Abstract
Interest in perinatal mental distress has been increasing in recent years. Data from international literature show that almost 25% of women of the general population in perinatal period (pregnancy and post partum) suffer from under diagnosed affective and anxiety disorders. These data make the need for early and adequate interventions in this field dramatically evident. The Multicentric Observatory for Perinatal Depression (OMDP) is an observatory born from the cooperation of Tor Vergata and Sapienza Perinatal Mental Health Services, which now oversees the participation of several universities and territorial structures located in central, southern and northern Italy. The purpose of the Multicentric Observatory for Perinatal Depression (OMDP), is to conduct an extensive and precocious screening program for perinatal depression with a uniform and standardized criterion for all the Italian Centres participating, starting from the first trimester of pregnancy to 1 year after delivery, to create in the future a prophylactic and therapeutic network, offering the most effective and the safest therapeutic pathways. Pandemic Covid-19 has dramatically changed perinatal assistance and the activity of OMDP, which now is starting again with the screening program, and adding telepsychiatry to traditional visits and evaluation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Perinatal mental health
- Pregnancy
- Post-partum
- Early screening
- Multicentric observatory for perinatal depression
- Pandemic Covid-19
- Telepsychiatry
1 Introduction
Interest in perinatal mental distress has been increasing in recent years. The publication in 2015 of data on maternal perinatal mortality (i.e., between 42 days and 1 year after birth) in the UK showed that around a quarter of perinatal deaths were caused by mental health problems; in particular, one in seven cases resulted in suicide. These data make the need for early and adequate interventions in this field dramatically evident. In Italy, since 2012, the Istituto Superiore di Sanità (ISS) has been coordinating the monitoring of maternal perinatal mortality, by collating data from ten Italian regions (Piedmont, Lombardy, Friuli Venezia Giulia, Emilia-Romagna, Tuscany, Lazio, Campania, Apulia, Sicily, and Sardinia), covering 77% of national births. This monitoring revealed that, for every 100,000 live births, there were 2.1 maternal deaths due to post-partum haemorrhage, while there were 2 deaths due to suicide, mainly occurring in a violent manner such as by hanging or jumping from a height. Due to these dramatic observations, 16 regional projects dedicated to the prevention and early recognition of perinatal mental distress were approved in 2018. In 2016, the project “Intervention for the recognition of perinatal psychological distress and support for fragile motherhood and fatherhood” had already started. This project is promoted by the network of services of the birth path and primary care, coordinated by the Emilia-Romagna region in collaboration with the National Centre for Disease Prevention and Control (CCM) and with the involvement of five other Italian regions: Piedmont, Tuscany, Lazio, Campania, and Sicily.
The UK guideline on Antenatal and Postnatal Health calls on maternity professionals, who are, often exclusively, focused on physical health, to carefully assess the woman’s psychological conditions “empathically”, thereby detecting information considered fundamental to the identification of women at risk of developing perinatal psychological distress: both the woman’s and the couple’s attitude towards pregnancy, the presence of a social and family network, the abuse of alcohol or other substances , the quality of the woman’s interpersonal relationships, any conditions of social and housing isolation, domestic abuse and violence, employment, and economic and migration conditions. As far as the anamnestic assessment is concerned, the ISS-CCM project suggests collecting, as part of the first clinical interview during pregnancy or after childbirth, information on conditions, which would necessitate the involvement of a specialist mental health service, i.e. current or previous serious mental disorders, current or previous treatment for mental disorders, close family history of serious psychological distress after childbirth, use of alcohol and drugs, eating disorders, and advises the use of screening tests. Also in 2018, the Ministry of Health funded the project “Measures pertaining to the prevention, diagnosis, treatment and care of postpartum depressive syndrome”, which involved the territorial services dedicated to primary care throughout the country. In the same period, a collaboration between the Perinatal Psychopathology Centres of three University Policlinics in Rome (Policlinico Tor Vergata, Policlinico Umberto I—Sapienza 1, Azienda Ospedaliera S. Andrea—Sapienza 2) led to the establishment of a Multicentric Observatory for Perinatal Depression (OMPD), supported by the association “Volontari per il Policlinico Tor Vergata o.n.l.u.s” with the patronage of the Italian Society of Psychiatry (SIP) Lazio regional section.
