. 2011). Although early mechanical loading inhibited vascular growth into the defect, it did not change the overall quantified angiogenic response to the injury, which suggests that loading had a localizing effect. Ultimately, delayed loading exhibited an accelerated maturation and remodeling of new vessels which thereby enhanced bone tissue regeneration, while early loading disrupted neovascular ingrowth and impaired bone formation. Their results indicate that neovascular network formation and growth are regulated by mechanical conditions. Further, the timing and magnitude of loading were suggested as key variables and warrant further research to determine the optimal window for therapeutic effect.
Shortly after this study, Boerckel et al. further analyzed the effect of mechanical loading on BMP-2-induced bone regeneration (Boerckel et al. 2012). Following a similar design as their previous work, this study analyzed 6 mm segmental bone defects in rat femurs that were treated with BMP-2 and stabilized by either a stiff or compliant fixation plate, where the compliant plate allowed for compressive ambulatory load transfers 4 weeks after surgery (Boerckel et al. 2012). Radiography and microcomputed tomography found that loading significantly increased the regenerated bone volume, as well as the amount and distribution of bone formation within the defect. Mechanical testing also found loading to result in bone that was torsional more stiff than that of the unoperated limb (Boerckel et al. 2012). However, new bone distribution was limited to the proximal defect region of the femur, which could stem from the less favorable vascular environment for progenitor differentiation. The lack of progenitor cells means a limited presence of mechanosensitive cells to respond to local stimulus. Histology also found that loading prolonged the presence of woven bone, based on the collagen organization. Overall, the load magnitude resulted in modulated bone maturity, which was previously observed and speculated to result from irregular osteoblast and osteoclast activity (Guldberg et al. 1997). As a whole, this preclinical study demonstrates that altering the fixation plate stiffness to modulate functional load transfers significantly impacted BMP-mediated bone repair. Further, more transfer of axial loads increased bone formation and distribution and modulated the tissue organization and cellular differentiation within the defect. Their work motivates further investigation into mechanical loading as a potential clinical treatment for challenging segmental bone defects. The lack of new bone formation at the distal end also warrants evaluation of the suboptimal vascular environment.
These studies reassured mechanical loading as a bone healing strategy, but work was still needed for clinical translation. Research with more complicated models, such as the composite bone and muscle injury model established by Willett et al., was needed because complex bone injuries often impact neighboring tissues (Willett et al. 2013). This model combines a critically sized segmental bone defect with an adjacent volumetric muscle loss injury and was used to quantitatively assess BMP-mediated tissue regeneration and restoration of limb function. Their analysis looked at three groups: muscle injury, bone injury, and composite injury of the femur and quadricep. Treatment included pre-gelled alginate injected into a cylindrical perforated nanofiber mesh. Their assessment included microcomputed tomography to assess bone regeneration, as well as gait analysis and muscle strength measurements to assess limb function. By week 12, the bone injury subjects were consistently bridged, but the composite injury group exhibited bone volume and mechanical strength that were attenuated by 45% and 58%, respectively. The injured muscle strength, normalized to the contralateral intact muscle, was also reduced by 51% in the composite injury group. Gait function was inhibited by all groups, but the composite group displayed the greatest functional deficit. The deleterious effects of concomitant muscle injury on bone regeneration may be attributed to a diminished blood supply. Altered blood supply may result in changes to nutrient and waste exchange, inflammation, circulating stem cell recruitment, and thus revascularization of the defect. The loss of muscle volume could diminish bone regeneration because the source of resident muscle stem cells and myokines is limited, especially since these cells have displayed osteogenic capabilities. Overall, the BMP levels which consistently healed large segmental bone defects failed to promote functional regeneration when challenged with a concomitant muscle injury, indicating the need for further intervention. After the effect of mechanical loading on bone, muscle, and vasculature tissue is better understood, future work should implement mechanical loading in concert with BMP treatment to promote healing in multi-tissue injury models.
Motivated to quantitatively assess the effect of mechanical loading on bone repair and revascularization, Klosterhoff et al. deployed a strain sensor platform to examine the evolution of biomechanical cues within the regenerative niche following injury (Klosterhoff et al. 2020). The functional loads consisted of two different loading magnitudes similar to previous work with either a stiff or compliant fixation plate (Boerckel et al. 2011, 2012). Previously the dynamic biomechanical signals were difficult to measure inside the body, so they engineered a wireless implantable sensor that integrates into the internal fixation plates to perturb and remotely quantify the mechanical environment in real-time during ambulation. The data from the strain sensors found an initial two-fold increase in deformation magnitude for the load-sharing compliant fixation plate, subsequent three-fold increase in mineralized bridging, and over 60% increase in bone formation (Klosterhoff et al. 2020). Additionally, their work formed strong implications that early mechanical cues play a critical role in predicting long-term healing response because the strain magnitude at week 1 had a significant, positive correlation with long-term bone healing outcomes. They also found that defects stabilized with the compliant load-sharing plate exhibited vessel size distribution that more closely matched naïve vasculature. Ultimately, the compliant plate allowed for increased strain across the defect during gait relative to the stiff plate, and the increased strain enhanced bone repair. The sensor readings also correlated with the status of healing, suggesting an X-ray-free healing assessment platform. The wireless sensor could provide a noninvasive readout of the progression of healing in a personalized, real-time manner, which represents a notable shift in the ability to prescribe and monitor regenerative rehabilitation therapies. This study further motivates inquiry into mechanical loading as a clinical therapeutic, with emphasis on the mechanosensitive thresholds critical to both angiogenesis and osteogenesis to leverage and augment tissue repair.
8.3 Future Opportunities in Bone Regenerative Rehabilitation
8.3.1 Advances in Computational Modeling
In addition to the mechanical roles of patient geometry and fixation design, there are often nonmechanical factors that lead to fracture nonunion which can be included in computational studies of fracture healing. As noted by Carlier and colleagues, much of the current hesitation to bring computational models to the clinic results from the over-idealization and over-simplification of models which assume the patient is healthy and typical; in reality, patients may experience a number of factors that impair the fracture repair process not limited to “age…, malnutrition, immune compromise, genetic disorders, osteoporosis, anticoagulants, smoking, and anti-inflammatory agents” (Carlier et al. 2015).
Future advances in computational modeling will likely rely on guidelines developed from patient-specific comorbidities and injury composition and geometry. For example, it has been shown that genetic deficiencies in MMP9—a matrix metalloproteinase involved in skeletal healing, inflammation, and release of matrix-bound VEGF—led to altered patterns of hard callus cartilage remodeling, callus mechanical properties, and angiogenesis (Colnot et al. 2003). Peiffer et al. studied the effect of VEGF injections (either as a daily bolus or a slow-release carrier) on mechanically stimulated fractures in MMP9 deficient individuals (Peiffer et al. 2011). They found that injection of slow-release VEGF carriers, but not bolus injections, led to improved vascularization and healing (although not quite to levels seen in wild-type MMP9 models). Carlier and colleagues later demonstrated that nonunion could be reduced by addressing patient and injury-specific factors (Carlier et al. 2015). Using mechanoregulatory and mechanobioregulatory approaches, they studied four etiologies that lead to nonunion: damage to the marrow canal, large interfragmentary gap, genetic disorder, and mechanical overload during healing. They showed that the success of various therapeutic interventions depended on the etiology of fracture—highlighting the ability of personalized or etiology-based simulations to guide treatment regimens and clinical guidelines.
