Abstract
An overview of implantable measurement systems suitable for the long-term, continuous monitoring of blood pressure is presented in this paper. The challenges, design considerations and tradeoffs inherent in these systems are overviewed and implantable sensors from both industrial and research environments are reviewed. The paper is concluded with an outlook of future directions for implantable blood pressure monitoring systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Long-term, continuous blood pressure monitoring is critically needed for a number of applications including the monitoring of an animal’s cardiovascular function in genetic and disease research (Whitesall et al. 2004), to monitor repaired aneurysms (Allen 2005), for the measurement of the intracardiac pressure of patients with congestive heart failure (Becker 2006), and for the monitoring of patients with a spinal cord injury (SCI; The National Spinal Cord Injury Association 2006). Furthermore, long term monitoring of a person’s blood pressure may lead to the early diagnosis of health problems and reduced health care costs (Mayo Clinic Staff 2006; O’Brien et al. 2003).
The most common methods for blood pressure measurement are through the use of an external cuff or through a catheter-based system. The fundamental reasons that these methods fail for long term, continuous pressure measurement are comfort, intermittent measurement, occlusion of blood flow, and percutaneous connections (e.g. an external cuff utilizing the oscillatory method; Staessen et al. 2000). In addition, non-invasive blood pressure measurements are usually less accurate and stable than invasive methods (Triedman and Saul 1994; Epstein et al. 1991; Kemmotsu et al. 1991; Kermode et al. 1989). Methods using a catheterization procedure and a pressure transducer, on the other hand, are very accurate, but prohibit free movement of the subject and may be unsafe for long-term use due complications such as trauma to the arterial vessel and infection (Bowdle 2002; Scheer et al. 2002; Frezza and Mezghebe 1998; Wilkins 1985). One solution that does not occlude flow or prohibit free movement and can provide continuous, accurate data is an implantable device. In addition, in certain cases, such as when the blood pressure at a specific area of the body needs to be monitored over an extended period of time, implantable devices may provide the only possible solution.
The ability to create long-term, implantable blood pressure measurement systems is the culmination of many technological advancements in the fields of electrical and biomedical engineering. The first of these advancements was the development of wireless power transmission and transformers by Nikola Tesla in the late 1800s (Tesla 1900, 1897). The theory of loosely coupled transformers, now used for power and data transfer, was fully developed by Terman in 1943 (Terman 1943). The next major advancement was the invention of the transistor in 1948 and the subsequent progress in the field of microelectronics driven by Moore’s Law. These developments led to a reduction in the size and power consumption of electronic circuitry and, thus, the size of implanted systems. The combination of microelectronic circuits and wireless technology led to the first efforts in the 1960s and 1970s towards developing implantable pressure sensors (Van Citters et al. 1966; Olsen et al. 1967; Casadei et al. 1972; Cooper and Beale 1977). The next major advancement was the development of micro-electro-mechanical systems (MEMS) technology (Petersen 1982; Wise and Clark 1978), spurred by microelectronic fabrication technology; MEMS technology enabled the creation of miniature sensors (Lee and Wise 1982) and integration of the sensor and circuitry on the same silicon chip (Borky and Wise 1979), further minimizing the total size of the system. Developments in biomaterials and packaging for implants (Ratner et al. 2004) were the final major advancement enabling the creation of long-term, implantable blood pressure monitoring systems. This development has occurred over many years and has increased the biocompatibility, performance, and lifetime of the system when implanted. However, all of these areas continue to advance, promising to enable new implantable pressure sensors with increased performance, lifetime, and biocompatibility.
This paper reviews the work and progress in the area of continuous, long-term, implantable blood pressure sensors and monitors; it is separated into four sections. First, the device and system design issues and challenges of these systems are considered. Then, the current methods, products, and research for intra-arterial and extra-arterial blood pressure measurement are covered. Finally, the paper is wrapped up with an outlook for the future application of implantable blood pressure monitors.
2 System overview and considerations
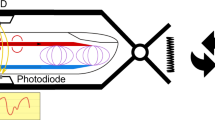
A block diagram of a generic implantable blood pressure sensing system is shown in Fig. 1 showing the various components in the system. The implanted sensor is shown on the right and is encapsulated in a biocompatible package. The external block on the left is needed to interface with, possibly provide power to, and download data from the implanted sensor. Wireless data transfer is utilized, as wired communication is unsuitable for long-term applications in which the patient is freely moving. A more in depth look at the sensor and circuitry considerations, data and power transfer, and biological and implant considerations of these systems is given in the following subsections.
2.1 Sensor and circuitry considerations
There are a number of important considerations for the sensor and circuitry in an implanted blood pressure monitoring system, many of which strongly depend on the application. First, the sensor should have an appropriate measurement range and signal bandwidth, high resolution and accuracy, and low signal drift. Resolution and accuracy are related, but not equivalent. Accuracy is the ability of the sensor to measure the true or actual value. Resolution is the smallest signal change that the sensor can distinguish. A sensor can have excellent resolution, but poor accuracy (e.g. if it has not been calibrated). The converse is not true. A list of sensing requirements for common ailments is given in Table 1. As can be seen, the required sensing parameters vary strongly based on the application. For example, heart failure is typically monitored by measuring the pressure in the pulmonary artery. This application requires a small measurement range and high resolution and bandwidth, but can tolerate a larger device due to the size of the pulmonary artery. On the other hand, coronary heart disease is monitored at the site of blockage in the coronary arteries and requires a large measurement range and very small device. Figure 2 shows a typical arterial blood pressure waveform with a blood pressure of 115/80 mmHg and a heart rate of 60 beats per minute (bpm). However, blood pressure and heart rate can vary between 40 and 250 mmHg and 40 and 200 bpm, respectively. Thus, for ailments such as hypertension and autonomic dysreflexia, a measurement range from 20 to 250 mmHg, a resolution of a couple mmHg, and a bandwidth of 20 Hz are sufficient (Webster 1997). However, applications interested in other features of the blood pressure waveform (such as aortic valve closure) may require much higher resolution and larger bandwidth (up to 200 Hz; Najafi and Ludomirsky 2004).
