Abstract
Basilar invagination (BI) and chronic atlanto-axial dislocation (AAD) are the most common congenital anomalies of the CVJ, can occur combined and become symptomatic when produce a ventral cervicomedullary compression. The standard transoral approach (TOA) allows a satisfactory surgical exposure and decompression in more then 80% of patients with BI and AAD. In cases of limited mandibular excursion (i.e. interdental space ≤30 mm) and/or severe basilar invagination (odontoid tip projecting ≥20 mm above the Chamberlain’s line) with a resultant neural compression at the level of the nasopharynx, the endonasal endoscopic approach is an effective alternative option. In patients with tonsillar prolapse and basilar invagination, transoral decompression allows the ascent of cerebellar tonsils into the posterior fossa and the resolution of associated syringomyelia due to the restoration to normal of CSF flow at the CVJ level. The occurrence of acute or delayed spinal instability (occipito-atlantal, atlanto-axial, or occipito-atlanto-axial instability) after transoral decompression is invariably high and requires posterior fixation and fusion. In our experience, the single anesthesia transoral decompression and subsequent posterior fusion eliminate the risk of postoperative instability and allow to mobilize the patients as soon as possible. After an adequate learning curve and following the basic tenets of skull base surgery, the approach related-morbidity in standard TOA is less than 10%.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Transoral approach
- Basilar invagination
- Atlanto-axial dislocation
- Craniovertebral junction
- Craniovertebral malformation
Malformations of the craniovertebral junction (CVJ) encompass a wide range of different bony abnormalities involving the axis, the atlas and the occipital bone. Basilar invagination (BI) and chronic atlanto-axial dislocation (AAD) are the most common congenital anomalies of the CVJ, can occur combined and become symptomatic when produce a ventral cervicomedullary compression. BI consists in the congenital prolapse of the spinal column into the skull base and is radiologically defined as the occurrence of the odontoid tip more than 2.5 mm above the Chamberlain’s line [1] (Fig. 19.1). The term platybasia refers to an angle greater than 140° between the clivus and the plane of the anterior cranial fossa (basal angle) and is an anthropological measure without pathological implications itself [2]. Platybasia can occur in association with BI. In this case shortening and horizontalization of the basiocciput displace the foramen magnum cranially with subsequent anterior (ventral) invagination of the odontoid (Fig. 19.2). Basilar impression is a term often erroneously used as a synonym of BI and consists in an acquired BI related to bone-softening disorders such as hyperparathyroidism, Paget’s disease, Hurler’s syndrome, and rickets [3]. BI and AAD are usually irreducible on skeletal traction and require surgical treatment when cause progressive cervicomedullary compression resulting in disabling neurological deficits [4]. Although the transoral approach (TOA) to the CVJ was originally described by Kanavel in 1917 to remove a bullet lodged between the atlas and the clivus, it wasn’t until the late 1970s that Menezes et al. proposed a rationale algorithm for the CVJ malformations based on the stability, reducible malformation and site of encroachment, that is still valid today [3, 5]. In this chapter, based on our experience with over the past four decades, we describe the surgical nuances of TOA that allow to achieve a satisfactory decompression of BI and AAD minimizing the postoperative complications [4, 6,7,8,9,10].