The inclusion of novel wireless sensors in preclinical and clinical studies will also allow better refinement of mechanobioregulatory models. Strain sensor measurements can now be used as inputs for image-based simulations to more accurately predict local strains and tissue differentiation. Biologic sensors and temperature sensors may also be used to better simulate etiology-specific healing environments. Guidelines formed from these simulations may also guide patient rehabilitation programs and identify when strategy interventions may be required based on individual comorbidities and sensor feedback.
8.3.2 Next Generation Wireless Implantable Orthopedic Devices
Section 8.2.2 has provided a review on the evolution and current state of implantable orthopedic sensors. This section will further describe the underlying technologies that enable the continuous development of current and future orthopedic sensors. This section will also highlight the various challenges for further clinical adoption of implantable orthopedic sensors in terms of their wireless communication, power source, long-term compatibility, etc.
8.3.2.1 Wireless Technologies for Orthopedic Monitoring
Although percutaneous wires were used in the earlier implementations of orthopedic sensors, they had been largely replaced by wireless sensors. The major advantage of wireless implantable sensors is that they can be employed without significant alteration to the standard orthopedic care while providing continuous, long-term monitoring for the study, treatment, and prevention of future orthopedic injuries and diseases (Karipott et al. 2018a). Today, most of the wireless implantable sensors are clinical tools for preclinical studies, but some of them have been clinically implemented. For example, implantable wireless sensors have been incorporated into orthopedic prostheses to characterize forces and design better prosthetics (Ledet et al. 2012). They are also used to measure flow and pressure in blood vessels as well as implemented as neurostimulators to treat muscular and neurological damages (Loeb et al. 2006; Potkay 2008). However, implantable sensors have limitations especially in their operational lifetime, safety, and potential interference with other medical devices; thus, careful design considerations regarding communication and power for wireless sensors are needed (Nelson et al. 2020).
Wireless sensors can be passive, which are powered through an external device, or active, which have an internal battery that can operate independently without an external energy source (Nelson et al. 2020). Passive sensors are typically simpler in design and smaller but limited in functionality, and only operate when being remotely powered. On the other hand, the main advantage of passive sensors is that they have a much longer operation lifetime since they are not constrained by battery capacity. Active sensors typically contain electrical components like microcontrollers and battery-powered transducers that need continuous power. Compared to passive sensors, the complexity of active sensors allows customization of its operation, simultaneous measurements of multiple analytes, and improved performance. However, the operation lifetime and footprint of active sensors are limited by their batteries (Nelson et al. 2020).
Both active and passive sensors have been employed for orthopedic monitoring. For example, Karipott and coworkers embedded a passive temperature sensor in an implantable screw to detect early infection of a wound site by monitoring the change in its local temperature. The sensor was an inductive-capacitive-resistive (LCR) sensor integrated into an interference screw and could be monitored wirelessly by a detection coil. Similarly, Melik and coworkers (Melik et al. 2008), and Burton and coworkers (Burton et al. 2019) developed LCR-type sensors for monitoring forces on lower body orthopedic implants as well as bone growth in osseointegrated implants, respectively. While these sensors provided real-time monitoring, they only operated when they were powered by an external device. Therefore, they were not suitable for continuous monitoring applications.
Compared to active sensors that can simultaneously measure multiple parameters and potentially provide comprehensive data on the in vivo physiological environments, passive sensors have relatively limited functionalities. However, passive sensors are still prevalent and have a significant place in the future of orthopedics. Passive sensors are simple, inexpensive, reliable, robust, and can be fabricated to be very small. In addition, the interest in biodegradable sensors that can be implemented for either short-term or long-term in vivo monitoring in orthopedic implants makes passive sensors crucial for orthopedic care since they are made from biodegradable materials.
For active implantable orthopedic sensors, the methods of wireless communication are paramount for their applicability and performance. Existing communication technologies such as Wi-Fi networks, Bluetooth, and Zigbee are frequently used by researchers (Baker 2005; Chakole et al. 2017). These wireless communication methods have their advantages and disadvantages, and the choice of modality depends on the distance of transmission, location of the device in the body as well as safety and security considerations. However, these communication methods will be critical for the development of future implantable orthopedic sensors because they allow flexibility for standardized transmission of in vivo physiological parameters, which coincides with the future trend of a more remote and personalized approach to healthcare.
8.3.2.2 New Innovations in Power Technologies
For active implantable devices, the method of powering them depends on the electronic circuit’s energy consumption rate, operational period, size constraints, and safety considerations (Nelson et al. 2020). For most implantable sensors, wireless communication is one of the major, if not the major, consumer of power (Mathúna et al. 2008). Communication power consumption depends on the microcontroller, antenna design, signal processing, and voltage levels. Compared to other commonly used communication protocols, Bluetooth is more optimized for power consumption since it can use a relayed transmission approach to maintain a linked connection between the implant and external devices (Nelson et al. 2020). Specifically, Bluetooth can form a network of devices, which is termed as the piconet, to link two or more devices together. Once on the network, the connected devices can serve as signal relays for one another to shorten the transmission distance for each device (Frenzel 2018). Since transmission power increases exponentially with distance, the shortening of transmission distance can result in lowering the overall power for a Bluetooth network. Aside from the choice of wireless communication method, power consumption by wireless communication can be reduced by minimizing the overhead of the microcontroller by dynamically adjusting the gain of the antenna and/or managing the transmission time (Nelson et al. 2020). These energy efficient communications are important for long-term monitoring of orthopedic regeneration, which may need to function for months to years inside the body.
Batteries are a crucial source of consistent power especially for implants that need to function continuously. However, they have a limited lifetime and their size prevents miniaturization of the implant (Mond and Proclemer 2011). To overcome these challenges, some wireless implants adopt rechargeable batteries that can be charged through various remote power methods (Nelson et al. 2020). Remote power can be transferred through RF or magnetic induction, ultrasound, and infrared (IR) light methods. RF or magnetic induction uses a coil antenna as a transmitter, where it generates electromagnetic (EM) waves that are received by a secondary coil that converts the EM energy into an electrical current (Nelson et al. 2020). Ultrasound is another mode of energy source that can remotely power the implant or charge its battery. It has higher energy transfer efficiency through greater distances and can be used in smaller implants. Although more complex to implement, ultrasound power has decreased tissue damage and lowered tissue heating compared to induction, making it a safer choice (Nelson et al. 2020). However, there are limitations with EM and acoustic remote power charging because the alignment between the implant and the external power source can significantly affect the power transfer efficiency. Nevertheless, advancements in charging systems can reliably resolve the time limitation for many orthopedic sensors.
