Abstract
Given the significant mortality and morbidities associated with isolated tricuspid valve surgery, transcatheter tricuspid valve repair has emerged as a viable, less-invasive alternative in patients with symptomatic severe tricuspid regurgitation who are deemed high risk for surgery. Several transcatheter tricuspid valve devices exist, including the coaptation-based TriClip, PASCAL, and FORMA systems. Growing evidence suggests that such devices are best suited for patients with annular dilatation with mild-to-moderate leaflet tethering. Preoperative transesophageal echocardiography is crucial for procedural planning and success. Although all three devices are still in their infancy, early safety and feasibility trials have shown encouraging results. Specifically, the TRILUMINATE trial demonstrated the safety and efficacy of the TriClip device at mid-term follow-up, while the US Early Feasibility Study showed the same with the FORMA system. First-in-human studies have also validated the clinical and echocardiographic success of the FORMA and PASCAL systems. Despite these promising early results, longer follow-up and pivotal trials are needed to validate the efficacy and durability of these coaptation-based devices.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tricuspid valve repair
- Tricuspid regurgitation
- Ttranscatheter tricuspid valve intervention
- Coaptation
- Edge-to-edge
- TriClip
- PASCAL
- FORMA
- TRILUMINATE
- Tricuspid valve surgery
Introduction
Tricuspid valve disease, specifically tricuspid regurgitation (TR), affects at least 1.5 million people in the United States, with an annual incidence of approximately 200,000 new cases [1]. Tricuspid valve disease is most often functional in the setting of left-sided heart disease, atrial fibrillation (AF), and pulmonary hypertension, where right ventricular remodeling leads to annular dilatation and leaflet tethering [2, 3]. As TR becomes moderate to severe, it becomes an independent predictor of increased mortality, even when patients are asymptomatic [4, 5]. Furthermore, untreated TR carries a grim prognosis, especially when irreversible right heart failure and end-organ dysfunction develop [6]. Tricuspid valve surgery (TVS) is currently the standard of care in symptomatic patients on maximal medical therapy, but it results in significant operative mortality and morbidities [7, 8]. In addition, isolated TVS is associated with the highest mortality among all contemporary valve procedures at 8.8–9.7% [8, 9]. TR, therefore, remains perceptibly undertreated despite guidelines urging prophylactic tricuspid valve repair (TVr) at the time of left-sided cardiac surgery under specific circumstances [10, 11].
To meet this clinical need, a number of transcatheter tricuspid valve interventions (TTVI) have been developed over the past decade. Patients currently referred for TTVI generally present with refractory heart failure. In the multicenter, international TriValve registry, the vast majority of patients were in New York Heart Association (NYHA) class III–IV, with a mean EuroSCORE II surgical mortality risk of 7.6 ± 5.7% [12].
Transcatheter tricuspid valve intervention technologies can be broadly categorized into devices for coaptation, annuloplasty, caval valve implantation (CAVI), and transcatheter tricuspid valve replacement (TTVR) [11]. Almost all these technologies are investigational with very limited clinical evidence, but early feasibility and safety trials have shown promise. Here, we critically review the various coaptation-based strategies in the context of their evolving clinical indications. Interventions other than leaflet approximation techniques, including TTVR, are covered elsewhere.
Pre-procedural Imaging and Assessment
Transthoracic (TTE) and transesophageal echocardiographic (TEE) evaluation remain the mainstay of pre-procedural pathoanatomical evaluation of the tricuspid valve, especially for predicting the feasibility of repair with a coaptation-based device. As seen in Fig. 13.1, critical TEE views include the four-chamber view, the tricuspid valve right ventricular inflow-outflow X-plane to grasping view (to visualize the septal and anterior/posterior leaflets for leaflet grasping), and the transgastric basal short-axis view (to evaluate the TR jet and assess septal leaflet mobility) [13]. Computed tomography (CT) is also helpful for defining the anatomy of the tricuspid apparatus (see Chap. 7). All coaptation-based strategies require accurate measurements of the maximal anteroposterior and septolateral diameters, right ventricular geometry, and the maximal distance from the tricuspid valve to the right ventricular apex [14]. The target anchoring site of a spacer-type coaptation device can also be selected using CT imaging by drawing a perpendicular line linking the annular plane with the right ventricular septal free wall on a sagittal reconstruction [15]. Furthermore, CT imaging can also assess the size of the venous access site (e.g., left subclavian or axillary vein) for spacer-based coaptation devices [3].