Treatment Algorithm for BI and AAD
The surgical strategy is dictated by extensive preoperative neuroradiological investigation including MRI, CT scan with flexion and extension views. In BI and AAD the site of encroachment is generally only anterior particularly when an associated atlas assimilation is present (Fig. 19.3). The detection of irreducible ventral compression is an indication for TOA [2,3,4, 6,7,8,9,10,11,12,13,14,15,16,17]. In our experience skeletal traction is not effective in congenital CVJ malformations and is poorly tolerated by the patients. In the rare instances of concomitant fixed posterior compression, an additional foramen magnum decompression can be considered [4]. Limitations of TOA are the limited mandibular excursion (i.e. interdental space ≤30 mm) and severe basilar invagination (odontoid tip projecting ≥20 mm above the Chamberlain’s line) with a resultant neural compression at the level of the nasopharynx [4, 12]. In these cases, we selected transmaxillary approaches [4]. The Le Fort I osteotomy with down-fracture of the maxilla allows exposure from the sphenoid sinus to the middle clivus and can be required in patients with severe basilar invagination [18]. The Le Fort osteotomy with palatal split (transmaxillary palatal split approach or open door maxillotomy approach) increases the caudal exposure compared to Le Fort I osteotomy and was used in patients with inability of sufficiently open the mouth [4, 19]. Over time, we moved away from performing transmaxillary approaches in cases of limited mandibular excursion and severe basilar invagination with neural compression at the level of the nasopharynx. In these situations, we now favor endonasal endoscopic approach (EEA) that allow a cranial exposure from the anterior fossa floor to the superior aspect of the clivus and a caudal exposure dictated by the nasopalatine line [12, 17, 20,21,22,23]. According to our experience, the standard TOA allows a satisfactory surgical exposure and decompression in more then 80% of patients with BI and AAD [4]. The rate of tonsillar prolapse in patients with CVJ malformations is between 33 and 38% [4, 16, 24,25,26]. The surgical treatment of this association is still matter of controversy. Several studies reported early deterioration or more often delayed worsening in patients treated with foramen magnum decompression due to postoperative angulation of cervicomedullary junction and progressive cranial settling [4, 27]. According to our experience corroborated by recent literature, transoral decompression is affective in removal of the CSF obstruction and the level of the cervicomedullary junction in most patients with fixed CVJ malformations and tonsillar prolapse [4, 27]. In these patients the tonsillar herniation is the result of reduced posterior fossa volume due to the infolding of the exoccipital bone which is exacerbated by the prolapse of the odontoid peg though the foramen magnum. After extensive anterior decompression, the ascent of cerebellar tonsils into the posterior fossa and the resolution of associated syringomyelia are generally observed and support the restoration to normal of CSF flow at the CVJ level [4, 27]. The occurrence of acute or delayed spinal instability (occipito-atlantal, atlanto-axial, or occipito-atlanto-axial instability) after transoral decompression is invariably high [7, 8, 28,29,30]. The single anesthesia transoral decompression and subsequent posterior fixation and fusion eliminate the risk of postoperative instability and allow to mobilize the patients as soon as possible [4, 8].
Transoral Approach
Preoperative Assessment, Anesthesiologic Considerations and Positioning
Careful assessment of preoperative neuroradiological investigations is required to establish the correct surgical strategy. TOA is indicated in patients with BI and/or AAD inducing fixed ventral compression of the cervicomedullary junction mainly located at the level of the oropharynx. According to our experience the standard TOA might expose the odontoid projecting ≤20 mm above the Chamberlain’s line [4]. TOA can be performed in patients with an interdental working distance of at least 30 mm and without active nasopharyngeal infection [3, 4]. Fiberoptic nasotracheal intubation is routinely used in all transoral cases. We reserve tracheostomy only in patients with preoperative brain stem compromise and lower cranial nerve dysfunction [4]. The patient is positioned supine with the head fixed in a Mayfield headholder and extended 10°–20° according to the severity of the BI. In fact, the head extension improves the rostral exposure of the CVJ and is particularly effective in patients with severe BI. In addition, the intraoperative use of moderate Trendelenburg position can help the rostral visualization of the CVJ. Anatomical studies demonstrated that division of the soft palate provides nearly 10 mm of clival exposure [31]. However, to reduce postoperative rhinolalia and nasal regurgitation we avoid soft palate splitting and we retract the soft palate with two rubber catheters inserted through the nares and stitched to the uvula. A dedicated transoral system (Crockard transoral instruments, Codman Raynham, MA) including retractors and extra-long instruments is required for an effective surgery. Lateral fluoroscopy is reliable in confirming the location of anterior tubercle of the atlas, which is easily palpated transorally, and in providing information on the extent of cranio-caudal exposure during the operation. Frameless navigation systems provide additional information of the medial-lateral orientation. Neurophysiological monitoring is used throughout the procedure and allows functional assessment of spinal cord.
