Abstract
After completing the maneuver of insertion, the securement of the catheter and protection of the exit site are of paramount importance for the optimal performance of the venous access device (VAD) and for the minimization of complications such as infection, catheter dislodgment and venous thrombosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
After completing the maneuver of insertion, the securement of the catheter and protection of the exit site are of paramount importance for the optimal performance of the venous access device (VAD) and for the minimization of complications such as infection, catheter dislodgment and venous thrombosis.
The exit site of the catheter is a relevant route of bacterial contamination (so called ‘extra-luminal’ route), and the prevention of infection is based on the proper choice of the exit site and its appropriate protection. Both for peripheral and central VADs, an exit site placed in a skin area of relevant bacterial contamination will increase the risk of infection. Skin contamination by bacteria and fungi is particularly high in skin areas that are humid, hairy, or close to natural or artificial connections with the digestive tract (mouth, anus, gastrostomy, enterostomy, etc.) or with the respiratory tract (nose, mouth, tracheostomy, etc.) or with any other skin breech (surgical drains, thoracostomy, nephrostomy, etc.). Examples of central VADs at high risk for infection are CICCs with the exit site at the neck or close to a tracheostomy, or FICCs inserted in the common femoral vein and coming out of the inguinal groove, or PICCs with the exit site to close to the axilla. Also, regardless of its location, the exit site should be appropriately protected by using one or more of the following strategies: tunneling, glue, proper securement devices, and semipermeable transparent membranes.
For both peripheral and central VADs, the choice of the exit site is very important also for the prevention of dislodgment. An exit site placed in a very unstable area such as the neck or the groin will be associated with a high risk of catheter dislodgment. Though, the choice of a skin area with minimal movements and maximal stability (for example: the infraclavicular region, mid-arm, mid-thigh, etc.) will not be enough for preventing dislodgment. Additional strategies should be added, such as proper securement device (skin-adhesive sutureless device or subcutaneous anchorage), cyanoacrylate glue, and semipermeable transparent membranes.
Finally, proper securement of the catheter has also a major role in preventing venous thrombosis. Catheter-related thrombosis is a phenomenon caused by the catheter insertion itself (damage of the vein wall integrity), by the permanence of the catheter inside the vein (obstacle to the blood flow), and by the possible endothelial irritation due to the infused solutions. Though, another major cause of catheter-related thrombosis is the friction of the catheter on the vein wall caused by the instability of the device. This occurs frequently both as ‘mechanical thrombophlebitis’ for peripheral short cannulas and as major venous thrombosis for central VADs, particularly for catheters with the exit site in the groin area or at the neck. Many clinical studies have shown that an optimal securement of the catheter is associated with a reduction of the risk of venous thrombosis.
In this chapter we will discuss different techniques and devices that may directly or indirectly enhance catheter securement and/or protection of the exit site, with a resulting favorable impact on the risk of infection, dislodgment, and thrombosis.
1 Protocols for Choosing the Exit Site
Different protocols have been described for the proper choice of the exit site of a VAD. These protocols take into considerations the different aspects discussed above: the contamination of the skin, its humidity, the stability of the region, and so on.
The first protocol of this kind was described by Dawson in 2013, as a guide for the proper choice of the exit site of a PICC (i.e., an ultrasound guided central VAD inserted in the deep veins of the arm): the so-called ‘ZIM’ (Zone Insertion Method). The ZIM has become rapidly popular for all PICC insertions, both in children and in adults. The basic concept of Dawson’s ZIM is that the ideal area for the exit site at the arm is the middle third of the arm (‘green’ zone): catheters coming out of the skin in the distal third (‘red’ zone), close to the antecubital fossa, will be too unstable, while an exit site in the proximal third (‘yellow’ zone), close to the axilla, will be easily contaminated by the local bacterial flora. In short, when the only reasonable puncture site is located in the yellow zone (for instance, because of the caliber of the veins), any effort should be done for obtaining an exit site in the green zone, tunneling the catheter. Interestingly, the ZIM method is useful in clinical practice both for defining when tunneling is needed (i.e., when the ideal puncture site is in the yellow zone and not in the green zone) and for estimating how long the tunnel must be (i.e., long enough to obtain the exit site in the green area).
