Abstract
Modern ultrasound scanners have become widely available light-weight portable machines used to produce a rapidly updated two-dimensional grayscale image that aids safe and successful vessel cannulation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Modern ultrasound scanners have become widely available; light-weight portable machines are commonly used to produce a rapidly updated two-dimensional grayscale image that aids safe and successful vessel cannulation.
The term ‘ultrasound’ describes all sound waves of frequencies beyond the range of human hearing (>20 kHz). Ultrasound imaging utilizes a high range of sound waves frequencies (2–15 MHz) to localize and characterize different tissues.
The ultrasound transducer “probe” is a complex and sophisticated piece of electrical equipment, housing piezoelectric crystals, which vibrate to produce an ultrasound pulse when exposed to an electrical current. This phenomenon is named the piezoelectric effect. Hockey-stick linear probes have a small footprint making them ideal for neonatal and pediatric vascular access.
Artefacts describe a range of appearances in the displayed image that are not accurate to the original anatomical features being scanned. The presence of artefacts reduces image quality and leads to potential tissue damage, should images be misinterpreted during invasive procedures.
1 Introduction
In the United Kingdom, the use of ultrasound imaging for obtaining central venous access has become routine practice. A 2015 Cochrane review concluded a benefit in safety and quality using ultrasound over landmark technique for internal jugular vein cannulation. The Association of Anesthetists of Great Britain & Ireland (AAGBI) subsequently published recommendations in May 2016, stating ultrasound should be used routinely for internal jugular venous catheter insertion [1]. Furthermore, the AAGBI Working Party recommended its use for all other central venous access sites, and difficult arterial and peripheral venous cannulation.
Ultrasound imaging can provide useful information during vascular access procedures, including puncture site evaluation, identification of local pathology, guidance during needle puncture, verification of guidewire position and early recognition of complications.
This chapter will provide readers with a brief history of ultrasound, as well as an outline of the principles of ultrasonography, the methods for ideal probe selection and setting adjustments to improve image quality.
2 History of Medical Ultrasound
In 1794, an Italian priest (Lazzaro Spallanzani) deduced that bats use sound inaudible to humans to accurately navigate in complete darkness. His observation saw him become a pioneer, inspiring others to explore the use of sound waves to understand the environment.
By 1880, the Curie brothers had discovered the piezoelectric effect. They observed that the application of mechanical pressure to a quartz crystal produced an electric potential. They also described the reciprocal piezoelectric effect. The generation and reception of high frequency sound waves using crystals was a significant moment in the history of ultrasound and quartz crystals remain integral to modern day ultrasound scanners.
During World War I, ultrasound was used to aid submarine navigation with underwater SONAR (Sound Navigation and Ranging) systems and detect defects in metal constructions (the integrity of a ship’s hull). The use of ultrasound in metal flaw detection alerted physicians to the possibilities within diagnostic medicine, with the first such application arriving when Karl Dussik, at the University of Vienna (1942) attempted to demonstrate changes in brain ventricle size secondary to tumor growth.
George Ludwig’s 1949 experiments using industrial flaw detector equipment on animal tissues reported the mean velocity of sound transmission to be 1540 m/s. This value is still in use today.
Professor Ian Donald (University of Glasgow) explored the application of ultrasound in the field of obstetrics in the 1950s. He used the one-dimensional A-mode (amplitude mode) to measure the parietal diameter of the fetal head. Later he would help invent and construct the world’s first two-dimensional compound B-mode scanner, enabling the operator to visualize the density of tissues.
Technological advances in electronics and piezoelectric materials are accredited for the subsequent developments in ultrasound application within medicine. Collectively these advances mean that ultrasound scanners have today become widely available light-weight portable machines capable of producing high quality real-time greyscale images.
As technology advances, the application of ultrasound expands. Current areas of development include portable wireless probes, three-dimensional images, elastography and contrast enhancement (microbubbles).
3 Ultrasound for Vascular Access
Ultrasound imaging utilizes high frequency sound waves to localize and characterize different tissues. With respect to pediatric vascular access, ultrasound technology can be used to produce a rapidly updated two-dimensional grayscale image that aids safe and successful vessel cannulation.