IR-based remote power is a newer concept that is being explored to power or recharge implantable sensors. This method uses superficial photodetectors to receive near-infrared lights which are transmitted through the skin with relatively high efficiency (Goto et al. 2001). Another approach is the use of photovoltaic power because near-infrared light exhibits low attenuation in tissues. However, the effectiveness of these methods might vary from person to person and requires more research before it can be implemented clinically (Bereuter et al. 2017).
Energy harvesting is another promising research area. Some of the more common techniques include using solar energy or the motion of the body to generate power. Furthermore, utilizing the body’s thermal energy is being proposed (Stark and Stordeur 1999). Although thermal energy harvesting techniques had been previously reported in wearable devices, the production cost of the thermoelectric components was very high, making the sensors expensive (Stark and Stordeur 1999). Another energy harvesting scheme involves the use of piezoelectric (PZT) elements, which convert mechanical energy to produce electricity in vivo (Holmberg et al. 2013; Platt et al. 2005). These energy harvesting techniques will be able to address limitations in battery power and allow for more reliable implantable sensors that can be applied for long-term monitoring of orthopedic regeneration.
8.3.2.3 Development of Biocompatible and Absorbable Implantable Sensors
A critical requirement for implantable sensors is their ability to be functional and stable for a prolonged amount of time in the human body without inducing severe foreign body response. Foreign body responses such as fibrous encapsulation and inflammation are some of the limitations of implantable sensors based on Micro-Electro-Mechanical Systems (MEMS) due to the materials used to make these sensors (Bashir 2004; Gilleo 2005). Therefore, using similar biocompatible materials as those used in fabricating the prosthesis is the first step to minimize the host response from the implantable sensors themselves (O’Connor and Kiourti 2017). Approaches to make sensors more biocompatible include changes to packaging and polymer encapsulation, as well as using materials that are flexible or tissue mimicking. Flexible implants and biological materials that closely resemble tissue can reduce local damage, leading to reduced inflammation and minimized chance of a foreign body response (Pang et al. 2013). Parylene and polyimide are some of the most biocompatible polymers used to fabricate implantable MEMS (Pang et al. 2013).
Another approach to reducing host response is the development of biodegradable implantable sensors that break down into nontoxic components after a specified functional lifetime. The duration of function for biodegradable sensors can be modified through the choice of the encapsulating material and the surface area of the exposed electrodes (Klosterhoff et al. 2017a). Aside from their biocompatibility, biodegradable sensors are ideal for use because they remove the need for secondary surgery. In recent years, there have been encouraging new developments in biodegradable implantable sensors. One example of a biodegradable sensor is the passive wireless pressure sensor developed by Luo and coworkers (Luo et al. 2014), which was consisted of Poly (l-lactic acid) (PLLA) and polycaprolactone (PCL) for its structural and dielectric material while the conductive portion was made of Zinc/Iron bilayers.
While biodegradable implantable sensors are promising, they are all passive sensors due to the challenges in developing biodegradable batteries and biocompatible active electronic components. However, new advancements in degradable batteries and electronic components have made the development of biodegradable active sensors a real possibility. For example, Tsang and coworkers developed a magnesium/iron battery packaged in PCL, which had six times the energy density while being 1–2 orders smaller in volume (Tsang et al. 2015). Another similar battery technology consisted of sodium chloride and PCL as the electrochemical cell and used the fluid that entered the cell as the electrolyte (She et al. 2015). However, these batteries have only been benchtop tested and demonstration for in vivo application has yet to be performed.
Biodegradable electronic components have also been developed to realize a fully biodegradable implantable sensor. Zhang and coworkers developed conductive polymer-based biodegradable interconnects that were made with iron microparticles as a conductor and PCL as the insulating material (Yin et al. 2014). Furthermore, Kim and coworkers fabricated an electronic system consisting of biodegradable silk fibroin as a supporting substrate (Kim et al. 2010). The development of biodegradable electronics and batteries allows monitoring of orthopedic injuries for a controlled timeframe while avoiding the need for an additional surgery for the sensor removal after the monitoring period.
8.3.2.4 Conclusion
Extensive research and development have been conducted to apply wireless implantable sensors to orthopedics. However, wireless implantable sensors have not been widely adopted clinically due to various issues and are mostly limited for research with few products available commercially. The two notable wireless implantable sensors in the market are the VERASENSE by Orthosensor used in intraoperative monitoring in TKA procedure, and the open eDisk developed by Theken Disc for measuring motions and loads experienced by a spinal disc implant. Some of the challenges associated with implementing wireless sensors include regulatory and cost issues, lack of research on long-term effectiveness, biocompatibility as well as privacy and security concerns from the wireless signals (Karipott et al. 2018a). Besides these challenges, the future is promising for implantable wireless sensors due to the rapid developments in wireless technologies, electronics, biodegradable materials, and energy harvesting techniques, which can help address the current issues with power, biocompatibility, reliability, and size of the sensors.
8.3.3 Current Gaps in Knowledge and Technologies
8.3.3.1 Utilizing more Complex Trauma Models
The field of regenerative rehabilitation works to minimize complications seen with severe injuries that often effects bone, skeletal muscle, nerve, and vascular tissue. However, preclinical research lacks knowledge and utility of multi-tissue models and thus therapeutics. Well-characterized preclinical models with quantified outcomes for functional restoration are crucial testbeds for evaluating emerging technologies and rehabilitation. However, most musculoskeletal trauma models consist of single-tissue defects, which have an undeniable place in the field of regenerative medicine but have limited utility for investigating regenerative strategies for complex, multi-tissue defects. In summary, research laboratories have developed composite bone and vascular injury models, bone and nerve injury models, as well as bone and muscle injury models (Uhrig et al. 2013). However, preclinical research that utilizes these complex models are limited because of their added complexity. In order to advance functional interventions and address multi-tissue injuries, a greater understanding of the biological interactions between damaged tissue is required upon injury and throughout healing. Although certain therapeutics will exhibit promising results in one tissue, unwanted negative consequences could arise in other damaged tissues, as seen with early mechanical loading that affects bone and vascular tissue differently (Klosterhoff et al. 2020). Selection of the model type is paramount to in vivo research, and work with composite models could motivate multistage and multifaceted therapeutic strategies to better address more complicated injuries, with hopes of optimizing therapeutics for clinical use (Uhrig et al. 2013).
8.3.3.2 Optimizing Regeneration of all Tissue Types
Another common limitation in the field of regenerative medicine is reestablishing the correct cellular environment for all tissue types involved. In the context of complex bone injuries, this often means an environment to promote adequate osteogenesis and angiogenesis. Further, when utilizing mechanical loading as a rehabilitative strategy, biological control is extremely important because progenitor cells for bone, muscle, and vascular tissue are highly mechanosensitive (Claes and Heigele 1999; Kalfas 2001). Past work found the time of loading to be crucial for bone healing, and strain sensors found that different tissue types may require specific timing and magnitude of loading to optimize tissue regeneration (Klosterhoff et al. 2020). The biological intricacies involved in regenerative medicine is extremely complex, and utilizing loading strategies adds to the complexity. Preclinical research needs to continue in vitro and in vivo work to identify the mechanical thresholds needed to promote functional tissue healing in all tissue types as well as composite models. Further, research should continue to investigate the mechanical boundary conditions that optimize the therapeutic effects of rehabilitation. Additionally, the continued development of wireless strain sensor that ensure loading remains within the boundary conditions can allow for dynamic, patient-specific adjustments to the rehabilitation regimen with hopes of accelerating the functional regeneration of musculoskeletal tissue.