Preoperative transesophageal echocardiographic evaluation of tricuspid valve and regurgitation. Preoperative TEE is essential in defining the pathoanatomy of the tricuspid valve apparatus. (a) RV inflow (left) and X-plane-to-grasping (right) views. (b) Transgastric view showing a central coaptation defect due to annular dilatation. (c, d) Doppler color flow mapping of the aforementioned views showing severe TR. A, anterior leaflet of the tricuspid valve; P, posterior leaflet of the tricuspid valve; RV, right ventricular; S, septal leaflet of the tricuspid valve; TEE, transesophageal echocardiography; TR, tricuspid regurgitation
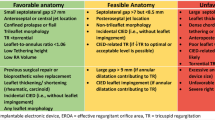
Although there is a dearth of strict guidelines on TTVI repair strategy selection, expert consensus suggests that coaptation-based devices should be used in patients with annular dilatation with mild-to-moderate leaflet tethering. This is particularly true when the regurgitant jet is predominantly anteroseptal or central [16]. Evidence also suggests that the probability of successful repair with this strategy increases when the largest measured coaptation gap is no greater than 7 mm [17, 18], thus underscoring the importance of precise echocardiographic assessment. In contrast, an annular device is likely to be sufficient when minimal leaflet tethering is present. Advanced right ventricular remodeling with severe leaflet tethering and/or large coaptation gaps often requires TTVR or CAVI [16].
Coaptation-Based Devices
Coaptation-based strategies are currently the most commonly used transcatheter techniques in treating functional TR. Numerous devices exist, including the TriClip (Abbott Structural Heart, Santa Clara, CA), PASCAL (Edwards Lifesciences LLC, Irvine, CA), and FORMA (Edwards Lifesciences LLC) systems.
TriClip
Given its widespread availability and operator familiarity, the MitraClip system (Abbott Structural Heart, Santa Clara, CA), typically used to treat mitral regurgitation, has become the leading choice in patients with functional TR undergoing TTVI (off-label application) (Fig. 13.2a). In fact, MitraClip was used in 66% of patients in the TriValve registry [19]. One or more clips may be used to bicuspidize the valve by approximating, most commonly, the anterior and septal leaflets (Fig. 13.3). Clips may also be used to create a triple orifice by connecting the septal leaflet to the anterior and posterior leaflets, thus directly reducing the coaptation gap and counteracting annular dilatation [20, 21]. Early studies have shown that the latter might be more efficient in reducing the septolateral tricuspid annular diameter [21]. In addition to patients with functional TR, the MitraClip system has been used, with varying degrees of success, in patients with degenerative and lead-associated TR, as well as in those with large leaflet notches [22,23,24].
Intraoperative transesophageal echocardiography and fluoroscopy of transcatheter tricuspid valve repair with the MitraClip System. The MitraClip device, which uses one or more clips to bicuspidize the tricuspid valve, is shown here via intraoperative TEE. (a, b) The device (yellow arrows and red asterisk) is seen to be grasping the anterior and septal leaflets. (c) Post-deployment TEE shows mild residual TR. Also shown are fluoroscopic images of (d) the device open in the right ventricle for grasping, (e) the anterior and septal leaflets being grasped, and (f) device deployment. A, anterior leaflet of the tricuspid valve; P, posterior leaflet of the tricuspid valve; S, septal leaflet of the tricuspid valve; TEE, transesophageal echocardiography; TR, tricuspid regurgitation
Outcomes of MitraClip TTVI show early promise. In a multicenter European registry, Nickenig et al. reported on 64 high-risk patients with moderate or greater TR who were treated with the MitraClip system. There were no intra-procedural deaths, strokes, or major vascular complications, and successful device implantation was achieved in 97% of patients. In-hospital mortality was 5%. TR was reduced by at least one grade in 91% of patients, with concurrent improvements in NYHA class and 6-minute walking distance [25]. These results were corroborated by Orban et al., where 50 patients with severe TR underwent edge-to-edge repair. At 6 months, mortality was 16%, and 90% of patients had achieved a persistent reduction of at least one echocardiographic TR grade [26].