Ultrasound imaging lends itself to vascular access as it is portable and uses non-ionizing sound waves, with few (if any) contraindications. Real time images and Doppler mode help identify vessel type and patency.
The main disadvantages to its use are operator dependence, poor image quality beyond structures of high impedance, thermal or mechanical injury, and artefacts. The presence of artefacts is important as they reduce image quality and lead to potential tissue damage should images be misinterpreted during invasive procedures.
4 Principles of Ultrasonography
4.1 Physics
A sound wave is formed by the vibration of molecules in a medium, along a line of propagation in a series of compressions (areas of high pressure) and rarefactions (areas of low pressure).
Sound waves can be described by their frequency (ƒ), wavelength (λ) or speed (ν) (Fig. 3.1).
The wavelength is the distance between two identical points on successive peaks or troughs. The number of waves passing a given point per second is the frequency. The speed of the sound wave is the product of the frequency and wavelength.
The term ‘ultrasound’ describes all sound waves of frequencies beyond the range of human hearing (>20 kHz). The ultrasound waves used in diagnostic medical imaging have a frequency of 2–15 MHz.
The speed of the sound wave in the human body varies depending on the tissue type through which the wave propagates (Table 3.1). The density and compressibility characteristics of different tissues (acoustic impedance) impact the speed at which the sound wave travels.
For the generation of a scan image an average speed in soft tissues is required for calculations.
The assumed average speed of ultrasound in soft tissue is 1540 m/s.
4.2 Ultrasound Wave Formation
The ultrasound transducer “probe” is a complex and sophisticated piece of electrical equipment, housing artificial polycrystalline ferroelectric materials (ceramics).
The piezoelectric crystals vibrate to produce an ultrasound pulse when exposed to an electrical current. This phenomenon is named the piezoelectric effect. Once a sound wave is produced, the crystals are dampened and switch to listening for the returning echoes. Modern ultrasound transducers oscillate between “emitting” and “listening” modes more than 7000 times a second (pulse echo principle).
The crystals convert the returning ultrasound echoes into an electrical impulse which is interpreted by the ultrasound machine to generate the displayed image.
The typical linear array probe has approximately 200 crystals along the flat surface of the transducer producing a rectangular field of view. Small subgroups of piezoelectric crystals are exposed to electric impulses in a coordinated and sequenced nature, to produce a narrow ultrasound beam that sweeps across the transducer surface (Fig. 3.2). Less than 0.1 s is required for all the crystals to emit their ultrasound waves, producing a high frame rate, allowing moving structures to be visualized in real time.
Each returning echo detected by the transducer is represented by a pixel on the screen, the brightness of which is directly proportional to the strength of the returning sound wave. Structures that strongly reflect ultrasound waves lead to the production of large electrical signal intensities, appearing white or hyperechoic on the final image.
The time from pulse generation to echo detection is used to determine the depth of the reflecting structure, which is represented by the pixel position on the display screen [3].
Each small subgroup of crystals is responsible for the formation of a vertical line of pixels on the final ultrasound scan image. The brightness and depth of the pixels is dependent on the strength of the returning echo from each depth. As the vertical line of pixels from each crystal subset are compiled in series, a complete image of the tissue is produced.
A major problem with grey scale image production is that echoes reflected from deeper structures are characteristically weaker. As these sound waves have travelled further through tissues, they are subject to greater degrees of attenuation, which results in images becoming dimmer at greater depths. Ultrasound machines use “time gain compensation” to counter the effects of attenuation, by increasing signal amplitude at greater depths. This in theory should produce an image of uniform brightness when scanning homogenous tissue.
4.3 Resolution
Resolution is an important marker of image quality and refers to the machines ability to distinguish the structures we need to see. The three types of resolution include: spatial (axial and lateral), contrast and temporal.
Axial resolution describes the ability to differentiate two objects that both lie in the path of the ultrasound beam (one directly above the other) (Fig. 3.3). Good axial resolution is vital for pediatric vascular access and requires probes producing short pulses with short wavelengths (high frequency). Should the distance between the two objects be less than 1.5 × wavelength, the machine will not be able to differentiate the reflected echoes.