2 The Multicentric Observatory for Perinatal Depression—OMDP
The purpose of the Multicentric Observatory for Perinatal Depression (OMDP) is to conduct an extensive and precocious screening programme for perinatal depression with a uniform and standardised criterion, which will lead, in the future, to the creation of a prophylactic and therapeutic network, offering the most effective and the safest therapeutic pathways.
Therefore, the OMDP programme entails the following activities:
-
Screening programme for women from the first trimester of pregnancy
-
Identification of social and psychiatric predictors of perinatal depression
-
Assessment of the risk and diagnosis of any disorders from the first trimester of pregnancy, so that early intervention can be established to reduce foetal damage in the early stages of pregnancy
-
Prospective re-evaluation during the whole peripartum period: second and third pregnancy trimester, 1 and 6 months after childbirth, 1 year after delivery, to facilitate early identification of new cases and protect the mental health of both of woman and child
OMDP oversees the participation of several universities and territorial structures located in central, southern, and northern Italy.
Currently the OMDP centres are the following:
Local Health Districts: Departments of Mental Health of Rome and Lazio and Psychiatric Service of the Health District of Bolzano
University Facilities: University of Rome “Tor Vergata”, University of Rome “La Sapienza” (Policlinico Umberto I and Azienda Ospedaliera Sant’Andrea), Catholic University of the Sacred Heart of Rome, University “Gabriele d’Annunzio” Chieti-Pescara, University of Foggia, University of L’Aquila, University of Campania “Luigi Vanvitelli”, University of Catania, University of Palermo, and Polytechnic University of Marche
Since December 2018, the screening programme promoted by the OMDP has taken the form of a research project in collaboration with the three Roman centres and the Italian Society of Psychiatry (SIP), Lazio regional section, promoted by the Association “Volunteers for the Policlinico Tor Vergata o.n.l.u.s”. The scientific managers of the project are Prof. Cinzia Niolu, Prof. Franca Aceti, and Prof. Gloria Angeletti. Among the collaborators of the scientific committee are Dr. Emanuela Bianciardi, Dr. Giulia Lisi, Dr. Nicoletta Giacchetti, Dr. Ilaria Adulti, Dr. Lavinia De Chiara, and Dr. Alexia Koukopoulos. The coordinator of OMDP is Prof. Alberto De Stefano, President of “Policlinico Tor Vergata Onlus”. The study is still in progress at all the centres, with the aim of collecting as much data as possible, which will be analysed from a dynamic and longitudinal point of view, to allow an accurate assessment, over time, of all the variables examined. Therefore, the aims of the OMDP can be summarised as the intention to implement a screening programme with a shared and uniformly applied criteria, in line with national and international programmes promoting women’s mental health, as well as studying the role and distribution of the psycho-socio-demographic factors most associated with maternal depression, in order to identify risk factors at an early stage. In this way, we try to highlight the need to create, in the near future, a network of preventions and treatment valid in all regions, including homogeneous therapeutic strategies.
A specific inter-university working group has been created to coordinate the project in order to:
-
1.
Integrate and systematise data collection from the different centres.
-
2.
Organise periodic meetings to update on the activities.
-
3.
Organise training activities (congresses, seminars, CME courses, masters of perinatal psychopathology, FAD courses, dedicated lectures, internships) aimed at professionals involved in patient and group/family management: doctors, psychologists, psychiatric rehabilitation technicians, nurses, midwives, and assistants. The training courses have been carried out both in-person (at the different university sites and at the local centres) and via virtual connection during the pandemic.
-
4.
Establishing and maintaining a periodic discussion on gender psychiatry issues and perinatal health with the regional mental health authorities, in particular with the Regional Consultation and the Mental Health Commission of the Medical Association, the ISS, and the Ministry of Health.
Study subjects are women over 18 years old in pregnancy or during the post-partum period, able to understand the purpose and procedures of the study and to give their written informed consent. The exclusion criteria considered are as follows: (a) diagnosis of mental retardation/intellectual disability; (b) diagnosis of autism spectrum disorder; and (c) inability to give written informed consent.