8.3.3.3 The Immune System’s Role in Bone Healing
Another emerging aspect of bone healing is the dysregulation of the systemic immune response following some severe bone injuries. This detrimental response involves dysregulation of the systemic inflammatory response and compensatory anti-inflammatory response following injury and is not well understood. The complications that arise from immune dysregulation often result in poor healing outcomes, which are devastating to patients. Novel research is investigating a potential link between systemic immune health and bone healing. This preclinical work is identifying cellular markers and cytokine levels that correlated to compromised bone healing (Ruehle et al. 2020). Future work could use these predictive markers as therapeutic targets. Additionally, research should consider how mechanical loading might modulate the immune response, as well as how the patients’ immune profile might impact the therapeutic effect of mechanical loading. The immune system plays a key role in tissue healing and regeneration, so future work should continue assessing immune cells at the time of injury and throughout the healing process.
8.3.3.4 Real-Time, Patient-Specific Monitoring for Clinical Application
One of the challenges in orthopedic regenerative medicine is the ability to accurately and continuously track the progression of key physiological parameters (Klosterhoff et al. 2017b). Therefore, technologies that enable real-time measurement of in vivo environmental conditions such as pH, temperature, and oxygen tension in orthopedic wound sites would provide great benefits to patient outcomes, as well as translatable knowledge to improve treatment approaches (Klosterhoff et al. 2017b). Today, preclinical and clinical methods used to quantify in vivo parameters in orthopedic regeneration are highly dependent on animal or human injury models (Klosterhoff et al. 2017b). Thus, platforms for longitudinal tracking of physiological cues in vivo can significantly increase the resolution and quantity of data acquisition from individual test subjects, which can lower the number of animals and/or human subjects needed for an adequately powered study (Klosterhoff et al. 2017b). Imaging modalities such as ultrasound strain imaging, shear wave elastography, and magnetic resonance imaging are also used in preclinical and clinical studies. However, these methods do not provide continuous measurement, are generally more expensive, and require a larger patient/animal sample size to be effective. On the other hand, FE analysis and computational fluid dynamic analysis are used to gather information such as the surface distribution of stress-strain and oxygen tension, but they are limited by assumed boundary conditions that are difficult to be validated without direct measurement with sensors (Klosterhoff et al. 2017b).
8.3.3.5 Miniaturizing Wireless Technologies
Advancements in MEMS and wireless technologies have allowed for the fabrication of small, flexible, and low-power implantable sensors that can be used in preclinical in vivo models and clinical settings. Miniaturized sensors fabricated for small animal models can wirelessly transmit quantitative measurement in real-time, eliminating the need to anesthetize the animal and disrupt normal activities (Klosterhoff et al. 2017b). Implementing minimally invasive implantable sensors in clinical settings has also improved the outcomes and safety of orthopedic regenerative therapies (Klosterhoff et al. 2017b).
8.3.3.6 Integration of Regenerative and Rehabilitation Strategies
The field of regenerative rehabilitation has suffered from a lack of integrated multidisciplinary research support to advance technology and current clinical standards. As a result, there is tremendous variability in treatment approaches and post-injury rehabilitation regimens. To help progress, multidisciplinary projects should focus on evidence-based guidelines to synergize regenerative therapies and rehabilitation protocols to functionally restore musculoskeletal tissue (Fig. 8.6).
Regenerative rehabilitation enabling technologies to invest complex bone injuries including (a) regenerative strategies such as BMP-2 delivery for bone regeneration (Kolambkar et al. 2011), (b) wireless strain sensors to monitor the strain in the defect region of segmental bone injuries (Klosterhoff et al. 2017a), (c) computational models to build predictive models related to optimal strain boundary conditions, and (d) integrating all of these strategies to optimize rehabilitation regimen for accelerated bone healing of complex bone injuries. Created with BioRender.com
In the long term, combining both regenerative medicines related to stem cells, orthobiologics, biomaterials, and tissue organoids with rehabilitation protocols related to functional imaging, assistive technologies, biophysical stimuli, and biosensors could optimize functional recovery and performance. Future integrative work should advance technologies and rehabilitative strategies that proactively avoid injury by promoting pre-injury reversal of tissue degeneration; improve post-injury rate and quality of healing; and decrease long-term pain and disability. In preclinical studies, research should focus on rigorous evaluations of regenerative rehabilitation strategies, predictive multivariate models of functional recovery, combined treatment related to regenerative medicine and rehabilitation, as well as evidence-based guidance that allows patient-specific treatment (Fig. 8.6). Focusing on these emerging aspects of regenerative rehabilitation will help patient outcomes because the rehabilitative protocol will rely on patient-specific factors to accelerated functional regeneration and overall recovery.
References
Ai-Aql ZS, Alagl AS, Graves DT, Gerstenfeld LC, Einhorn TA (2008) Molecular mechanisms controlling bone formation during fracture healing and distraction osteogenesis. J Dent Res 87:107–118. https://doi.org/10.1177/154405910808700215
Alierta JA, Pérez MA, García-Aznar JM (2014) An interface finite element model can be used to predict healing outcome of bone fractures. J Mech Behav Biomed Mater 29:328–338. https://doi.org/10.1016/j.jmbbm.2013.09.023
Ament C, Hofer EP (2000) A fuzzy logic model of fracture healing. J Biomech 33:961–968. https://doi.org/10.1016/s0021-9290(00)00049-x
