Abstract
Approximately 10–20% of women experience perinatal depression (PND) (Gaynes et al., AHRQ Evid Rep Summ. 119:1–8, 2005). PND is often underdiagnosed and underreported, due in part to the overlap in PND symptoms and normative changes that occur during the perinatal period (Leung and Kaplan, J Am Diet Assoc 109:1566–1575, 2009). Further, many women experiencing PND feel hesitant to share struggles with health professionals and loved ones, often due to societal stigma and the shame associated with feeling depressed during a time when they are expected to feel joy (Dennis and Chung-Lee, Birth. 33:323–331). This pause that mothers may have in opening up about their experience can make women feel alone during this time, thereby worsening mental health outcomes (McCarthy and McMahon Health Care Women Int 29:618–637, 2008). PND is one of the most common complications that perinatal women experience, above and beyond many other prominent pregnancy or delivery-related complications (e.g., preeclampsia, c-section) (Robertson et al., Gen Hosp Psychiatry. 26:289–295, 2004).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Diagnosis
PND is characterized by a non-psychotic depressive episode with symptoms that mirror those of a major depressive episode (MDE), including a depressed mood, disturbed sleep or appetite, low energy, and poor concentration [6]. As opposed to a general MDE, distinguishing pregnancy-specific features are often present among women in the perinatal period [2]. These features can include a persistent fear of hurting the newborn, lack of interest in the child, and severe anxiety or agitation in the context of motherhood.
According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), the criteria for depression during the perinatal period mirrors the diagnostic criteria for major depressive disorder (MDD) [6]. Specifically, a diagnosis requires the presence of either depressed mood or anhedonia (loss of interest or pleasure in nearly all activities); in addition to either depressed mood or anhedonia, at least four of the additional symptoms listed below must be met for at least 2 weeks. These symptoms must represent a clear worsening relative to the individual’s pre-episode functioning. In order to make this diagnosis, the presence of these symptoms must also be associated with clinically significant distress or impairment in social or occupational functioning. Finally, the symptoms cannot be attributed to substance use behavior nor any other medical condition.
-
1.
Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, hopeless) or observation made by others (e.g., appears tearful)
-
2.
Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation)
-
3.
Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day
-
4.
Insomnia or hypersomnia nearly every day
-
5.
Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down)
-
6.
Fatigue or loss of energy nearly every day
-
7.
Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick)
-
8.
Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others)
-
9.
Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
A “peripartum” specifier within the DSM-5 is used to capture women who meet criteria for depression during pregnancy or within the first 4 weeks of postpartum. Despite this recommendation, most perinatal mental health experts extend the postpartum window and conceptualize postpartum depression (PPD) as a depressive episode that occurs anytime within 1-year postpartum [7]. This is a notable departure from the DSM-5 guidelines, and our recommendation is to use this one-year timeline, as PPD cases tend to peak 2–3 months after delivery [8].
More broadly, it is important for clinicians to be discerning in making this diagnosis given the aforementioned symptom overlap between depression and normative perinatal experiences. Although research consistently demonstrates that non-depressed women in the perinatal period endorse symptoms that are associated with depression (e.g., fatigue, insomnia, decreased concentration) [9], features that may differentiate depressed from non-depressed women during the postpartum period include irritability, insomnia, fatigue, and appetite loss [10]. This speaks to the importance of engaging in a thorough assessment with careful examination of when symptoms emerged, and not dismissing symptoms of depression as being normative for the postpartum period. In contrast, this also highlights the importance of making the diagnosis only when a depressed mood or anhedonia are present. In that way, if a patient endorses five criterion items without either of the first two symptoms, they may simply be experiencing a constellation of symptoms commonly associated with the physical and physiological challenges of the perinatal period. Notably, other medical conditions such as diabetes (T1, T2, and gestational) and thyroid disorders can trigger depressive symptoms during the perinatal period [10]. As such, symptoms of hypothyroidism and diabetes, along with work-up for any other underlying medical comorbidities (e.g., anemia, vitamin insufficiencies, etc.) should be assessed, with follow-up blood tests as needed.
Given the range of evidence-based medication and non-medication treatments available for perinatal depression, proper assessment, history taking, and diagnosis are imperative. Further, assessment should also include the investigation of co-occurring mental and physical health disorders, as well as psychosocial issues. Issues of race and ethnicity must also be assessed in contextualizing each patient’s presentation, given that many women in the USA experience significant racism, sexism, and other forms of discrimination that may impact their experience of motherhood, childbirth, and the medical system [11]. The widespread lack of access to basic resources must be considered when conceptualizing the patient’s symptoms and their etiology, and mental health providers may serve as an advocate and communication hub within the medical system for patients experiencing discrimination.