After signing the informed consent to participate in the study, women are required to fill out a data sheet that investigates the following anamnestic data: personal data, level of education, occupation, presence or absence of a stable relationship, information regarding the current pregnancy, and stressful life events that occurred in the 12 months prior to pregnancy.
Participants are also asked to complete the EPDS (Edinburgh Perinatal Depression Scale). The EPDS excludes somatic symptoms (e.g. changes in appetite and sleep) that are very common in women during the perinatal period. Item 10 investigates thoughts of self-harm and suicidal tendencies. Final score reaches a maximum of 30. Cut-off for a positive screening is, generally, applied at 13. In a summary of over 40 studies using EPDS, Hewitt et al. have, instead, adopted 12 as the cut-off for major depression and 10 for a combination of major and minor depression. Recent review work shows that both sensitivity and specificity of EPDS range from 80 to 90%, considering the most common cut-offs applied, but there is a considerable variability between studies in terms of setting, population, and screening threshold. In addition to identifying a condition of possible depression, three EPDS sections investigate the anxiety element arising in the prenatal and postnatal population. EPDS is available in many different languages other than English. In fact, for South Tyrolean patients whose mother tongue was German, we translated the informed consent and the data sheet into German and used EPDS validated in Germany. The evaluation is repeated in the three quarters of the pregnancy and at 1 month, 6 months, and 1 year after childbirth.
In the results presented below, when considering EPDS, a minimum cut-off of 9 was used. It was, also, useful to propose a subdivision of the scores obtained into ranges:
A score from 9 to 11 is an indication of a possibility of depression.
A score higher than 12 correlates with a greater probability of depression.
Certainly, in accordance with the most recent literature and with the DSM V, the EPDS cannot be used as the sole tool for diagnosing perinatal depression, as it, always, requires clinical confirmation by a psychodiagnostic interview, but it provides a concrete indication of the need for in-depth clinical investigation in a specialist setting. Health professionals, subsequently, contacted each patient found to be at risk of perinatal depression, to investigate the presence of possible pathology.
3 Data Analysis: Big Data and Machine Learning
We have chosen to analyse and process the preliminary data collected from the various participating centres using machine learning tools that allow us to analyse as many variables as possible, thereby giving us a point of reference for the future.
In particular, we refer to the Bayesian network, a machine learning tool, which “learns” from past data, relying on previously collected data and the associated evolution, to make predictions from input of new data.
The tool has a solid scientific basis, utilising the Bayes theorem, which manages the calculation of conditional probabilities. The idea is to build a network between variables (graph) in which the available data are connected by “cause-effect” relationships, with scientifically verified reliability.
Therefore, the potential of this tool is, easily, understood, when applied to the characteristics investigated in our patients. Basically, from the data provided at the first evaluation, the Bayesian network is able to calculate, in the first trimester, the individual risk of developing post-partum depression or, at least, of experiencing an increase in EPDS scores after childbirth.
Thus, the Bayesian network offers a completely transparent analysis tool, capable of calculating and providing the relationships between specific variables and able to easily identify the individual relative weight. It is an easy-to-use system, quick to activate, since a few hundred historical data are generally sufficient to build a training dataset in preparation for learning. Finally, as well as a screening and projection tool for individual patient, it can also be used to outline the most incisive risk factors and to identify the most exposed profiles for depression.