Illustration demonstrating the transoral atlas-sparing technique. This technique is generally feasible in patients with mild basilar invagination and/or fixed atlanto-axial dislocation. (a) The base of the dens and few millimeters of the inferior half of the anterior arch of the atlas are resected with high speed drill. (b) When the base of the dens is transected, the ligaments are sectioned while the odontoid is grasped with an odontoid rongeur and pulled inferiorly without any pressure on the cervicomedullary junction. (c) Odontoid removal allows exposure of the cervicomedullary region which appears decompressed. (Modified with permission from Acta Neurochir (Wien) 2014;156(6):1231–1236)
Incision and Soft Tissue Dissection
The surgical procedure is entirely performed with the aid of the surgical microscope while the surgeon is seated at the top of patient’s head. The posterior pharynx is infiltrated with 1% lidocaine and epinephrine, and a midline incision along the median raphe of the posterior pharyngeal wall is carried through the mucosa and the pharyngeal muscles. The incision is extended cranially and caudally depending on the peculiar anatomy of the single patient. Monopolar cautery is used to dissect the pharyngeal constrictor, longus colli and longus capitis muscles which are elevated in a single layer and maintained laterally using tooth-bladed pharyngeal retractors. After dissection of the anterior longitudinal ligament, the anterior arch of C1, the inferior tip of the clivus and the ventral surface of the body of C2 are exposed.
Transoral Atlas-Sparing Technique
Preservation of anterior arch of C1 during the TOA minimizes postoperative instability of the CVJ and is usually feasible in the treatment of retro-odontoid pannus. However, it in can be achieved in patients with fixed AAD and in selected cases of mild basilar invagination (Fig. 19.4) [4, 9, 10, 29, 32]. When the C1 ring is preserved, the stability of the CVJ can be obtained with C1–C2 screw techniques instead of occipitocervical fusion [10, 32]. Biomechanical studies demonstrated that interruption of the anterior arch of the atlas can promote lateral spreading of C1 and subsequent cranial settling with resultant kinking of bulbo-medullary junction and progressive neurological worsening [28, 29, 33]. The atlas-sparing technique requires drilling the base of the dens and approximately 5 mm of the inferior half of the anterior arch of C1. After transection of the base of the dens, the odontoid is grasped with an odontoid rongeur and pulled inferiorly while the alar and apical ligaments are sharply dissected without pressure on the cervicomedullary junction (Fig. 19.5). This maneuver allows the surgeon to remove the invaginated odontoid in an en bloc fashion without pressure on the cervicomedullary junction (Fig. 19.6). When AAD and BI are associated with atlas assimilation, preservation of the anterior ring of the atlas is not a concern. In this scenario after transoral decompression a posterior occipito-cervical fixation and fusion is mandatory also in case of atlas preservation.