In addition to the device’s resolution, signal drift may also affect the accuracy of the measurement over time; it can be grouped into two categories and has two main causes. The two categories are offset drift and sensitivity drift. The two causes of drift are (1) changes in the performance of the sensor from its calibrated state independent of its surrounding environment, and, (2) changes due to the environment in which the device is implanted. The first cause can occur due to a number of reasons, including aging of the device and mechanical fatigue; it can be minimized through device and system design. Additionally, the environment can cause drift in the device through the attachment of tissue to (or encapsulation of) the sensor over time, to diffusion of substances from the environment into the sensing system, to the sensor’s position physically changing or drifting over time, and to variations to the local pressure and composition within the body, among others. These causes can be reduced through the careful design of device packaging and materials (see Section 2.3). Both causes of drift can lead to sensitivity and offset drift; some drift is present in all devices. If there is significant drift, at best, the sensor will need to be frequently calibrated and, at worst, its readings will be unreliable. Some commercial devices have achieved a signal drift of less than 2 mmHg per month (Data Sciences International 2005).
Next, power consumption of the implanted sensor and circuitry should be minimized as much as possible for a number of reasons. First, power consumption generates heat which may damage the surrounding tissue (see Biological and Implant Considerations). Second, if the system is battery driven, a low power consumption will reduce the frequency of recharges, increase the system’s lifetime, and reduce the required battery size. On the other hand, if the system is remotely powered, decreasing its power consumption will increase its communication distance due to the fact that it will require less transmitted energy to operate. The next section has more information on the communication and power options for implanted systems.
Finally, the overall size of the implanted sensor and circuitry should be small in order to minimize its impact on the body (e.g. blood flow). For this reason, microtechnology (micro-electro-mechanical systems or MEMS) and nanotechnology (nano-electro-mechanical systems or NEMS) are favorable techniques for device fabrication due to their ability to create miniature devices.
2.2 Communication and power
Wireless communication systems can be grouped into three categories based on the characteristics of the primary and secondary communication nodes (in this case, the external implanted node, respectively; DeHennis 2004). In the first category, known as wireless communication, both nodes have internal power sources and only data is transmitted wirelessly. This category has the advantages of high data bandwidth and a large wireless range. However, the power sources are typically batteries with finite lifetimes and requiring frequent charging. In addition, these systems tend to be large in order to accommodate the power source and associated circuitry. For long-term implants, the finite lifetime and large size of this category may not be acceptable, depending on the application. However, having an on-board power source enables continuous or periodic data collection without the need for an external interface. Overall, this category has a wireless range between 20 and 1000 cm. The PA-C10 from Data Sciences International (Data Sciences International 2005) implements wireless communication to achieve a device with a size of 1.1 cm3 and a communication distance of up to 10 m; however, its lifetime is only 1.5 months.
In the second category, known as active telemetry, the power source is only located in the primary node, the secondary node is remotely powered by the primary node, and each node has a transmitter and receiver for communication. Relative to the first category, active telemetry has a longer lifetime due to no power system in the secondary node, but it has a limited communication range due to its limited (remotely delivered) power. In addition, wireless communication and power transfer can theoretically occur via a number of means, including antenna-based transmission, inductively coupled transmission, and optical transmission. Overall, this category has a wireless range between 5 and 30 cm. To date, very few implantable pressure sensors have utilized active telemetry, likely due to the increased complexity compared to passive telemetry (see below). However, a wireless environmental monitor implementing active telemetry (DeHennis and Wise 2005) achieved a communication distance of 4 cm and a size of 0.32 cm3 without an integrated battery.
The third category, or passive telemetry, is different from active telemetry in that there is only one transmitter and receiver for communication. In this case, the secondary node passively loads the primary node and that loading can be correlated to the measurement of the secondary node. In practice, passive telemetry is typically achieved through the use of coupled inductors. This type of system has an extended lifetime and minimized secondary node size, but has the smallest data bandwidth and wireless range of the three systems. This category is thus highly suited for implanted applications that are close to the surface of the body and require low data rates and minimum size. However, both the second and third categories require an external interface for operation and frequent or continuous measurements may not be possible. This category has a wireless range around 0.5 to 20 cm. CardioMEMS has achieved a passive-telemetry-based system (Becker 2006; Ellozy 2004) with a communication distance of 20 cm, size less than 0.23 cm3 and lifetime greater than 3 years.
Overall, the type of wireless communication is determined by the required communication distance (location of the implant in the body and of the external node), by the required device lifetime (battery versus remotely powered), by the required device size (implant location), and by the required data bandwidth (informational content of the specific blood pressure waveform). More examples of devices that utilize each type of communication are given in Sections 2 and 3. For all three of the categories of wireless communication, however, it is important that the data and power transmission does not cause tissue damage, as discussed in the next section.
2.3 Biological and implant considerations
For long-term operation, the implanted blood pressure monitor must additionally be designed so that it has a minimal impact on the body that will host it and vice-versa. Biocompatibility is a complex subject with many components and issues. A thorough treatment is given elsewhere (Harsanvi 2000); however, an overview of the most relevant issues and packaging solutions is given below.
2.3.1 Influence of the body on the system
The body is a harsh environment and it will do its best to isolate and passivate any object that appears foreign or impacts its function. Thus, the implanted blood pressure monitoring system must be designed not only to appear native to the body, but also to be minimally impacted by the properties and actions of the body. Most generally, the body can be approximated as a warm saline bath. Thus, the system must be able to withstand submersion in a wet solution at a mean temperature of 37°C with a variation of plus or minus a few degrees. Therefore, the systems are typically designed with hermetic packages (see Section 2.3.3) to prohibit the diffusion of substances into the device. In addition, the system must be designed so that it is not impacted by the attachment of various biological substances, such as connective tissue. In the case of diaphragm pressure sensors, the mechanical stiffness of the diaphragm must be much greater than the mechanical stiffness of the potential attached tissues in order to minimize their impact on the device’s functionality.
2.3.2 Impact of the device on the body
In general, the implantation and long term impact of the device on the body should be minimized. Thus, the device should be implanted non-invasively, if possible—perhaps delivered by a catheter or through a needle injection. The sensor materials must also be biocompatible and cause very little or no short or long-term damage to the artery or inflammation of the surrounding tissue. The sensor should not lead to an infection or hardening of the artery wall, and should not restrict blood flow or cause the blood to coagulate or clot significantly. It should be designed so that it does not become dislodged and its location does not migrate. The system may not contain toxic materials that may be released into the blood or body tissue if the device is fractured or destroyed.