Access to such an innovative calculation tool was guaranteed by the profitable collaboration with KPMG (“Klynveld Peat Marwick Goerdeler”), a network of independent companies that deals with the provision of professional services to companies, active in more than 150 countries. In particular, KPMG in the healthcare sector is recognised by the market as a centre of absolute excellence, thanks to a portfolio of best practices and integrated services able to support the evolution of the national, regional, and local health service. KPMG has, freely, made available to the OMDP the activity of expert consultants in the field of big data, for the creation of a Bayesian network demo, in which the data coming from the following centres have converged:
LAZIO: University of Rome “Tor Vergata”, University of Rome “La Sapienza” (Policlinico Umberto I and Azienda Ospedaliera Sant’Andrea), and Catholic University of the Sacred Heart of Rome
ABRUZZO: University “d’Annunzio” Chieti-Pescara and University of L’Aquila
CAMPANIA: University of Campania “Luigi Vanvitelli”
PUGLIA: University of Foggia
SICILY: University of Palermo
TRENTINO ALTO ADIGE: Psychiatric Service of the Health District of Bolzano
The data collection period stops to the immediate pre-pandemic, February 2020. The lockdown situation, with the consequent remodelling of the afferent to perinatal mental health services, resulted in a prolonged stop to OMDP activity, with most centres active only for emergencies and different procedures for routine visits. Later, we will discuss the new approaches used during the pandemic, which the OMDP shared with the working group of the Istituto Superiore di Sanità in the ISS report COVID-19 n 44/2020 [1].
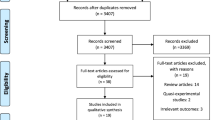
The data refer to a total of 1294 assessments of which 907 were performed in the pre-partum period and 387 in the post-partum period.
The first waffle chart shows the prevalence by trimester of pregnancy and by region, considering the cut-off at EPDS ≥ 12 (Fig. 20.1). There is considerable heterogeneity between regions in the prevalence estimates. This is due to regional differences in the organisation of perinatal health that make it difficult, for example, in some centres, to recruit patients in the first trimester. In the first trimester, the prevalence is higher in Campania, while in the third trimester, the highest prevalence is found in Abruzzo.
The waffle chart in Fig. 20.2 shows the prevalence of perinatal depression post-partum divided by follow-up period and by region. The data for Sicily and Trentino Alto Adige are not yet available. The number for Puglia is very small. In Lazio there is a particularly high prevalence in all follow-up periods. By the way, data from Lazio are pooled from three centres, Tor Vergata, Sapienza 1 and 2, and Sacred Heart Universities. We would like to specify that the entry of the University of Foggia into the study was, despite their best efforts, delayed by bureaucratic constraints. This explains the lack of data collected by this centre at the time of the statistical evaluation. The Apulian centre is rapidly coming into line with the sample size.
The variables considered and investigated, especially from the biographical data sheet, are extremely useful in defining clinical risk variability. The aim of the OMDP is to overcome these regional differences, providing valid instruments for conducting standardised screening in the general population. Although the administration of the EPDS, alone, is useful for this purpose, it is clear that this instrument may be incomplete and undoubtedly reductive, given the complexity of psychiatric pathology which is ill-suited to objective and binary measurements and moreover considering the huge organising inequalities in mental health facilities in different regions in our country. This is even more true regarding depression during pregnancy, when, at more than any other time of life, biology is intertwined with numerous other social, psychological, and environmental factors.
In light of these reflections, there is an urgent need to resort to new calculation tools, capable of functioning in a big data mining system, with machine learning software being the only ones able to respond to one of the specific and perhaps most pressing needs we have in psychiatry, that is, the need for personalisation, precision psychiatry, and patient-tailored treatment strategies.
For decades, we have been working on group averages and statistics that examine general populations with only diagnostic homogeneity, but which are insufficient to respond to the needs and complex individuality of the single patient. Machine learning will allow us to make individualised predictions, with an accuracy that psychiatric medicine has never been capable of, leading to the common goal of precision psychiatry and hoping that this tool will be extended to our entire field of research and clinical practice.
4 Notes on the First Multicentre Experience
The OMDP project aims to analyse the perinatal period from the very beginning, i.e. from the first trimester of gestation. From the data collected so far, the importance of investigating symptoms and pre-morbid characteristics, from the very first moments of pregnancy, is highlighted for predicting the possible development and evolution of perinatal depression.