Screening Tools
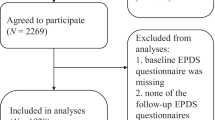
There are several evidence-based screening tools that are recommended for use with perinatal populations. The Edinburgh Postnatal Depression Scale (EPDS) is a 10-item self-report questionnaire used commonly in research and clinical settings [12]. It is designed to assess for symptoms of both depression and anxiety, given the comorbidity of these symptoms among women with PND. The EPDS’ strengths lie in the fact that it is (a) relatively short in duration, (b) quick to administer (it takes less than 5 minutes to complete, on average), and (c) widely translated, which allows for broader use than measures that are not validated in other languages [13]. Further, because it was designed with perinatal populations in mind, the measure has greater specificity than general depression measures (e.g., rather than assessing for disrupted sleep (which is normative in the perinatal period), it specifically assesses for sleep that has been disrupted as a result of mood symptoms).
The Patient Health Questionnaire 9 (PHQ-9) is another evidence-based screening measure that is validated for use with perinatal populations (though it was not designed specifically for perinatal populations) [14]. Although the PHQ-9 mirrors the EPDS in its brief nature, one key drawback of the PHQ-9 as compared to the EPDS is that it does not assess for anxiety symptoms [15]. Given the prevalence of co-morbid mood and anxiety symptoms among women in the perinatal period, this represents a meaningful limitation of the PHQ-9 in this context. For that reason, we recommend that the EPDS be used as the first line of assessment for perinatal mood and anxiety symptoms.
Psychiatric Comorbidity
From a psychological standpoint, PND is associated with various comorbid psychiatric conditions, both during the antepartum and postpartum periods. Most notably, anxiety disorders co-occur with PND in almost half of depressed women in the perinatal period, which far exceeds rates of such disorders in non-depressed pregnant women [16]. PND has also been associated with substance use disorders [17] and eating disorders [18]. Thus, in addition to assessing PND symptoms, clinicians should provide a comprehensive psychiatric assessment, including questions about anxiety, substance use, and eating disorder symptoms.
There are a range of behavioral consequences that mothers with PND endure that undermine their physical and mental health. In more acute cases, women with PND are at heightened risk of attempting suicide [19]. PND is also associated with increased maternal use of cigarettes, alcohol, and cocaine [17]. Further, pregnant women with depression tend to experience a diminished appetite and, as a result, gain less weight during pregnancy, which portends negative health outcomes for both mother and child [20]. PND has also been linked to deficiencies in other areas of self-care, such as sleep, exercise, and the likelihood of regularly attending obstetrical visits [21]. Broadly, these behavioral sequelae of depression are likely to contribute to the diminished self-esteem and impaired decision-making that women with PND tend to experience as compared to non-depressed women in the perinatal period [21, 22].
Sequelae
As covered in Chap. 5, PND can have a profound impact on mothers and families. The presence of maternal antepartum depression negatively impacts the health of the developing child, both in utero and beyond the gestational period. Depressed mothers also tend to be more self-focused [23] and less engaged with their newborns [24]. Further, interactions with their children are more likely to be characterized by hostility and unresponsiveness [25]. Concurrently, rates of child neglect and abuse are also greater in mothers with postpartum depression [26]. Depressed mothers attend fewer well-child exams within the first 2 years of their child’s life [27] and visit the emergency room with their infants significantly more [28]. These findings suggest that mothers with PPD experience cognitive and emotional deficits that make it difficult to attend to their children fully and consistently.
The presence of PND has also been shown to act as a chronic stressor on intimate relationships, resulting in elevated conflict and distress within relationships, as well as greater depressive symptomology in partners. Research on depression has consistently highlighted the bidirectional association between depressive symptomology and relationship distress [29]. Consistent with those findings, women with PPD report that they experience higher rates of marital conflict and feel less happy in their marriages than women who are not depressed during this time [30]. Their partners also experience worsened relational outcomes, in addition to heightened depressive symptomology, as evidenced by the strong correlation between maternal and paternal PPD [31]. These factors likely contribute to the higher rates of divorce documented in women with PND [32].
Summary
PND is common, often associated with anxiety, and causes significant distress for women, children, and families. Left untreated, PND is associated with high risk of suicidality, divorce, and negative outcomes for infants. Clinicians should assess not only mood and anxiety symptoms but also contextual factors that may impact illness risk and clinical presentation, including culture, race, living situation, family support, and trauma history. Patients should be provided with psychoeducation regarding their individual risk factors to help reduce stigma associated with PND and enable prevention and treatment planning.