In recent papers, similar Zone Insertion Methods have been described also for CICCs and FICCS.
The so-called Central ZIM divides the neck/chest area in three zones: the red zone corresponds to the neck, the yellow zone to the supraclavicular region, and the green zone to the infraclavicular region. The red zone is an area of high skin contamination (due to the bacteria coming from the mouth and the nose) and high instability; non-tunneled CICC inserted in this area are prone to infection, dislodgment, and venous thrombosis. The yellow zone is the area where central venipuncture is often performed: ultrasound-guided access to the internal jugular vein (IJV), brachio-cephalic vein (BCV), subclavian vein (SBV) and external jugular vein (EJV) is commonly performed with the puncture site in this area. The yellow zone may be also acceptable as exit site in many patients, for example in older children without tracheostomy. On the other hand, in neonates and in infants (and in any patient with tracheostomy), an exit site in the yellow zone is not appropriate, and the catheter should be tunneled so to obtain an exit site in the green zone. Finally, the green zone is an ideal area both as puncture site and as exit site.
The so-called Femoral ZIM divides the groin/thigh area in three zones. The red zone corresponds to the area close to the knee, quite unstable and not recommended as exit site (this is also an area where venipuncture is quite difficult, as the superficial femoral vein is too deep). The yellow zone is the groin area and the upper third of the thigh; while venipuncture is almost always quite easy in this area, since the common femoral vein is quite large and easy to access (with the possible exceptions of very small premature neonates and very obese children), the exit site is not ideal since it is an unstable and highly contaminated area (inguinal groove, close to the urinary tract and to the perineum). FICCs with exit site at the groin are acceptable for limited period; if a FICC is planned to stay in place for more than 48 h and the only option is the venipuncture in the yellow zone, the catheter should be tunneled to the green zone (mid-thigh). Direct access to the superficial femoral vein at mid-thigh would represent probably the ideal solution, as the exit site is in a clean and stable area, with no tunneling required, but this venous access is feasible only in older children, as in neonates and infants the superficial femoral vein is too small.
Very recently, the ‘ZIM’ has been proposed also for the insertion of peripheral VADs in the upper limb. Different versions have been proposed, usually considering ‘green’ zones that corresponds to an ideal exit site (the forearm; the area above the antecubital fossa), ‘yellow’ zones where the exit site is not ideal but acceptable for cannulas inserted in emergency and expected to stay in place for less than 24 h (the dorsal side of the hand and of the wrist; the antecubital fossa), and ‘red’ zones where the insertion of a short peripheral cannula is consistently discouraged (the ventral side of the wrist).
2 Tunneling
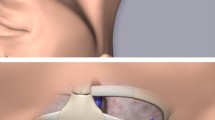
Tunneling is a powerful technical tool for obtaining the ‘ideal’ exit site independently from the choice of the puncture site. The most typical example is the insertion of ultrasound guided CICCs in neonates, where the brachio-cephalic vein (BCV) represents the safest and easiest access to the central veins; though, the puncture site of ultrasound-guided access to the BCV is located in the supraclavicular area, which is a rather unstable area for the exit site; therefore, in this situation it is mandatory to tunnel the catheter so to move the exit site far from the puncture site, to a stable and clean skin area (typically, to the infraclavicular region) (Fig. 8.1).

Fig. 8.3
Catheter tunneling is a simple and safe maneuver that can be applied to any central VAD (CICC, PICC or FICC), as long as the catheter is inserted using the modified Seldinger technique (needle venipuncture—guidewire through needle—introducer over guidewire—catheter through introducer). Though theoretically possible, the tunneling maneuver has never been described for ECC.