In this first multicentric experience, we have noticed a certain rate of non-participation in the study mainly due to the lack of interest in the topic and the belief in the low relevance of the problem. The number of women who dropped out of the current study was approaching half of the initial participating sample. We have, also, identified the cause as the stigma that still surrounds the concept of mental illness, and especially perinatal mental illness, added to the lack of knowledge of the pathology. Many women were surprised and put off by the proposal to administer the test during pregnancy, as they were unaware that depression could occur even before birth and not only post-partum. Other women felt it necessary to specify that the pregnancy was planned and experienced with extreme joy, ascribing peripartum depression to unwanted pregnancies only. The women who were most enthusiastic about participating in the project were those who were, already, well informed about the topic or who reported personal experiences, direct or indirect, of perinatal depression or psychiatric disorders in general.
A truly decisive factor in promoting the adherence of the participants was the collaboration of the gynaecologists and midwives, who, in several cases, were personally involved in proposing the study in advance, during routine visits. So, it was possible to include the questionnaire in the classic gynaecological pathway followed by all pregnant women, and in these cases, we have been able to ascertain a greater ease and immediacy of proposal and higher rates of adherence to the project. The data obtained for this sample, which we can probably consider representative of the entire population, also show the unfortunately well-rooted presence of stigma, which continues to affect psychiatric pathology. Similarly, our data seem to carry with them the solution to the problem. They show us the clear and incontrovertible need for collaboration between specialists in order to spread correct knowledge of the illness and the need for screening. Only if doctors begin to consider psychiatric pathology in the same way as other complications that can affect pregnancy, can we, really, envisage active and effective prevention of peripartum depression.
Considering the current data in our possession and the experiences of the clinicians involved in the OMDP project, there is a need to structure national screening programmes that can reach the entire population from the first trimester. The identification of a disorder that is so widespread and so sadly fraught with complications cannot be left to chance or to the good sense of gynaecologists, but requires regulation and clear guidelines. Complications due to perinatal depression can be avoided, or at least improved, through early identification and care of the mother. With the OMDP project, we propose to implement a standardised, efficient, and functionally economical screening programme, demonstrating the real feasibility of such a project, which, without burdening health budgets, would reach all pregnant women in a widespread and early way, thus enabling real prevention.
Unfortunately, many women are still unaware of the importance of perinatal depression for themselves, for the child, and for the whole family, but what is most shocking is the refusal to cooperate, albeit fortunately, in only a few cases, by professionals who should follow women at all stages of their lives, especially the most delicate and fragile one, namely, reproduction.
The hope for the future is that, through close coordination between psychiatrists, obstetricians, gynaecologists, and paediatricians, an adequate level of awareness and knowledge of the disease can be achieved and that screening can be included as a routine examination, to be carried out directly in the obstetrical environment and then assessed in the psychiatric setting. The questionnaires for perinatal depression must be included in the routine medical records of the pregnant woman, in the same way as all other specialist examinations and tests carried out to ensure the well-being of the maternal-foetal dyad. This is one specific target of OMDP program, which we submitted to the Regional Council of Lazio, to the Minister of Health Beatrice Lorenzin during the third day for Woman’s Health in April 2018, and to the Health Councilor of Lazio in 2019.
It is essential that a proper screening programme starts as soon as the woman becomes aware of her pregnancy, because the first trimester is actually a time of great psychological (A), endocrine (B), and immunological (C) upheaval (A) [2]; (B) [3]; (C) [4]; [5, 6]. These changes lead to a significantly increased risk of developing depression and anxiety. This is also a crucial period for foetal development, so early intervention improves obstetric and neonatal outcomes [7].
The effects of perinatal depression on the child have as yet not been fully clarified and undoubtedly need further study and investigation to extend knowledge to neonatology, paediatrics, and child neuropsychiatry and, why not, to adult psychiatry, because, after all, “there is no health without perinatal mental health”. In fact, the increasing amount of data in the literature shows that the length of the study of peripartum should be extended up to 1 year after delivery, because throughout this period the probability of the onset of the disease remains constantly high and, therefore, prevention must continue well after discharge from the obstetric ward.
Another important factor highlighted in the context of the OMDP is the importance of administering not only an EPDS questionnaire but also a comprehensive data sheet that collects all the information needed to stratify the population into risk classes and direct prevention interventions towards the most vulnerable groups. Prevention should also include fathers, who play an important role in perinatal care and can act as both a protective and risk factor in the development of perinatal depression, as well as being affected by their partner’s mental health status and needing support themselves.
