Abstract
This chapter is a collaborative effort from an oculoplastic surgeon and plastic surgeons. It considers the unique functional anatomy of the eyelids, globe, orbital contents, regional relationships and visual physiology. A variety of cancers occur in the periorbital region. The commonest are basal cell (BCC), squamous cell (SCC), sebaceous gland (SGC), Merkel cell carcinomas and cutaneous melanoma. These cancers can be locally invasive and spread by regional lymphovascular invasion, perineural invasion and in some cases life-threatening distant metastases. Immunocompromised patients can present with extensive cancer spread. Multidisciplinary care optimises the management of these tumours. When managing periocular cancers, the preservation of eyesight is an obligatory consideration. However, in some cases vision has to be sacrificed to achieve an optimal oncological result or to preserve life. Surgical margins of cancers invading the orbit are ill-defined, necessitating aggressive multimodality therapy. In surgical reconstruction, special attention must be given to preserving (1) ocular motility and (2) the protective function of the eyelids while retaining (3) an adequate palpebral aperture for vision. Preserving an eye’s tear film and an adequate tear outflow system is also vital for maintaining eyesight and a patient’s quality of life.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Orbital and eyelid tumours
- Multidisciplinary care
- Preservation of vision
- Reconstruction of major eyelid defects
-
Invasive cancers in the periorbital region have the potential to invade the orbit and cause loss of vision, distant disease and life-threatening complications.
-
Resection of cancers in the periorbital region needs to be complete, and reconstruction aimed to preserve normal eyelid and visual function.
-
Optimal management is achieved by a multidisciplinary team (MDT).
-
Depending on the clinical situation, retaining an eye’s vision can take priority over optimal disease control or vice versa.
1 Introduction
Extreme cancers of the periorbital region are rare but an even greater challenge that often requires the expertise of an MDT. Dr. Jack Mustardé (1916–2010) initially an ophthalmologist before retraining as a plastic surgeon in Britain during the Second World War emphasised the complex structures of the small but vital eyelids.
Eyelids are multilaminar but for surgical purposes are considered as bi-laminar structures composed of an anterior lamella of skin and orbicularis oculi muscle and a posterior lamella of tarsus lined by conjunctiva. Unique structures in the eyelids include the elevators of the upper eyelid. The upper eyelid contains Muller’s muscle and the levator aponeurosis arising from the levator palpebrae superioris. Analogous to the levator aponeurosis in the lower eyelid is the capsulopalpebral fascia, which lowers the eyelid on contraction of the inferior rectus muscle. The orbital septum is a fibrous, inelastic membrane that arises from orbital periosteum at the orbital rim (the arcus marginalis) and extends to the tarsal plates. Posterior to it are the orbital tissues. Highly organised connective tissue septa are found within the orbit. The periocular area also contains the lacrimal apparatus consisting of the lacrimal glands and the tear outflow system [1,2,3].
The periorbital region is a common site for facial cancers due to the high prevalence of ultraviolet light exposure. This varies with ethnicity, latitude and other environmental factors.
Extreme periocular facial cancers can occur due to patient-related factors including immunosuppression and hereditary conditions such as the basal cell naevus (Gorlin-Goltz) syndrome. Anatomical factors include periocular tumours invading the adjacent orbit and the lack of intraorbital barriers to tumour spread after the orbital septum is breached. There is potential for distant tumour spread by pagetoid, lymphovascular and perineural invasion. Another surgical challenge is the difficulty obtaining clear surgical margins in the orbit and around an eye if it is essential in a case to preserve the vision.
Multidisciplinary care is required in extreme periocular facial cancers due to the eye’s location in the orbit, its proximity to the nose, sinuses and intracranial cavity. This includes various surgical specialities: oculoplastic, plastic surgeons, head and neck and maxillofacial surgeons. The input of Mohs surgeons and neurosurgeons can also be required. Medical specialities in the multidisciplinary team include histopathologists, radiologists, radiation and medical oncologists, geriatricians, palliative care physicians, anaesthetists and maxillofacial prosthetic technicians.
Multimodality therapy, e.g. surgical excision coupled with adjunctive radiotherapy, is often required due to the limitations of surgery to obtain clear margins around the orbit. Preservation of vision is always a consideration but often needs to be balanced against treatment to achieve the best oncological result.
2 Management/Technique
2.1 Multidisciplinary Care
Complex and extreme facial cancer cases may be managed by an experienced surgeon, but ideally the forces of a multidisciplinary team (MDT) should be employed to offer the patient a wide range of experienced opinions and treatment options. With the aid of modern internet audiovisual systems, this can be organised virtually, but it is still mandatory that the patient has a specialist who is their nominated lead provider and with whom all communications and offers of management are coordinated.
Sir Archibald McIndoe (1900–1960) always maintained the principle that connectedness with your patient equals a confident and trusting patient. This holds true for not only the severely traumatised patient but also the patient with an extreme and perhaps even a life-threatening facial cancer.
Each member of the MDT arguably brings a prejudice to the table, based on their specialty of origin and varying years of surgical, oncological and anaesthetic experience. Egos and prejudices are inevitable and should be acknowledged and left out of the final decision-making process.
Young surgeons will gain much from being involved in MDT groups early in their career. Older surgeons with many clinical cases managed over their long careers will also find inspiration and education from this collective environment. The key is finding the balance, the best practice and at all times being patient-focussed with a bedrock of sound surgical and scientific principles.
Plastic surgeons and oculoplastic surgeons will inevitably bring different approaches to the management planning table. For example, the supratarsal skin bipedicled or unipedicled Tripier flap is a common choice for anterior lamella lower eyelid reconstruction (see Figs. 10 and 11) used by plastic surgeons since the 1950s. This flap is not commonly used by oculoplastic surgeons. Plastic surgeons are wary about using posterior lamellar tissue from the upper eyelid for lower eyelid reconstruction. On the other hand, oculoplastic surgeons are comfortable using the upper lid tarsal plate as donor material (see in Fig. 13 the Hughes tarsoconjunctival flap). Plastic surgeons would also probably rely less on Mohs micrographic excision techniques (predominantly the choice of dermatologists) or the laissez-faire philosophy of allowing an eyelid defect to heal by cicatrisation and secondary intention. Oculoplastic surgeons utilise these techniques routinely. Plastic surgeons are driven perhaps obsessively by the mantra of the late Sir William Manchester (1913–2001) who often stated ‘that in plastic surgery, perfection is only just good enough’ [4]. The key is for all multidisciplinary team members to work collaboratively, utilising its philosophy of inclusiveness and diversity, to achieve the best result for the patient.