The 1-year outcomes of the TRILUMINATE trial (which used the tricuspid valve-specific TriClip system) were recently reported. This was a prospective, multicenter, early feasibility study that assessed 85 patients, with symptomatic moderate or greater TR, who underwent TriClip implantation [27]. TR reduction was achieved in 87% of subjects at 1 year, and the proportion of patients in NYHA class I/II increased from 22% at baseline to 80% at 1 year. All-cause mortality was 5.9% and there were no device-related safety events beyond the 30-day mark, thus validating the safety and durability of repair with the TriClip system [28]. The TRILUMINATE Pivotal Trial (NCT03904147), a prospective, multicenter, randomized controlled trial comparing the efficacy of TriClip to medical therapy is currently underway.
There are certain limitations, however, with the TriClip system. First, the anterior location of the tricuspid valve may hamper intraprocedural TEE assessment. In these cases, intracardiac echocardiography may be considered to ensure coaxial alignment with the device to avoid acoustic shadowing of the delivery catheter against the tricuspid leaflets, thus improving confirmation of leaflet insertion after grasping [29]. Steering of the Clip system within the right atrium can sometimes also be limited with the MitraClip system, requiring use of alternative strategies such as the “miskey” technique with 90° counterclockwise insertion [23]. Additionally, patients with functional TR often have large coaptation gaps that necessitate multiple grasping attempts and clips. Pacemaker leads may also pose significant challenges due to acoustic shadowing against the tricuspid leaflets, leaflet tethering, or interference with the Clip delivery system. Finally, the relatively smaller subvalvular space within the right ventricle may cause the Clip delivery system to entangle with the tricuspid valve or its chordae [3, 30].
With pending CE mark approval of the TriClip system, the growing experience with the next-generation TriClip NTR and XTR devices will undoubtedly improve clinical and procedural outcomes. Given that the tricuspid valve, as well as its associated coaptation gap, tends to be larger compared to its mitral counterpart, the longer device arms of the XTR system may be especially effective in reducing TR [16].
PASCAL
The PASCAL system constitutes two paddle-shaped, independently closeable, clasps (~25 mm width, ~10 mm length) and a central spacer (Fig. 13.2b) that was originally intended for the treatment of mitral regurgitation [31]. It is delivered via a 22-French steerable guide sheath, a steerable catheter, and an implantation catheter, and it is repositionable and recapturable if required [3]. The larger and wider device arms, presence of a central spacer, and the ability to grasp leaflets independently may all contribute to this system’s unique applications within TTVI [32].
The feasibility, safety, short-term durability, and clinical outcomes of PASCAL were recently reported in a multicenter, observational study. Twenty-eight patients with severe TR and heart failure underwent compassionate use of this system. Procedural success was 86% with no intra-procedural complications. Overall, 30-day mortality was 7.1%. Furthermore, the incidence of patients in NYHA functional class ≥III was reduced from 100% at baseline to 12% at 1 month. In addition, 85% had less than moderate TR at the 30-day post-repair follow-up [33]. Although this early report demonstrated significant clinical improvements with the PASCAL system, larger prospective studies and clinical trials are required to assess its long-term safety and durability.
FORMA
The FORMA device treats TR by using a passively expanding, foam-filled balloon to occupy the regurgitant orifice area and reduce the leaflet coaptation gap (Fig. 13.2c). It is delivered via a left subclavian-axillary approach (using a 20–24 French sheath introducer) through a rail anchored at the right ventricular apex. The device, currently available in three sizes (12, 15, and 18 mm), is completely retrievable and unique in its ability to treat very large coaptation gaps not amenable to repair with other systems [11].
Much progress has been made since the first-in-human FORMA experience in 2015 [34]. Perlman et al. reported the 1-year outcomes of treatment of severe TR with FORMA system in 18 patients. Procedural success was 89% (the two unsuccessful procedures were right ventricular perforation requiring open surgery and device dislocation). There was no mortality at 1 year. Furthermore, 79% of patients were in NYHA class I/II with similar improvements in the average 6-minute walk test. Finally, 46% of patients had moderate or less TR, thus demonstrating mid-term safety and efficacy of the FORMA system [14].
More recently, the short- and mid-term outcomes on 29 patients with severe functional TR from the FORMA US Early Feasibility Study (US EFS) were reported [35]. Mortality was 7% at 30 days and 31% at 1 year. Also, 20% and 31% of patients were in NYHA class I at 30 days and 1 year, respectively, with similar improvements in mean vena contracta and effective regurgitant orifice area in paired analyses. Despite demonstration of feasibility and improvements in heart failure symptoms and quality of life, the US EFS raised several safety concerns that have yet to be addressed [36]. Interestingly, these results were in contrast to those reported by Asmarats et al. in their study of 19 patients who underwent TTVI with the FORMA system. The long-term outcomes from this study suggested a favorable safety profile in high-surgical-risk patients with sustained functional improvements and reductions in TR severity [37].