Intraoperative photographs of the patient presented in Fig. 19.6. The tongue is oriented at the top of the photograph with the palate at the bottom. (a) The posterior wall of the pharynx is exposed after retraction of the soft palate into the rhinopharynx. The nasotracheal tube is mobilized laterally using the Crockard retractor. (b) After midline incision of the posterior pharyngeal wall and dissection of the longus colli muscles, the bony surface of the craniovertebral junction is exposed. (c) The drilling involves the dens and the inferior rim of the anterior arch of C1. (d) The remaining shell of the base of the dens is removed with Kerrison rongeur. (e) The offending odontoid peg (asterisk) is removed after section of the alar and apical ligaments. (f) After generous bony decompression the ventral surface of cervicomedullary junction is exposed. (g) The mucosa and pharyngeal muscles are closed in a single layer. (h) Normal appearance of oropharyngeal mucosa at the end of the transoral approach
Case illustration of a 64-year-old lady with craniovertebral junction malformation suitable for transoral atlas-sparing approach. Preoperative sagittal T2-weighted image (a) and sagittal reformatted (b), and axial (c) CT scan showing basilar invagination, atlas assimilation and atlanto-axial dislocation with severe compression of the cervicomedullary junction. The soft palate was retracted in the nasopharynx (d) and fluosocopy confirmed the location of the anterior arch of the atlas (e). The altas-sparing technique allowed wide decompression and preservation of the atlas as seen on postoperative sagittal reformatted (f) and axial (g) CT scan images
Transoral Trans-atlas Technique
In patients with severe basilar invagination transection of anterior arch of C1 is required to expose and resect the offending odontoid peg in a piecemeal fashion (Fig. 19.7). After atlas resection using a 3- to 4-mm diamond burr the odontoid is shaved until a thin sheet remains, which is removed with Kerrison and curettes (Fig. 19.8). The retro-odontoid ligaments are dissected only when appear thick and distorting the dura avoiding unintentional dural tearing. After decompression, hemostasis is achieved and the wound is closed in a single layer with 2-0 Vicryl sutures [4, 10]. It our policy to perform the posterior fixation and fusion during the same anesthesia session to eliminate the risk of acute postoperative instability and to mobilize the patients early in the postoperative period.
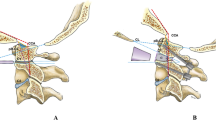
Illustration demonstrating the transoral trans-atlas technique. This technique is required in patients with moderate basilar invagination (odontoid peg projecting ≤20 mm above the Chamberlain’s line). (a) After transection of the anterior arch of the atlas, the odontoid is shelled out with high speed drill. (b) the residual shell is progressively removed with kerrison rongeurs. (c) After careful dissection of the retrodental ligaments the dura of the craniovertebral junction is exposed. (Acta Neurochir (Wien) 2014;156(6):1231–1236. Reprinted with permission)
Case illustration of a 72-year-old lady with craniovertebral junction malformation requiring transoral trans-atlas technique. Sagittal reformatted CT scan (a) and 3D CT reconstruction (b) domonstrating severe basilar invagination, atlas assimilation and fixed atlanto-axial dislocation. Intraoperative fluoroscopy (c) shows initial resection of the dens. Complete resection of the offending odontoid peg required transection of the anterior arch of C1, as seen on postoperative CT scan (d)
Postoperative Management
Postoperatively, patients are transferred to the intensive care unit where the endotracheal tube is maintained for 12–18 h, depending on soft tissue swelling and respiratory function. Nutrition is administered intravenous, and patients are allowed to sip cold fluids only after 3 days. Broad spectrum antibiotics are administered for 72 h. A CT scan of the cranio-cervical region with sagittal and coronal reconstructions is done before patients are mobilized to assess the extent of CVJ decompression and the correct position of posterior fixation system.
