Abstract
Purpose
Recently, it has been demonstrated that anterior release of tight structures via a transoral approach can assist posterior distraction–reduction technique in restoring the cranio-cervical anatomy in irreducible atlantoaxial dislocations. Our aim was to evaluate the radiological and clinical outcome of anterior release and posterior instrumentation for irreducible congenital basilar invagination.
Methods
A consecutive series of 15 patients (2007–2009) with irreducible congenital basilar invagination were treated with anterior release using transoral approach. A retrospective chart review was performed. All patients presented with myelopathy. Dislocation was treated as irreducible if acceptable reduction was not achieved with traction under general anesthesia and neuromuscular paralysis. The anterior release comprised of transverse sectioning the longus colli and capitis, C1–C2 joint capsular release and intra-articular adhesiolysis with or without anterior C1 arch excision. Cantilever mechanism using posterior instrumentation was used to correct any residual malalignment.
Results
Mean age was 21.4 (10–50) years. Average duration of follow-up was 28 (24–40) months. The average preoperative JOA score was 11.4 (8–16), which improved to 15.4 (10–18) after surgery. Anatomical reduction was achieved in thirteen patients. Fusion was documented in all patients. Complications included persistent nasal phonation in one, and superficial wound dehiscence in one.
Conclusion
We believe that a significant number of irreducible dislocations can be anatomically reduced with this procedure thus avoiding odontoid excision. Encouraging results from this short series have given us a new perspective in dealing with these challenging problems.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There are two ways to achieve neural decompression in a patient with atlantoaxial dislocation. Either anatomically realign the craniovertebral junction (CVJ) or excise the offending anatomical structure. The latter option, e.g. odontoidectomy, has been confined to irreducible craniovertebral dislocations including basilar invagination [1]. Although advances in microsurgical techniques have improved outcomes of transoral odontoidectomy, it still remains a formidable procedure in irreducible basilar invagination [2]. Elevated craniovertebral junction and increased depth of operative field make resection of apex of deformity a challenge, frequently requiring extended approaches [3]. Iatrogenic dural tear during transoral resection has the potential to lead to meningitis. Moreover, patients with torticollis may have poor cosmetic outcome, as facetal realignment is not addressed [4].
Recently, there has been a paradigm shift in the approach to such irreducible dislocations. The authors have questioned the concept of irreducibility, stating that it is possible surgically to reduce apparently “irreducible” dislocations by facetal manipulation and release [4, 5]. Wang et al. [4] have proposed an anterior transoral approach for facetal release and reduction. The release of anteriorly bow-strung ligamentous structures in the concavity of the craniovertebral kyphosis allows re-positioning of the atlantoaxial complex. We present consecutive series of fifteen patients with irreducible congenital basilar invagination treated by the Wang’s procedure of transoral anterior release and posterior instrumentation. The odontoid was preserved in all cases.
Materials and methods
Retrospective analysis of fifteen consecutive patients, treated by a single surgeon between 2007 and 2010 at a single tertiary-care referral hospital is presented. An Institutional Review Board (IRB) approval was obtained to review the medical records.
Basilar invagination has been classified into two types by Goel et al. [2]. Type A basilar invagination has atlantoaxial dislocation with the tip of odontoid invaginating into the foramen magnum, and it is above the Chamberlain line, McRae line and Wackenheim line. In Type B basilar invagination, the entire craniovertebral complex is rostrally located with the tip of odontoid above Chamberlain line, but below McRae line and Wackenheim line. There is no atlantoaxial dislocation in Type B basilar invagination. Irreducible Type A basilar invaginations (tip of odontoid 7 mm or more above the McGregor line on sagittally reconstructed CT scan) were included in the study. Irreducibility was defined by the persistence of odontoid tip above the Wackenheim’s line on traction under general anesthesia and muscle paralysis. Type B basilar invaginations and atlantoaxial dislocations without basilar invagination were excluded.
Study group
Records were obtained from a prospectively maintained database. All fifteen patients presented with varying grades of motor myelopathy (Table 1). In one patient, the myelopathy was precipitated by trauma (Case 3). Neurological deficit was measured using the modified Japanese Orthopedic Association Score (JOA) [6]. The average duration of symptoms before surgery was 4.8 (1–12) months.
