Abstract
Asia is home to a community of diverse ethnicities and races which contributes to more than half of the world’s population. Asia also shares a significant number in the statistics of worldwide mortality and morbidity, in particular, cerebrovascular disease. Cerebrovascular disease or stroke is a leading cause of mortality and long-term disability worldwide. Globally, there was a downward trend of stroke statistics since the 1990s, however, the collective stroke burden in terms of absolute number of people affected still increases. Stroke is an important health concern as about 60% of the world’s population is in Asia and with many countries regarded as developing economies. Notably, Asia has a higher burden related to stroke compared to coronary artery disease, while the opposite is observed in Western countries. Also, Asia has a higher burden of cerebrovascular risk factors with hypertension as the most prevalent cause of both ischemic and hemorrhagic strokes. Compared to Western countries, Asia has a higher incidence of hemorrhagic strokes and ischemic strokes related to cerebral small vessel disease such as lacunar infarcts, silent strokes, white matter hyperintensities, and cerebral microbleeds. Cases of large vessel occlusion and subarachnoid hemorrhages are variable.
Unique to Asia is the higher incidence of hemorrhagic strokes and AIS related to CSVD. Among the many known and established risk factors for stroke, HTN remains to be the most significant, though modifiable and preventable. Through time, chronic HTN leads to degeneration of the intracranial blood vessel wall leading to occlusion in cerebral ischemia or rupture in cerebral hemorrhages. This chapter highlights cerebrovascular disease in Asia and its causative factors by exploring different stroke subtypes and impact of hypertension. A discussion on blood pressure variability is provided as it is currently an emerging factor contributing to the development of strokes including the Asian population.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cerebrovascular disease
- Ischemic stroke
- Intracerebral hemorrhage
- Subarachnoid hemorrhage
- Cerebral small vessel disease
- Large vessel occlusion
Cerebrovascular disease (CVD) or stroke is the second leading cause of mortality and leading cause of long-term disability worldwide [1, 2]. Globally, there was a downward trend of stroke statistics since the 1990s; however, the collective stroke burden in terms of absolute number of people affected still increases [3]. Stroke is an important health concern as about 60% of the world’s population is in Asia and with many countries regarded as developing economies [4]. Notably, Asia has a higher burden related to stroke compared to coronary artery disease (CAD), while the reverse is observed in Western countries [5]. Also, Asia has a higher burden of cerebrovascular risk factors with hypertension (HTN) being the most prevalent cause of both ischemic and hemorrhagic strokes [4].
In contrast to Western countries, Asia has a higher incidence of hemorrhagic strokes [6] and acute ischemic strokes (AIS) related to cerebral small vessel disease (CSVD) [7]. Cases of large vessel occlusion (LVO) and subarachnoid hemorrhages (SAH) are variable.
This chapter highlights CVD in Asia by discussing the epidemiology, causative risk factors, pathophysiology, and outcome of these different stroke subtypes: AIS due to large vessel occlusion (LVO) and CSVD as well as ICH and SAH. The impact of HTN for each stroke subtype is explored. A section on blood pressure variability (BPV) is provided as it is currently one of the emerging factors contributing to the development of strokes including the Asian population.
19.1 Large Vessel Occlusion and Atherosclerosis
Large vessel occlusion (LVO), a subtype of ischemic stroke under The Trial of Org 10172 in Acute Stroke Treatment Classification, has been variably defined in different clinical studies. Despite this variation, LVO was generally defined as any acute-onset occlusion of the intracranial internal carotid artery (ICA), proximal posterior, middle, and anterior cerebral arteries (PCA, MCA, and ACA, respectively), intracranial vertebral artery (VA), and/or basilar artery (BA) [8]. Prior to the advent of thrombectomy, LVO studies typically defined LVO as those involving ICA and first segment of the MCA (M1). As endovascular interventions such as thrombectomy gained popularity, the definition of LVO expanded to include the occlusions in the other segments as defined above.
Large vessel occlusion has been widely studied through the years due to its huge impact in stroke outcomes in relation to infarct size, severity of neurologic deficits, mortality, and treatment availability.
In a systematic review by Lakomkin et al. identifying the proportion of patients with AIS presenting with LVO on image analysis, it was shown that the prevalence of LVO ranges from 7.3% to 60.6% with a mean prevalence of 31.1% across all included studies [9]. Rai et al., in a US population-based study, indicated that LVOs involving occlusions of the M1, ICA terminus, and BA had an estimated annual incidence of 24 per 100,000 people per year [10]. Approximately two-thirds of LVOs occur in the anterior circulation, mainly in the ICA and MCA, and the remaining occur in the posterior circulation with equal distribution among VA, BA, and PCA [11].
The epidemiology of stroke subtype distribution differs across races and ethnicity. Among the causes of stroke, cardioembolic stroke accounts for about 25–30% of cases in Western countries, while intracranial atherosclerosis accounts for up to 25–65% in Asian countries [12]. Young AIS Asian patients aged 18–49 were investigated by Kay Sin Tan et al. and their study showed that the predominant stroke subtypes were large artery atherosclerosis (29.8%) and small vessel occlusion (20.2%) [13]. The preceding statements suggest that a large proportion of Asian stroke patients with AIS are classified as having large vessel disease and as will be discussed further in the later sections, CSVD as well.