Next, the wireless implanted system should not exceed recommended levels for electromagnetic radiation and tissue heating (Tech. Rep. ANCI 1982; Tech. Rep. IEEE 1992; Lin 2003; Yu 2004; Adair and Petersen 2002). In 1966, the American Standards Association set a recommended limit of 10 mW/cm2 for frequencies from 10 MHz to 100 GHz (Tech. Rep. USASI Standard 1966). More recently, the recommendations have been updated to include frequency dependent limits (Tech. Rep. ANCI 1982; Tech. Rep. IEEE 1992). For instances where only a small part of the body is exposed to the field (as in wireless implants), the limits are substantially relaxed (Tech. Rep. IEEE 1992; Yu 2004), resulting in a magnetic and electric field and power density limits shown in Table 2. If the implanted system uses radio frequency (RF) communication or emits electromagnetic fields, these limits should be followed.
In addition, it is recommended that the implanted system should not cause greater than a 1°C temperature rise in the surrounding tissue to avoid tissue damage (Yu 2004). Thus, its power dissipation should be closely regulated. For a 15 × 15 × 2 mm implant, approximately 23 mW is required to increase the temperature of surrounding body tissue by 1°C (Yu 2004) and, thus, a device of this size should be designed to consume less than 23 mW.Footnote 1 The power required to achieve a 1°C temperature rise increases with the square root of the device’s surface area. Thus, a larger device can consume more power because that power is spread out over a larger area. In general, for an implant utilizing RF communication, a frequency in the low-MHz region provides a good compromise between bandwidth and tissue absorption (DeHennis 2004; Yu 2004). Similarly, for a device utilizing optical wireless communication, such as in (Ackermann et al. 2006; Kudo et al. 1988), tissue damage due to heating and radiation exposure should be minimized. For wavelengths from 600 to 1300 nm (from the orange region of the visible spectrum to the near infrared), light absorption of most tissues is minimal permitting significant penetration of the signal into the body (Vo-Dinh 2003). Even so, some absorption occurs and long-term tissue damage must be avoided.
2.3.3 Biocompatible packaging
In order the meet the requirements of the two subsections above, various materials and packaging technologies have been developed for implantable blood pressure monitoring systems. The most common approach utilizes a hermetic enclosure that is coated with a biocompatible material. The hermetic enclosure protects the sensitive portion of the system from the body and the biocompatible coating is used to improve the interface of the implant with body. In previous work, the hermetic housing has been formed from a silicon-glass anodic bond (Najafi and Ludomirsky 2004; Park et al. 1998; Takahata et al. 2004; DeHennis and Wise 2006; Ziaie and Najafi 2001), a glass-glass fusion bond (Allen 2005), chemical vapor deposited oxide (Eggers et al. 2000), and ceramic (Fonseca et al. 2006).
Various coatings have also been utilized; in addition to being biocompatible and hemocompatible, an ideal coating should uniformly cover the entire implanted system and have good adhesion to the device (Behrend et al. 1998). The most widely used coating is silicone rubber (Allen 2005; Becker 2006; Data Sciences International 2005; Cong et al. 2004), which can be injection molded to completely encapsulate the implanted device. Parylene has been utilized as well (DeHennis and Wise 2006), mainly due to its reduced water absorption compared to silicone. Thus, it serves as a secondary barrier to the harsh environment of the body or to protect components outside the hermetic housing. Other encapsulants that have been utilized include polytetrafluoroethylene (PTFE; Fonseca et al. 2006) and parylene (DeHennis and Wise 2006).
2.4 Impacts of potential energy, kinetic energy, and absolute pressure sensing
The measurement of blood pressure is affected by a number of practical issues which must be taken into account when designing the measurement system. Most significantly, it is affected by potential energy and kinetic energy at the site of measurement, and, if an absolute pressure sensor is used, by changes in the surrounding atmospheric pressure. These issues are discussed below.
Blood pressure, by definition, is a relative quantity; its value is the absolute pressure of blood minus the absolute pressure of the surrounding atmosphere. However, many micromachined and miniature sensors today are absolute pressure sensors. Systems that employ absolute sensors must therefore include a secondary sensor to measure atmospheric pressure, so that this value may be subtracted from the pressure measured by the sensor to achieve a true measurement of blood pressure. If this is not done, blood pressure measurements will vary with changes in atmospheric pressure. For remotely powered passive systems (Najafi and Ludomirsky 2004; CardioMEMS 2007a), an atmospheric pressure sensor may be included in the external interface. For other systems, the solution is not as straight forward and a means to measure the pressure of blood relative to atmospheric pressure must be implemented. To solve this problem, implantable sensors that measure the pressure of blood relative to that of the body have been investigated (Cong et al. 2004).
In various practical situations, potential and kinetic energy may also impact the accuracy of blood pressure measurements (Webster 1997). This can be seen through Bernoulli’s equation for frictionless flow (Burton 1972):
In Equation 1, PT is the total measured pressure, P is the blood pressure, ρ is the density of blood, g is the acceleration of gravity, h is the height of the sensor above the heart, and v is the velocity of blood flow. As can be seen, the measured blood pressure, PT, can differ from the desired static blood pressure, P, due to the potential energy (ρgh) and kinetic energy (ρv2/2) terms. Because of potential energy, the measured value of blood pressure will change if the position of the sensor is varied relative to the heart. In fact, each 1.3-cm increase in the height of the sensor relative to that of the heart will increase the blood pressure reading by 1 mmHg (Webster 1997). This clearly has an impact on long-term monitoring of blood pressure. Either a means to ensure that the sensor is always at the same height relative to the heart or a way to compensate for changes in potential energy must be incorporated into the system for accuracy. Note that sensors that are placed close to the heart or in the heart will undergo very little change in potential energy, and thus will not suffer as much from this problem.
Finally, because of the impact of kinetic energy on measurement energy, care must be taken in the positioning of the sensor in the body and to ensure that its position will not change over time. Since this effect is highly dependent on blood flow velocity, it can be minimized by placing the sensor parallel to the flow of blood and near the wall of the artery. Note that kinetic energy will only impact sensors that are in direct contact with blood flow. More details on this artifact can be found elsewhere (Webster 1997; Burton 1972).
The next sections review the current industrial work and research in the area of implantable intra-arterial and extra-arterial blood pressure sensor systems.
3 Intra-arterial blood pressure monitors
As covered in the previous section, there are numerous tradeoffs and considerations for implantable blood pressure monitors. This section looks at the various approaches that have been taken in academia and industry. Although the pressure sensing techniques and considerations reviewed in this paper are suitable for other applications including the long-term measurement of intraocular (Frischholz 2006; Scknakenberg et al. 2000), intracranial (Frischholz 2006; Banister et al. 2000; Flick and Orglmeister 2000) and bladder pressures (Siwapornsathain et al. 2002; Coosemans and Puers 2005), only the work related to blood pressure measurement is reviewed in this paper.