Radiographic evaluation
Radiographs (open-mouth, dynamic lateral views) were obtained. MRI and CT scan with vertebral artery angiogram were obtained in all patients. Angiogram was particularly useful to identify the course of the vertebral artery. The cervicomedullary angle was measured on T1-weighted sagittal MRI image [7]. Extent of ventral cord compression measured as the perpendicular distance (pB-C2) of the odontoid tip from the line joining the basion and the inferior–posterior aspect of C2 body [8]. The relationship of the tip of odontoid with respect to the Wackenheim’s line (line drawn along the posterior border of clivus) [9] was noted. Perpendicular distance of the tip of odontoid from the McGregor line was measured [9]. Aim of the reduction was to restore CMA to more than 135 degrees without any residual ventral or dorsal compression on the spinal cord (pB-C2 <9 mm) with the odontoid tip below the McGregor and Wackenheim’s line.
Surgical technique
Reduction, as assessed on lateral radiograph, was attempted using preoperative Gardner Wells cervical traction up to 5 kg for 2 days. Intravenous broad-spectrum antibiotics were administered half an hour prior to incision. Nasotracheal intubation and nasogastric tube were used in all.
Traction, under anesthesia and complete neuromuscular paralysis, was increased up to a maximum of one-sixth of the body weight and irreducibility confirmed with intraoperative radiographs after 10 min.
Anterior release
The neck was positioned in hyperextension under cervical traction. A transnasal catheter sutured to the uvula was used to retract the soft palate. Crockard transoral retractor system provided a standard transoral exposure.
The longus colli, longus capitis muscles and the anterior longitudinal ligament were transversely divided along the inferior border of the C1 arch (Fig. 1a–d). The anterior capsule of the atlantoaxial joint was incised. A 5-mm periosteal elevator was used to distract the atlantoaxial joint taking care to remain within the lateral edge. (Figs. 1e, 2c–d). This released any intra-articular adhesions. In most cases, this maneuver allowed significant vertical downward migration of the odontoid. Assimilated anterior C1 arch was excised to expose the odontoid tip. This allowed the anterior displacement of the odontoid when the atlantoaxial joint was reduced with posterior instrumentation (Fig. 1d–f). The fibrous tissue anterior and lateral to the odontoid process was excised. The anteroinferior edge of the dislocated C1 lateral mass was burred down only if it overlapped the C2 facet (Fig. 1c). The apical, alar or transverse ligaments were left undisturbed. Decision not to proceed with odontoidectomy was taken if the release procedure was successful in bringing down the odontoid, as assessed on the lateral intraoperative radiograph. Anterior bone grafting was not performed. Meticulous hemostasis and mucosal closure were achieved. The patient was then carefully turned prone. This was achieved by keeping the neck immobilized in a rigid collar while maintaining cervical traction.
Diagrammatic representation of sequential correction of irreducible basilar invagination. a, c, e Parasagittal views through the atlantoaxial joints. Oc occiput, C1–C1 lateral mass fused with occipital condyle, C2–C2 pars with superior facet of axis, LoC longus capitis, Cap atlantoaxial joint capsule. b, d, f Midsagittal views of the CVJ. Note the excision of the anterior–inferior margin of the C1 lateral mass (c arrow head) and the excision of the anterior C1 arch (d starred)
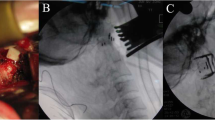
Case 6 lateral cervical spine radiograph without traction (a) and with skeletal traction under anesthesia and muscle paralysis (b). Reduction is unacceptable on traction as the tip of odontoid is above the Wackenheim’s line (W) and McGregor line (McG). Intraoperative transoral distraction of atlantoaxial joints using a small periosteal elevator as shown in c and d. Excision of anterior C1 arch so that the tip of odontoid moves into position under the basion (e). f Posterior instrumentation and stabilization
Posterior surgery
Under traction, the vertical translocation of the dens corrected to a significant degree. Subperiosteal exposure of the CVJ was performed. The posterior capsule of the atlantoaxial joint was excised and the joint distracted. 3.5-mm diameter polyaxial C2 pedicle screws were inserted. C3 lateral mass screw was additionally used in most cases. The occipital plate was undercontoured such that when locked into the screws, its occipital portion would remain slightly elevated from the occipital bone (Fig. 1d). Cantilever force was then applied to approximate the plate to the occiput (Fig. 1f). This maneuver allowed correction of posterior angulation of the odontoid thereby achieving reduction. Bicortical occipital screws were inserted in the occipital bone. Foramen magnum decompression was also performed in cases with associated Chiari malformation and where in the space available for cord was judged inadequate. Morselized iliac crest graft was placed into the atlantoaxial joints and over the decorticated posterior elements. The wound was closed in layers over a subfascial drain. Figure 2 shows the sequence of intraoperative correction in Case 6.