Postoperative Complications and Their Avoidance
In recent clinical studies complications after TOA are minimal ranging from 7 to 10% [15, 32]. Potential complications include CSF leak and meningitis, velopharyngeal dysfunction, neurological deterioration, vascular injury, pharyngeal wound breakdown, and postoperative soft tissue swelling. CSF leak due to accidental dural injury can occur in the final stages of odontoid resection. When the dura is clearly lacerated a direct repair should be attempted followed by insertion of a lumbar drain for up to 5 postoperative days. Velopharyngeal insufficiency is the result of scarring and fibrosis of the soft palate, and causes hypernasality of the voice, nasal regurgitation and dysphagia [34]. Retraction instead of cutting the soft palate minimizes the occurrence of velopharyngeal dysfunction [4]. Neurological deterioration after transoral decompression occurs in roughly 1% of cases and is though to be the result of direct trauma during the operation or loss of spinal alignment during patient repositioning between anterior decompression and posterior fixation [32]. Careful evaluation of preoperative CT scan is required to avoid injury of the vertebral artery which can occur in case of rotatory subluxation of C1. Pharyngeal wound dehiscence occurs in 3% of cases [4] after TOA. In our experience the single-layer closure of the posterior pharyngeal wall with interrupted absorbable sutures minimizes the occurrence of this complication. When wound dehiscence occurs the pharyngeal wound should be revised under general anesthesia [4, 10, 30]. Although infection has long been considered a serious drawback of TOA, large clinical series reported rates of pharyngeal infection less than 1% [32]. In fact, local resistance of oral tissue to its own bacterial flora facilitates wound healing. The postoperative soft tissue swelling is common after TOA, generally subsides after 24–48 h and its occurrence is minimized by delicate tongue retraction and careful intraoperative handling of soft tissues.
Conclusion
TOA with or without transection of the atlas allows a direct and unobstructed corridor for the effective treatment of most patients with BI and AAD exerting irreducible ventral compression of the cervicomedullary junction. In cases of severe basilar invagination with the offending odontoind peg at the level of the nasopharynx, transmaxillary approaches or, more recently, endoscopic endonasal approaches, should be considered. After an adequate learning curve and following the basic tenets of skull base surgery, the approach related-morbidity in standard TOA is minimal.
References
Chamberlain WE. Basilar impression (platybasia). A bizzarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med. 1939;11:487–96.
Hadley MN, Spetzler RF, Sonntag VKH. The transoral approach to the superior cervical spine. A review of 53 cases of extradural cervicomedulary compression. J Neurosurg. 1989;71:16–23.
Menezes AH, VanGilder JC, Graf CJ, McDonnell DE. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980;53:444–55.
Perrini P, Benedetto N, Guidi E, Di Lorenzo N. Transoral approach and its superior extensions to the craniovertebral junction malformations: surgical strategies and results. Neurosurgery. 2009;64(5 Suppl 2):331–42.
Kanavel AB. Bullet located between the atlas and the base of the skull: technique of removal through the mouth. Surg Clin Chicago. 1917;1:361–6.
Di Lorenzo N, Fortuna A, Guidetti B. Craniovertebral junction malformations. Clinicoradiological findings, long-term results and surgical indications in 63 cases.J. Neurosurgery. 1982;57:603–8.
Di Lorenzo N. Transoral approach to extradural lesions of the lower clivus and upper cervical spine: an experience of 19 cases. Neurosurgery. 1989;24:37–42.
Di Lorenzo N. Craniocervical junction malformation treated by transoral approach. A survey of 25 cases with emphasis on postoperative instability and outcome. Acta Neurochir. 1992;118:112–6.
Perrini P, Benedetto N, Di Lorenzo N. Transoral approach to extradural non-neoplastic lesions of the craniovertebral junction. Acta Neurochir. 2014;156:1231–6.
Perrini P, Benedetto N, Cacciola F, Gallina P, Di Lorenzo N. Refinement of the transoral approach to the craniovertebral junction malformations. Acta Neurochir Suppl. 2019;125:235–40.
Crockard HA, Johnston F. Development of transoral approaches to lesions of the skull base and craniocervical junction. Neurosurg Q. 1993;3(2):61–82.
Dlouhy BJ, Dahdaleh NS, Menezes AH. Evolution of transoral approaches, endoscopic endonasal approaches, and reduction strategies for treatment of craniovertebral junction pathology: a treatment algorithm. Neurosurg Focus. 2015;38(4):E8.
Menezes AH, VanGilder JC. Transoral-transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988;69:895–903.
Menezes AH, Traynelis VC, Gantz BJ. Surgical approaches to the craniovertebral junction. Clin Neurosurg. 1994;41:187–203.
Menezes AH. Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervicxal junction”. Childs Nerv Syst. 2008;24:1187–93.