The aforementioned initial findings have spurred a number of modifications within the second-generation FORMA system. For instance, larger spacers are now available that address “torrential” forms of TR. Additionally, device anchoring is improved by a new sheath and a radiopaque apposition indicator [38]. The ongoing Repair of Tricuspid Valve Regurgitation Using the Edwards TricuSPid TrAnsCatheter REpaiR System (SPACER) trial (NCT02787408), with 78 enrolled participants, will shed further light on the safety, efficacy, and durability of this technology.
Experimental Devices
Three experimental, coaptation-based devices – the Cerclage-TR block (Tau-PNU Medical), Mistral device (Mitralix), and CroíValve system (CroíValve) – will be briefly discussed here.
Cerclage-TR Block
This system uses a septal leaflet extension (a soft membrane attached to a backbone column that crosses the tricuspid valve obliquely) to compensate for the regurgitant orifice (Fig. 13.2d). In preclinical studies, this technology was shown to reduce the severity of TR by at least one grade in four of five swine models [39]. However, further research and clinical first-in-human studies are needed to validate these promising results.
Mistral
This is a spiral-shaped device that targets the subvalvular chordae tendineae of the tricuspid valve apparatus (Fig. 13.2e). Delivered through an 8.5-French delivery system, this device is rotated within the right ventricle to grasp the chordae of two adjacent leaflets, thus pulling them together to enhance coaptation [40]. Eight first-in-human and four compassionate-use cases have been reported with variable amounts of follow-up (1–12 months). Procedural success was obtained in 10 out of the 12 patients with significant improvements in reduction of TR severity seen in 5 out of the 12 patients [41]. As with the Cerclage-TR block system, further clinical evaluation is necessary to affirm the safety and efficacy of this device.
CroíValve
The CroíValve system is a coaptation-based strategy that is anchored in the superior vena cava and placed, as a spacer, among the leaflets of the tricuspid valve, thus reducing the size of the regurgitant orifice (Fig. 13.2f). This device also consists of an inner apparatus that augments diastolic flow through the valve, thus mitigating the risk of device thrombosis. Preclinical studies showed early promise, and acute and chronic feasibility studies are ongoing [42].
Conclusion
Transcatheter tricuspid valve intervention is quickly emerging as a viable alternative to tricuspid valve surgery in high-risk surgical patients. Within TTVI repair strategies, coaptation-based devices are particularly efficacious for patients with tricuspid annular dilatation with mild-to-moderate leaflet tethering. Preoperative TEE and CT imaging are essential for procedural planning and success. Three main coaptation technologies, namely the TriClip, PASCAL, and FORMA systems, have emerged this past decade, with varying clinical and echocardiographic outcomes at short- and mid-term follow-up. The results of ongoing clinical trials will undoubtedly shed light on the long-term efficacy and durability of these devices.
References
Stuge O, Liddicoat J. Emerging opportunities for cardiac surgeons within structural heart disease. J Thorac Cardiovasc Surg. 2006;132(6):1258–61.
Rodes-Cabau J, Taramasso M, O'Gara PT. Diagnosis and treatment of tricuspid valve disease: current and future perspectives. Lancet. 2016;388(10058):2431–42.
Asmarats L, Puri R, Latib A, Navia JL, Rodes-Cabau J. Transcatheter tricuspid valve interventions: landscape, challenges, and future directions. J Am Coll Cardiol. 2018;71(25):2935–56.
Singh JP, Evans JC, Levy D, Larson MG, Freed LA, Fuller DL, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol. 1999;83(6):897–902.
Topilsky Y, Nkomo VT, Vatury O, Michelena HI, Letourneau T, Suri RM, et al. Clinical outcome of isolated tricuspid regurgitation. JACC Cardiovasc Imaging. 2014;7(12):1185–94.
Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004;43(3):405–9.
Kilic A, Saha-Chaudhuri P, Rankin JS, Conte JV. Trends and outcomes of tricuspid valve surgery in North America: an analysis of more than 50,000 patients from the Society of Thoracic Surgeons database. Ann Thorac Surg. 2013;96(5):1546–52; discussion 52.
Zack CJ, Fender EA, Chandrashekar P, Reddy YNV, Bennett CE, Stulak JM, et al. National trends and outcomes in isolated tricuspid valve surgery. J Am Coll Cardiol. 2017;70(24):2953–60.