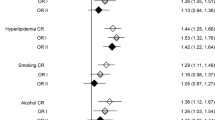
Risk factors for all AIS include HTN, diabetes, dyslipidemia, and excessive alcohol consumption. Notably, cigarette smoking is associated with large vessel disease leading to LVO [13,14,15].
Several mechanisms are associated with the development of LVOs, namely: occlusion at the primary site resulting from intracranial atherosclerosis; embolism from an atherosclerotic extracranial artery or plaque rupture resulting from intracranial vessel occlusion (artery-to-artery embolism); intracranial artery occlusion due to cardioembolism which is usually from atrial fibrillation and cryptogenic etiology [8, 16]. As with the other types of IS, LVOs occur when there is inadequate blood supply to the brain parenchyma, causing cellular, metabolic derangements, inflammatory mechanisms, and activation of the ischemic cascade leading to neuronal cell death. However, a more important feature of LVO is the infarct size and volume which are determined by the degree and length of hypoperfusion and the status of the collateral circulation which is significant in determining stroke severity, progression, and outcome [8, 17].
Large vessel occlusions, if not treated promptly, result in worse outcomes with increased morbidity and mortality. Patients with AIS must be immediately assessed for eligibility to undergo reperfusion therapies, such as intravenous-recombinant tissue Plasminogen Activator (IV-rtPA) and/or mechanical thrombectomy. However, there have been studies demonstrating the limitation of IV-rtPA in the treatment of LVO with successful reperfusion seen only in 13–50% of patients with intracranial ICA or MCA occlusion [16, 18, 19].
In a review by Malhotra et al., LVOs were found to contribute disproportionately to severe functional outcomes after AIS. In their review, LVOs cause about 38.7% of acutely presenting acute cerebral ischemic events, but significantly contributes to poststroke dependence or death in about 61.6%, and poststroke mortality in 95.6% [20]. Endovascular interventions made significant impact in improving the prognosis of patients with LVOs. Using literature-based projections of AIS patients with LVO treatable within 8 h of onset, in the review by Malhotra et al., endovascular thrombectomy could potentially be applied to 21.4% of all the AIS patients and improve the numbers to only 34% of poststroke dependence and death, and 52.8% poststroke mortality. In the meta-analysis by Goyal et al. assessing the efficacy of endovascular thrombectomy in proximal anterior circulation occlusions performed up to 6 h from symptom onset, thrombectomy significantly reduced 90-day disability with a number-needed-to-treat of 2.6 to reduce the modified Rankin Scale Score in one patient by at least one point [8, 21]. Though endovascular treatment revolutionized management of eligible AIS patients, there is still a large gap in access to endovascular thrombectomy between high- and low-income countries [22].
Hypertension remains to be the most important modifiable risk factor for all types of AIS and is said to worsen stroke outcome. In a study by Inoue et al., atrial fibrillation and systolic BP of 170 mmHg or lower were found to have a significant correlation with LVO [23]. Other studies have shown that patients who are known to be hypertensive tend to have less viable or salvageable brain tissue and are prone to develop larger infarctions compared to patients with normal BP levels [24,25,26]. In some animal studies, chronic HTN has detrimental effects on the cerebral circulation, both in the small and large arteries, as it may cause structural abnormalities such as hypertrophy and inward re-modeling. Decrease in the diameter of the vessel lumen and vasodilatory reserve may ensue leading to hypoperfusion and hemodynamic instability contributing to more cerebral damage [27,28,29,30,31,32]. Another factor that was studied in relation to large infarct size and HTN is the status of the collateral circulation especially in chronically hypertensive patients. Studies showed that poor collateral circulation, especially the pial or leptomeningeal collaterals in patients with HTN, may result in large infarctions due to a decrease in salvageable tissue or penumbra [24, 31,32,33].
19.2 Cerebral Small Vessel Disease
Cerebral small vessel disease (CSVD) is a disease affecting the smaller blood vessels that impairs the perfusion to the brain parenchyma. It can affect the small penetrating arteries, arterioles, venules, and capillaries. Arteriosclerosis and small vessel atherosclerosis are the most common pathologies seen related to HTN [34].
The epidemiology of CSVD varies depending on which parameters are taken into account. Lacunar infarcts account for almost 25% of all AIS [35]. Obviously, this does not include the clinically undetected silent ischemic changes that are discovered using cranial Magnetic Resonance Imaging (MRI). There is little data in the literature regarding the prevalence of CSVD as it is challenging to determine its prevalence since most of the small vessel diseases start insidiously and are clinically silent. In many cases, it will take years before they become clinically evident. Moreover, these patients may present with cognitive impairment or vascular dementia later in life.
There are few Asian prevalence studies on CSVD, including white matter hyperintensities (WMH), periventricular hyperintensities (PVHI), silent strokes (SS), and cerebral microbleeds (CMB). In a study by Akthar et al., involving participants from the Middle East and Southeast Asia who were admitted to their stroke service, a preexisting CSVD in the MRI was seen in 65% and distributed as follows: 19.6% with WMH, 33.2% with PVHI, 51.4% with SS, and 22% with CMB. Silent strokes were more common in IS, while CMBs were more common in ICH [7]. In a study by Hilal et al., 3-T brain MRI assessments were performed among participants from Singapore, Hong Kong, and Korea. The results showed that the prevalence of WMH was 36.6%, lacunes was 24.6%, and CMB was 26.9%. Also, the presence of the three small vessel disease parameters demonstrated a sharp increase with increasing age rising from 1.9% in the lowest to 46.2% in the highest 5-year age strata [36].