The important steps for either the individual surgeon or MDT of which he or she is a member are tumour staging and determining a treatment plan for each patient considered.
2.2 Staging
According to Sir Harold Gillies’ second fundamental principle ‘diagnose before you treat’, the first step is to obtain a diagnosis with an incisional biopsy. Special cases encountered in the periorbital region are sebaceous gland carcinomas and cutaneous melanomas. In the former, it is mandatory to do a full-thickness (wedge resection) eyelid biopsy to detect pagetoid intraepithelial invasion. Conjunctival biopsies are also used by many surgeons to detect pagetoid conjunctival epithelial invasion in otherwise normal-appearing conjunctival tissue [5, 6]. Suspected nodular melanomas require an excision biopsy to determine the Breslow thickness. Further treatment will then include wide local excision and staging.
Once the diagnosis is established and to detect loco-regional and distant metastases, the management may include a sentinel lymph node biopsy and radiological assessment including computed tomography scanning of the head, neck and beyond. Magnetic resonance imaging (MRI) is used to image soft tissue disease and detect perineural invasion. Positron emission computed tomography (PET CT) also has a role in staging of periorbital tumours. The expertise and anatomical insights of an experienced head and neck radiologist are pivotal in the diagnosis and surgical planning, which are illustrated in Chap. 4 “Applied Facial Anatomy”. Disease staging is then classified with the TMN staging system [7].
Based on a discussion with an MDT, management options including surgery, reconstruction, radiotherapy, immunotherapy, chemotherapy and palliation can then be presented to the patient and their family. A clear goal must be established—whether treatment is for cure or palliation.
3 Treatment
3.1 Margin Control in Tumour Excision
In facial basal cell carcinomas, excision with a 4 mm margin has been shown to have up to a 95% cure rate [8]. However other authors reported that in 54% of primary tumours removed with a 3–4 mm margin of normal-appearing eyelid tissue, frozen sections demonstrated tumour in at least 1 margin [9]. In a study using frozen section margin control in eyelid basal cell carcinoma, after 5 years a 1.8% recurrence rate was reported [10].
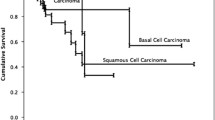
Mohs micrographic surgery (MMS) can be employed to excise non-melanoma tumours in the periocular region. Mohs reported 5-year cure rates of 99% in 1773 cases of basal cell carcinoma and of 98.1% in 213 cases of squamous cell carcinoma of the eyelids [11]. In a large prospective, multicentre Australian case series, the 5-year basal cell carcinoma recurrence rates were 1.4% for primary tumours and 4% for recurrent tumours [12]. For squamous cell carcinomas, the corresponding 5-year recurrence rates were 2.6% and 5.9% [13].
In the periocular region, to minimise disruption to the eye and the vision, a key consideration in tumour management is to conserve as much as possible of the conjunctiva, eyelid tissue, palpebral ligaments and the lacrimal outflow system. Narrow margins are possible with MMS and therefore it maximises tissue conservation. Plastic surgeons would take an alternative view, based on the wide range of reconstructive options they can offer. Therefore, for plastic surgeons, the size of the periorbital defect is not a concern.
At the medial canthus, the anatomical barrier to orbital invasion, the orbital septum, is deficient. If tumours are not completely excised, orbital invasion can result. The high cure rate from MMS means it is strongly indicated for excising medial canthal tumours. Plastic surgeons would favour wider surgical margins and immediate reconstruction with like tissue, instead of MMS.
The cost of MMS, compared with other techniques of margin control, has been cited as a significant limitation for its use. When recurrences are taken into account, the cost is comparable to multiple surgical procedures over many years [14]. The cost can potentially be reduced when Mohs surgeons are co-located with other members of the multidisciplinary team. In common with other methods of margin control, MMS cannot provide margin control for tumours that have invaded orbital fat.
In response to the historical limited availability of MMS services, several authors have proposed alternative margin control techniques [15, 16].
A key advantage of MMS is the separation of tumour excision and eyelid reconstruction. The Mohs surgeon will remove periocular tissues containing tumour without needing to be concerned about how the eyelid will be reconstructed. Similarly, the reconstructive surgeon can proceed without concerns about tumour clearance. When a single surgeon performs tumour excision and then reconstruction, the oncological result can be compromised. The periocular region is the ideal location for Mohs surgeons and reconstructive surgeons to collaborate and provide optimal oncological and reconstructive outcomes.
3.2 Surgical Treatment
Surgical treatment is multidisciplinary with the principles of CLEAR and DRAPE (Complete Local Excision + Aesthetic Reconstruction/Delayed Reconstruction After Pathology Examination). The concept of DRAPE was coined by Professor Felix Behan FRACS, in his pioneering work describing the anatomy, physiology and clinical application of the keystone perforator island loco-regional flap [17]. The concept of CLEAR was an original idea by Klaassen when compiling a book with Dr. Earle Brown, to aid plastic surgical trainees preparing for their final professional exams. It was a conceptual framework around which to organise thought processes in considering any common skin cancer case, in response to the Mohs concept advocated by dermatologists, and it dovetails conveniently with the DRAPE concept. No matter where the surgeon is practising, these and other fundamental principles will give a clear and reliable guideline to make the best decisions for the patient [18].
Special considerations in the management of periocular facial tumours are below.