Working on the prejudice that, unfortunately, still surrounds this pathology, improving coordination between maternal and neonatal health specialists and promoting the spread of adequate longitudinal perinatal screening programmes, means protecting the health of the whole family and, in particular, permitting the healthiest possible development of the foetus and the newborn. This will be achieved thanks to the activity that therapy for depression has, indirectly, on the uterine environment in which the foetus grows, by decreasing the impact of all the neurohormonal and inflammatory factors on epigenetic mechanisms. In addition, achieving maternal psychopathological compensation promotes a correct and healthy way of interacting with the newborn and thus the creation of the attachment bond after birth. This makes it possible to interrupt the chain of intergenerational transmission of mental disorders and, more generally, of pathology and distress in the newborn, as well as in the future adolescent and adult.
5 OMDP in the Lockdown and New Challenges in Perinatal Mental Health
The COVID-19 pandemic has been and continues to be in its various waves, an element that has profoundly modified the content and manifestations of mental health, in general, and of perinatal health in particular.
While we are starting to collect the first data on the short-term effects, we still do not know what the medium- and long-term effects will be on the psyche of women who experienced pregnancy during the first lockdown.
The November 2020 [8] review and meta-analysis by Hessami et al., for example, show evidence of an increased risk of mental disorders, such as depression and anxiety, in women in the perinatal period, due to the restrictions associated with the COVID-19 pandemic. Eight studies reporting depressive and anxiety states of 7750 women, either pregnant or post-partum, were included. The overall pooled EPDS score was higher among women during the pandemic (SMD = 0.40, 95% CI: −0.05 to 0.86, p = .083) compared to previous non-pandemic times, without reaching a statistically significant difference. However, the overall pooled STAI score was significantly higher during the pandemic (SMD = 0.82, 95% CI: 0.49–1.16, p < .001).
In order to investigate the presence of peripartum anxious and depressive symptoms, during the SARS-Co-V2 pandemic, and in an attempt to highlight any existing relationships between the COVID-19 worry and psychopathological or sociodemographic variables, the OMDP conducted a study on a sample of 100 women in pregnancy and post-partum. The study (Noos et al.; [9]) was born from the collaboration between the Policlinico Tor Vergata and the territorial service of the ASL of Latina. The subjects were administered:
-
EPDS
-
PSS (Perceived Stress Scale)
-
DES-T (Dissociative Experience Scale)
-
DASS-21 (Depression, Anxiety, Stress Scales)
-
PHQ-9 (Patient Health Questionnaire)
-
Questionnaire on the Degree of Preoccupation About Virus COVID-19 Contagion [10]
From the analysis of the data collected, it emerged that 11% (n = 11) of the women had a minor depressive disorder, having obtained an EPDS score between 9 and 11, while 24% (n = 24) had an overt perinatal depression, having obtained values greater than or equal to 12 (Figs. 20.3 and 20.4). In addition, 7% of the sample had mild symptoms of anxiety, 8% had moderate symptoms, 6% had severe symptoms, and 1% had severe symptoms of anxiety. Finally, 84% of the sample scored between 5 and 9 on the PHQ-9, indicating the presence of subthreshold depression.
With regard to the items and instruments most closely related to stress and its COVID-related consequences, at the PSS 24% of the sample scored between 11 and 14, indicating the presence of stressful events but a good coping capacity, able to ensure the maintenance of a good level of well-being. 27% had a score between 15 and 18, a medium-high result that indicates the possibility that, although unconscious, the accumulated stress is already affecting the body, thoughts, emotions, and behaviour. 22% scored above 19, indicating a state of suffering experienced by both body and mind in response to high levels of potentially harmful stress in the medium to long term.
Finally, analysis of the responses to the questionnaire on concern about COVID-19 infection showed that 84% of the sample had at least a mild-to-moderate degree of concern. Specific data are presented in Table 20.1.
Preliminary results showed a statistically significant relationship between scores obtained in the EPDS, DASS21, PHQ-9, and PSS psychometric scales and the degree of worry about COVID-19 infection. On the other hand, as regards the linear relationship between dissociative symptomatology, age of the sample, and preoccupation with contagion, a trend was observed without reaching a statistical significance. Figure 20.5 below summarises the results of the various relationships measured.