The pathogenesis of CSVD is still poorly understood although many pathophysiologic mechanisms are in development. Among the most commonly recognized mechanisms are small vascular atherosclerosis and arteriolosclerosis. While arteriolosclerosis increases with age, the hardening and loss of elasticity of the arterioles are further aggravated by HTN as well as diabetes mellitus. Both HTN and age are thought to be the most important risk factors in the development of small vessel disease due to narrowing of the arteriolar lumen and small penetrating arteries [37].
The effects of CSVD on the cerebral tissue are best visualized using MRI. Brain changes that are most commonly seen are WMH, enlarged perivascular spaces, small subcortical infarcts, CMB, lacunar infarcts, and atrophy. In a cohort study conducted in chronically hypertensive patients, a significant correlation was seen between the progression of periventricular white matter lesions and executive function impairment [38].
Over time, chronic HTN leads to a slow and gradual development of minute structural changes in the microvasculature of the cerebral small blood vessels. These are brought about by multiple factors such as chronic inflammation, oxidative stress, and other HTN-related changes that occur over time [37]. The vasculopathy associated with HTN, together with concurrent inflammatory changes, significantly contributes to the development of CSVD. In a paper by Rouhl et al., putative endothelial progenitor cells (cell types that play roles in the regeneration of the endothelial lining of vessels) were lower among hypertensive patients with CSVD in contrast to hypertensive patients without CSVD [39].
Small vessel disease plays a crucial role in various conditions such as aging, stroke, cognitive impairment, and other age-related disabilities including motor-gait issues and mood disorders. It can manifest with significant functional disabilities in the later stage of life. While CSVD may present abruptly such as seen in ICH and lacunar strokes, it may also present insidiously as progressive cognitive decline, among others [40]. Among the important long-term sequelae of CSVD in the Asian population is its effect on cognitive decline and dementia in the elderly. Hilal et al. demonstrated that increasing severity of small vessel disease markers showed significant association with worse cognitive performance independent of the other concomitant risk factors [36].
19.3 Primary Intracerebral Hemorrhage
Intracerebral hemorrhage is defined as any bleeding in the brain parenchyma that may extend into the ventricles and subarachnoid space [41]. Spontaneous, non-traumatic ICH may be primary or secondary. Primary ICH represents about 78–88% of all cases and is usually due to spontaneous rupture of small vessels as complications of chronic HTN or cerebral amyloid angiopathy (CAA) [41], while secondary ICH is due to other known bleeding etiologies such as arteriovenous malformations (AVM), tumors, or cerebral aneurysms.
Intracerebral hemorrhage may be categorized as lobar or deep depending on its location within the brain parenchyma. Lobar ICH refers to hemorrhages which are in the cortical-subcortical brain regions involving one or more lobes of the brain and this accounts for about one-third of all ICH cases. Conversely, deep ICH refers to hemorrhages which are in the deeper subcortical regions such as the basal ganglia and internal capsule, brainstem, and cerebellum, and accounts for the remaining two-thirds [42, 43].
The worldwide incidence of ICH is 10–20 cases per 100,000 individuals [41] but it varies substantially across different countries and race. In a systematic review by van Asch et al., the incidence rate of ICH per 100,000 person-years was 51.8 in Asians, 24.2 in Whites, 22.9 in Blacks, and 19.6 in Hispanics [44]. While it accounts for approximately 10–20% of all strokes, Western countries such as the USA and UK have lower incidence with about 8–15% compared to Asian countries such as Japan, China, and Korea with about 18–24% [6, 45].
A review of various Asian studies explored epidemiological data and highlighted the temporal trends. Studies from Japan, China, Korea, Taiwan, Malaysia, Singapore, India, Bangladesh, Pakistan, Iran, and Israel were included to ensure adequate representation from almost all regions in Asia. The frequency of ICH was higher compared to Western countries. Intracerebral hemorrhage accounts for about 20–39% of cases in these countries except for Iran, Thailand, and Israel with 17%, 13%, and 10%, respectively. The review showed an increase in the absolute number of stroke cases except for Japan where there was a significant decline in ICH incidence probably due to better HTN control [46]. Cases of ICH accounted for more than one-third of stroke cases in Asian countries especially in East and South Asia but notably decreased over time [47].
In the summary of findings from the Global Burden of Disease 2010 Study by Krishnamurthi et al. [48], the absolute number of hemorrhagic strokes (combined ICH and SAH) worldwide between 1990 and 2010 showed a 47% increase. Low- and middle-income countries such as Sub-Saharan Africa, Central Asia, and Southeast Asia showed the largest proportion of ICH incidence of about 80%. Comparing high-income and low- and middle-income countries, the age-adjusted incidence rate of hemorrhagic stroke is reduced by 8% in the former while increased by 22% in the latter. A systematic analysis of the Global Burden of Disease Study 2017 showed higher primary ICH rates in Oceania, East, Central, and Southeast Asia. There was a trend towards greater burden of primary ICH in high-income countries which may be associated with better evaluation by neuroimaging of acute strokes, increased prevalence of diabetes mellitus, and overweight. There was a slightly reduced burden in low- and middle-income countries which may be attributed to epidemiologic transitions in these countries [49].