Arazi M, Oğün TC, Oktar MN, Memik R, Kutlu A (2001) Early weight-bearing after statically locked reamed intramedullary nailing of comminuted femoral fractures: is it a safe procedure? J Trauma 50:711–716. https://doi.org/10.1097/00005373-200104000-00019
Aronson JMD (1994) Experimental and clinical experience with distraction osteogenesis. Cleft Palate Craniofac J 31:473–482
Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, Ziran BH, Stahel PF (2008) A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: open reduction and internal fixation versus external ilizarov fixation. Injury 39:196–202. https://doi.org/10.1016/j.injury.2007.09.003
Bailón-Plaza A, van der Meulen MC (2001) A mathematical framework to study the effects of growth factor influences on fracture healing. J Theor Biol 212:191–209. https://doi.org/10.1006/jtbi.2001.2372
Bailón-Plaza A, van der Meulen MCH (2003) Beneficial effects of moderate, early loading and adverse effects of delayed or excessive loading on bone healing. J Biomech 36:1069–1077. https://doi.org/10.1016/S0021-9290(03)00117-9
Baker N (2005) ZigBee and Bluetooth: strengths and weaknesses for industrial applications. Comput Control Eng 16:20–25. https://doi.org/10.1049/cce:20050204
Bashir R (2004) BioMEMS: state-of-the-art in detection, opportunities and prospects. Adv Drug Deliv Rev 56:1565–1586. https://doi.org/10.1016/j.addr.2004.03.002
Beaupré GS, Orr TE, Carter DR (1990) An approach for time-dependent bone modeling and remodeling—theoretical development. J Orthop Res 8:651–661. https://doi.org/10.1002/jor.1100080506
Bereuter L, Williner S, Pianezzi F, Bissig B, Buecheler S, Burger J, Vogel R, Zurbuchen A, Haeberlin A (2017) Energy harvesting by subcutaneous solar cells: a long-term study on achievable energy output. Ann Biomed Eng 45:1172–1180. https://doi.org/10.1007/s10439-016-1774-4
Bergmann G, Graichen F, Bender A, Kääb M, Rohlmann A, Westerhoff P (2007) In vivo glenohumeral contact forces--measurements in the first patient 7 months postoperatively. J Biomech 40:2139–2149. https://doi.org/10.1016/j.jbiomech.2006.10.037
Boerckel JD, Uhrig BA, Willett NJ, Huebsch N, Guldberg RE (2011) Mechanical regulation of vascular growth and tissue regeneration in vivo. Proc Natl Acad Sci 108:E674–E680
Boerckel JD, Kolambkar YM, Stevens HY, Lin AS, Dupont KM, Guldberg RE (2012) Effects of in vivo mechanical loading on large bone defect regeneration. J Orthop Res 30:1067–1075
Borchani W, Aono K, Lajnef N, Chakrabartty S (2016) Monitoring of postoperative bone healing using smart trauma-fixation device with integrated self-powered piezo-floating-gate sensors. IEEE Trans Biomed Eng 63:1463–1472. https://doi.org/10.1109/TBME.2015.2496237
Brand RA (2010) Biographical sketch: Julius Wolff, 1836–1902. Clin Orthop Relat Res 468:1047–1049. https://doi.org/10.1007/s11999-010-1258-z
Brumback RJ, Toal TR Jr, Murphy-Zane MS, Novak VP, Belkoff SM (1999) Immediate weight-bearing after treatment of a comminuted fracture of the femoral shaft with a statically locked intramedullary nail. J Bone Joint Surg Am 81:1538–1544. https://doi.org/10.2106/00004623-199911000-00005
Burny F, Donkerwolcke M, Moulart F, Bourgois R, Puers R, Van Schuylenbergh K, Barbosa M, Paiva O, Rodes F, Bégueret JB, Lawes P (2000) Concept, design and fabrication of smart orthopedic implants. Med Eng Phys 22:469–479. https://doi.org/10.1016/s1350-4533(00)00062-x
Burton AR, Sun P, Lynch JP (2019) Bio-compatible wireless inductive thin-film strain sensor for monitoring the growth and strain response of bone in osseointegrated prostheses. Struct Health Monit 1475921719831452. https://doi.org/10.1177/1475921719831452
Byrne DP, Lacroix D, Prendergast PJ (2011) Simulation of fracture healing in the tibia: mechanoregulation of cell activity using a lattice modeling approach. J Orthop Res 29:1496–1503. https://doi.org/10.1002/jor.21362
Carlier A, Geris L, Lammens J, Oosterwyck HV (2015) Bringing computational models of bone regeneration to the clinic. WIREs Syst Biol Med 7:183–194. https://doi.org/10.1002/wsbm.1299
Carter DR, Fyhrie DP, Whalen RT (1987) Trabecular bone density and loading history: regulation of connective tissue biology by mechanical energy. J Biomech 20:785–794. https://doi.org/10.1016/0021-9290(87)90058-3
Carter DR, Beaupré GS, Giori NJ, Helms JA (1998) Mechanobiology of skeletal regeneration. Clin Orthop Relat Res (1976–2007) 355:S41
Chakole MS, Jibhkate RR, Choudhari AV, Gawali SR, Tule PR (2017) A healthcare monitoring system using. WiFi Module 04:5
Checa S, Prendergast PJ (2009) A mechanobiological model for tissue differentiation that includes angiogenesis: a lattice-based modeling approach. Ann Biomed Eng 37:129–145. https://doi.org/10.1007/s10439-008-9594-9
Cheng A, Krishnan L, Pradhan P, Weinstock LD, Wood LB, Roy K, Guldberg RE (2019) Impaired bone healing following treatment of established nonunion correlates with serum cytokine expression: cytokines correlate with nonunion healing. J Orthop Res 37:299–307. https://doi.org/10.1002/jor.24186
Cheville AL, Smith SR, Basford JR (2018) Rehabilitation medicine approaches to pain management. Hematology/Oncology Clinics of North America, Pain Control 32:469–482. https://doi.org/10.1016/j.hoc.2018.02.001
Claes LE, Heigele CA (1999) Magnitudes of local stress and strain along bony surfaces predict the course and type of fracture healing. J Biomech 32:255–266. https://doi.org/10.1016/s0021-9290(98)00153-5
Clausen I, Glott T (2014) Development of clinically relevant implantable pressure sensors: perspectives and challenges. Sensors (Basel) 14:17686–17702. https://doi.org/10.3390/s140917686
Colnot C, Thompson Z, Miclau T, Werb Z, Helms JA (2003) Altered fracture repair in the absence of MMP9. Development 130:4123–4133. https://doi.org/10.1242/dev.00559
Compton J, Fragomen A, Rozbruch SR (2015) Skeletal repair in distraction osteogenesis: mechanisms and enhancements. JBJS Rev 3:1. https://doi.org/10.2106/JBJS.RVW.N.00107
Deramo P, Rose J (2020) Flaps, muscle and musculocutaneous. StatPearls, Treasure Island (FL)
DeRouin AJ, Pacella N, Zhao C, An K, Ong KG (2016) A wireless sensor for real-time monitoring of tensile force on sutured wound sites. IEEE Trans Biomed Eng. https://doi.org/10.1109/TBME.2015.2470248
Egol KA, Koval KJ, Zuckerman JD (2010) Handbook of fractures, 4th edn. Lippincott Williams & Wilkins, Philadelphia, PA