The overview described in the previous paragraphs highlights the urgency and importance of promoting and supporting research concerning the impact of the pandemic and its psychopathological influences in such a delicate period as the peripartum.
The result of the OMDP Lazio study is greater than that described by the previous case studies: 35% of the sample presented depressive symptoms (also subthreshold symptoms) with an EPDS score > or equal to 9.
The psychopathological variables investigated (depression, anxiety, stress) were found to be correlated with the dimension “COVID-19 worry”. In the sample recruited, age does not influence the degree of COVID-19 worry; however, the sample has a limited age range (women of childbearing age between 21 and 44 years with an average age of 33 years) which does not allow the results to be extended to the general population. Furthermore, there is no relationship between the level of concern by COVID-19 and the carrying out of a working activity in the week preceding data collection. It is also clear that the presence of material socio-economic determinants (the presence or absence of employment) is not a variable that influences COVID-19 anxiety and distress. As widely demonstrated in the literature, there are psycho-social determinants of mental health that are not strictly related to a concrete economic-employment condition, but are more inherent to an existential condition of “vital poverty”.
Among the risk factors specifically linked to the pandemic, loneliness and isolation stand out. Norms for social distancing have made it impossible for fathers to access both pregnancy check-ups and the delivery room itself. The distancing of the partner from these shared procedures not only creates discomfort for the latter, which is likely to increase the already large number of paternal perinatal depressions, but also increases the woman’s sense of isolation and perceived loneliness, with a consequent increase in the risk of depressive experiences of loneliness, helplessness, and inability. By the same token, with estrangement from extended family members, mother and mother-in-law, especially in the post-partum period, the woman finds herself alone and facing a new and potentially destabilising situation, unable to “lean on” her own attachment figures. Therefore, women find themselves in a state of loneliness, at just the moment when, more than any other, they have need of support. This has, inevitably, generated a strong concern and anxiety in facing the whole peripartum period. Loneliness can be defined as “a psychological condition arising from the lack of meaningful interpersonal relationships or from the discrepancy between the human relationships a subject wishes to have and those he actually has. They may be unsatisfactory by their nature, their number, or the subject’s inability to establish or maintain positive and meaningful relationships with others” [11, 12]. As a reminder of how this is a significant risk factor for women’s psychological and physical well-being, the World Health Organisation emphasises the right of all women to a positive birth experience, regardless of COVID-19 infection. The presence of the father, or of a person of the woman’s choice (chaperone), during labour, birth, and hospitalisation is an organisational aspect that falls within the competence of individual healthcare facilities. At present, there is a great deal of variability between healthcare facilities, even within the same regions, although the evidence on the positive effects (well-being and safety of the woman) of having a trusted person present during childbirth is now well established. The indications, therefore, recommend the presence of a person of the woman’s choice during labour and childbirth, as an essential element for her well-being. In addition to setting up perinatal mental health screening programmes as early as the first trimester of pregnancy, there is a particularly urgent need to set up programmes to monitor the psychological conditions of women facing motherhood at this sensitive time [13]. This is also aimed at preventing psychophysical damage to the foetus and repercussions for the development of the mother-child relationship linked to the conditions described above. Dedicated applications (app) can be made available for use by the mother on her smartphone, with the aim of collecting the emotional diary, the online appointment diary, and the weekly EPDS. This practice was carried out by the SOS Mamma service, implemented during the COVID-19 emergency by the Policlinico di Tor Vergata in Rome and by many other centres belonging to the Multicentric Observatory for Perinatal Depression.