Hypertension is considered as the most important risk factor for spontaneous, non-traumatic ICH and is seen more commonly in patients with deep ICH than lobar ICH [6]. The second most common risk factor is CAA which is predominantly seen in the elderly population and is regarded as a significant etiology of lobar ICH. Other risk factors include advancing age, anticoagulation, use of antiplatelet agents, leukoaraiosis, prior stroke, hematologic abnormalities, chronic kidney disease, excessive alcohol consumption, and use of sympathomimetic drugs [6, 50].
As mentioned, the primary etiologies leading to primary ICH and vasculopathy are HTN and CAA. Chronic HTN leads to lipohyalinoses of the small penetrating arteries which eventually rupture leading to deep hemorrhages frequently extending to the ventricles [41]. Deep hemorrhages have been attributed to the degeneration of media and smooth muscles of the vessel wall in association with long-standing HTN, advancing age, diabetes, and other vascular risk factors. Most bleeding occurs at or near the bifurcation of the affected arterioles [41]. The underlying mechanism in CAA-associated ICH is a combination of deposition of amyloid-β peptide at capillaries, arterioles, and arteries in the cerebral cortex, leptomeninges, and cerebellum [51] and breakdown of the vessel wall. The amyloid deposits lead to vasculopathic changes such as microaneurysms, concentric splitting of the vessel wall, fibrinoid necrosis, and chronic inflammation of the perivascular space [50]. Lipohyalinoses, which is more prominently associated with chronic HTN, are mostly seen in deep ICH, while CAA is more associated with lobar ICH [6].
The outcome of ICH is variable but comparing with IS, ICH leads to higher mortality and more severe disability. The case fatality rate is approximately 40% at 30 days and about 54% at 1 year [6]. In the acute setting, general predictors of 30-day mortality include size of the hematoma and its expansion, age, presence of coma, intraventricular extension, infratentorial location, and other co-morbid cardiovascular conditions [52]. In two Asian studies, identified independent predictors of poor outcome after primary ICH include fever, low initial Glasgow Coma Scale, large hematoma, intraventricular hemorrhage, and concomitant diabetes [53, 54]. Almost 50% of mortality occurs during the first 2–3 days and are usually associated with neurological complications such as mass effect, increased intracranial pressure, and/or herniation. Deaths occurring after 7 days of hospitalization are usually due to medical complications including pneumonia, aspiration, respiratory distress/failure, or sepsis [55].
The quality of life of ICH survivors are expected to be worse compared to the general population. Caucasians and Asians differ in their views about family values, cultural attitudes, and care preferences which greatly affect the stroke outcome. Despite Asians having worse function, they are more likely to be discharged early and cared for at home, while Caucasians are less likely to be discharged to home despite better functional status [56].
Many studies have identified HTN as a major risk factor for developing primary ICH. There seems to be a stronger association between BP and hemorrhagic stroke compared to that for IS [57] although the relationship between the patterns of changes in BP over time and the risks of ischemic versus hemorrhagic stroke still remains unclear. Elevated BP is associated with an increased risk of stroke incidence and mortality. In the Asia-Pacific Cohort Studies Collaboration study [58], the risk of ischemic and hemorrhagic stroke incidence increased with elevations in BP levels in a dose-dependent manner from the systolic BP level of 115 mmHg. The INTERSTROKE study [59] identified that self-reported HTN of BP ≥ 140/90 mmHg conferred a population-attributable risk of about 56.4% for hemorrhagic stroke. The Hisayama study in Japan [60] showed a considerable decline in stroke incidence. The age-adjusted ICH incidence declined in men and women particularly with a significant decline of 61% from the first cohort (enrolled in 1961) to the second cohort (enrolled in 1974) in men and sustained in both sexes in the third cohort (enrolled in 1988). During this period, the prevalence of severe HTN was significantly decreased and the use of antihypertensive medication increased. With all of these studies it is clear without any doubt that better control of HTN leads to better protection against hemorrhagic strokes.
19.4 Subarachnoid Hemorrhage
Subarachnoid hemorrhage means blood between the arachnoid layer and pia mater. Bleeding into this space is caused by a number of factors, most commonly trauma (tearing of blood vessels) and ruptured intracranial aneurysms. Other causes include presence of an AVM, blood dyscrasia, anticoagulation, and intracranial hemorrhage. This section focuses on aneurysmal SAH (aSAH) since HTN is an independent risk factor for the development, growth, and rupture of an intracranial aneurysm.
The worldwide incidence of aSAH is 7.9 per 100,000 person-years [61]. Looking at temporal trends, the incidence of SAH declined from 10.2 per 100,000 person-years in 1980 to 6.1 per 100,000 person-years in 2010. The incidence widely varies across geographic regions [62]. In 2010, the incidence per 100,000 person-years are as follows: 6.9 in North America, 5.1 in South and Central America, 5.1 in Switzerland, 7.4 in Australia/New Zealand, and 3.7 in Asia with the exception of Japan, 28 [61]. In Asia, registries from different countries showed the incidence of SAH as follows: 6.2 in China, 3.3 in Iran, 4.5 in India, 14.2 in Israel, 0.5 in Kuwait, while 13.7–27.9 in Japan [63]. There is a 2.0% decline annually in Asian countries except Japan, where an increase of 1.6% annually was noted [61].
Known risk factors for aneurysm formation, growth, and rupture include HTN, cigarette smoking, family history, and connective tissue disease. Particularly in the Asia-Pacific region, cigarette smoking and elevated systolic BP each doubles the risk of aSAH [63].