Elliott DS, Newman KJH, Forward DP, Hahn DM, Ollivere B, Kojima K, Handley R, Rossiter ND, Wixted JJ, Smith RM, Moran CG (2016) A unified theory of bone healing and nonunion: BHN theory. Bone Joint J 98-B:884–891. https://doi.org/10.1302/0301-620X.98B7.36061
Frenzel LE (2018) Chapter 9 - networking: wired and wireless: all devices talking to one another. In: Electronics explained, 2nd edn. Newnes, London
Fyhrie DP, Carter DR (1986) A unifying principle relating stress to trabecular bone morphology. J Orthop Res 4:304–317. https://doi.org/10.1002/jor.1100040307
Ganadhiepan G, Zhang L, Miramini S, Mendis P, Patel M, Ebeling P, Wang Y (2019) The effects of dynamic loading on bone fracture healing under ilizarov circular fixators. J Biomech Eng 141:051005. https://doi.org/10.1115/1.4043037
Gardner TN, Stoll T, Marks L, Mishra S, Knothe Tate M (2000) The influence of mechanical stimulus on the pattern of tissue differentiation in a long bone fracture — an FEM study. J Biomech 33:415–425. https://doi.org/10.1016/S0021-9290(99)00189-X
Geris L, Gerisch A, Sloten JV, Weiner R, Oosterwyck HV (2008) Angiogenesis in bone fracture healing: a bioregulatory model. J Theor Biol 251:137–158. https://doi.org/10.1016/j.jtbi.2007.11.008
Geris L, Sloten JV, Oosterwyck HV (2010) Connecting biology and mechanics in fracture healing: an integrated mathematical modeling framework for the study of nonunions. Biomech Model Mechanobiol 9:713–724. https://doi.org/10.1007/s10237-010-0208-8
Gilleo K (2005) MEMS in medicine. Circuit. Assembly 16:32–33
Goto K, Nakagawa T, Nakamura O, Kawata S (2001) An implantable power supply with an optically rechargeable lithium battery. IEEE Trans Biomed Eng 48:830–833. https://doi.org/10.1109/10.930908
Graichen F, Arnold R, Rohlmann A, Bergmann G (2007) Implantable 9-channel telemetry system for in vivo load measurements with orthopedic implants. IEEE Trans Biomed Eng 54:253–261. https://doi.org/10.1109/TBME.2006.886857
Greising SM, Corona BT, Call JA (2020) Musculoskeletal regeneration, rehabilitation, and plasticity following traumatic injury. Int J Sports Med 41:495–504. https://doi.org/10.1055/a-1128-7128
Guder C, Gravius S, Burger C, Wirtz DC, Schildberg FA (2020) Osteoimmunology: a current update of the interplay between bone and the immune system. Front Immunol 11:58
Guldberg RE, Caldwell NJ, Guo XE, Goulet RW, Hollister SJ, Goldstein SA (1997) Mechanical stimulation of tissue repair in the hydraulic bone chamber. J Bone Miner Res 12:1295–1302. https://doi.org/10.1359/jbmr.1997.12.8.1295
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2017) A targeted approach to ligament balancing using kinetic sensors. J Arthroplast 32:2127–2132. https://doi.org/10.1016/j.arth.2017.02.021
Hernandez CJ (2000) A model of mechanobiologic and metabolic influences on bone adaptation. J Rehabil Res Dev 37(2):235–244. PMID: 10850830
Holmberg J, Alexander L, Rajamani R, Bechtold JE (2013) Battery-less wireless instrumented knee implant. J Med Devices 7:011006. https://doi.org/10.1115/1.4023412
Hoyt BW, Pavey GJ, Pasquina PF, Potter BK (2015) Rehabilitation of lower extremity trauma: a review of principles and military perspective on future directions. Curr Trauma Rep 1:50–60. https://doi.org/10.1007/s40719-014-0004-5
Huiskes R, Driel WDV, Prendergast PJ, Søballe K (1997) A biomechanical regulatory model for periprosthetic fibrous-tissue differentiation. J Mater Sci Mater Med 8:785–788. https://doi.org/10.1023/A:1018520914512
Hurkmans HL, Bussmann JB, Selles RW, Benda E, Stam HJ, Verhaar JA (2007) The difference between actual and prescribed weight bearing of total hip patients with a trochanteric osteotomy: long-term vertical force measurements inside and outside the hospital. Arch Phys Med Rehabil 88:200–206. https://doi.org/10.1016/j.apmr.2006.11.005
Ilfeld BM, Duke KB, Donohue MC (2010) The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg 111:1552–1554. https://doi.org/10.1213/ANE.0b013e3181fb9507
Inverarity L (2020) Weight-bearing restrictions and activity after surgery [WWW document]. Verywell Health. URL https://www.verywellhealth.com/weight-bearing-restrictions-2696668 (accessed 2.26.21)
Joslin CC, Eastaugh-Waring SJ, Hardy JRW, Cunningham JL (2008) Weight bearing after tibial fracture as a guide to healing. Clin Biomech (Bristol, Avon) 23:329–333. https://doi.org/10.1016/j.clinbiomech.2007.09.013
Kalfas IH (2001) Principles of bone healing. Neurosurg Focus 10:1–4. https://doi.org/10.3171/foc.2001.10.4.2
Kannan RY, Salacinski HJ, Sales K, Butler P, Seifalian AM (2005) The roles of tissue engineering and vascularisation in the development of micro-vascular networks: a review. Biomaterials 26:1857–1875
Karipott SS, Nelson BD, Guldberg RE, Ong KG (2018a) Clinical potential of implantable wireless sensors for orthopedic treatments. Expert Rev Med Devices 15:255–264. https://doi.org/10.1080/17434440.2018.1454310
Karipott SS, Veetil PM, Nelson BD, Guldberg RE, Ong KG (2018b) An embedded wireless temperature sensor for orthopedic implants. IEEE Sensors J 18:1265–1272. https://doi.org/10.1109/JSEN.2017.2780226
Kenwright J, Goodship AE (1989) Controlled mechanical stimulation in the treatment of tibial fractures. Clin Orthop Relat Res 241:36–47
Kershaw CJ, Cunningham JL, Kenwright J (1993) Tibial external fixation, weight bearing, and fracture movement. Clin Orthop Relat Res (293):28–36
Kim D-H, Viventi J, Amsden JJ, Xiao J, Vigeland L, Kim Y-S, Blanco JA, Panilaitis B, Frechette ES, Contreras D, Kaplan DL, Omenetto FG, Huang Y, Hwang K-C, Zakin MR, Litt B, Rogers JA (2010) Dissolvable films of silk fibroin for ultrathin conformal bio-integrated electronics. Nat Mater 9:511–517. https://doi.org/10.1038/nmat2745
Klosterhoff BS, Tsang MM, She D, Ong KG, Allen MG, Willett NJ, Guldberg RE (2017a) Implantable sensors for regenerative medicine. J Biomech Eng 139(2). https://doi.org/10.1115/1.4035436
Klosterhoff BS, Ghee Ong K, Krishnan L, Hetzendorfer KM, Chang Y-H, Allen MG, Guldberg RE, Willett NJ (2017b) Wireless implantable sensor for noninvasive, longitudinal quantification of axial strain across rodent long bone defects. J Biomech Eng 139(11):111004-8. https://doi.org/10.1115/1.4037937
Klosterhoff BS, Kaiser J, Nelson BD, Karipott SS, Ruehle MA, Hollister SJ, Weiss JA, Ong KG, Willett NJ, Guldberg RE (2020) Wireless sensor enables longitudinal monitoring of regenerative niche mechanics during rehabilitation that enhance bone repair. Bone 135:115311. https://doi.org/10.1016/j.bone.2020.115311