Aftercare
Bedside mobilization was started on the second or third postoperative day. Nasogastric feeding was commenced on return of peristalsis. Oral feeding was resumed after the pharyngeal wound healed after 7th postoperative day. Patients were discharged 2 weeks post surgery after suture removal.
Follow-up
The patients were examined 1.5, 3, 6, and 12 monthly and yearly thereafter. Dynamic flexion–extension radiographs of the cervical spine were obtained. Postoperative MRI scan was available in twelve patients. Three patients with stainless steel implants had a CT myelogram. All patients had CT scan at 12 months to assess fusion. Fusion was deemed complete if bridging bone was visible across C1–C2 and O–C1 segments on reconstructed postoperative CT scans.
Results
The congenital malformations noted were: C1 assimilation in fourteen, condylar hypoplasia in ten, C2–3 fusions in eight, C2–C4 fusion in one, Klippel–Feil syndrome in three, Chiari malformation in two, malformed odontoid in 2, and incomplete ring of C1 in one. None had preexisting fusion of C1–C2 joints. Clinico-radiological and surgical findings are presented in Table 1.
Surgical
All patients underwent anterior transoral release and posterior instrumented reduction and fusion. In all patients, the longus colli, longus capitis, anterior longitudinal ligament, C1–C2 anterior capsule and intra-articular adhesions were released. Anterior C1 arch was excised in 12 patients. Posterior instrumentation was performed from occiput to C3 in thirteen, occiput to C2 in one, and occiput to C4 in one. Stainless steel implants were used in first three patients of the series (case 1–3). Foramen magnum decompression was performed in 5 patients, two of whom had Chiari malformation.
The average surgical time required for the transoral procedure and posterior fusion was 75.6 min (SD 23.1 min) and 180 min (SD 39.3 min), respectively, while the average estimated blood loss was 142.7 ml (SD 43.9 ml) and 374.7 ml (SD 135.4 ml), respectively. The average length of stay in the hospital was 21.1 days (18–30 days).
Clinical
Average follow-up following surgery was 28 (24–40) months. All patients improved neurologically. The average preoperative JOA score was 11.5 (SD 2.6), which improved to 15.4 (SD 1.9) after surgery (P < 0.0001). None of the patients had neurological deterioration after surgery. Torticollis corrected in all three patients who presented with head tilt. In all patients, tube feeding was discontinued once pharyngeal wound had healed.
Radiological
The preoperative and postoperative cranio-cervical measurements are enumerated in Table 2. Postoperatively the tip of the odontoid was reduced below the Wackenheim’s line. The average preoperative cervicomedullary angle (CMA) was 110 ° (SD 11.4), which corrected to 146 ° (SD 6.8) after surgery. The average pB-C2 measurement was 16.9 mm (SD 3.9), which corrected to 3.9 mm (SD 3.2) after surgery. Both these improvements were statistically significant (Table 2). Anatomical reduction (CMA >135 °, pB-C2 <9 mm and tip of odontoid beneath the basion) was achieved in 13 patients.
In 2 patients (Case 1 and 2), in spite of achieving correction of basilar invagination and CMA correcting to more than 135 °, pB-C2 measurement remained high. This resulted in focal cord compression by the odontoid tip. Both patients did not consent for a second stage transoral odontoidectomy. Thus, odontoidectomy was not performed in any patient during the study period. Posterior fusion was documented on CT scans in all patients. In five patients, solid fusion was demonstrated between the clivus and the odontoid process (Figs. 3, 4).
Two complications were noted. One patient had persistent nasal phonation without regurgitation of food. ENT assessment suggested that this was due to scarring in the soft palate probably secondary to excessive intraoperative traction. One patient had superficial posterior wound dehiscence. No patient had dysphagia requiring prolonged tube feeding.
Discussion
Congenital basilar invagination typically results in cranio-cervical kyphosis that causes ventral brain stem compression. Vertical translocation and posterior angulation of odontoid contribute to the kyphosis. Grabb et al. [8] proposed the pB-C2 measurement, which is an objective measure of ventral brain stem compression. They found that greater degrees of posterior angulation and height of odontoid correlated with persistent cord compression (pB-C2 >9 mm), even in the absence of basilar invagination. Furthermore, skulls with assimilated atlas have 15–35 % smaller foramen magnum dimensions than normal skulls [10]. Thus, in patients with residual posterior angulation the odontoid acts as a space occupying entity in a narrowed foramen magnum outlet. On the basis of these studies, we believe that in addition to correction of vertical translocation, posterior angulation of the odontoid should also be addressed when attempting an anatomical realignment procedure.