Intracranial aneurysms are pathologic protrusions from the intracranial arteries. Compared to the normal vessels, the walls of aneurysms are composed of a very thin or absent tunica media, and an absent or fragmented internal elastic lamina [64]. Most intracranial aneurysms are acquired and not congenital. Several factors contribute to aneurysm formation [65]. Turbulent and hyperdynamic blood flow produces changes in the vessel wall and subsequent aneurysm development. Hemodynamic stress produces excessive wear and tear in the vessels and eventual breakdown of the internal elastic lamina. Turbulence further produces vibrations resulting in structural fatigue of the vessel wall. The above-mentioned risk factors further play contributory roles in aneurysm development and growth.
However, the rupture rate of aneurysms varies and is influenced by several risk factors: size, growth rate, location, prior hemorrhage, family history, and race. Some aneurysms do not rupture at all and are only found incidentally or during autopsy series. Two of the largest prospective studies on unruptured intracranial aneurysms (ISUIA [66] and UCAS [67]) have identified that smaller aneurysms have lower rates of rupture than larger ones. Low risk of rupture for both studies was seen with aneurysms <7 mm in diameter, and for which growth rate is also slower. However, this rupture risk is modified by the location: with posterior circulation aneurysms generally having the highest rate of rupture, followed by anterior circulation, and lowest with cavernous carotid artery aneurysms [66, 67].
Aneurysmal SAH is associated with significant neurologic morbidity and mortality especially if left untreated. The risk of rebleeding is highest in the first few hours from rupture and this re-rupture is associated with an even higher mortality. Aneurysm treatment by surgical or endovascular means is the only way to prevent rebleeding.
Around 18% of patients with aSAH die even before reaching the hospital [68]. Even among patients who get evaluated in the hospital, rates of early mortality are still high due to rebleeding, vasospasm and cerebral ischemia, hydrocephalus, increased intracranial pressure, seizures, and cardiac complications. Due to medical advances and more research, the case fatality rate has significantly decreased from 50% to about 30% if treated in a timely manner [69]. Among survivors, long-term neurologic complications include cognitive dysfunction, epilepsy, and focal deficits.
As mentioned above, HTN is a major risk factor for aneurysm formation, growth, and eventual rupture, causing SAH. In a systematic review, the presence of HTN has a statistically significant relative risk of 2.5% (95% CI 2.0–3.1) in longitudinal studies and an odds ratio of 2.6% (95% CI 2.0–3.1) in case-control studies [3]. There is a corresponding decrease in the incidence of SAH per unit decrease of BP: 7.1% decrease per mmHg of systolic BP decrease, while 11.5% for diastolic BP [61]. A global decline in the incidence of aSAH is noted and this is partly due to a parallel decline in prevalence of HTN. In China, it was found that higher average levels of BP were linearly and positively associated with SAH, and elevated BP accounted for about 23% of all SAH cases [70].
After rupture of an intracranial aneurysm, BP control is of paramount importance to avoid further morbidity. Although optimal BP therapy in SAH is not clear, hypotension should definitely be avoided. While lowering the BP may decrease the risk of rebleeding of an unsecured aneurysm, it may also present a risk of cerebral infarction if too low. Some guidelines recommend to have a goal of maintaining SBP <160 mmHg, while others use the mean arterial pressure (MAP) of <110 mmHg. It may be reasonable to use the patient’s premorbid baseline BP control to define targets of therapy [71, 72]. Intravenous agents, such as labetalol or nicardipine, are preferred for BP control because they can easily be titrated.
19.5 Blood Pressure Variability and Its Impact in Stroke and Vascular Dementia
Normally, there are some short-term fluctuations in BP during the 24-h period which are largely influenced by the circadian modulations. In about 10–20% of the population, there is a physiological reduction of nocturnal BP. Blood pressure variability can be classified as very-short-term (beat-to-beat), short-term (during 24 h), mid-term (day-by-day), long-term (less than 5 years), and very-long-term (more than 5 years) [73]. This is associated with hypertension-mediated-organ-damage or target-organ-damage, and in some cases, it triggers significant vascular events during transient rises in the BP.
Blood pressure variability is a novel factor in the development of cardiac events, stroke, and cognitive impairment. Emerging literatures are showing consequences of increased BPV among certain populations including people with morning surge HTN, night sleep HTN, non-dippers, reverse dippers, and dippers with morning surges of BP. The wide fluctuations of BP in these instances are thought to increase the cerebral microcirculatory changes and cumulative lesions in the brain—be it ischemic (as seen in ischemic white matter changes) or hemorrhagic (as observed in CMBs).
Increasing BPV seems to negatively impact stroke outcome in the acute phase and probably, even in the subacute phase. This is seen in both the acute ischemic and hemorrhagic stroke types. Why this is so is not yet fully understood. One mechanism that possibly explains the negative effect of BPV is the impaired cerebral autoregulation in the region affected with stroke. For instance, in AIS, a drop in the cerebral perfusion secondary to BPV can worsen the condition of the ischemic core and convert the ischemic penumbra into an enlarging infarct core [74]. Chung et al. considered BPV as an independent factor that is associated with early neurological deterioration [75]. Increased BPV can also negatively impact hemorrhagic strokes. Very high BP can increase hematoma size and brain edema. A significant drop in systolic BP can also be detrimental as it potentially can increase perihematomal ischemia and cause acute renal hypoperfusion leading to acute kidney injury [76].