When the two objects are adjacent to each other (equal depth from probe face), the ability to differentiate them relies on the machine’s lateral resolution (Fig. 3.4). Lateral resolution is always worse than axial and is improved with narrow and well-defined ultrasound beams (small subsets of crystals).
Temporal resolution is directly related to the frame rate and depends on the scanning rate (sweep speed) of the ultrasound machine. With relatively slow advancement of needles for regional or vascular access, this is rarely a major issue with modern machines.
Contrast resolution describes the ability to identify structures with different reflection characteristics, by subtle changes in their shade of grey on the image.
4.4 Doppler
Color Doppler ultrasound provides directional information about blood flow and can aid differentiation between veins and arteries. The “color map” is superimposed over the grayscale image (B-mode image), reducing the frame rate (Fig. 3.5).
The frequency of ultrasound echoes returning to the probe is dependent on the directional movement of the reflective source, relative to the probe. Should the scanned object be moving towards the transducer, the frequency of the ultrasound wave would increase. Such movement is best demonstrated at a vector 0° and completely absent at 90° (i.e., when flow is perpendicular to the probe).
For vascular access, Color Doppler ultrasound enables a color map to overlay the greyscale image. Flow towards the probe will be represented by colors from red to yellow dependent on calculated velocities. Flow away from the probe will be represented as blue through to green (Fig. 3.6). Therefore, it is wrong to assume that imaged blood flow highlighted as red is arterial or that blue would represent venous blood flow.
Color bar used to indicate direction of flow [with permission from SonoSite [4]]
4.5 Artefact
Ultrasound machines rely on a number of assumptions to simplify the production of the displayed image, one of which is that the average speed of ultrasound in soft tissues at 1540 m/s. The net result of the assumptions is potential artefact generation.
Artefacts describe a range of appearances in the displayed image that are not accurate to the original anatomical features being scanned.
The false image can lead to misinterpretation and injury during invasive procedures. Therefore, structures in the displayed image should not be assumed to be real, until scanned in two planes (transverse and longitudinal).
It is not crucial to diagnose the artefacts affecting the image, but an understanding of why the artefacts occur may help in there eliminate or simply alert the operator to their existence.
4.6 Contact Artefacts
Images with shadowing or loss of image from the top are subject to contact artefact (Fig. 3.7). The use of smaller hockey stick ultrasound probes in pediatrics helps to avoid contact artefact. The most common reasons are poor skin contact with the probe, lack of gel, faulty transducers, or air interface.
4.7 Acoustic Shadowing
Bony structures reflect ultrasound waves extremely well (bone and calcification) and are said to be acoustically opaque. The lack of ultrasound penetration produces a dark shadow deep to the acoustically opaque structure on the display image. Vessel walls - when scanned in plane - exhibit the same acoustic shadowing, potentially complicating plane vessel cannulation.
4.8 Post-Cystic Enhancement
Echoes returning from deeper structures tend to be of lower signal strength because of attenuation. To produce an image with consistent brightness, the machine compensates by increasing the amplitude of echoes from deeper structures proportionally to their depth of origin (time gain compensation). However, fluid filled cysts have low echogenicity and the area distal to the cyst will have more gain applied, so appear (falsely) brighter; this artefact is often used to differentiate between solid and fluid filled cysts.
4.9 Reflection Artefact
Large smooth surfaces such as the pleura or diaphragm can act as mirror reflectors of the ultrasound beam. The resultant image will contain the true target structure, in addition to a false second reflected image. Good knowledge of anatomy will help differentiate between true and reflected images.
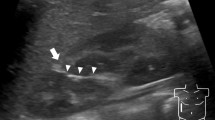
4.10 Reverberation
Multiple linear or hyperechoic areas distal to a reflective structure are observed when ultrasound waves reflect back and forth between two strongly reflecting structures (Fig. 3.8). Shallow or flat advancement of the cannulating needle during in plane vessel cannulation may be complicated by reverberation artefact. Increasing the angle of entry should reduce this.
Comet tail artefacts are a type of reverberation artefact. They are bright echoes that fade with depth, producing the characteristic comet tail appearance. They are often encountered during vascular access procedures, whilst scanning the needle tip out of plane.