In 1972, an early effort in the area of implanted wireless pressure monitoring devices utilized an active transmitter and integrated battery (Casadei et al. 1972). The system consisted of a 13 × 47 × 67 mm transmitter coated with an epoxy resin and weighing 58 g, and a commercial pressure sensor with a 3 mm titanium diaphragm. It boasted an impressive 20 m telemetry range, but its total lifetime was estimated at 1 year assuming 2 h of operation each day. It was successfully tested in dogs for periods of up to 9 months and exhibited an implanted signal drift of 7% per month. Overall, the size and limited lifetime of the device were its major drawbacks. With the improvements in the field of rechargeable batteries and microfabrication, more recent efforts have investigated devices with longer lifetimes and smaller sizes.
In 1998, Park, et al., at the Korea Advanced Institute of Science and Technology (KAIST), investigated a capacitive pressure sensor with passive telemetry (Park et al. 1998) that was targeted towards the measurement of cardiovascular, intraocular and brain pressure monitoring. The compact device was the first of its kind to integrate a pressure sensor and inductor on the same chip, minimizing the size of the device and maximizing its performance (by minimizing parasitic capacitance and resistance). The 3 × 3 × 0.6 mm structure, shown in Fig. 3, was formed using bulk micromachining and silicon–glass anodic bonding and had a pressure range from 0 to 100 mmHg. Both the pressure sensitive capacitor and inductor for passive telemetry were encased in hermetic chambers. The compact, high-performance device only lacked a biocompatible coating and acute and chronic in vivo testing before it would be applicable for clinical use (likely for monitoring heart failure due to its limited measurement range). However, its efficient design likely inspired later work in the field.
A passive telemetry, LC resonant pressure sensor with integrated inductor and capacitor by Park et al. (1998)
In 2000, Chatzandroulis et al., at the NCSR “Demokritos” Institute of Microelectronics in Athens, Greece, continued the work in implantable blood pressure monitors through their investigation of a passive telemetry system using a capacitive pressure sensor with a SiGeB diaphragm and a capacitance-to-frequency converter to control the RF modulator (Chatzandroulis et al. 2000). The system performed well in a simulated arterial environment and consumed 4 mW of power. However, due to the small device size (~3 × 2 × 0.6 mm), the power required to operate the device may result in a temperature increase that is dangerous to surrounding tissue (depending on the implant location). For clinical application, the device would need to be encased in a biocompatible package, its power consumption possibly reduced, and its short and long-term in vivo performance verified.
In 2004, Takahata, et al., at the University of Michigan presented a combination of an arterial stent and a passive telemetry (no battery) blood flow and pressure sensor (Takahata et al. 2004, 2003). The stainless steel stent was fabricated using micro-electro-discharge machining and the pressure sensors were formed using bulk and surface micromachining and anodic bonding. The 20 mm-long and 3.5 mm-diameter device was deployed in an artificial artery using a standard angioplasty balloon. Once inflated, the stent also served as the inductor in the inductive link. The work at Michigan continued with the development, by DeHennis et al., of a fully integrated, battery free, remotely powered system for arterial pressure and flow sensing (DeHennis and Wise 2006). The inductor for telemetry, pressure sensors and circuitry were fabricated using a combination BiCMOS process and bulk micromachining on a single 2 mm3 chip and consumed only 340 μW of power. The device was coated in a 1 μm layer of parylene-C to improve its biocompatibility and successfully tested in a mock artery. It had a minimum detectible differential pressure of 3 mmHg (corresponding to a 13% reduction in arterial flow) and is shown in Fig. 4. In this novel work, greater attention was given to designing the device for implantation than previous work; a large portion of the device was formed from stainless steel, it was coated in parylene, and it had a very thin profile. However, no in-vivo testing was performed to investigate hemocompatibility and biocompatibility.
A fully integrated, passive telemetry, arterial pressure and flow sensor by DeHennis, et al. (DeHennis and Wise 2006)
In 2006 at Georgia Institute of Technology, Fonseca, et al., reported the first flexible micromachined wireless pressure sensor (Fonseca et al. 2006). Made out of Liquid Crystal Polymer (LCP), polytetrafluoroethylene (PTFE), and Fluorinated Ethylene Propylene copolymer (FEP), the devices (Fig. 5) are flexible and can be folded into shapes suitable for injection into the body via a catheter. An acute version of the device was successfully tested in canines over a 60-day period and improved results are expected for the chronic version. Targeted at monitoring abdominal aortic aneurisms (AAAs), this work represents one of the first academic implantable blood pressure monitors with strong consideration for biocompatibility and minimally invasive delivery. However, the device’s in vivo accuracy has thus far been limited by signal drift.
Cross-section (left) and picture (right) of the Georgia Tech flexible wireless pressure sensor (Fonseca et al. 2006)
In industry, Data Sciences International (DSI) of St. Paul, MN, has developed a series of implantable transmitters that can measure various physical parameters in research animals. The PA-C10, PA-C40 and PA-D70 (Data Sciences International 2005), shown in Fig. 6, measure pressure and activity in small, medium, and large animals, respectively. The integrated catheter transfers pressure from the specified measurement location (in this case, the artery) to the body of the transmitter. These systems have successfully been used to measure arterial systolic and diastolic pressure, mean pressure and heart rate. The PA-C10, PA-C40, PA-D70 weigh 1.4, 9.0, and 37 g, have volumes of 1.1, 4.5 and 25 cc, and have batteries with warranted lives of 1.5, 4, and 4 months, respectively. All of the transmitters are encapsulated in silicone elastomer and have initial accuracies of ±3 mmHg. The drift of the PA-C10 and PA-D70 is less than 2 mmHg per month. Research studies have utilized DSI’s devices (Kramer et al. 2000; Mills et al. 2000) and a study in 2004 (Whitesall et al. 2004) showed that a DSI PA transmitter compared favorably with the tail-cuff blood pressure measurement method in mice. There are two main drawbacks of the DSI devices. First, an incision must be made in the artery to insert the integrated catheter and measure arterial pressure. This incision may result in possible complications. Second, the batteries in the devices have a warranted lifetime of less than 4 months and would need to be surgically replaced after expiration. For these reasons, the devices are only suitable for the short or medium term measurement of blood pressure in laboratory animals.