Aside from ischemic and hemorrhagic strokes, large BPV is also associated with cognitive impairment and dementia. There is mounting data linking marked BPV to higher risk of heart diseases, strokes, and dementia, even beyond the effect of the BP per se [77]. In a Japanese elderly population study by Oishi et al. on the relationship of BPV and incident dementia, the results suggested that increased day-to-day BPV is independent of average home BP and is a significant risk factor for the development of all-cause dementia, vascular dementia, and Alzheimer’s disease [78].
In a systematic review and meta-analysis of prospective cohort studies that looked into the association of BPV with the presence or progression of CSVD markers such as WMH, lacunes, and CMBs in MRI, the analysis showed that the association of systolic BPV with the presence of lacunes and CMBs were not statistically significant. However, increased BPV was associated with increased odds of presence or progression of WMHs [79].
A study by Liu et al. conducted in China among the geriatric community dwelling areas looked at the effect of systolic BP variability through self-measured BP at home for 7 consecutive days. Mini Mental State Examination (MMSE) scores as well as brain MRI WMH at baseline and at final follow-up visits were taken. After an average of 2.3 years, a decline in MMSE score and an increase in brain MRI WMHs were noted. The results of the study suggested that excessive variability in self-measured systolic BP exacerbates the progression of cognitive impairment and brain white matter lesions in the oldest-old geriatric population [80].
References
Feigin VL. Stroke in developing countries: can the epidemic be stopped and outcomes improved? Lancet Neurol. 2007;6(2):94–7.
Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182–7.
Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120:439–48.
Venketasubramanian N, Yoon BW, Pandian J, Navarro JC. Stroke epidemiology in south, east, and south-East Asia: a review. J Stroke. 2017;19:286–94.
Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702–9.
An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke. 2017;19:3–10.
Akhtar N, Salam A, Kamran S, D’Souza A, Imam Y, Own A, et al. Pre-existing small vessel disease in patients with acute stroke from the Middle East, Southeast Asia, and Philippines. Transl Stroke Res. 2018;9:274–82.
Rennert RC, Wali AR, Steinberg JA, Santiago-Dieppa DR, Olson SE, Pannell JS, et al. Epidemiology, natural history, and clinical presentation of large vessel ischemic stroke. Clin Neurosurg. 2019;85:S4–8.
Lakomkin N, Dhamoon M, Carroll K, Singh IP, Tuhrim S, Lee J, et al. Prevalence of large vessel occlusion in patients presenting with acute ischemic stroke: a 10-year systematic review of the literature. J Neurointerv Surg. 2019;11(3):241–5.
Rai AT, Seldon AE, Boo S, Link PS, Domico JR, Tarabishy AR, et al. A population-based incidence of acute large vessel occlusions and thrombectomy eligible patients indicates significant potential for growth of endovascular stroke therapy in the USA. J Neurointerv Surg. 2017;9:722–6.
Smith WS, Lev MH, English JD, Camargo EC, Chou M, Johnston SC, et al. Significance of large vessel intracranial occlusion causing acute ischemic stroke and tia. Stroke. 2009;40:3834–40.
Bang OY. Considerations when subtyping ischemic stroke in Asian patients. J Clin Neurol. 2016;12(2):129–36.
Tan KS, Navarro JC, Wong KS, Huang YN, Chiu HC, Poungvarin N, et al. Clinical profile, risk factors and aetiology of young ischaemic stroke patients in Asia: a prospective, multicentre, observational, hospital-based study in eight cities. Neurol Asia. 2014;19:117–27.
Ihle-Hansen H, Thommessen B, Wyller TB, Engedal K, Fure B. Risk factors for and incidence of subtypes of ischemic stroke. Funct Neurol. 2012;27:35–40.
Bejot Y, Caillier M, Ben Salem D, Couvreur G, Rouaud O, Osseby GV, et al. Ischaemic stroke subtypes and associated risk factors: a French population based study. J Neurol Neurosurg Psychiatry. 2008;79:1344–8.
Al Kasab S, Holmstedt CA, Jauch EC, Schrock J. Acute ischemic stroke due to large vessel occlusion. Emerg Med Rep. 2018;39:13–22.
Brouns R, De Deyn PP. The complexity of neurobiological processes in acute ischemic stroke. Clin Neurol Neurosurg. 2009;111(6):483–95.
De Silva DA, Brekenfeld C, Ebinger M, Christensen S, Barber PA, Butcher KS, et al. The benefits of intravenous thrombolysis relate to the site of baseline arterial occlusion in the echoplanar imaging thrombolytic evaluation trial (EPITHET). Stroke. 2010;41:295–9.
Jansen O, Von Kummer R, Forsting M, Hacke W, Sartor K. Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. Am J Neuroradiol. 1995;16:1977–86.
Malhotra K, Gornbein J, Saver JL. Ischemic strokes due to large-vessel occlusions contribute disproportionately to stroke-related dependence and death: a review. Front Neurol. 2017;8:651.
Goyal M, Menon BK, Van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Tsang ACO, Yang IH, Orru E, Nguyen QA, Pamatmat RV, Medhi G, et al. Overview of endovascular thrombectomy accessibility gap for acute ischemic stroke in Asia: a multi-national survey. Int J Stroke. 2020;15:516–20.