Alqahtani F, Berzingi CO, Aljohani S, Hijazi M, Al-Hallak A, Alkhouli M. Contemporary trends in the use and outcomes of surgical treatment of tricuspid regurgitation. J Am Heart Assoc. 2017;6(12)
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(22):e57–185.
Asmarats L, Taramasso M, Rodes-Cabau J. Tricuspid valve disease: diagnosis, prognosis and management of a rapidly evolving field. Nat Rev Cardiol. 2019;16(9):538–54.
Taramasso M, Hahn RT, Alessandrini H, Latib A, Attinger-Toller A, Braun D, et al. The international multicenter TriValve registry: which patients are undergoing transcatheter tricuspid repair? JACC Cardiovasc Interv. 2017;10(19):1982–90.
Tang GHL. Tricuspid clip: step-by-step and clinical data. Interv Cardiol Clin. 2018;7(1):37–45.
Perlman G, Praz F, Puri R, Ofek H, Ye J, Philippon F, et al. Transcatheter tricuspid valve repair with a new transcatheter coaptation system for the treatment of severe tricuspid regurgitation: 1-year clinical and echocardiographic results. JACC Cardiovasc Interv. 2017;10(19):1994–2003.
Naoum C, Blanke P, Cavalcante JL, Leipsic J. Cardiac computed tomography and magnetic resonance imaging in the evaluation of mitral and tricuspid valve disease: implications for transcatheter interventions. Circ Cardiovasc Imaging. 2017;10(3)
Ho EC, Ong G, Fam NP. Transcatheter tricuspid valve intervention: a practical algorithm for patient selection. Curr Opin Cardiol. 2019;34(2):164–72.
Besler C, Orban M, Rommel KP, Braun D, Patel M, Hagl C, et al. Predictors of procedural and clinical outcomes in patients with symptomatic tricuspid regurgitation undergoing transcatheter edge-to-edge repair. JACC Cardiovasc Interv. 2018;11(12):1119–28.
Hausleiter J, Braun D, Orban M, Latib A, Lurz P, Boekstegers P, et al. Patient selection, echocardiographic screening and treatment strategies for interventional tricuspid repair using the edge-to-edge repair technique. EuroIntervention. 2018;14(6):645–53.
Taramasso M, Alessandrini H, Latib A, Asami M, Attinger-Toller A, Biasco L, et al. Outcomes after current transcatheter tricuspid valve intervention: mid-term results from the international TriValve registry. JACC Cardiovasc Interv. 2019;12(2):155–65.
Latib A, Mangieri A, Agricola E, Denti P, Regazzoli D, Giannini F, et al. Percutaneous bicuspidalization of the tricuspid valve using the MitraClip system. Int J Cardiovasc Imaging. 2017;33(2):227–8.
Braun D, Orban M, Orban M, Hagl C, Massberg S, Nabauer M, et al. Transcatheter edge-to-edge repair for severe tricuspid regurgitation using the triple-orifice technique versus the bicuspidalization technique. JACC Cardiovasc Interv. 2018;11(17):1790–2.
Fam NP, Ho EC, Ahmed N, Connelly KA. Transcatheter edge-to-edge repair of lead-associated tricuspid regurgitation. EuroIntervention. 2017;13(10):1166–7.
Braun D, Nabauer M, Orban M, Orban M, Gross L, Englmaier A, et al. Transcatheter treatment of severe tricuspid regurgitation using the edge-to-edge repair technique. EuroIntervention. 2017;12(15):e1837–e44.
Fam NP, Ho EC, Edwards J, Connelly KA. Edge-to-edge repair of a large anterior leaflet notch with severe tricuspid regurgitation. EuroIntervention. 2018;14(6):654–5.
Nickenig G, Kowalski M, Hausleiter J, Braun D, Schofer J, Yzeiraj E, et al. Transcatheter treatment of severe tricuspid regurgitation with the edge-to-edge MitraClip technique. Circulation. 2017;135(19):1802–14.
Orban M, Besler C, Braun D, Nabauer M, Zimmer M, Orban M, et al. Six-month outcome after transcatheter edge-to-edge repair of severe tricuspid regurgitation in patients with heart failure. Eur J Heart Fail. 2018;20(6):1055–62.