3.2.1 Vision
In the management of periocular tumours, the eye and vision are crucial considerations. An ophthalmic assessment is required to assess the vision in both eyes. If due to treatment of a periocular tumour, the vision in an eye is likely to be compromised, it is important to assess the vision in the contralateral eye. To maximise visual function, the contralateral eye’s vision may need to be maximised with spectacles or surgery (e.g. cataract surgery) prior to treatment of the periocular tumour. If one eye must be sacrificed to optimise the oncological result, an ophthalmologist can advise on the loss of binocularity. This is to enable safe mobility, returning to driving and other activities such as operating machinery.
3.2.2 Structural Considerations
To maintain vision, it is important to note the role of the periocular tissues in maintaining a healthy ocular surface, the eyelids’ role in preventing mechanical damage and the lacrimal apparatus’ role in tear drainage.
3.2.3 Tears
The ocular surface must be bathed in tears. The tear film is a multilaminar liquid comprised of mucin, aqueous and an overlying oily film that retards evaporation. Aqueous tears are secreted by the lacrimal gland and accessory lacrimal glands scattered through the conjunctiva. Mucin-secreting glands are located in the conjunctival epithelium. The eyelid meibomian glands in the tarsal plates secrete the tear’s oily component. Tears deliver dissolved oxygen to the corneal epithelium. Tears have a protective function to dilute noxious fluids and wash away foreign bodies. If the tear film is compromised, adverse effects range from chronic ocular irritation, drying of the ocular surface with secondary reflex tear hypersecretion and epiphora, reduced vision due to glare, loss of contrast and exposure keratitis. In severe cases corneal ulceration, scarring and permanent vision loss can occur.
In some cases of facial palsy (e.g. due to cerebellopontine angle syndrome), there is concomitant reduced corneal sensation. Such cases of neuropathic, dry corneas have a high risk of decompensation leading to corneal perforation, infection and irretrievable loss of vision.
3.2.4 Blinking
Passive blinking from frequent reflex contraction of the orbicularis oculi spreads the tear film across the ocular surface. Blinking is the key component of the ‘lacrimal pump’ that forces tears medially to the lacrimal puncta and lacrimal outflow system. Altered passive blinking frequency or amplitude can be caused by eyelid scarring or ill-suited reconstructive techniques. The resultant lagophthalmos (incomplete eye closure) and ocular surface drying cause chronic irritation, corneal scarring and possible loss of vision. The blink reflex is crucial for protective rapid eye closure and the ‘sweeping’ of foreign bodies from the corneal surface.
3.2.5 Eyelid Posture
Upper eyelid ptosis, causing visual obstruction, can occur in upper eyelid reconstruction if a bulky graft or flap is used or the medial or lateral ends of the eyelid are pulled inferiorly. A ptotic eyelid also affects vision by distorting the cornea and inducing astigmatism.
After lower lid reconstruction, a common complication is ectropion. It results from cicatrisation of the eyelid’s anterior lamella. If the posterior lamella is also involved, lower eyelid retraction results. Mechanical ectropion can also occur due to a bulky lower lid reconstruction that distracts the eyelid away from the ocular surface. Ectropion and lower eyelid retraction result in varying degrees of corneal exposure and lagophthalmos. The resulting evaporative dry eye causes chronic ocular irritation, mucus over-secretion, exposure keratitis and secondary hypersecretion of tears. Compromised blinking disrupts the lacrimal pump. Stasis of tears occurs in the trough formed between the ocular surface and an ectropic eyelid. This causes chronic conjunctivitis and epiphora.
The medial palpebral ligament consists of an anterior and a posterior limb. It is the latter which inserts into the posterior lacrimal crest to pull the lid posteriorly so that the lower lid sits against the anterior surface of the eye. (See in Complication Management—Ectropion.)
If the lid margin is distorted, the eyelashes can become misdirected (trichiasis) and abrade the ocular surface, causing chronic irritation, corneal scarring and loss of vision.
In cases of posterior lamellar cicatrisation and loss of the lid margin mucocutaneous junction, keratinised skin and vellus hairs can also abrade the eye. In addition, loss of the protective function of the lashes can occur, further compromising the blink reflex.
3.2.6 The Periorbital Tissues’ Mechanical Protective Function
The periocular tissues have a protective mechanical function for the eye. An intact orbital rim protects the eye from direct mechanical trauma. The eyelids are the eyes’ most important protective barrier. Bell’s phenomenon consists of reflex upwards eye rotation with reflex blinking. It protects the cornea from mechanical trauma. If it is absent (10% of otherwise healthy persons) or inverted, an eye with compromised blinking is at greater risk of corneal damage and visual loss.
3.2.7 Tear Drainage
If tears are not able to drain from the eye via the tear outflow system, epiphora results. Depending on the site of the obstruction, chronic conjunctivitis can also occur due to stasis of tears in the conjunctival and/or lacrimal sac. Significant visual disability can result and have a significant adverse effect on a patient’s quality of life. If the nasolacrimal duct is obstructed, stasis of tears in the lacrimal sac occurs. Epiphora occurs and in some cases bacterial colonisation, causes chronic or acute dacryocystitis. In severe cases, abscess formation and facial cellulitis can occur. In extreme cases, or if there is delayed treatment, orbital cellulitis and even cavernous sinus thrombosis can occur. Nasolacrimal duct obstruction can be corrected by a dacryocystorhinostomy.
3.2.8 Orbital Invasion by Facial Tumours
Facial skin tumours invade the orbit by direct spread through the orbital septum or perineural invasion. In the post-septal orbit, there are no anatomical barriers to tumour spread. Due to the ultrastructure of the orbital fat, it is not possible to obtain histologically clear margins.
Furthermore, it is not generally possible to remove a significant amount of orbital soft tissue without damaging the extraocular muscles, the intermuscular septa and intraorbital nerves and blood vessels. Invariably the result is altered vision and/or disabling diplopia. Therefore, the standard approach for addressing intraorbital spread of facial skin cancers is orbital exenteration.
Sacrificing a seeing eye is never an easy decision but must sometimes be considered in extreme periorbital cancer cases. Exenteration removes, within the periorbital envelope, the anterior two thirds of the orbital tissues and the eye. Piecemeal removal of the posterior orbital soft tissues is then performed. Adjunctive radiotherapy is used postoperatively to treat microscopic disease.