A recently published protocol, so-called RAVESTO (Rapid Assessment of Venous Exit Site and Tunneling Options) lists and describes all the possible options for tunneling PICCs, CICCs, and FICCs.
PICC tunneling (Figs. 8.2 and 8.3) is indicated whenever the best puncture site appears to be in the yellow zone. Tunneling has dramatically increased the feasibility of PICC insertion in children, considering that the availability of a vein of proper caliber is the main limitation to PICCs in this age group. Current PICCs (i.e., peripherally inserted central catheters inserted in the deep veins of the arm adopting ultrasound guidance and modified Seldinger technique) should be in polyurethane and power injectable; as such, they are available of no less than 3Fr of caliber (i.e., 1 mm). Considering that the inner diameter of the vein should be at least three times the external diameter of the catheter, the smallest acceptable vein for PICC insertion must have a diameter of 3 mm. Veins of this caliber are rare in the green zone of the arm of small children, but they may be present in the yellow zone; in these cases, the vein is punctured in the yellow zone but the catheter is subsequently tunneled so to obtain an exit site in the green zone. The technique of PICC tunnelling is described in Figs. 8.4, 8.5, and 8.6.
Several options of CICC tunneling are described in the RAVESTO protocol: (a) CICC with puncture site in the supraclavicular area but tunneled downward, so to obtain an exit site in the infraclavicular area (typically in neonates and infants after access to the BCV, but also in critically ill children with tracheostomy) (Figs. 8.7, 8.8, and 8.9); (b) CICC with puncture site in the infraclavicular area but tunneled downward so to obtain an exit site in the lower chest area (this may be used in children, after access to the axillary vein, if a cuffed catheter is indicated: see below) (Fig. 8.10); (c) CICC with puncture site in the supra/infraclavicular area but tunneled to the arm (so-called ‘chest-to-arm’ tunneling) so to have an exit site similar to a PICC (this strategy is adopted when an exit site at the arm is preferred but the insertion of a PICC is unfeasible); (d) CICC with puncture site in the supra/infraclavicular area but tunneled to the back, so to obtain an exit site in the scapular region (this ‘back tunneling’ has been used in non-collaborative children at high risk for pulling out the catheter, since the catheter exit site is out of reach, but also in critically neonates and children who must stay pronated most of the day) (Fig. 8.11). The technique of CICC tunnelling is described in Figs. 8.12, 8.13, and 8.14.

Fig. 8.8

Fig. 8.9
The typical indication for tunneling a FICC is when the puncture site is at the groin (access to the common femoral vein) and the planned exit site is at mid-thigh. In short, an exit site at mid-thigh can be achieved either by direct puncture of the superficial femoral vein at mid-thigh or by puncture of the common femoral vein at the groin, with subsequent tunneling to the mid-thigh area. In both cases, the catheter will be relatively protected by the risk of complications (infection, dislodgment, thrombosis). The technique of FICC tunnelling is described in Figs. 8.15 and 8.16.
Different techniques of tunnelling are available. In most cases, it is recommended to use metallic tunnelers. The tip of the catheter is connected to one end of the tunneler and the tunnel is made passing the device into the subcutaneous tissue.
A short tunneling can be achieved using a short peripheral cannula (Fig. 8.17). The needle-cannula is passed in the subcutaneous tissue from the puncture site to the planned exit site; the needle is removed, and the catheter is passed inside the cannula. A 4-5Fr catheter can be threaded through a 14G cannula, while a 3Fr catheter can adapt to a 16G cannula. The main disadvantages of this technique are (a) that the needle is sharp (and not blunt as most metallic tunnelers) so that it may cause subcutaneous bleeding, and (b) that the tunnel cannot be longer than 3–4 cm.
‘Pseudo-tunneling’ refers to the technique of extended subcutaneous route, i.e., a long trajectory of the needle in the subcutaneous tissue from the skin to the vein; this is not a real tunnel, since the puncture site and the exit site coincide.