In May 2020, just at the end of the first lockdown, the staff of OMDP collaborated with the ISS working group Mental Health and Emergency to the writing of Report no. 44/2020 of the Istituto Superiore di Sanità. This document, among other detailed recommendations and suggestions on dealing with perinatal mental health and pandemic, establishes that the screening programme can also be presented by means of information material (containing complete information for contacting operators by telephone or email) on occasions when contact with the healthcare facility is maintained by necessity: routine visits during pregnancy in consulting rooms or hospital wards; at the time of delivery and, in any case, before the woman and child are discharged from the hospital ward; during post-delivery visits, in particular those with the midwife, gynaecologist, and free-choice paediatrician; and the child’s first vaccination at vaccination points. A basic requirement of the programme is the signing of the privacy policy and the informed consent, which can be sent by e-mail to the address the woman provided at the first telephone contact. As a second option, for women who do not have an email address, confirmed adherence via the functions of a smartphone may be sufficient.
After screening, it is also possible to offer an in-person interview, given the willingness to come to the facility, to women with high EPDS scores and who are assumed to have a high level of depression or anxiety. In this case the recommended measures to limit the spread of the epidemic should be respected. Meetings in the facility should be conducted according to current recommendations: face-to-face interviews should be conducted with the necessary PPE (mask), maintaining a safe distance of at least 1 m between the user and the operator. Interviews should be staggered to avoid crowding, and waiting rooms should be reorganised: fewer chairs should be provided and spaced out, and magazines and newspapers should be removed. In addition, carers should be asked to wait outside.
In any case, whatever the method chosen by health professionals, it is highly desirable, in the current emergency scenario, that the monitoring of women’s psychological well-being in the postnatal period be maintained by means of attentive follow-ups, in order to intercept any forms of psychological distress linked to the experience of the epidemic that might also manifest themselves at a later date.
References
ISS Report COVID-19, n. 44/2020. Indications of an intervention plan for the management of perinatal anxiety and depression in COVID-19 emergency and post-emergency phase. Version of May 31, 2020. ISS Working Group Mental Health and Emergency Covid-19-2020
Stewart DE. Clinical practice. Depression during pregnancy. N Engl J Med. 2011;365(17):1605–11.
Sacher J, et al. The peripartum human brain: current understanding and future perspectives. Front Neuroendocrinol. 2020:100859.
Mellor, A. L., & Munn, D. H. Extinguishing maternal immune responses during pregnancy: implications for immunosuppression. In: Seminars in immunology, vol. 13(4), pp. 213–218, 2001, Academic Press
Trowsdale J, Betz AG. Mother’s little helpers: mechanisms of maternal-fetal tolerance. Nat Immunol. 2006;7(3):241–6.
Molendijk ML, et al. Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations (N = 9484). Mol Psychiatry. 2014;19(7):791–800.
Rosenberg MD. Baby brains reflect maternal inflammation. Nat Neurosci. 2018;21(5):651–3.
Hessami K, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Mater Fetal Neonatal Med. 2020:1–8.
Zerbin F, Lisi G, Siracusano A, Niolu C. Salute mentale perinatale e Covid 19. Noos. 2020;26(2):97–107.
Lisi G, Ribolsi M, Siracusano A, Niolu C. Maternal vitamin D and its role in determining fetal origins of mental health. Curr Pharm Des. 2020;26(21):2497–509.
Van Amelsvoort TAMJ. Eenzaamheid is ongezond [Loneliness is unhealthy]. Tijdschr Psychiatr. 2020;62(10):824–5.
Giacchetti N, Roma P, Pancheri C, Williams R, Meuti V, Aceti F. Personality traits in a sample of Italian filicide mothers. Rivista di Psichiatria. 2019;54(2):67–74.
Giacchetti N, Pancheri C, Williams R, Marconi M, Magistro R, Pozzuoli S, Aceti F. Violence and motherhood: a case study about the personality profile and attachment style of a Filicide woman. Deviant Behav. 2020a;41(5):607–18.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Niolu, C., Aceti, F., Angeletti, G., Giacchetti, N., Adulti, I. (2022). Prevention and Treatment in Peripartum: The Multicentric Observatory for Perinatal Depression. In: Percudani, M., Bramante, A., Brenna, V., Pariante, C. (eds) Key Topics in Perinatal Mental Health. Springer, Cham. https://doi.org/10.1007/978-3-030-91832-3_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-91832-3_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91831-6
Online ISBN: 978-3-030-91832-3
eBook Packages: MedicineMedicine (R0)