3.2.9 Perineural Invasion
Perineural invasion centripetally along the infraorbital and supraorbital nerves is not uncommonly encountered in periorbital squamous cell carcinomas. It can also occur rarely with basal cell carcinomas. Perineural invasion is often heralded by abnormal skin sensations along the distribution of the ophthalmic and maxillary branches of the trigeminal nerve.
3.2.10 Lymphovascular Invasion and Tumour Staging
Anatomically the medial half of the upper and lower eyelids drain to the submandibular nodes. The lateral half of the lids drain to the preauricular nodes. Sentinel lymph node biopsy has been advocated as a staging method in eyelid melanoma, SCC, SGC and Merkel cell carcinomas. The exact correlation between sentinel lymph node biopsy, tumour recurrence rates and patient survival is not yet known [19].
4 Indications
4.1 Medial Canthal Lesions
4.1.1 Basal Cell Carcinoma of the Medial Canthus
The medial canthal region is one of the commonest sites for BCC in the oculoplastic surgeon’s/plastic surgeon’s clinical practice. It is most important to treat these early and get good clearance. Incomplete excision can lead to recurrence and invasion down the medial side of the bony orbit. This anatomical region with its concave contour acts like a sun trap, and BCCs vary from small to moderate to extensive cancers (Fig. 1). Local flaps from the glabellar region or full-thickness skin grafts are a simple solution for reconstruction.
The glabellar local flap is a variant of the rhomboid flap. It brings thicker forehead and upper lateral nasal skin into the surgical defect. It is an easy flap to raise and transpose into the medial canthal defect after wide excision of the tumour. This surgery is commonly performed under local anaesthetic with or without intravenous sedation (Figs. 2 and 3). Sometimes secondary thinning of the local flap contour is required.
(a and b) 1-year appearance of glabellar local flap for nodular BCC left medial canthal region in an 85-year-old man. (c and d) 5-year appearance of a full-thickness graft (supraclavicular donor site) in a 85-year-old man, with what was reported as an SCC in situ. He has also had a forehead flap reconstruction of his nasal dorsum for an SCC, 3 years previously
4.1.2 The Rhomboid Flap in Medial Canthal Reconstruction
The rhomboid flap, usually performed under local anaesthetic, is a rapid and effective flap for reconstructing medial canthal defects. Suturing the cut medial lower lid edge to the lateral edge of the rhomboid flap exerts an upwards traction on the eyelid’s anterior lamella. This assists in preventing ectropion (Fig. 4) [20].
(a–c) An 82-year-old man underwent Mohs micrographic surgery to excise a recurrent medial canthal BCC. The cut medial end of the tarsal plate was reattached to the medial palpebral ligament remnants. The anterior lamellar defect was repaired with a rhomboid flap from the bridge of the nose (outline of flap in blue). Figure 4c shows the result after 3 weeks
4.1.3 Full-Thickness Skin Grafts for Medial Canthal Reconstruction (Fig. 5)
(a–d) In this 74-year-old man, Mohs micrographic surgery was used to excise a recurrent BCC involving the medial canthus, upper tear outflow system and the medial ends of the upper and lower eyelids. A medial periosteal flap was used to reattach the cut medial ends of the eyelids. A full-thickness skin graft from the upper inner arm was used to cover the skin defect. Tethering of the medial end of the repaired upper eyelid caused a visually significant ptosis. This was corrected with a medial canthoplasty to release the medial upper lid followed by a Muller’s muscle resection to correct the residual ptosis
4.1.4 The Pericranial Flap in Medial Canthal Reconstruction (Fig. 6)
(a–d) A 76-year-old woman with a defect of the medial canthus, side wall of the nose (with periosteum excised) and medial lower eyelid, after excision of an SCC using Mohs micrographic surgery. The defect of the periosteum at the medial canthus was covered by a forehead pericranial flap. This provides vascularised tissue onto which a skin graft can be placed. A transverse scalp incision just below the hairline provided access to form a 3-cm-wide pericranial flap. This was hinged above the supraorbital neurovascular bundle. It was sutured inferiorly to the cut edge of the nasal periosteum. If required, the cut medial ends of the eyelids can be secured to the pericranial flap. A full-thickness skin graft was placed on to the pericranial flap. This is a less bulky alternative to a median forehead flap
4.1.5 Squamous Cell Carcinoma of the Medial Canthus with Orbital Invasion
This 70-year-old man (Fig. 7) with chronic lymphocytic leukaemia was referred as an urgent case from a district hospital, with a neglected and significantly ulcerated SCC of his nasal bridge and left medial canthal regions. The latter appeared to be invading his left medial orbit and was highly vascular. During resection, the tumour was close to the left nasoethmoid bones, and a retrobulbar haematoma occurred in the left orbit, intra-operatively. This was decompressed immediately and his left eye vision was saved. A month later the large right paramedian forehead flap was divided and inset. Further extensive skin cancers of his temples and cheeks bilaterally were also excised (Fig. 7a–d).
His progress after this was predictably downhill. Within a year, he developed metastatic SCC in his left parotid gland as well as recurrent SCC of his right cheek, which invaded his right maxilla and right orbital floor. Despite further radical resection of his right hemiface and free flap reconstruction followed by adjuvant radiation therapy, a year later he became demoralised, withdrew from treatment and died in a palliative care facility just over 2 years after initial presentation. (We acknowledge the contribution of Dr. Nita Ling FRACS from Townsville Hospital, North Queensland, for his follow-up care.)
4.1.6 Lower Eyelid Reconstruction
Sir William Manchester (1913–2001), who founded the Middlemore Plastic Surgical Unit in Auckland in late 1950 after training with Gillies, McIndoe and Mowlem during the 1941–1942 WWII period, was a skilled surgeon in periorbital reconstruction. His influence on the two plastic surgeon authors (MFK and EB) was considerable, and we still follow his fundamental principles [21]. Figure 8, showing an infiltrating extensive BCC of the left medial canthal region and medial lower eyelid, illustrates the use of a chondro-mucosal septal graft for the posterior lamella and a staged right paramedian forehead flap for the anterior lamella. These images were from his teaching slide collection which cover the 1950s–1970s.