References
Gaynes BN, Gavin NI, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. AHRQ Evid Rep Summ. 2005;119:1–8.
Leung BMY, Kaplan BJ. Perinatal depression: prevalence, risks, and the nutrition link—a review of the literature. J Am Diet Assoc. 2009;109(9):1566–75.
Dennis C-L, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323–31.
McCarthy M, McMahon C. Acceptance and experience of treatment for postnatal depression in a community mental health setting. Health Care Women Int. 2008;29(6):618–37.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Stuart-Parrigon K, Stuart S. Perinatal depression: an update and overview. Curr Psychiatry Rep. 2014;16(9):468.
O’Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):3–12.
O’Hara MW, Zekoski EM, Philipps LH, Wright EJ. Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol. 1990;99(1):3–15.
Melville JL, Gavin A, Guo Y, Fan M-Y, Katon WJ. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116(5):1064–70.
Holdt Somer SJ, Sinkey RG, Bryant AS. Epidemiology of racial/ethnic disparities in severe maternal morbidity and mortality. Semin Perinatol. 2017;41(5):258–65.
Cox JL, Holden JM, Sagvosky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–6.
Adouard F, Glangeaud-Freudenthal NMC, Golse B. Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of women with high-risk pregnancies in France. Arch Womens Ment Health. 2005;8(2):89–95.
Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22:1596–602.
Kroenke K, Spiltzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Le Strat Y, Dubertret C, Le Foll B. Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord. 2011;135(1–3):128–38.
Zuckerman B, Amaro H, Cabral H. Depressive symptoms during pregnancy: relationship to poor health behaviors. Am J Obstet Gynecol. 1989;160(5):1107–11.
Kessler RC, Nelson CB, Mcgonagle KA, Swartz M, Blazer DG. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry. 1996;14
Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77–87.
Paarlberg K, Vingerhoets A, Passchier J, Dekker G, Van Geijn H. Psychosocial factors and pregnancy outcome: a review with emphasis on methodological issues. J Psychosom Res. 1995;39(5):563–95.
Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, Koren G. Perinatal risks of untreated depression during pregnancy. Can J Psychiatr. 2004;49(11):726–35.
Hall LA, Kotch JB, Browne D, Raynes MK. Self-esteem as a mediator of the effects of stressors and social resources on depressive symptoms in postpartum mothers. Nurs Res. 1996;45(4):231–8.
Salmela-Aro K, Nurmi J-E, Saisto T, Halmesmäki E. Goal reconstruction and depressive symptoms during the transition to motherhood: evidence from two cross-lagged longitudinal studies. J Pers Soc Psychol. 2001;81(6):1144–59.
Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20(5):561–92.
Flykt M, Kanninen K, Sinkkonen J, Punamäki R-L. Maternal depression and dyadic interaction: the role of maternal attachment style. Inf Child Develop. 2010;19(5):530–50.
Cadzow SP, Armstrong KL, Fraser JA. Stressed parents with infants: reassessing physical abuse risk factors. Child Abuse Negl. 1999;23(9):845–53.
Gaffney KF, Kitsantas P, Brito A, Swamidoss CSS. Postpartum depression, infant feeding practices, and infant weight gain at six months of age. J Pediatr Health Care. 2014;28(1):43–50.
Zajicek-Farber ML. Postnatal depression and infant health practices among high-risk women. J Child Fam Stud. 2009;18(2):236–45.
Beach SRH, Katz J, Kim S, Brody GH. Prospective effects of marital satisfaction on depressive symptoms in established marriages: a dyadic model. J Soc Pers Relat. 2003;20(3):355–71.
Mamun AA, Clavarino AM, Najman JM, Williams GM, O’Callaghan MJ, Bor W. Maternal depression and the quality of marital relationship: a 14-year prospective study. J Women's Health. 2009;18(12):2023–31.
Dudley M, Roy K, Kelk N, Bernard D. Psychological correlates of depression in fathers and mothers in the first postnatal year. J Reprod Infant Psychol. 2001;19(3):187–202.
Holden K, Smock P. The economic costs of marital dissolution: why do women bear a disproportionate cost? Annu Rev Sociol. 1991;17(1):51–78.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cohen, M.J., Lundegard, L., Bernhardt, L., Schiller, C.E. (2021). Perinatal Patients with Symptoms of Depression. In: Cox, E. (eds) Women's Mood Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-71497-0_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-71497-0_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71496-3
Online ISBN: 978-3-030-71497-0
eBook Packages: MedicineMedicine (R0)