4.11 Slice Thickness Artefact
This is a common artefact caused by structures outside the sector being scanned, producing echoes that affect the final displayed image. The curved nature of vessel walls means that when scanned in plane, echoes outside the image plane show up as in the vessel.
4.12 Refraction Artefact
As a needle passes through two tissues of different acoustic impedance, the final image may indicate a step deformity in the needle structure. This occurs as most scanners assume a fixed speed of sound in tissues, as previously discussed.
5 Transducer or “Probe” Selection
The part of the probe in contact with the patient is called the “face of the transducer” and it determines the probes’ footprint. The common probes available are Linear, Curvilinear and Phased Array.
Each probe differs in their operating frequency, physical size, and footprint. Appropriate probe selection is critical in the production of high-quality images, so increasing the success rates of cannulation.
Inappropriate probe selection can make a difficult task even harder and potentially unsafe.
5.1 Linear
The piezoelectric crystals are arranged in a line across the flat transducer face, to produce a rectangular ultrasound image (Fig. 3.9). With operating frequencies between 5 and 18 MHz, they are ideal for older children, and will produce images with good resolution of detail at depths of 2–3 cm, ideal for vascular access.
5.2 Hockey-Stick Linear
These probes are small and can be held with a “fountain pen” grip (Fig. 3.10). With a small footprint, this subtype of linear probe is ideal for obtaining images from awkward areas. Enabling excellent skin contact, the probe is ideal for neonatal and pediatric vascular access.
5.3 Curvilinear (Convex)
With their curved face, these probes produce a fan-shaped scan field, these probes operate at lower frequencies (2–5 MHz) and penetrate deeper structures (Fig. 3.11). They will produce images of structures up to 10 cm deep, albeit with coarse detail, ideal to examine the abdominal organs.
5.4 Phased Array (Sectorial)
The piezoelectric crystals produce ultrasound in phases resulting in a triangular image. They are frequently used for cardiac imaging.
Probes operating at a higher frequency, will produce images of higher resolution of detail. The draw back will be lack of depth. Therefore, appropriate probe and frequency selection is the first key step to achieving a quality image. Once this has been achieved, there are several further small adjustments that can be made to improve image quality to aid the operator.
6 Improving Images
6.1 Gain
The option of adjusting the overall gain allows the operator to control the brightness of the entire image (Fig. 3.12). Increasing the “receive” gain adjusts the amplitude of the ultrasound echoes and increases the “brightness” of the resultant image. As all pixels in the image are equally brightened, artefacts also appear brighter. Excessive gain is detrimental, as the image appears too bright, artefacts are enhanced, and subtle textural changes are obscured.
Time gain compensation (TGC) proportionally increases the amplitude of distant echoes to compensate for the effect of attenuation (Fig. 3.13). Without TGC, images would progressively become darker with depth. This compensation produces a more uniform image with regards to brightness. Sophisticated machines automatically increase the gain of echoes from deeper structures being imaged. Certain machines will allow the operator to control the level of gain by rotary control for “near gain” and “far gain”, or slider controls.
6.2 Depth
The use of the depth control allows the target and other important structures to be appropriately placed on the display. Ideally the target area should be focused on the center of the screen, approximately two thirds of the total depth of the scan image.
6.3 Focus
Most machines have a focus control that enables an area of the scan image to be enhanced, providing greater detail. For the best results, this should be set just deep to the target area.
6.4 Dynamic Range
This control adjusts the number of different shades of grey available for the image generation (Fig. 3.14). The lower the dynamic range, the greater the contrast and more “black and white” the ultrasound image. A low dynamic range is the ideal setting for vascular access.
With more shades of grey available, images using a high dynamic range show less contrast but subtler textural changes in the scan image. This setting would be ideal for imaging abdominal organs, especially the liver.
6.5 Zoom
The zoom feature enlarges an area of the image. There are two different types of zoom: the ‘write zoom’ increases the resolution of the selected area and the ‘read zoom’ simply magnifies the pixels.
7 Practical Tips
7.1 Tracking Structures
To aid understanding and image interpretation, target structures can be “tracked” from different locations where they are easier to identify. Tilting the probe in the longitudinal axis alters the angle of incidence at which the ultrasound wave strikes the target object. This phenomenon is called anisotropy and it can greatly improve image quality or expose a previously unseen target.