4.1.7 The Lacrimal Outflow System
To prevent epiphora, lacrimal procedures performed at the time of primary surgery are more effective than later secondary procedures. Excision of the punctum or partial excision of a canaliculus can be treated by marsupialisation of the remaining vertical or horizontal part of the canaliculus. Various lacrimal stents can be used to prevent canalicular obstruction if the canalicular wall is breached or a segment of canaliculus is excised. If the canaliculi are unable to be repaired, or the lacrimal sac is partially excised, a glass (Lester Jones) tube can be inserted as a secondary procedure by an oculoplastic surgeon. However, this may not be required if the lid posture approximates the normal lid posture and ocular exposure is minimised, thus reducing drying of the ocular surface and secondary hypersecretion of tears (Figs. 9, 10, 11, 12, and 13).
Treatment of breaches of the canalicular wall or excisions of a segment of the horizontal part of the canaliculus. These are treated by inserting a self-retaining stent and the pericanalicular tissues are apposed (the ‘one-stitch’ canalicular repair [22])
One of the authors (EB) has had personal experience of a BCC infiltrating his lower eyelid: Dr. Earle Brown’s right lower lid BCC, wide excision and repair by Glenn Bartlett FRACS (Fig. 14).
(a–f) An infiltrating BCC of the right lower eyelid and involving the lower lacrimal punctum, widely excised and repaired with a bipedicled upper eyelid Tripier local flap for anterior lamella and a septal chondro-mucosal graft for posterior lamella. Images show the eyelid margin tumour, early and later postoperative results. There was no epiphora at long-term follow-up
The Tripier bipedicled upper eyelid local flap is a staged reconstruction which was championed by Sir William Manchester. The case illustrated in Fig. 15 is one of his cases from over 60 years ago and emphasises the precision and perfection required for reconstruction of the lower eyelid region [23]. Interestingly, Manchester did not favour the supraorbital Fricke local flap because of its bulkiness.
The patient in Fig. 16 is a 72-year-old woman from a high UV light region and a long history of multiple skin cancers including malignant melanoma and BCC. She presented with a rapidly growing nodular BCC close to her left lower eyelid margin. A full-thickness excision with 4 mm margins was performed under IV sedation and local anaesthetic. The eyelid defect was immediately reconstructed with a lateral cantholysis and a McGregor lateral temporal local flap incorporating a Z-plasty. The healed result is shown at 3 months post-surgery.
For defects of the lower eyelid after excision of lower eyelid lesions, alternative techniques commonly used by oculoplastic surgeons are direct closure (which can be facilitated by lateral canthotomy/cantholysis), the Hughes tarsoconjunctival flap (see Fig. 17), composite grafts and laissez-faire (see Fig. 23).
(a–i) Mohs micrographic surgery was used to excise a recurrent BCC in this 76-year-old woman. The defect involved the whole lower eyelid. The posterior lamella of the lid was reconstructed using medial and lateral periosteal flaps, and a central tarsoconjunctival flap 15 mm in horizontal extent (the Maximal Hughes procedure [24]). The tarsoconjunctival flap is harvested from the superior part of the upper lid tarsal plate. The inferior 4 mm of the tarsal plate is left intact. The anterior lamella was reconstructed with a skin/muscle advancement flap. The division of the tarsoconjunctival flap was performed after 2 weeks. The new lower eyelid margin is left to granulate
4.1.8 The Hughes Tarsoconjunctival Flap in Lower Eyelid Reconstruction
A variety of tissues can be used to replace an eyelid’s posterior lamella. Oculoplastic surgeons commonly use the Hughes tarsoconjunctival flap [25]. This flap can be performed under local anaesthetic alone or with sedation. It uses the ipsilateral upper eyelid, and a graft does not need to be harvested from a remote site. Alternative remote site free grafts are hard palate, conchal cartilage or nasal septal cartilage. The former’s epithelial surface will not abrade the cornea. The latter two grafts must be lined posteriorly by residual conjunctiva. The main disadvantage of the Hughes flap is that the eye is sutured closed. Another procedure is needed to divide the flap and reopen the eye. However, the second stage can be performed from as little as 7 days after the initial surgery [26]. This flap cannot be used if the operative eye is the patient’s only seeing eye.
If the posterior lamellar graft has an inherent vascular supply, as in the Hughes flap, the anterior lamella can be replaced by a full-thickness skin graft. Skin/muscle advancement flaps from residual lower eyelid tissue are also commonly used. If the posterior lamellar graft is a free graft, a pedicle flap must be used, e.g. a skin/muscle advancement flap from the lower eyelid, a Fricke flap, forehead flap or a cheek rotation flap (Fig. 17).
4.1.9 Periosteal Flaps in Eyelid Reconstruction
Periosteal flaps are used to anchor the medial or lateral ends of the lower eyelid if the medial or lateral palpebral ligaments have been excised. They are constructed from the medial and lateral orbital rim periosteum. Access to the periosteum is through a defect or horizontal incisions at the medial and lateral canthi. To minimise ocular exposure, the medial and lateral contour of the eyelids is approximated by hinging the flaps as posterior as possible at the orbital rim. The medial periosteal flap is hinged at the anterior lacrimal crest, and the lateral periosteal flap is hinged posterior to the arcus marginalis.
A periosteal flap can be horizontally divided to provide anchor points for both the upper and lower eyelids. An upper eyelid periosteal flap must be long enough to allow for upper eyelid excursion and to avoid inducing ptosis.