Nickenig G, Weber M, Lurz P, von Bardeleben RS, Sitges M, Sorajja P, et al. Transcatheter edge-to-edge repair for reduction of tricuspid regurgitation: 6-month outcomes of the TRILUMINATE single-arm study. Lancet. 2019;394(10213):2002–11.
Nickenig G; on behalf of the TRILUMINATE investigators. Percutaneous edge-to-edge repair for tricuspid regurgitation: Initial 1-year outcomes from the TRILUMINATE clinical trial. Presented at: PCR London Valves 2019. November 18, 2019.
Pozzoli A, Taramasso M, Zuber M, Maisano F. Transcatheter tricuspid valve repair with the MitraClip system using intracardiac echocardiography: proof of concept. EuroIntervention. 2017;13(12):e1452–e3.
Braun D, Orban M, Nabauer M, Orban M, Gross L, Englmaier A, et al. Transcatheter treatment of severe tricuspid regurgitation using the edge-to-edge repair technique in the presence and absence of pacemaker leads. JACC Cardiovasc Interv. 2017;10(19):2014–6.
Praz F, Spargias K, Chrissoheris M, Bullesfeld L, Nickenig G, Deuschl F, et al. Compassionate use of the PASCAL transcatheter mitral valve repair system for patients with severe mitral regurgitation: a multicentre, prospective, observational, first-in-man study. Lancet. 2017;390(10096):773–80.
Fam NP, Ho EC, Zahrani M, Samargandy S, Connelly KA. Transcatheter tricuspid valve repair with the PASCAL system. JACC Cardiovasc Interv. 2018;11(4):407–8.
Fam NP, Braun D, von Bardeleben RS, Nabauer M, Ruf T, Connelly KA, et al. Compassionate use of the PASCAL transcatheter valve repair system for severe tricuspid regurgitation: a multicenter, observational, first-in-human experience. JACC Cardiovasc Interv. 2019;12(24):2488–95.
Campelo-Parada F, Perlman G, Philippon F, Ye J, Thompson C, Bedard E, et al. First-in-man experience of a novel transcatheter repair system for treating severe tricuspid regurgitation. J Am Coll Cardiol. 2015;66(22):2475–83.
Kodali S, Hahn R, Babaliaros V, Lerakis S, Thourani V, Makkar R, et al. TCT-4 Transcatheter tricuspid valve repair in patients with functional tricuspid regurgitation: 2-year outcomes from the FORMA US early feasibility study. J Am Coll Cardiol. 2019;74(13 Supplement):B4.
Muntane-Carol G, Del Val D, Bedard E, Philippon F, Rodes-Cabau J. Transcatheter innovations in tricuspid regurgitation: FORMA device. Prog Cardiovasc Dis. 2019;
Asmarats L, Perlman G, Praz F, Hensey M, Chrissoheris MP, Philippon F, et al. Long-term outcomes of the FORMA transcatheter tricuspid valve repair system for the treatment of severe tricuspid regurgitation. J Am Coll Cardiol Intv. 2019;12(15):1438.
Asmarats L, Philippon F, Bedard E, Rodes-Cabau J. FORMA tricuspid repair system: device enhancements and initial experience. EuroIntervention. 2019;14(16):1656–7.
Chon M-K, Jung S-M, Lee SY, Lee S-H, Hwang KW, Kim J, et al. TCT-18 novel concept of catheter-based treatment for tricuspid regurgitation (Cerclage-TR block): a preliminary animal experiment in a swine model. J Am Coll Cardiol. 2018;72(13 Supplement):B8.
Curio J, Demir OM, Pagnesi M, Mangieri A, Giannini F, Weisz G, et al. Update on the current landscape of transcatheter options for tricuspid regurgitation treatment. Interv Cardiol. 2019;14(2):54–61.
Planer D. The Mistral Device (Mitralix): Device Features and First-In-Human Data. Presented at: TVT 2019. June 12, 2019.
Quinn M. CroíValve Percutaneous Tricuspid Coaptation Valve. Presented at: TVT 2019. June 12, 2019.
Author Disclosures
Dr. Tang receives speaker’s honoraria and is a consultant for Abbott Structural Heart. The remaining authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sengupta, A. et al. (2022). Transcatheter Tricuspid Valve Intervention: Coaptation-Based Strategies. In: Mathelier, H., Lilly, S.M., Shreenivas, S. (eds) Tricuspid Valve Disease. Contemporary Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-030-92046-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-92046-3_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92045-6
Online ISBN: 978-3-030-92046-3
eBook Packages: MedicineMedicine (R0)