3 Catheter securement
Since a decade, sutures have been recognized as an inappropriate and dangerous method for securing external catheters. The stitches that secure the wing to the skin are inevitably associated with multiple chronic infective granulomas, with overgrowth of germs in the proximity of the exit site, increasing the risk of bacterial contamination by the extra-luminal route. All current guidelines recommend avoiding stitches as method of securement and adopt sutureless methods such as (a) skin-adhesive sutureless devices that keep the wing attached to the skin; (b) semipermeable transparent dressing with integrated securement; (c) subcutaneous anchorage systems (SAS).
Skin-adhesive sutureless systems (Figs. 8.18 and 8.19) and transparent dressing with integrated securement have the advantage of being relatively inexpensive and easy to apply, but the disadvantage of requiring a weekly replacement. Also, during the replacement maneuver, there is some risk of accidental catheter dislodgment.
Subcutaneously anchorage (SAS) (Figs. 8.20 and 8.21) is probably the most effective strategy currently available for catheter securement. SAS must be applied at the time of insertion and stays in place as long as the catheter is in place, as no routine replacement is required. Though SAS are more expensive than the other securement devices, they are surely cost-effective (a) when the VAD is expected to stay in place for more than 5 weeks, and (b) when the risk of accidental dislodgment is estimated to be high. Recent clinical studies have demonstrated the high effectiveness of SAS in preventing dislodgment in neonates and children, as well as their safety. The main limitation of SAS is that they are not available for catheter smaller than 3Fr or bigger than 12Fr: this implies that they cannot be used for ECC in neonates or for peripheral VADs, except for midline catheters. In all other central VADs (PICCs, CICCs, FICCs) in infants and children, the adoption of SAS is certainly beneficial and cost-effective and should be recommended. Figure 8.22 shows the technique of SAS placement. Though not specifically recommended by the manufacturers, many centers place a sterile gauze under the SAS, so to avoid pressure damage to the skin (Fig. 8.23).
4 Cuffed catheters
The only other strategy that allows a definitive securement of an external central VAD as effective as the SAS is the use of tunneled-cuffed catheters. As opposed to uncuffed catheters, which can be either tunneled or non-tunneled (depending on the clinical situation), cuffed catheters are supposed to be always tunneled: the cuffed tract of the catheter is placed inside the tunnel, so that the cuff can progressively anchor the catheter to the subcutaneous tissue, by the slowly development of a sterile chronic inflammatory reaction. Recent studies have discussed the benefits of cuffed-tunneled catheters compared to uncuffed tunneled catheters secured with SAS. In both cases, tunneling has a proven role in reducing the risk of bacterial contamination by the extraluminal route, but - as regards securement - SAS may have some advantage over cuffs: (a) it is immediately effective as securement (while the cuff requires a few weeks before the chronic inflammation secures the catheter); (b) the cost of a cuffed catheter is superior to the cost of an uncuffed catheter + SAS; (c) the incidence of cuff-related complications (infection, dislodgment, etc.) seems to be higher than the incidence of SAS-related complications; (d) cuff-related complications always imply the removal of the VAD, while SAS-related complications do not; (e) removal of a cuffed catheter often requires sedation or local anesthesia, while removal of a catheter secured with SAS is rapid and painless. It is quite likely than in the next future cuffed-tunneled catheters will be replaced by uncuffed tunneled catheters secured with SAS.
5 Cyanoacrylate glue
Cyanoacrylate glue is one of the most effective and versatile technologies introduced in the world of venous access in the last decade. Glue for venous access is used in minimal amounts (0.15–0.35 ml) (Fig. 8.24) and should preferably be either butyl-cyanoacrylate or octyl-butyl-cyanoacrylate, since octyl-cyanoacrylate dries too slowly.