The PA-C10, PA-C40, and PA-D70 implantable pressure sensors from Data Sciences, International (Data Sciences International 2005)
Integrated Sensing Systems, Inc., of Ypsilanti, MI, is developing an ultraminiature, battery-less, capacitive pressure sensor that can be implanted via a minimally invasive, outpatient procedure (Najafi and Ludomirsky 2004; Integrated Sensing Systems 2002). In 2004, the battery-less, RF device was successfully tested in animals and achieved a real time, 400 samples/second heart pressure waveform that was in good agreement with a catheter-based pressure sensor, had an accuracy less than 1 mmHg, and achieved a communication/powering (using a handheld unit) distance of 3–4 cm. The device is formed using etched-back anodically bonded silicon and glass wafers in the Dissolved Wafer Process (Zhang et al. 2001). The second revision of the device, in development, will have a volume less than 20 mm3, a resolution less than 0.1 mmHg, a handheld readout up to 10 cm from the implanted system and a 10-year, implanted lifetime. This device, shown in Fig. 7, has not yet been approved for use in humans.
Second generation implantable cardiovascular monitor from ISSYS, Inc. (Integrated Sensing Systems 2002)
CardioMEMS, founded in 2001 on technology from the Georgia Institute of Technology and located in Atlanta, GA, has successfully implanted wireless blood pressure sensors in humans for the monitoring of abdominal aortic aneurysms and heart failure (Becker 2006; CardioMEMS 2007b). As of December 2005, the EndoSensor™ has been implanted in over 100 patients with abdominal aortic aneurysms in 4 countries. The battery-less, 5 × 30 mm device has a wireless range of about 20 cm. The micromachined device, shown in Fig. 8, is formed utilizing two fused silica wafers, electrodeposited inductors, and fusion bonding (Allen 2005). In February of 2006, CardioMEMS achieved the first human implant of a wireless catheter-based pressure sensor (CardioMEMS 2007b). The device, known as the HeartSensor™ and targeted at detecting heart failure, utilizes a capacitive pressure sensor and measures a resonant frequency shift with changes in pressure. The clinical success of the CardioMEMS devices can be attributed to several factors. First, the designs (both performance and biocompatibility) were targeted at specific niche applications. Also, the structure and operation of the device are simple and elegant. Finally, it should also be noted that in the case of the EndoSensor™ device, the implanted device is not located within the bloodstream, but instead outside of the endovascular repair. Thus, clotting and coagulation of blood are not as much of an issue as in other blood pressure monitoring applications.
Picture of the CardioMEMS EndoSensor™ (Becker 2006)
Campus Micro Technologies is a German company developing a family of implantable telemetric pressure monitoring systems (Campus Micro Technologies GmbH 2007). Its system targeted at monitoring aneurysm repair is based, in part, off of technology developed by Eggers et al. in 2000 (Eggers et al. 2000). The wirelessly powered system developed by Eggers et al. consisted of a surface micro-machined capacitive type absolute pressure sensor (0.8 × 2 × 0.5 mm) and two low power ASIC for sensor read-out and telemetry. The sensor technology consisted of an array of 16 75 × 75 μm capacitive pressure sensors and an identical pressure-insensitive reference array. The complete system demonstrated a resolution less than 1 mmHg, a frequency response of 15 Hz, a power consumption less than 350 μW, and a transmission distance up to 5 mm. It was encased in a silicone-based coating to improve its biocompatibility and decrease moisture absorption.
Medtronic has also entered into the field of implantable blood pressure monitoring devices with its implantable haemodynamic monitoring (IHM) series of devices. The wristwatch-sized product line was intended to continuously monitor patients with heart failure and provide data to doctors via the internet. Although the devices achieved some clinical success (Steinhaus et al. 2005; Braunschweig et al. 2006), it failed to be approved by the FDA in 2007 (Feder 2007). According to a panel of experts assembled by the FDA, the device did not keep enough patients out of the hospital to prove its effectiveness.
Remon Medical Technology, an Isreali company, is developing implantable sensing systems tartgeted at monitoring congestive heart failure (CHF) and sac pressure after an abdominal aortic aneurysm (AAA) repair (Remon Medical Technologies Inc. 2007). Both devices utilize acoustic waves to transmit power and data. The advantage of this approach is that acoustic waves are not absorbed by tissue and, thus, data and power can be transmitted very efficiently. In addition, it does not require an antenna and, thus, helps to minimize the device size. The company achieved the first human implantation of its ImPressure® device to monitor intra-aneurysm pressures in 2003 (Ellozy 2004; Remon Medical Technologies Inc. 2007) and its first European use of its implantable CHF monitor in 2006 (Remon Medical Technologies Inc. 2007). In the clinical trials of the ImPressure®, the 3 × 9 × 1.5 mm devices were hand-sewn to the outside of a stent graft. Excellent agreement was found between a catheter-based and the ImPressure® device and it successfully detected endoleaks in several patients. Despite their clinical success, sensor details and specifications are difficult to find.
4 Extra-arterial blood pressure monitors
Most of the work to date has focused on developing implantable intra-arterial blood pressure sensors. In this technique, the pressure of the artery is directly measured. However, because the devices are located inside the artery, there is a risk of dislocation, blood coagulation and clotting. Extra-arterial blood pressure monitors seek to mitigate this problem by measuring pressure indirectly through the arterial wall or through the expansion and contraction of the artery. However, these devices have the disadvantage that they must usually be implanted via an invasive surgical procedure.
In 2001 at the University of Michigan, Ziaie and Najafi presented an implantable pressure microsystem based on the principle of tonometry (Ziaie and Najafi 2001). The device consisted of a bulk micromachined silicon capacitive pressure sensors and a miniature titanium cuff. The cuff surrounds and reshapes the artery, forcing contact between the pressure sensors and the arterial wall, as shown in Fig. 9. The 10 × 6.5 × 3 mm device contained integrated electronics and had a resolution of 0.5 mmHg. The device was tested using a silastic tube that mimicked a blood vessel; however, no in vivo tests or long-term tests that investigated device drift were performed. A potential drawback of this design is that the long term reshaping of the artery may have adverse physiological effects and long term in vivo tests would be needed to verify its safety.