Inoue M, Noda R, Yamaguchi S, Tamai Y, Miyahara M, Yanagisawa S, et al. Specific factors to predict large-vessel occlusion in acute stroke patients. J Stroke Cerebrovasc Dis. 2018;27:886–91.
Cipolla MJ, Liebeskind DS, Chan SL. The importance of comorbidities in ischemic stroke: impact of hypertension on the cerebral circulation. J Cereb Blood Flow Metab. 2018;38(12):2129–49.
Lima FO, Furie KL, Silva GS, Lev MH, Camargo ÉCS, Singhal AB, et al. The pattern of leptomeningeal collaterals on CT angiography is a strong predictor of long-term functional outcome in stroke patients with large vessel intracranial occlusion. Stroke. 2010;41:2316–22.
Menon BK, Smith EE, Coutts SB, Welsh DG, Faber JE, Goyal M, et al. Leptomeningeal collaterals are associated with modifiable metabolic risk factors. Ann Neurol. 2013;74:241–8.
Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, et al. Relationship of blood pressure, antihypertensive therapy, and outcome in ischemic stroke treated with intravenous thrombolysis: retrospective analysis from safe implementation of thrombolysis in stroke-international stroke thrombolysis register (SITS-ISTR). Stroke. 2009;40:2442–9.
Leonardi-Bee J, Bath PMW, Phillips SJ, Sandercock PAG. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke. 2002;33:1315–20.
Strandgaard S. Autoregulation of cerebral circulation in hypertension. Acta Neurol Scand Suppl. 1978;57:1–82.
Muller M, Van Der Graaf Y, Visseren FL, Mali WPTM, Geerlings MI. Hypertension and longitudinal changes in cerebral blood flow: the SMART-MR study. Ann Neurol. 2012;71:825–33.
Coyle P, Heistad DD. Development of collaterals in the cerebral circulation. Blood Vessels. 1991;28(1-3):183–9.
Shuaib A, Butcher K, Mohammad AA, Saqqur M, Liebeskind DS. Collateral blood vessels in acute ischaemic stroke: a potential therapeutic target. Lancet Neurol. 2011;10(10):909–21.
Zhang H, Prabhakar P, Sealock R, Faber JE. Wide genetic variation in the native pial collateral circulation is a major determinant of variation in severity of stroke. J Cereb Blood Flow Metab. 2010;30:923–34.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;10(10):689–701.
Petty GW, Brown RD, Whisnant JP, Sicks JRD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of functional outcome, survival, and recurrence. Stroke. 2000;31:1062–8.
Hilal S, Mok V, Youn YC, Wong A, Ikram MK, Chen CLH. Prevalence, risk factors and consequences of cerebral small vessel diseases: data from three Asian countries. J Neurol Neurosurg Psychiatry. 2017;88:669–74.
Liu Y, Dong YH, Lyu PY, Chen WH, Li R. Hypertension-induced cerebral small vessel disease leading to cognitive impairment. Chin Med J (Engl). 2018;131:615–9.
Uiterwijk R, Staals J, Huijts M, De Leeuw PW, Kroon AA, Van Oostenbrugge RJ. MRI progression of cerebral small vessel disease and cognitive decline in patients with hypertension. J Hypertens. 2017;35:1263–70.
Rouhl RPW, Mertens AECS, Van Oostenbrugge RJ, Damoiseaux JGMC, Debrus-Palmans LL, Henskens LHG, et al. Angiogenic T-cells and putative endothelial progenitor cells in hypertension-related cerebral small vessel disease. Stroke. 2012;43:256–8.
Pasi M, Cordonnier C. Clinical relevance of cerebral small vessel diseases. Stroke. 2020;51:47–53.
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344:1450–60.
Flaherty ML, Woo D, Haverbusch M, Sekar P, Khoury J, Sauerbeck L, et al. Racial variations in location and risk of intracerebral hemorrhage. Stroke. 2005;36:934–7.
Grysiewicz RA, Thomas K, Pandey DK. Epidemiology of ischemic and hemorrhagic stroke: incidence, prevalence, mortality, and risk factors. Neurol Clin. 2008;26:871–95.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9:167–76.
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480687 adults. Circulation. 2017;135:759–71.
Toyoda K. Epidemiology and registry studies of stroke in Japan. J Stroke. 2013;15:21.
Mehndiratta MM, Khan M, Mehndiratta P, Wasay M. Stroke in Asia: geographical variations and temporal trends. J Neurol Neurosurg Psychiatry. 2014;85:1308–12.
Krishnamurthi RRV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013;1:e259–81.
Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of Ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54:171–9.
Aguilar MI, Brott TG. Update in intracerebral hemorrhage. Neurohospitalist. 2011;1:148–59.
Rosand J, Hylek EM, O’Donnell HC, Greenberg SM. Warfarin-associated hemorrhage and cerebral amyloid angiopathy: a genetic and pathologic study. Neurology. 2000;55:947–51.
Safatli DA, Günther A, Schlattmann P, Schwarz F, Kalff R, Ewald C. Predictors of 30-day mortality in patients with spontaneous primary intracerebral hemorrhage. Surg Neurol Int. 2016;7:S510–7.
Poungvarin N, Suwanwela NC, Venketasubramanian N, Wong LKS, Navarro JC, Bitanga E, et al. Grave prognosis on spontaneous intracerebral haemorrhage: GP on stage score. J Med Assoc Thail. 2006;89:84–93.