4.1.10 The Lateral Periosteal Flap (Fig. 18)
4.1.11 The Medial Periosteal Flap (Fig. 19)
4.1.12 The Mustardé Cheek Rotation Flap in Lower Eyelid Reconstruction (Fig. 20)
The cheek rotation flap [1] as described by Mustardé transposes close-matching, adjacent lower lid and periocular skin into lower eyelid defects. It can fill a large anterior lamellar eyelid defect usually in the lateral two-third of the lower eyelid. Disadvantages, due to the extensive cheek dissection, are a risk of damage to the branches of the facial nerve to the orbicularis oculi muscle, haematomas and induced lower eyelid ectropion. To reduce the risk of postoperative lower eyelid ectropion, the superior edge of the flap is sutured to the periosteum at the lateral orbital rim. This results in an upwards vector of tension on the medial end of the flap (Figs. 21 and 22).
(a–c) A 72-year-old man with severe actinic skin damage and an extensive SCC involving the side of the nose. This was excised using Mohs micrographic surgery. A forehead pericranial flap was used to cover the exposed bone on the sidewall of the nose. The medial cut end of the lower eyelid tarsal plate was then attached to the periosteal flap. The eyelid was pulled superiorly and medially to prevent postoperative lower lid ectropion. A glabellar flap and a cheek rotation flap were used to cover the medial canthus, side of the nose and lower lid anterior lamella
(a–d) A 78-year-old woman with a Merkel cell carcinoma of the left lower eyelid. This was excised with 6 mm margins. Complete excision was confirmed with conventional tissue processing & histological examination. A Hughes tarsoconjunctival flap was used to reconstruct the posterior lamella. A Mustardé cheek rotation flap was used to reconstruct the anterior lamella
(a–d) An infiltrating SCC in an 82-year-old man was excised using Mohs micrographic surgery. A lateral periosteal flap was used to re-attach the detached upper and lower eyelids. The anterior lamella was reconstructed with a Mustardé cheek rotation flap. Due to the severely sun-damaged, taut skin, part of the secondary defect from the flap was covered with a split-thickness skin graft
4.1.13 Laissez-Faire in Eyelid Reconstruction
A “Less is More” approach for periocular defects can be utilised, and it is often welcomed by patients. The lower eyelid and medial canthus are particularly suitable sites. It can be used when surgery would be hazardous or contraindicated, e.g. patients unsuitable for anaesthesia and extensive surgery due to significant cognitive impairment or systemic health conditions. It can be used in monocular patients if the operative eye is their only seeing eye and reconstructive surgery can temporarily or permanently disrupt the vision. Disadvantages of laissez-faire, depending on the amount of eyelid involved, include worsening of pre-existing ectropion, eye exposure, irritation, redness, inflammation, discharge and watering. Secondary surgery can be required, e.g. to address hypertrophic scars or lid margin notching. It should be noted that these complications can also occur after eyelid reconstructive surgery.
4.1.13.1 Laissez-Faire for Full-Thickness Eyelid Margin Defects (Fig. 23)
4.1.13.2 Laissez-Faire for Medial Canthal Defects (Fig. 24)
(a–d) A 65-year-old man with right upper eyelid sebaceous gland carcinoma (SGC). This was excised with 6 mm margins. Conventional tissue processing and histological examination of the specimen demonstrated the lesion had been completely excised. Reconstruction was undertaken 7 days after excision. In the upper eyelid, posterior slips of the medial palpebral ligament were intact. Eyelid closure was not affected. In the lower lid, the canaliculus and medial palpebral ligament were intact and did not require repair. The skin and canthal conjunctival defects healed satisfactorily by granulation
4.1.13.3 Laissez-Faire for Large Lower Eyelid Defects (Fig. 25)
Loss of an upper eyelid inevitably leads to loss of vision since the upper eyelid has an essential role in maintaining corneal hydration. However, an eye can retain satisfactory visual function after loss of an entire lower eyelid.
(a–d) A multiply recurrent lower lid BCC affecting the whole lower eyelid in an 82-year-old man. At the time of Mohs micrographic surgery, tumour was found to be invading the anterior orbital fat. Due to the risk of worsening his pre-existing cognitive impairment, an anaesthetic was considered to be too hazardous so further tumour excision was not undertaken and the eyelid was left to heal by laissez-faire. Adjunctive radiotherapy was performed after 6 weeks. The vision remained at 6/9 unaided. Exposure and inferior corneal drying were managed conservatively with ocular lubricants
5 Large Upper Eyelid Defects
5.1 Upper Eyelid Reconstruction with the Mustardé Lower Lid Flap
This eyelid-sharing technique described by Mustardé [1] transposes a full-thickness lower eyelid pedicle flap into a moderate-sized upper eyelid defect. After several weeks, the pedicle is divided in a second stage. Advantages are that it is a single flap of identical eyelid tissue (lined by conjunctiva). It transplants into the defect a normal upper eyelid margin complete with eyelashes. A disadvantage is the temporary closure of the eye and the requirement for a second surgical stage. If the upper eyelid defect involves the medial or lateral commissures, eyelid distortion can occur, and corrective secondary surgery may be required (Figs. 26 and 27).
(a–f) A 77-year-old man with left upper eyelid SGC. The tumour was excised with a 6 mm margin. Conjunctival map biopsies were also performed. Conventional tissue processing and histological examination were performed. Pagetoid intraepithelial invasion was present at the lateral eyelid wound margin, a further excision biopsy was performed and further histological examination was undertaken. No further disease was identified. The conjunctival map biopsies did not demonstrate any disease. The wound was repaired using a Mustardé lower eyelid flap. Three weeks later the eyelids were opened and the lid margins reformed
5.2 Subtotal Upper Eyelid Reconstruction with a Mustardé Staged Lower Eyelid Flap
This 54-year-old woman (Fig. 28) presented with a biopsy-proven SGC of her right upper eyelid. This had arisen as a crusty lesion on her right upper eyelid over the previous 18 months and had not responded to cryotherapy from her family doctor. The initial wedge excision assumed that the tumour was a BCC. Under general anaesthetic the previous scar was widely excised (10 mm) full thickness, and the margins checked with frozen section biopsies. This confirmed no tumour present, so stage 1 subtotal upper eyelid reconstruction proceeded according to the technique of Mustardé [1]. A laterally based full-thickness lower eyelid flap was turned 180° and cephalad in a caterpillar fashion. This was inset into the lateral upper eyelid defect. The levator palpebrae muscle and aponeurosis were identified and attached laterally to the tarso-muscular layer of the lower eyelid flap. The conjunctival lining was mobilised and sutured to protect the right cornea. Protective eye dressings were applied (Fig. 28a–c).