An extra-arterial implantable blood pressure microsystem by Ziaie and Najafi (Ziaie and Najafi 2001)
In 2004 at Case Western Reserve University in Cleveland, OH, Cong, et al., presented an implantable pressure sensor targeted at long-term applications (Cong et al. 2004). The prototype device consisted of a soft biocompatible rubber cuff filled with a low viscosity, biocompatible liquid and wrapped around a mock artery. A high resolution MEMS pressure sensor immersed in the fluid detects a scaled version of the blood pressure waveform. An additional benefit of this design is that it measures the pressure difference between the blood and the body and, thus, does not require an additional atmospheric sensor. The stiffness of the cuff was chosen to be much less than that of the blood vessel, hopefully minimizing any restriction of the artery and, thus, mitigating long-term adverse biological effects. Experimental results for the prototype had excellent agreement with a reference pressure sensor in the mock artery. In 2005, the investigators presented an updated version of the cuff (Cong et al. 2005) that was molded from a medical-grade silicone elastomer and implanted in laboratory rats. The 5 mm × 2 mm × 100 μm device was compared to a commercial catheter-tip transducer; the two in vivo measured blood waveforms closely matched (with a scaling factor). In 2006, this work was further improved with the integration of a rigid isolation ring that surrounds and isolates the cuff from its environment leading to reduced long-term sensor drift (Cong et al. 2006). Devices with and without the isolation ring were wrapped around the right carotid artery of a laboratory rat and the improved device displayed a baseline drift of 0.6 mmHg in 120 s, three times smaller than the original device and dominated by drift in the commercial pressure sensor. The improved device is shown in Fig. 10.
An improved drift, long-term arterial cuff developed at Case Western Reserve University (Cong et al. 2006)
5 Conclusion and outlook
This paper has given an overview of long-term implantable blood pressure monitoring technology and reviewed the industrial work and research in that area. Tables 3 and 4 summarize the work in this area to date. Thus far, intra-arterial devices specifically targeted at niche clinical applications have been the most successful. Extra-arterial devices have the benefit of a reduced risk of blood-related complications; however, future devices should be designed to have little impact on the artery and their signal drift (when implanted) needs to be improved before they achieve clinical success. The need for invasive surgical implantation may continue to hamper these devices, however.
Overall, significant progress has been made in the field since the idea was first introduced in the 1960s (Van Citters et al. 1966; Olsen et al. 1967), with advances in batteries, wireless communication, wireless power transmission, miniaturization and microtechnology, and biocompatible materials. Companies are offering long-term implantable blood pressure sensors for animal research and one has received FDA approval and been implanted in over 100 human subjects (Becker 2006). To date, most devices have contained capacitive sensors, required remote powering, and utilized RF communication. However, devices utilizing optical communication and powering are being investigated and promise to possibly reduce communication error and improve transmission distance into the body. In addition, acoustic waves have been utilized in industry to achieve wireless powering and communication (Remon Medical Technologies Inc. 2007). MEMS technology has been utilized to micromachine sensors and sensors systems. This trend will continue along with the use of nanotechnology to miniaturize systems further. Next, research has been suggested or performed on scavenging energy from the environment (Starner and Paradiso 2004; Paradiso ans Starner 2005). Future implants may utilize energy sources within the body to achieve self-powering (Ko 1980; Lewandowski et al. 2007). Such abilities will remove the lifetime restriction of batteries and enable continuous data collection and storage without remote powering. Such advancements will continue to improve the field of long-term blood pressure monitoring and will benefit patients that critically need such technology.
Notes
This calculation assumes a tissue thermal conductivity of 4.2 mW/cm-°C. This value will vary based on the location in the body and the composition of the surrounding tissue.
References
D.M. Ackermann, B. Smith, K.L. Kilgore, P.H. Peckham, Design of a high speed transcutaneous optical telemetry link, in Engineering in Medicine and Biology Society, 2006. EMBS ‘06. 28th Annual International Conference of the IEEE, pp. 2932–2935, 2006
E.R. Adair, R.C. Petersen, Biological effects of radiofrequency/microwave radiation IEEE Trans. Microwave Theor. Tech. 50, 953–962 (2002)
M.G. Allen, Micromachined endovascularly-implantable wireless aneurysm pressure sensors: from concept to clinic Transducers ’05 1, 275–278 (2005)
American national standard for safety levels with respect to human exposure to radio frequency electromagnetic fields, 300 kHz to 300 GHz, Tech. Rep. ANSI C95.1 (1982)
K. Banister, I.R. Chambers, M.S. Siddique, H.M. Fernandes, A.D. Mendelow, Intracranial pressure and clinical status: assessment of two intracranial pressure transducers Physiol. Meas. 21, 473–479 (2000)
T.J. Becker, Heart healthy: CardioMEMS moves closer to commercializing innovative sensors for heart patients. [Online]. 2007(01/23), Available: http://gtresearchnews.gatech.edu/newsrelease/cardiomems.htm, (2006, Jan.)
D. Behrend, B. Clasbrumme, D. Etuodt, C. Hierold, H. Kapels, E. Landgraf, K. Oppermann, T. Scheiter, M. Steger, D. Wenzel, Implantable low power integrated pressure sensor system for minimal invasive telemetric patient monitoring, Micro Electro Mechanical Systems, 1998. MEMS 98. Proceedings., the Eleventh Annual International Workshop on
J.M. Borky, K.D. Wise, Integrated signal conditioning for silicon pressure sensors IEEE Trans. Electron Devices 26, 1906–1910 (1979)
T.A. Bowdle, Complications of invasive monitoring Anesthesiol. Clin. North Am. 20, 333 (2002)
F. Braunschweig, B. Kjellstrom, M. Soderhall, N. Clyne, C. Linde, Dynamic changes in right ventricular pressures during haemodialysis recorded with an implantable haemodynamic monitor Nephrol. Dial. Transplant. 21, 176–183 (2006)
A.C. Burton, Physiology and Biophysics of the Circulation, 2nd edn. (Year Book Medical Publishers, Chicago (1972)
Campus Micro Technologies GmbH. [Online]. 2007(11/18), Available: http://www.campus-micro-technologies.de/index.htm
CardioMEMS, CardioMEMS, inc. announces first patient implant of wireless pressure sensor for heart failure monitoring in the united states. [Online]. 2007(04/09), Available: http://www.cardiomems.com/content.asp?display=news&view=7 (2006, Dec.)
CardioMEMS, CardioMEMS, inc. announces FDA clearance of the EndoSureä wireless AAA pressure measurement system for measuring intrasac pressure during thoracic aortic aneurysm (TAA) repair. [Online]. 2007(04/09), Available: http://www.cardiomems.com/content.asp?display=news&view=9 (2007a, Mar.)