7.2 Probe Orientation
In-plane needling has the advantage of imaging much of the needle, thereby minimizing damage to adjacent structures. However, a pure in-plane technique requires considerable skill as the ultrasound beam may be only 0.2–3 mm thick. Complications can occur during advancement with a partial view of the needle shaft. The size of the neck in neonates can be so small that an in-plane technique is impractical due to significant loss of contact. Out-of-plane techniques are frequency used for this very reason. With an out-of-plane technique, the hyperechoic “dot” represents the needle crossing the ultrasound beam. To find the needle tip, the probe can be moved on the skin surface along the needle’s axis until the “dot” disappears.
The more acute the angle of needle insertion, the poorer the ultrasound reflection from the needle surface. Therefore, insertion of the needle at less than 45 degrees to the ultrasound beam improves needle imaging.
Key Points
-
Today, the use of ultrasound imaging for obtaining central venous access has become routine practice
-
Ultrasound scanners have become widely available as light-weight portable machines capable of producing high quality real-time greyscale images
-
The term ultrasound describes all sound waves of frequencies beyond the range of human hearing (>20 kHz)
-
The ultrasound transducer “probe” is a complex and sophisticated piece of electrical equipment, housing piezoelectric crystals
-
Ultrasound machines use “time gain compensation” to counter the effects of attenuation, by increasing signal amplitude at greater depths
-
Artefacts describe a range of appearances in the displayed image that are not accurate to the original anatomical features being scanned
-
Due to the occurrence of artefacts, structures in the displayed image should not be assumed as real, until scanned in two planes (transverse and longitudinal)
-
Inappropriate probe selection can make a difficult task even harder and potentially unsafe.
-
To aid understanding and image interpretation, target structures can be “tracked” from different locations where they are easier to identify.
Bibliography
Brass P, Hellmich M, Kolodziej L, Schnik G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev. 2015;1:CD006962.
Woo J. A short history of the development of ultrasound in obstetrics and gynecology. http://www.ob-ultrasound.net/history1.html. Accessed 10 Nov 2017.
SonoSite. Physics of ultrasound notes. http://cutsurgery.com/assets/physics_notes_v2.pdf. Accessed 12 Nov 2017.
Warman P, Nicholls B, Conn D, Wilkinson D, editors. Oxford specialist handbooks in anaesthesia: regional anaesthesia, stimulation, and ultrasound techniques. Oxford: Oxford University Press; 2014.
Association of Anaesthetists of Great Britain and Ireland. Safe vascular access 2016. Anaesthesia. 2016;71:573–85.
Kaproth-Joslin KA, Nicola R, Dogra VS. The history of US: From bats and boats to the bedside and beyond. RadioGraphics. 2015; 35 (3):960–970. https://pubs.rsna.org/doi/pdf/10.1148/rg.2015140300
Lin E, Gaur A, Jones M, Ahmed A. Sonoanatomy for anaesthetists. Cambridge: Cambridge University Press; 2012.
Smith T, Pinnock C, Lin T, editors. Fundamentals of anaesthesia. 3rd ed. Cambridge: Cambridge University Press; 2009.
Thoirs K. Physical and technical principles of sonography: a practical guide for non-sonographers. Journal of Medical Radiation Sciences. 2012;59(4):124–32. https://doi.org/10.1002/j.2051-3909.2012.tb00188.x.
Ziskin MC. Fundamental physics of ultrasound and its propagation in tissue. RadioGraphics. 1993; 13 (3):705–709. https://pubs.rsna.org/doi/pdf/10.1148/radiographics.13.3.8316679.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Malhi, G.S., Bennett, J. (2022). Principles of Ultrasonography and Settings of Ultrasound Devices for Children. In: Biasucci, D.G., Disma, N.M., Pittiruti, M. (eds) Vascular Access in Neonates and Children. Springer, Cham. https://doi.org/10.1007/978-3-030-94709-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-94709-5_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94708-8
Online ISBN: 978-3-030-94709-5
eBook Packages: MedicineMedicine (R0)