Two weeks later, the second stage was completed again under general anaesthetic with division and inset of the lower eyelid flap and formal reconstruction of the right lower eyelid donor site. This was achieved with a Mustardé rotation cheek flap. Under the Mustardé flap, a nasal septal chondro-mucosal free graft provided the posterior lamella. The levator muscle was sutured to the orbicularis oculi muscle layer of the lower eyelid flap (Fig. 28d–f). The 2-year result is shown with a close-up of her right upper lid reconstruction at 2 years post-surgery and a long-term photograph kindly supplied by her daughter at 20 years post-surgery (Fig. 28g–j).
This patient survived with no recurrence until she was 75 years old, when she died of natural causes.
5.3 The Cutler Beard Procedure for Upper Eyelid Reconstruction
This is a full-thickness cutaneo-conjunctival lower eyelid advancement flap suitable for elderly patients with lax lower eyelid tissues (Fig. 29).
(a–h) An 85-year-old woman with a left upper eyelid Merkel cell carcinoma. The tumour was removed with a 6 mm margin. Complete tumour excision was confirmed with conventional tissue processing & histological examination. A Cutler-Beard procedure was performed. A lower eyelid conjunctival pedicle and a pedicle of lower eyelid anterior lamella were pulled superiorly and sutured to the cut ends of the corresponding layers in the upper eyelid defect. A shaped conchal cartilage graft was placed between these two layers. A second stage opening of the eyelids was performed after 1 month. A wedge resection was performed to correct the resulting lower eyelid laxity
The advantage of this procedure is that it can fill large defects of the upper eyelid. It can be combined with periosteal flaps if the medial and lateral palpebral ligament upper eyelid attachments have been excised. Disadvantages include a period of eye closure until the second stage is performed, having to use a graft from a remote site (a free conchal or other cartilaginous graft) and secondary lower eyelid laxity. Lower eyelid laxity is corrected with a lower lid wedge resection at the time of the second stage of surgery. Conjunctival sutures can cause corneal damage if not adequately buried. Postoperative lagophthalmos can occur, resulting in chronic ocular surface dryness, irritation and altered vision.
5.4 The Upper Eyelid Composite Graft in Upper Eyelid Reconstruction
This utilises a free composite graft from the contralateral upper lid (Fig. 30).
(a–f) A 73-year-old man with a central right upper eyelid defect after excision of a BCC. This was reconstructed with a full-thickness eyelid wedge graft harvested from the contralateral upper eyelid. This technique can be used for central upper lid defects involving up to approximately 1/3–1/2 of the eyelid
6 Lateral Canthal Lesions (Fig. 31)
(a–e) An 80-year-old woman with a recurrent BCC of the lower eyelid and lateral canthus. The defect after Mohs micrographic surgery involved the whole lower eyelid margin, the lateral canthus and the lateral one-third of the upper eyelid. To prevent a postoperative ectropion, the lower eyelid was drawn upwards and laterally by suturing the lower eyelid septal remnants to a periosteal flap. The cut end of the upper eyelid tarsal plate was sutured to the upper limb of the periosteal flap. The eyelid margins were left to granulate. The lateral skin wound was then closed directly. Photo e) shows the result after 3 months
6.1 Basal Cell Carcinoma of the Lateral Canthus
This 91-year-old man presented with a 2 × 3 cm infiltrating nodular BCC of his right lateral canthus, of at least 12 months duration. Under local anaesthetic with intravenous sedation, a wide excision was performed including the lateral 25% of the lower lid. A lateral canthoplasty was performed with mobilisation of a conjunctival local flap, and the large lateral canthal defect reconstructed with a Mustardé rotation local flap from the right lateral cheek region (Fig. 32). The result is shown at 3 months post-surgery.
6.2 Squamous Cell Carcinoma of the Lateral Canthus
This 70-year-old man (Fig. 33) presented with a 2.5-mm-thick (Clark’s level III), moderately well-differentiated SCC of his right lateral canthus/lower eyelid region, which had an expansile and exophytic growth pattern. There was a nearby 4.1-mm-thick nodular BCC of his right lateral eyebrow region. Clinical and histological images are below. He was taking warfarin for a previous mesenteric vein thrombosis which increased the peri-operative risk of bleeding and haematoma. A wide excision of the SCC was performed under local anaesthetic with intravenous sedation. The defect was triangulated caudally, and the deep margin included a cuff of lateral orbicularis oculi muscle. The repair was achieved with a Mustardé lateral cheek rotation flap, which incorporated the excision defect for the cephalad BCC. Auersvald haemostatic net sutures were placed through the centre of the rotation local flap to close the dead space and prevent haematoma formation. These were removed at day 3 (Fig. 33b) and the final result is shown at 3 months.
(a–d) Invasive SCC of the right lateral canthus in a 70-year-old man, with nearby BCC. Mustardé principle of immediate reconstruction again. Result shown after 3 months. (e and f) Moderately well-differentiated SCC low-power and medium-power photo-micrographs. (g and h) Nodular BCC low-power and medium-power photo-micrographs (with thanks to Dr. Ben Tallon FRACP)
This 59-year-old man (Fig. 34) presented with a large fungating SCC of his left lateral canthal/lower eyelid region. There was an additional infiltrating BCC on the dorsum of his nose. This case was being considered by a junior colleague, and the lead author offered his assistance. The original plan had been for a wide excision and Mustardé upper temporal rotation flap with a skin graft for the dorsal nasal defect. Reconstruction with a temporary Fricke supraorbital transposition flap was undertaken initially while awaiting a CT scan to assess the left lateral orbit. The CT scan showed no obvious sign of left intraorbital tumour spread. A glabellar local flap was used to repair the dorsal nasal defect. The early result is shown at 1 week post-surgery (Fig. 34a–f).