CardioMEMS. [Online]. 2007b(01/23), Available: http://www.cardiomems.com
F.W. Casadei, M. Gerold, E. Baldinger, Implantable blood pressure telemetry system IEEE Trans. Biomed. Eng. BME-9, 334–341 (1972)
S. Chatzandroulis, D. Tsoukalas, P.A. Neukomm, Miniature pressure system with a capacitive sensor and a passive telemetry link for use in implantable applications J. Microelectromech. Syst. 9, 18–23 (2000)
P. Cong, D.J. Young, W.H. Ko, Novel long-term implantable blood pressure monitoring system Proc IEEE Sensors 3, 1359–1362 (2004)
P. Cong, K. Olszens, D.J. Young, W.H. Ko, Implantable blood pressure monitoring of small animal for advanced biological research Transducers ’05 2, 2002–2006 (2005)
P. Cong, D.J. Young, B. Hoit, W.H. Ko, Novel long-term implantable blood pressure monitoring system with reduced baseline drift, EMBS ‘06, 1854–1857 (2006)
R. Cooper, D. Beale, Radio telemetry of intraocular pressure in vitro, Invest. Ophthalmol. Vis. Sci. 16, 168–171 (1977)
J. Coosemans, R. Puers, An autonomous bladder pressure monitoring system Sens. Actuators, A. Phys. 123–124, 155–161 (2005)
Data Sciences International, Guide to PhysioTel transmitters. [Online]. 2007(01/23), Available HTTP: http://www.datasci.com/pdf/products/DSI_Transmitters.pdf (2005, Dec 5)
A.D. DeHennis, Remotely-powered wireless monitoring systems, PhD Dissertation, University of Michigan, Ann Arbor, 2004
A.D. DeHennis, K.D. Wise, A wireless microsystem for the remote sensing of pressure, temperature, and relative humidity J. Microelectromech. Syst. 14, 12–22 (2005)
A.D. DeHennis, K.D. Wise, A fully integrated multisite pressure sensor for wireless arterial flow characterization J. Microelectromech. Syst. 15, 678–685 (2006)
T. Eggers, C. Marschner, U. Marschner, B. Clasbrummel, R. Laur, J. Binder, Advanced hybrid integrated low-power telemetric pressure monitoring system for biomedical applications, Proceedings of the IEEE Micro Electro Mechanical Systems (MEMS), pp. 329–334 (2000)
S.H. Ellozy, First experience in human beings with a permanently implantable intrasac pressure transducer for monitoring endovascular repair of abdominal aortic aneurysms J. Vasc. Surg. 40, 405–411 (2004)
R.H. Epstein, S. Huffnagle, R.R. Bartkowski, Comparative accuracies of a finger blood-pressure monitor and an oscillometric blood-pressure monitor J. Clin. Monit. 7, 161–167 (1991)
B.J. Feder, A remote heart monitor fails to impress F.D.A. panel. [Online]. 2007(11/18), Available: http://www.nytimes.com/2007/03/02/business/02device.html (2007, March 2)
B.B. Flick, R. Orglmeister, A portable microsystem-based telemetric pressure and temperature measurement unit IEEE Trans. Biomed. Eng. 47, 12–16 (2000)
M.A. Fonseca, M.G. Allen, J. Kroh, J. White, Flexible wireless passive pressure sensors for biomedical applications, Technical Digest of the Solid-State Sensor, Actuator, and Microsystems Workshop (Hilton Head 2006), pp. 38–42, 2006.
E.E. Frezza, H. Mezghebe, Indications and complications of arterial catheter use in surgical or medical intensive care units: analysis of 4932 patients Am. Surg. 64, 127–131 (1998)
M. Frischholz, Wireless pressure monitoring systems Med. Device Technol. 17, 24–27 (2006)
G. Harsanvi, Sensors in Biomedical Applications: Fundamentals, Technology, and Applications (CRC Press, Boca Raton, FL (2000)
IEEE standard for safety levels with respect to human exposure to radio frequency electromagnetic fields, 3 kHz to 300 GHz, Tech. Rep. IEEE C95.1–1991 (1992)
Integrated Sensing Systems, Medical products overview. [Online]. 2007(01/23), Available: http://www.mems-issys.com/html/medfamily.html (2002)
K. Kramer, H. Voss, J.A. Grimbergen, P.A. Mills, D. Huetteman, L. Zwiers, B. Brockway, Telemetric monitoring of blood pressure in freely moving mice: a preliminary study Lab. Anim. 34, 272–280 (2000)
O. Kemmotsu, M. Ueda, H. Otsuka, T. Yamamura, D.C. Winter, J.S. Eckerle, Arterial tonometry for noninvasive, continuous blood-pressure monitoring during anesthesia Anesthesiology 75, 333–340 (1991)
J.L. Kermode, N.J. Davis, W.R. Thompson, Comparison of the Finapres blood-pressure monitor with intra-arterial manometry during induction of anesthesia Anaesth. Intensive Care 17, 470–475 (1989)
W.H. Ko, Power sources for implant telemetry and stimulation systems A Handbook on Biotelemetry and Radio Tracking C.J. Amlaner, D. MacDonald (Pergamon Press, INc., Elmsford, NY (1980), 225–245
N. Kudo, K. Shimizu, G. Matsumoto, Fundamental study on transcutaneous biotelemetry using diffused light. Front. Med. Biol. Eng. 1, 19–28 (1988)
Y.S. Lee, K.D. Wise, A batch-fabricated silicon capacitive pressure transducer with low temperature sensitivity IEEE Trans. Electron Devices 29, 42–48 (1982)
B.E. Lewandowski, K.L. Kilgore, K.J. Gustafson, Design considerations for an implantable, muscle powered piezoelectric system for generating electrical power Ann. Biomed. Eng. 35, 631–641 (2007)
J.C. Lin, Safety standards for human exposure to radio frequency radiation and their biological rationale IEEE Microw. Mag. 4, 22–26 (2003)
Mayo Clinic Staff, High blood pressure: Get the most out of home monitoring. [Online]. 2007(01/25), Available: http://www.mayoclinic.com/health/high-blood-pressure/HI00016 (2006, May)
P.A. Mills, D.A. Huetteman, B.P. Brockway, L.M. Zwiers, A.J.M. Gelsema, R.S. Schwartz, K. Kramer, A new method for measurement of blood pressure, heart rate, and activity in the mouse by radiotelemetry J. Appl. Physiol. 88, 1537–1544 May 1(2000)
N. Najafi, A. Ludomirsky, Initial animal studies of a wireless, batteryless, MEMS implant for cardiovascular applications Biomed. Microdevices 6, 61–65 (2004)