Menezes AH, Fenoy KA. Remnants of occipital vertebrae: proatlas segmentation abnormalities. Neurosurgery. 2009;64:945–54.
Visocchi M. Transnasal and transoral approach to the clivus and the craniovertebral junction. J Neurosurg Sci. 2019;63(5):498–500.
Sasaki CT, Lowlicht RA, Tokashiki R. Horizontal maxillotomy for exposure of the central skull base: the Yale experience. J Neuro-Oncol. 2001;55:173–7.
James D, Crockard HA. Surgical access to the base of skull and upper cervical spine by extended maxillotomy. Neurosurgery. 1991;29:411–6.
de Almeida JR, Zanation AM, Snyderman CH, Carrau RL, Prevedello DM, Gardner PA, Kassam AB. Defining the nasopalatine line: the limit for endonasal surgery of the spine. Laryngoscope. 2009;119(2):239–44.
El-Sayed IH, Wu JC, Dhillon N, Ames CP, Mummaneni P. The importance of platybasia and the palatine line in patient selection for endonasal surgery of the craniocervical junction: a radiographic study of 12 patients. World Neurosurg. 2011;76(183):188.
Husain M, Rastogi M, Ojha BK, Chandra A, Jha DK. Endoscopic transoral surgery for craniovertebral junction anomalies. Technical note. J Neurosurg Spine. 2006;5:367–73.
Lindley T, Greenlee JD, Teo C. Minimally invasive surgery (endonasal) for anterior fossa and sellar tumors. Neurosurg Clin N Am. 2010;21:607–20.
Fenoy AJ, Menezes AH, Fenoy KA. Craniovertebral junction fusions in patients with hindbrain herniation and syringohydromyelia. J Neurosurg Spine. 2008;9:1–9.
Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88:962–8.
Goel A, Desai K. Surgery for syringomyelia: an analysis based on 163 surgical cases. Acta Neurochir. 2000;142:293–302.
Menezes AH. Craniovertebral junction abnormalities with hindbrain herniation and syringomyelia: regression of syringomyelia after removal of ventral craniovertebral junction compression. J Neurosurg. 2012;116(2):301–9.
Dickman CA, Locantro J, Fessler RG. The influence of odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992;77:525–30.
Naderi S, Crawford NR, Melton MS, Sonntag VK, Dickman CA. Biomechanical analysis of cranial settling after transoral odontoidectomy. Neurosurg Focus. 1999;6(6):Article 7.
Tuite GF, Veres R, Crockard HA, Sell D. Pediatric transoral surgery: indications, complications and long-term outcome. J Neurosurg. 1996;84(4):573–83.
Balasingam V, Anderson GJ, Gross ND, Cheng CM, Noguchi A, Dogan A, McMenomey SO, Delashaw JB Jr, Andersen PE. Anatomical analysis of transoral surgical approaches to the clivus. J Neurosurg. 2006;105:301–8.
Choi D, Crockard HA. Evolution of transoral surgery: three decades of change in patients, pathologies, and indications. Neurosurgery. 2013;73:296–304.
Naderi S, Pamir MN. Further cranial settling of the upper cervical spine following odontoidectomy. Report of two cases. J Neurosurg. 2001;95(2 Suppl):246–9.
Jones DC, Hayter JP, Vaughan ED, Findlay GF. Oropharyngeal morbidity following transoral approaches to the upper cervical spine. Int J Oral Maxillofac Surg. 1998;27:295–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Perrini, P., Benedetto, N., Di Lorenzo, N. (2022). Basilar Invagination and Atlanto-Axial Dislocation. In: Menchetti, P.P.M. (eds) Cervical Spine. Springer, Cham. https://doi.org/10.1007/978-3-030-94829-0_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-94829-0_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94828-3
Online ISBN: 978-3-030-94829-0
eBook Packages: MedicineMedicine (R0)