When inserting VADs, glue is potentially useful for many different goals: (a) it is highly effective in stopping any bleeding or oozing from the exit site soon after insertion (and such action is also quite cost-effective, as it avoids the risk for an unscheduled dressing change, as it may occur when bleeding is excessive); (b) closing the breach of the exit site, glue effectively reduces the extraluminal contamination by bacteria; (c) it contributes to proper securement of the catheter, preventing dislodgment; (d) last, it is precious for closing skin incisions without the need of stitches.
Glue has been shown to be effective and safe as additional securement of short peripheral cannulas and ECC, used together with semipermeable transparent dressing. It has been shown to be safe, effective, and cost-effective in any CICC, PICC or FICC, where it significantly reduces the risk of local bleeding and infection by sealing the exit site (Fig. 8.25). Also, it is the first option for skin closure (Fig. 8.26) after placement of ports or tunneled catheters.
Clinical studies have shown glue to be safe even on the skin of premature newborns. In vitro studies have demonstrated that the long-term use of glue does not alter the chemical and physical properties of polyurethane catheters.
Obviously, even if glue represents an important strategy for the protection of the exit site, it must be always used in association with semipermeable transparent membranes.
6 Semipermeable Transparent Membranes
Sterile semipermeable transparent dressings in polyurethane are the best protection of the exit site and of the area surrounding the emergency of the catheter from the skin, also contributing to catheter securement (Fig. 8.27). Gauze dressings should not be used routinely for covering the exit site of venous access devices, as they offer no protection at all from bacterial contamination, and they do not contribute to catheter securement. In short, current guidelines recommend that all exit sites of peripheral and central VADs should be protected by transparent membranes: they must be applied properly and replaced weekly.
Commercially available transparent dressings may have different clinical performance, since they have different degrees of transparency, of skin adhesiveness, of permeability, etc.; some transparent dressings are bordered (a feature that decreases the risk of unscheduled dressing change), while some have integrated securement devices. One important feature is permeability, which becomes critical in premature newborns, characterized by a very high trans-epidermal water loss (TEWL). In all neonates, infants, and children, we recommend using transparent membranes with high MVTR (Moisture Vapor Transfer Rate). A transparent membrane with poor permeability (MVTR <1500)—if used in a child with high perspiration—will be associated with accumulation of humidity below the dressing and possible maceration of the skin. For the same reason, the adoption of transparent dressings with chlorhexidine-releasing gel pad should be always avoided in pediatric patients, since the transpiration of the skin area covered by the gel pad will be completely abolished; furthermore, the chlorhexidine released by the gel, acting on the macerated skin, may increase the local damage to the epidermidis.
7 Conclusions
In short, proper catheter securement and proper protection of the exit site require a multimodal strategy that should include: (a) wise choice of the exit site and the adoption—when needed—of tunneling techniques; (b) sutureless securement devices (preferably: subcutaneous anchorage for central VADs with caliber 3Fr or bigger); (c) cyanoacrylate glue (to be used for all VADs); (d) semipermeable transparent dressings (to be used for all VADs).
Catheter securement and protection of the exit site is still an unsolved issue for UVC (see chapter below), though in the future cyanoacrylate glue may play a role in this regard.
The association of cyanoacrylate glue and semipermeable transparent dressing is currently the best securement/protection strategy for ECC and short peripheral cannulas.
Long peripheral cannulas, midline catheters and all external central VADs should be secured and protected by a triple strategy: cyanoacrylate glue, sutureless device, and transparent dressing. In most central VADs, the most effective and cost-effective sutureless device is the SAS (subcutaneous anchored securement).
Bibliography
Barone G, Pittiruti M, Ancora G, Vento G, Tota F, D'Andrea V. Centrally inserted central catheters in preterm neonates with weight below 1500 g by ultrasound-guided access to the brachio-cephalic vein. J Vasc Access. 2021 May;22(3):344–52. https://doi.org/10.1177/1129729820940174.