Koike N, Fukumura D, Gralla O, Au P, Schechner JS, Jain RK (2004) Creation of long-lasting blood vessels. Nature 428:138–139
Kolambkar YM, Dupont KM, Boerckel JD, Huebsch N, Mooney DJ, Hutmacher DW, Guldberg RE (2011) An alginate-based hybrid system for growth factor delivery in the functional repair of large bone defects. Biomaterials 32:65–74
Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, Heislein DM, Mustafa J, Pardasaney P, Giorgetti M, Holt N, Goehring L, Jette AM (2014) Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture a randomized clinical trial. JAMA 311:700–708. https://doi.org/10.1001/jama.2014.469
Ledet EH, Tymeson MP, Dirisio DJ, Cohen B, Uhl RL (2005) Direct real-time measurement of in vivo forces in the lumbar spine. Spine J 5:85–94
Ledet EH, D’Lima D, Westerhoff P, Szivek JA, Wachs RA, Bergmann G (2012) Implantable sensor technology: from research to clinical practice. J Am Acad Orthop Surg 20:383–392. https://doi.org/10.5435/JAAOS-20-06-383
Ledet EH, Liddle B, Kradinova K, Harper S (2018) Smart implants in orthopedic surgery, improving patient outcomes: a review. Innov Entrep Health 5:41–51. https://doi.org/10.2147/IEH.S133518
Levenston ME, Beaupré GS, Schurman DJ, Carter DR (1993) Computer simulations of stress-related bone remodeling around noncemented acetabular components. J Arthroplast 8:595–605. https://doi.org/10.1016/0883-5403(93)90006-P
Lin S-J, Chen C-L, Peng K-T, Hsu W-H (2014) Effect of fragmentary displacement and morphology in the treatment of comminuted femoral shaft fractures with an intramedullary nail. Injury 45:752–756. https://doi.org/10.1016/j.injury.2013.10.015
Liu RW, Kim YH, Lee DC, Inoue N, Koo TK, Chao EYS (2005) Computational simulation of axial dynamization on long bone fractures. Clin Biomech 20:83–90. https://doi.org/10.1016/j.clinbiomech.2004.08.009
Loboa EG, Wren TAL, Beaupré GS, Carter DR (2003) Mechanobiology of soft skeletal tissue differentiation—a computational approach of a fiber-reinforced poroelastic model based on homogeneous and isotropic simplifications. Biomech Model Mechanobiol 2:83–96. https://doi.org/10.1007/s10237-003-0030-7
Loeb GE, Richmond FJR, Baker LL (2006) The BION devices: injectable interfaces with peripheral nerves and muscles. Neurosurg Focus 20:E2. https://doi.org/10.3171/foc.2006.20.5.3
Long WT, Ward SR, Dorr LD, Raya J, Boutary M, Sirianni LE (2006) Postoperative pain management following total knee arthroplasty: a randomized comparison of continuous epidural versus femoral nerve infusion. J Knee Surg 19:137–143. https://doi.org/10.1055/s-0030-1248096
Lord JM, Midwinter MJ, Chen Y-F, Belli A, Brohi K, Kovacs EJ, Koenderman L, Kubes P, Lilford RJ (2014) The systemic immune response to trauma: an overview of pathophysiology and treatment. Lancet 384:1455–1465. https://doi.org/10.1016/S0140-6736(14)60687-5
Luo M, Martinez AW, Song C, Herrault F, Allen MG (2014) A microfabricated wireless rf pressure sensor made completely of biodegradable materials. J Microelectromech Syst 23:4–13. https://doi.org/10.1109/JMEMS.2013.2290111
Masquelet AC (2003) Muscle reconstruction in reconstructive surgery: soft tissue repair and long bone reconstruction. Langenbeck’s Arch Surg 388:344–346. https://doi.org/10.1007/s00423-003-0379-1
Mathúna CÓ, O’Donnell T, Martinez-Catala RV, Rohan J, O’Flynn B (2008) Energy scavenging for long-term deployable wireless sensor networks. Talanta, Special Section: Remote Sensing 75:613–623. https://doi.org/10.1016/j.talanta.2007.12.021
McKibbin B (1978) The biology of fracture healing in long bones. J Bone Joint Surg Br 60-B:150–162. https://doi.org/10.1302/0301-620X.60B2.350882
Mehboob A, Chang S-H (2018) Biomechanical simulation of healing process of fractured femoral shaft applied by composite intramedullary nails according to fracture configuration. Compos Struct 185:81–93. https://doi.org/10.1016/j.compstruct.2017.11.002
Melik R, Perkgoz NK, Unal E, Puttlitz C, Demir HV (2008) Bio-implantable passive on-chip RF-MEMS strain sensing resonators for orthopaedic applications. J Micromech Microeng 18:115017. https://doi.org/10.1088/0960-1317/18/11/115017
Mitkovic MB, Bumbasirevic MZ, Lesic A, Golubovic Z (2002) Dynamic external fixation of comminuted intra-articular fractures of the distal tibia (type C pilon fractures). Acta Orthop Belg 68:508–514
Mond HG, Proclemer A (2011) The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009--a World Society of Arrhythmia’s project. Pacing Clin Electrophysiol 34:1013–1027. https://doi.org/10.1111/j.1540-8159.2011.03150.x
Nauth A, McKee MD, Einhorn TA, Watson JT, Li R, Schemitsch EH (2011) Managing bone defects. J Orthop Trauma 25:462–466. https://doi.org/10.1097/BOT.0b013e318224caf0
Nelson BD, Karipott SS, Wang Y, Ong KG (2020) Wireless technologies for implantable devices. Sensors 20:4604. https://doi.org/10.3390/s20164604
O’Connor C, Kiourti A (2017) Wireless sensors for smart orthopedic implants. J Bio Tribo Corros 3:20. https://doi.org/10.1007/s40735-017-0078-z
Oess NP, Weisse B, Nelson B (2009) Magnetoelastic strain sensor for optimized assessment of bone fracture fixation. IEEE Sensors J. https://doi.org/10.1109/JSEN.2009.2025575
Olesen UK, Eckardt H, Bosemark P, Paulsen AW, Dahl B, Hede A (2015) The Masquelet technique of induced membrane for healing of bone defects. A review of 8 cases. Injury. https://doi.org/10.1016/S0020-1383(15)30054-1
Osterweis M, Kleinman A, Mechanic D (1987) Rehabilitation approaches and issues in chronic pain, pain and disability: clinical, behavioral, and public policy perspectives. National Academies Press (US), Washington, DC
Pacella N, DeRouin A, Pereles B, Ong KG (2014) Geometrical modification of magnetoelastic sensors to enhance sensitivity. Smart Mater Struct 24:025018. https://doi.org/10.1088/0964-1726/24/2/025018
Pang C, Lee C, Suh K-Y (2013) Recent advances in flexible sensors for wearable and implantable devices. J Appl Polym Sci 130:1429–1441. https://doi.org/10.1002/app.39461
Peiffer V, Gerisch A, Vandepitte D, Van Oosterwyck H, Geris L (2011) A hybrid bioregulatory model of angiogenesis during bone fracture healing. Biomech Model Mechanobiol 10:383–395. https://doi.org/10.1007/s10237-010-0241-7
Platt SR, Farritor S, Garvin K, Haider H (2005) The use of piezoelectric ceramics for electric power generation within orthopedic implants. IEEE/ASME Transactions on Mechatronics 10:455–461. https://doi.org/10.1109/TMECH.2005.852482