While transoral odontoidectomy has been the recommended treatment for irreducible dislocations, Goel et al. [11] proposed an alternative and suggested that “irreducible” or “fixed” dislocations can be reduced by distraction of the facet joints via the posterior approach. Several authors have employed this concept of distraction–reduction for basilar invagination [12–14]. However, ability of these methods to achieve anatomical reduction in severe rigid cases has been questioned by some authors [15].
As with any deformity, the primary tether is located in the concavity of the kyphosis. Longus colli, longus capitis, anterior longitudinal ligament and capsule of atlantoaxial joint are contracted and tight [4]. Assimilated C1 arch is another obstacle to reduction, especially of posterior angulation of odontoid. The normal anatomic location of the odontoid tip lies just caudad to the basion. In patients with atlas assimilation, the fused anterior C1 arch frequently occupies this location preventing adequate anterior translation of the odontoid tip (Fig. 4b). Infrequently, the odontoid tip is malformed and anteverted, possibly due to traction of the apical ligament (Fig. 3a) blocking correction of posterior angulation. These obstacles to reduction cannot be adequately addressed via the posterior approach distraction–reduction techniques.
In 2006, Wang et al. [4] proposed a novel method for treating irreducible craniovertebral dislocations. They achieved anatomical reduction by releasing the above-mentioned tethers via transoral approach followed by further correction by utilizing special posterior instrumentation. Although described by Wang et al., we believe that the release of transverse, apical and alar ligament is not necessary. Considering their anatomic location with respect to the displacement, these ligaments are likely to be stretched and redundant rather than contracted (Fig. 1b). Also, without an odontoidectomy, release of alar and transverse ligaments is technically difficult without risking damage to dura or cord. Another difference from the Wang’s procedure is the step in which the anterior–inferior border of the C1 lateral mass is drilled off to allow for the C2 superior facet to move beneath the C1 lateral mass. We also avoid a routine tracheostomy after a transoral release, as it is a relatively short procedure.
Anatomical realignment of cranio-cervical anatomy, in addition to complete neural decompression, also leads to correction of torticollis if any. An unexpected advantage of excising the assimilated anterior C1 arch—also noted by Wang et al. [16]—was the frequent spontaneous fusion of the odontoid tip with the basion providing a solid anterior column support (Figs. 3, 4). Early in our series (in the first two cases) we did not excise the anterior C1 arch. These two cases had suboptimal reductions (Table 2) and we retrospectively concluded that the reduction was blocked by the assimilated C1 arch. In later cases, we routinely excised the C1 arch to allow the tip of odontoid to move more ventrally.
An argument can be made that once reduction has been achieved via a transoral approach, leaving behind the odontoid can cause potential cord injury during positioning and posterior reduction maneuver [17]. We believe that the risk involved in transoral odontoidectomy, even after reduction, is greater that the risk posed by the odontoid during positioning or reduction maneuvers. However, we acknowledge that an anterior release creates significant instability and utmost care should be taken during prone positioning as the residual odontoid peg can compromise the spinal cord. Hence we would recommend this surgery to be done at specialized centers by surgeons who are well-versed with treating craniovertebral pathologies. Electrophysiological monitoring may be helpful, especially during prone positioning and during posterior reduction procedure. Unfortunately, due to economic reasons we have not been able to employ this in our hospital as of yet.
Presently, our protocol for treating irreducible dislocations including congenital basilar invagination is the following. The decision to address the irreducible deformity with either transoral release or transoral odontoidectomy is similar and this decision is based on traction X-rays under anesthesia and complete neuromuscular paralysis. We always perform transoral release to assess reducibility before attempting odontoidectomy. If adequate reduction cannot be achieved, then the surgery can proceed to an odontoid resection. Excluding the first two cases in our series, we have yet to encounter a situation where we were not able to reduce the deformity adequately.
A limitation of our study is the small sample size and the absence of a control group. Hence direct comparisons with transoral odontoidectomy and the posterior distraction–reduction technique are not possible. However, we believe that an anterior release and posterior instrumented reduction is viable and probably a safer alternative to transoral odontoidectomy. Also, this procedure has the potential to deliver better deformity correction compared to posterior distraction–reduction techniques. Future comparative studies with traditional methods may provide a useful insight into the generalizability of this procedure.
In conclusion, a significant number of irreducible dislocations can be anatomically reduced with this procedure. Anatomical deformity correction may allow better subaxial cervical alignment and correction of torticollis (Fig. 5). However, anterior release creates significant instability and utmost care should be taken during prone positioning for posterior surgery. Encouraging results from our short series of patients have given us a new perspective in dealing with these challenging craniovertebral pathologies.