E. O’Brien, R. Asmar, L. Beilin, Y. Imai, G. Mancia, T. Mengden, M. Myers, P. Padfield, P. Palatini, G. Parati, T. Pickering, J. Redon, J. Staessen, G. Stergiou, P. Verdecchia, European society of hypertension recommendations for conventional, ambulatory and home blood pressure measurement J. Hypertens 21, 821–848 (2003)
E.R. Olsen, C.C. Collins, W.F. Loughborough, V. Richards, J.E. Adams, D.W. Pinto, Intracranial pressure measurement with a miniature passive implanted pressure transensor, Am. J. Surg. 113(6), 727–729 (1967)
J.A. Paradiso, T. Starner, Energy scavenging for mobile and wireless electronics Pervasive Computing, IEEE 4, 18–27 (2005)
E. Park, J. Yoon, E. Yoon, Hermetically sealed inductor-capacitor (LC) resonator for remote pressure monitoring Jpn. J. Appl. Phys. 37, 7124–7128 (1998)
K.E. Petersen, Silicon as a mechanical material Proc. IEEE 70, 420–457 (1982)
T.G. Pickering, J.E. Hall, L.J. Appel, B.E. Falkner, J. Graves, M.N. Hill, D.W. Jones, T. Kurtz, S.G. Sheps, E.J. Roccella, Recommendations for blood pressure measurement in humans and experimental animals: part 1: Blood pressure measurement in humans: a statement for professionals from the subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research, Hypertension 45, 142–161, January 1 (2005)
B.D. Ratner, A.S. Hoffman, F.J. Schoen, J.E. Lemons, Biomaterials Science: An Introduction to Materials in Medicine, 2nd edn. (Elsevier Academic Press, 2004), p. 864
R. Receveur, Microsystem technologies for implantable applications J. Micromech. Microeng. 17, R50–R80 (2007)
Remon Medical Technologies Inc. [Online]. 2007(11/18),Available: http://www.remonmedical.com/
Safety level of electromagnetic radiation with respect to personnel, Tech. Rep. USASI Standard C95.1–1966 (1966)
B. Scheer, A. Perel, U. Pfeiffer, Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine Crit. Care 6, 199–204 (2002)
U. Schnakenberg, P. Walter, G. vom Bogel, C. Kruger, H. Ludtke-Handjery, H.A. Richter, W. Specht, P. Ruokonen, W. Mokwa, Initial investigations on systems for measuring intraocular pressure Sens. Actuators, A, Phys. 85, 287–291 (2000)
E. Siwapornsathain, A. Lal, J. Binard, A telemetry and sensor platform for ambulatory urodynamics, in Microtechnologies in Medicine & Biology 2nd Annual International IEEE-EMB Special Topic Conference on, 2002, pp. 283–287.
J.A. Staessen, E.T. O’Brien, L. Thijs, R.H. Fagard, Modern approaches to blood pressure measurement Occup. Environ. Med. 57, 510–520 (2000)
T. Starner, J.A. Paradiso, Human generated power for mobile electronics, in Low-Power Electronics Design, ed. C. Piguet (CRC Press, 2004), pp. 44.1–44.35
D. Steinhaus, D.W. Reynolds, F. Gadler, G.N. Kay, M.F. Hess, T. Bennett, Implant experience with an implantable hemodynamic monitor for the management of symptomatic heart failure Pacing Clin. Electrophysiol. 28, 747–753 (2005)
K. Takahata, A. DeHennis, K.D. Wise, Y.B. Gianchandani, Stentenna: a micromachined antenna stent for wireless monitoring of implantable microsensors Proc. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 4, 3360–3363 (2003)
K. Takahata, A. DeHennis, K.D. Wise, Y.B. Gianchandani, A wireless microsensor for monitoring flow and pressure in a blood vessel utilizing A dual-inductor antenna stent and two pressure sensors, Proceedings of the IEEE International Conference on Micro Electro Mechanical Systems (MEMS), pp. 216–219 (2004)
F.E. Terman, Radio Engineer’s Handbook (McGraw Hill, New York (1943)
N. Tesla, Electrical transformer, US Patent No. 593,138, Issued: 1897
N. Tesla, System of transmission of electrical energy, US Patent No. 645,576, Issued: 1900
The National Spinal Cord Injury Association, Autonomic dysreflexia. [Online]. 2007(01/25), Available: http://www.spinalcord.org/html/factsheets/aut_dysreflexia.php (2006)
J.K. Triedman, J.P. Saul, Comparison of intraarterial with continuous noninvasive blood-pressure measurement in postoperative pediatric patients J. Clin. Monit. 10, 11–20 (1994)
U.S. Department of Health and Human Services, Blood pressure measurement devices (sphygmomanometers)—accuracy. Report # CPG 7124.23 (2005, Feb. 18)
R.L. Van Citters, W.S. Kemper, D.L. Franklin, Blood pressure responses of wild giraffes studied by radio telemetry, Science 152(3720), 384–386 (1966)
T. Vo-Dinh, Biomedical Photonics Handbook (CRC Press, Boca Raton, FL (2003)
J.G. Webster, Medical Instrumentation: Applicaiton and Design, 3rd edn. (John Wiley & Sons, 1997), p. 720
S.E. Whitesall, J.B. Hoff, A.P. Vollmer, L.G. D’Alecy, Comparison of simultaneous measurement of mouse systolic arterial blood pressure by radiotelemetry and tail-cuff methods Am. J. Physiol. Heart Circ. Physiol. 286, H2408–H2415 (2004)
R.G. Wilkins, Radial artery cannulation and ischemic damage - a review Anaesthesia 40, 896–899 (1985)
K.D. Wise, S.K. Clark, Diaphragm formation and pressure sensitivity in batch-fabricated silicon pressure sensors, in Electron Devices Meeting, 1978 International, 1978, pp. 96–99
H. Yu, A wireless microsystem for multichannel neural recording microprobes, PhD Dissertation, University of Michigan, Ann Arbor, 2004
Y. Zhang, S. Massoud-Ansari, G. Meng, W. Kim, N. Najafi, An ultra-sensitive, high-vacuum absolute capacitive pressure sensor, in Micro Electro Mechanical Systems, 2001. MEMS 2001. the 14th IEEE International Conference on, 2001, pp. 166–169
B. Ziaie, K. Najafi, An implantable microsystem for tonometric blood pressure measurement Biomed. Microdevices 3, 285–292 (2001)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Potkay, J.A. Long term, implantable blood pressure monitoring systems. Biomed Microdevices 10, 379–392 (2008). https://doi.org/10.1007/s10544-007-9146-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-007-9146-3