Potkay JA (2008) Long term, implantable blood pressure monitoring systems. Biomed Microdevices 10:379–392. https://doi.org/10.1007/s10544-007-9146-3
Rohlmann A, Schwachmeyer V, Graichen F, Bergmann G (2014) Spinal loads during post-operative physiotherapeutic exercises. PLoS One 9:e102005. https://doi.org/10.1371/journal.pone.0102005
Rosenthal MD, Moore FA (2016) Persistent inflammation, immunosuppression, and catabolism: evolution of multiple organ dysfunction. Surg Infect 17:167–172. https://doi.org/10.1089/sur.2015.184
Ruehle MA, Li M-TA, Cheng A, Krishnan L, Willett NJ, Guldberg RE (2019) Decorin-supplemented collagen hydrogels for the co-delivery of bone morphogenetic protein-2 and microvascular fragments to a composite bone-muscle injury model with impaired vascularization. Acta Biomater 93:210–221. https://doi.org/10.1016/j.actbio.2019.01.045
Ruehle MA, Eastburn EA, LaBelle SA, Krishnan L, Weiss JA, Boerckel JD, Wood LB, Guldberg RE, Willett NJ (2020) Extracellular matrix compression temporally regulates microvascular angiogenesis. Sci Adv 6:eabb6351. https://doi.org/10.1126/sciadv.abb6351
Rydell NW (1966) Forces acting on the femoral head-prosthesis: a study on strain gauge supplied prostheses in living persons. Acta Orthop Scand 37:1–132. https://doi.org/10.3109/ort.1966.37.suppl-88.01
Sato K, Kikuchi S, Yonezawa T (1999) In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine (Phila Pa 1976) 24:2468–2474. https://doi.org/10.1097/00007632-199912010-00008
She D, Tsang M, Kim J, Allen M (2015) Immobilized electrolyte biodegradable batteries for implantable MEMS. 2015 Transducers – 2015 18th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS). https://doi.org/10.1109/TRANSDUCERS.2015.7180968
Shefelbine SJ, Augat P, Claes L, Simon U (2005) Trabecular bone fracture healing simulation with finite element analysis and fuzzy logic. J Biomech 38:2440–2450. https://doi.org/10.1016/j.jbiomech.2004.10.019
Soares dos Santos MP, Ferreira JAF, Ramos A, Simões JAO, Morais R, Silva NM, Santos PM, Reis MJCS, Oliveira T (2013) Instrumented hip implants: electric supply systems. J Biomech 46:2561–2571. https://doi.org/10.1016/j.jbiomech.2013.08.002
Stark I, Stordeur M (1999) New micro thermoelectric devices based on bismuth telluride-type thin solid films. In: Eighteenth International Conference on Thermoelectrics Proceedings, ICT’99 (Cat. No.99TH8407). IEEE, Piscataway. https://doi.org/10.1109/ICT.1999.843432
Stevens SS, Beaupré GS, Carter DR (1999) Computer model of endochondral growth and ossification in long bones: biological and mechanobiological influences. J Orthop Res 17:646–653. https://doi.org/10.1002/jor.1100170505
Stucky F, Vesin J-M, Kayser B, Uva B (2018) The effect of lower-body positive pressure on the cardiorespiratory response at rest and during submaximal running exercise. Front Physiol 9:34. https://doi.org/10.3389/fphys.2018.00034
Szivek JA, Roberto RF, Margolis DS (2005) In vivo strain measurements from hardware and lamina during spine fusion. J Biomed Mater Res B Appl Biomater 75:243–250. https://doi.org/10.1002/jbm.b.30262
Taljanovic MS, Jones MD, Ruth JT, Benjamin JB, Sheppard JE, Hunter TB (2003) Fracture fixation. Radiographics 23:1569–1590. https://doi.org/10.1148/rg.236035159
Tsang M, Armutlulu A, Martinez AW, Allen SA, Allen M (2015) Biodegradable magnesium/iron batteries with polycaprolactone encapsulation: a microfabricated power source for transient implantable devices. Microsystems Nanoeng. https://doi.org/10.1038/MICRONANO.2015.24
Uhrig BA, Li M-TA, Willett NJ, Guldberg RE (2013) Models of composite bone and soft-tissue limb trauma. In: Ma PX (ed) Biomaterials and regenerative medicine. Cambridge University Press, Cambridge, pp 534–554. https://doi.org/10.1017/CBO9780511997839.035
Vantucci CE, Roy K, Guldberg RE (2018) Immunomodulatory strategies for immune dysregulation following severe musculoskeletal trauma. J Immunol Regen Med 2:21–35. https://doi.org/10.1016/j.regen.2018.07.001
Vlaisavljevich E, Holmes HR, Tan EL, Qian Z, Trierweiler S, Ong KG, Rajachar RM (2013) Magnetoelastic vibrational biomaterials for real-time monitoring and modulation of the host response. J Mater Sci Mater Med 24:1093–1104. https://doi.org/10.1007/s10856-013-4854-0
Willett NJ, Li M-TA, Uhrig BA, Boerckel JD, Huebsch N, Lundgren TS, Warren GL, Guldberg RE (2013) Attenuated human bone morphogenetic protein-2–mediated bone regeneration in a rat model of composite bone and muscle injury. Tissue Eng Part C Methods 19:316–325. https://doi.org/10.1089/ten.tec.2012.0290
Wilson CJ, Schütz MA, Epari DR (2017) Computational simulation of bone fracture healing under inverse dynamization. Biomech Model Mechanobiol 16:5–14. https://doi.org/10.1007/s10237-016-0798-x
Wolff J (1892) Das gesetz der transformation der knochen. A Hirshwald 1:1–152
Wong TM, Lau TW, Li X, Fang C, Yeung K, Leung F (2014) Masquelet technique for treatment of posttraumatic bone defects. ScientificWorldJournal 2014:710302. https://doi.org/10.1155/2014/710302
Wren TA, Beaupré GS, Carter DR (2000) Tendon and ligament adaptation to exercise, immobilization, and remobilization. J Rehabil Res Dev 37:217–224
Yazar S, Lin C-H, Wei F-C (2004) One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg 114:1457–1466. https://doi.org/10.1097/01.PRS.0000138811.88807.65
Yin L, Huang X, Xu H, Zhang Y, Lam J, Cheng J, Rogers JA (2014) Materials, designs, and operational characteristics for fully biodegradable primary batteries. Adv Mater 26:3879–3884. https://doi.org/10.1002/adma.201306304
Zadeh LA (1965) Fuzzy sets. Inf Control 8:338–353. https://doi.org/10.1016/S0019-9958(65)90241-X
Zlowodzki M, Vogt D, Cole PA, Kregor PJ (2007) Plating of femoral shaft fractures: open reduction and internal fixation versus submuscular fixation. J Trauma Acute Care Surg 63:1061–1065. https://doi.org/10.1097/TA.0b013e318154c0b4
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Nash, K.E. et al. (2022). Regenerative Rehabilitation Strategies for Complex Bone Injuries. In: Greising, S.M., Call, J.A. (eds) Regenerative Rehabilitation. Physiology in Health and Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-95884-8_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-95884-8_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95883-1
Online ISBN: 978-3-030-95884-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)