Case 7 preoperative (a, c, e, g) and postoperative (b, d, f, h) CT reconstruction images. a pB-C2 Measurement as described. b Midsagittal CT demonstrating correction of basilar invagination. d, f Left and right parasagittal CT reconstruction showing realignment of C1–C2 joint after surgery, respectively. h Coronal reconstruction showing correction of the torticollis due to unequal distraction of the facet joints
Abbreviations
- CVJ:
-
Cranio vertebral junction
- JOA:
-
Japanese Orthopedic Association
- pBC2:
-
Distance of the odontoid tip from the line joining the basion and the posteroinferior corner of C2
References
Menezes AH, VanGilder JC, Graf CJ, McDonnell DE (1980) Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg 53:444–455. doi:10.3171/jns.1980.53.4.0444
Mouchaty H, Perrini P, Conti R, Di Lorenzo N (2009) Craniovertebral junction lesions: our experience with the transoral surgical approach. Eur Spine J 18:13–19. doi:10.1007/s00586-009-0988-7
Perrini P, Benedetto N, Guidi E, Di Lorenzo N (2009) Transoral approach and its superior extensions to the craniovertebral junction malformations: surgical strategies and results. Neurosurgery 64:331–342. doi:10.1227/01.NEU.0000334430.25626.DC (discussion 342)
Wang C, Yan M, Zhou HT et al (2006) Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine 31:E306–E313. doi:10.1097/01.brs.0000217686.80327.e4
Goel A (2004) Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 1:281–286. doi:10.3171/spi.2004.1.3.0281
Benzel EC, Lancon J, Kesterson L, Hadden T (1991) Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord 4:286–295
Wang S, Wang C, Passias PG et al (2009) Interobserver and intraobserver reliability of the cervicomedullary angle in a normal adult population. Eur Spine J 18:1349–1354. doi:10.1007/s00586-009-1112-8
Grabb PA, Mapstone TB, Oakes WJ (1999) Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery 44:520–527 (discussion 527–8)
Smoker WR (1994) Craniovertebral junction: normal anatomy, craniometry, and congenital anomalies. Radiographics 14:255–277
Tubbs RS, Lancaster JR, Mortazavi MM et al (2011) Morphometry of the outlet of the foramen magnum in crania with atlantooccipital fusion. J Neurosurg Spine 15:55–59. doi:10.3171/2011.3.SPINE10828
Goel A, Kulkarni AG, Sharma P (2005) Reduction of fixed atlantoaxial dislocation in 24 cases: technical note. J Neurosurg Spine 2:505–509. doi:10.3171/spi.2005.2.4.0505
Jian F-Z, Chen Z, Wrede KH et al (2010) Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery 66:678–687. doi:10.1227/01.NEU.0000367632.45384.5A (discussion 687)
Hsu W, Zaidi HA, Suk I et al (2010) A new technique for intraoperative reduction of occipitocervical instability. Neurosurgery 66:ons319–ons324. doi:10.1227/01.NEU.0000369925.81522.60
Yoshizumi T, Murata H, Ikenishi Y et al (2014) Occipitocervical fusion with relief of odontoid invagination: atlantoaxial distraction method using cylindrical titanium cage for basilar invagination—case report. Neurosurg Rev. doi:10.1007/s10143-014-0531-0
Smith JS, Shaffrey C, Abel MF, Menezes AH (2010) Basilar invagination. Neurosurgery 66:39–47. doi:10.1227/01.NEU.0000365770.10690.6F
Wang S, Wang C (2010) Response to the expert’s comment of P. Suchomel concerning grand rounds case entitled “Syringomyelia with irreducible atlantoaxial dislocation, basilar invagination and Chiari I malformation”, Eur Spine J, 19(3), 2010, pp. 367–369 (by Shenglin Wang et al.). Eur Spine J. doi:10.1007/s00586-010-1397-7
Suchomel P (2010) Expert’s comment concerning Grand Rounds case entitled “Syringomyelia with irreducible atlantoaxial dislocation, basilar invagination and Chiari I malformation” (by Shenglin Wang, Chao Wang, Ming Yan, Haitao Zhou, Liang Jiang). Eur Spine J 19:367–369. doi:10.1007/s00586-009-1209-0
Conflict of interest
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. Approval by the authors’ institutional review board (IRB) was obtained.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laheri, V., Chaudhary, K., Rathod, A. et al. Anterior transoral atlantoaxial release and posterior instrumented fusion for irreducible congenital basilar invagination. Eur Spine J 24, 2977–2985 (2015). https://doi.org/10.1007/s00586-015-3836-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3836-y