Biasucci DG, Pittiruti M, Taddei A, Picconi E, Pizza A, Celentano D, Piastra M, Scoppettuolo G, Conti G. Targeting zero catheter-related bloodstream infections in pediatric intensive care unit: a retrospective matched case-control study. J Vasc Access. 2018 Mar;19(2):119–24. https://doi.org/10.5301/jva.5000797.
Cellini M, Bergadano A, Crocoli A, Badino C, Carraro F, Sidro L, Botta D, Pancaldi A, Rossetti F, Pitta F, Cesaro S. Guidelines of the Italian Association of Pediatric Hematology and Oncology for the management of the central venous access devices in pediatric patients with onco-hematological disease. J Vasc Access. 2020;10:1129729820969309. https://doi.org/10.1177/1129729820969309.
Crocoli A, Martucci C, Sidro L, Delle Donne D, Menna G, Pittiruti M, De Pasquale MD, Strocchio L, Natali GL, Inserra A. Safety and effectiveness of subcutaneously anchored securement for tunneled central catheters in oncological pediatric patients: A retrospective study. J Vasc Access. 2021;4:11297298211009364. https://doi.org/10.1177/11297298211009364.
D'Andrea V, Barone G, Pezza L, Prontera G, Vento G, Pittiruti M. Securement of central venous catheters by subcutaneously anchored suturless devices in neonates. J Matern Fetal Neonatal Med. 2021;9:1–4. https://doi.org/10.1080/14767058.2021.1922377.
D'Andrea V, Pezza L, Barone G, Prontera G, Pittiruti M, Vento G. Use of cyanoacrylate glue for the sutureless securement of epicutaneo-caval catheters in neonates. J Vasc Access. 2021;8:11297298211008103. https://doi.org/10.1177/11297298211008103.
Dawson R. PICC Zone Insertion Method™ (ZIM™): A Systematic Approach to Determine the Ideal Insertion Site for PICCs in the Upper Arm. Journal of the Association for Vascular Access. 2011;16(3):156–65.
Giustivi D, Gidaro A, Baroni M, Paglia S. Tunneling technique of PICCs and Midline catheters. J Vasc Access. 2021;16:11297298211002579.
Gorski L, Hadaway L, Hagle M, et al. Infusion therapy standards of practice. J Infus Nurs. 2021;44(1S Suppl 1):S1–S224.
Ostroff MD, Pittiruti M, Ostroff MD, Pittiruti M. Alternative exit sites for central venous access: Back tunneling to the scapular region and distal tunneling to the patellar region. J Vasc Access. 2020 Jul;9:1129729820940178.
Pinelli F, Pittiruti M, Van Boxtel T, Barone G, Biffi R, Capozzoli G, Crocoli A, Elli S, Elisei D, Fabiani A, Garrino C, Graziano U, Montagnani L, Prato AP, Scoppettuolo G, Zadra N, Zanaboni C, Zerla P, Konstantinou E, Jones M, Rosay H, Simcock L, Stas M, Pepe G. GAVeCeLT-WoCoVA Consensus on subcutaneously anchored securement devices for the securement of venous catheters: Current evidence and recommendations for future research. J Vasc Access. 2020;2:1129729820924568. https://doi.org/10.1177/1129729820924568.
Pittiruti M, Scoppettuolo G, Dolcetti L, Celentano D, Emoli A, Marche B, Musarò A. Clinical experience of a subcutaneously anchored sutureless system for securing central venous catheters. Br J Nurs. 2019;28(2):S4–S14. https://doi.org/10.12968/bjon.2019.28.2.S4.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pittiruti, M. (2022). Technique and Devices for Securement of the Catheter and Protection of the Exit Site. In: Biasucci, D.G., Disma, N.M., Pittiruti, M. (eds) Vascular Access in Neonates and Children. Springer, Cham. https://doi.org/10.1007/978-3-030-94709-5_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-94709-5_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94708-8
Online ISBN: 978-3-030-94709-5
eBook Packages: MedicineMedicine (R0)