Chen HS, Hsieh CF, Chau TT, Yang CD, Chen YW. Risk factors of in-hospital mortality of intracerebral hemorrhage and comparison of ICH scores in a Taiwanese population. Eur Neurol. 2011;66:59–63.
Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
McNaughton H, Feigin V, Kerse N, Barber PA, Weatherall M, Bennett D, et al. Ethnicity and functional outcome after stroke. Stroke. 2011;42:960–4.
Zia E, Hedblad B, Pessah-Rasmussen H, Berglund G, Janzon L, Engström G. Blood pressure in relation to the incidence of cerebral infarction and intracerebral hemorrhage—hypertensive hemorrhage: debated nomenclature is still relevant. Stroke. 2007;38:2681–5.
Lawes C. Blood pressure indices and cardiovascular disease in the Asia Pacific region: a pooled analysis. Hypertension. 2003;42:69–75.
O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388:761–75.
Kubo M, Kiyohara Y, Kato I, Tanizaki Y, Arima H, Tanaka K, et al. Trends in the incidence, mortality, and survival rate of cardiovascular disease in a Japanese community: the Hisayama study. Stroke. 2003;34:2349–54.
Etminan N, Chang HS, Hackenberg K, De Rooij NK, Vergouwen MDI, Rinkel GJE, et al. Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol. 2019;76:588–97.
Hughes JD, Bond KM, Mekary RA, Dewan MC, Rattani A, Baticulon R, et al. Estimating the global incidence of aneurysmal subarachnoid hemorrhage: a systematic review for central nervous system vascular lesions and meta-analysis of ruptured aneurysms. World Neurosurg. 2018;115:430–447.e7.
Feigin V, Parag V, Lawes CMM, Rodgers A, Suh I, Woodward M, et al. Smoking and elevated blood pressure are the most important risk factors for subarachnoid hemorrhage in the Asia-Pacific region: an overview of 26 cohorts involving 306620 participants. Stroke. 2005;36:1360–5.
Austin G, Fisher S, Dickson D, Anderson D, Richardson S. The significance of the extracellular matrix in intracranial aneurysms. Ann Clin Lab Sci. 1993;23:97–105.
Wiebers DO, Piepgras DG, Meyer FB, Kallmes DF, Meissner I, Atkinson JLD, et al. Pathogenesis, natural history, and treatment of unruptured intracranial aneurysms. Neuroradiol J. 2006;19:504–15.
Wiebers DO. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–10.
Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012;366:2474–82.
Lindbohm JV, Kaprio J, Jousilahti P, Salomaa V, Korja M. Risk factors of sudden death from subarachnoid hemorrhage. Stroke. 2017;48:2399–404.
Mackey J, Khoury JC, Alwell K, Moomaw CJ, Kissela BM, Flaherty ML, et al. Stable incidence but declining case-fatality rates of subarachnoid hemorrhage in a population. Neurology. 2016;87:2192–7.
McGurgan IJ, Clarke R, Lacey B, Kong XL, Chen Z, Chen Y, et al. Blood pressure and risk of subarachnoid hemorrhage in China. Stroke. 2019;50:38–44.
Diringer MN, Bleck TP, Hemphill JC, Menon D, Shutter L, Vespa P, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care. 2011;15:211–40.
Connolly ES, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43(6):1711–37.
Rosei EA, Chiarini G, Rizzoni D. How important is blood pressure variability? Eur Heart J Suppl. 2020;22:E1–6.
Zhang T, Wang X, Wen C, Zhou F, Gao S, Zhang X, et al. Effect of short-term blood pressure variability on functional outcome after intra-arterial treatment in acute stroke patients with large-vessel occlusion. BMC Neurol. 2019;19(1):228.
Chung JW, Kim N, Kang J, Park SH, Kim WJ, Ko Y, et al. Blood pressure variability and the development of early neurological deterioration following acute ischemic stroke. J Hypertens. 2015;33:2099–106.
Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med. 2016;375:1033–43.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Oishi E, Ohara T, Sakata S, Fukuhara M, Hata J, Yoshida D, et al. Day-to-day blood pressure variability and risk of dementia in a general Japanese elderly population: the Hisayama study. Circulation. 2017;136:516–25.
Ma Y, Song A, Viswanathan A, Blacker D, Vernooij MW, Hofman A, et al. Blood pressure variability and cerebral small vessel disease: a systematic review and meta-analysis of population-based cohorts. Stroke. 2020;51:82–9.
Liu Z, Zhao Y, Zhang H, Chai Q, Cui Y, Diao Y, et al. Excessive variability in systolic blood pressure that is self-measured at home exacerbates the progression of brain white matter lesions and cognitive impairment in the oldest old. Hypertens Res. 2016;39:245–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Diaz, A.B.F., Belen, A.A., Tenorio-Javier, A.M.J., Juangco, D.N.A. (2022). Cerebrovascular Disease in Asia: Causative Factors. In: Ram, C.V.S., Teo, B.W.J., Wander, G.S. (eds) Hypertension and Cardiovascular Disease in Asia. Updates in Hypertension and Cardiovascular Protection. Springer, Cham. https://doi.org/10.1007/978-3-030-95734-6_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-95734-6_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-95733-9
Online ISBN: 978-3-030-95734-6
eBook Packages: MedicineMedicine (R0)