6.3 Uncommon Orbital Invasion at the Lateral Canthus by a Desmoplastic SCC
Orbital invasion at the lateral canthus is uncommon yet may occur with aggressive variants of squamous cell carcinoma. Figure 35 shows an 84-year-old retired farmer with an aggressive desmoplastic SCC of the right temple. Two years prior to presentation, the SCC had been excised and treated with adjuvant radiotherapy. Mohs micrographic surgery was used to excise the cutaneous and subcutaneous tumour. Orbital fat infiltration was identified but the patient declined orbital exenteration. The defect was covered with a large scalp rotation flap. Since he had previously had radiotherapy, further adjunctive radiotherapy could not be used. An extensive recurrence occurred 11 months later. Salvage surgery was undertaken: orbital exenteration, periorbital resection, parotidectomy and neck dissection. One year later a further orbital rim recurrence occurred and was treated with palliative radiotherapy. This highly aggressive subtype of squamous cell carcinoma produces dense collagenous stroma around the tumour. When it occurs in the periorbital region, there is a high risk of orbital invasion and vision and life-threatening complications [27].
7 Loss of the Entire Upper and Lower Lids (Figs. 36 and 37)
7.1 Orbital Invasion by Facial Cancer
The 87-year-old retired farmer in Fig. 38 presented with a longstanding ulcerated BCC of his left supraorbital region and a large melanoma in situ of his medial cheek/nasojugal region. The duration of tumour growth was 2 years. The pre-surgery images show left brow ptosis and loss of left forehead wrinkles suggesting frontalis muscle invasion. Wide excision down to the periosteum of his left supraorbital ridge revealed transection of the deep margin and both focal perineural and lymphovascular invasion. Local flap repair was performed for wound closure, but a further wide excision did not occur. Within a year he re-presented with left orbital invasion and recurrence. This was managed by an MDT, and he was offered palliative radiotherapy, which failed to cure him. He also lost the sight in his left eye. This subtype of BCC has an incidence of 1–3% and is associated with recurrence rates of up to 45%. It is most common in elderly males, with white skin and extensive actinic damage as in this patient.
(a–c) A multiply recurrent, locally advanced BCC in an 81-year-old woman. There was an extensive facial defect after Mohs micrographic surgery involving complete excision of the left upper and lower eyelids and the right lower lid. No suitable eyelid donor tissue remained to reconstruct the left upper eyelid. Therefore the left eye’s conjunctival remnants were closed to cover the cornea, and a forehead flap was used to cover the skin defect
(a and b) A 92-year-old man with a recurrent left conjunctival SGC, initially diagnosed as a conjunctival SCC. Four years earlier the cornea had perforated and the eye had been eviscerated. The patient presented with rapid growth of a painful anterior orbital mass. He underwent orbital exenteration and adjunctive radiotherapy
(a–e) Recurrence of a high-risk left supraorbital ulcerated BCC in the left orbit despite initial surgical excision in a retired 87-year-old farmer. The MRI scan demonstrated frontal bone and superior orbital invasion. The scan also demonstrated perineural invasion into the cavernous sinus and the mandibular division of the trigeminal nerve. The final image shows a centrolateral tarsorrhaphy used to treat chronic painful corneal ulceration and prevent corneal perforation after radiotherapy
The female patient in Fig. 39 is a case of recurrent adenocarcinoma of the right orbit shown also in Chap. 6 “The Burden of Facial Deformity”. Invasion of the orbit by cancer is an indication for exenteration of the orbit. Her vision had already been lost due to the tumour and radiotherapy, but she is an example of the principle that sometimes the eye has to be sacrificed to save life. Her right orbito-cranial reconstruction was achieved with split calvarial bone grafts, a temporalis transposition muscle and pericranial flaps deeply, plus a large cervico-facial flap for skin cover. Brachytherapy tubes were placed deep to the skin flap for further adjuvant radiation.
8 Prosthetic Rehabilitation/Reconstruction
The use of prosthetic options began in the Great War (1914–1918) with painted tin masks and has evolved to a modern science/craft with 3D computerised planning, life-like silicone prosthetic implants and osseo-integrated abutment technology for fixation. This is covered comprehensively in Chap. 17 “Modern Maxillofacial Rehabilitation”, by the authors Williams et al.
The male patient in Fig. 40 has a large right orbito-cranial defect after exenteration, which has been reconstructed with an elegant life-like prosthetic by Dr. Keith Pine PhD, an experienced ocular prosthetist, who previously worked in Sir William Manchester’s Middlemore Plastic Surgery/Dental Unit, from the 1970s for 16 years. He has published a textbook on Ocular Prosthetics in 2015, the first textbook to offer a comprehensive account of ocular prosthetics and the evidence used to underpin and support this field of healthcare [28].
A case (used with permission from Michael Williams) of ocular prosthetist is shown in Fig. 41. The aesthetic standard of the right orbital reconstruction with osseo-integrated prosthetic is exceptional, with added spectacle frames.
9 Complication Management
9.1 Lower Eyelid Ectropion (Figs. 42, 43, and 44)
All lower eyelid reconstruction needs to pre-empt postoperative lower lid ectropion. Lower lid skin grafts must be accompanied by procedures to horizontally shorten the palpebral ligaments. Generally, the lateral palpebral ligament is shortened, for example, by a lateral tarsal strip or other lateral palpebral tightening procedure [29]. If the lateral end of the lower lid has been disinserted, fixation of the cut end of the tarsal plate and/or other orbital septal remnants to the lateral orbital rim or periosteal flap is required.
(a–c) Lower eyelid wounds must be closed vertically to prevent ectropion. Figure 42c shows fixation of the cut end of the tarsal plate and other lateral retinacular tissues to the orbital rim periosteum (dotted lines indicate the location of the lateral orbital rim) to prevent postoperative ectropion
Medial ectropion after medial canthal tumour excision repaired with a full-thickness skin graft. Correction would involve horizontally tightening the posterior limb of the medial palpebral ligament, taking care not to damage the lower canaliculus. Alternatively a medial canthoplasty could be used to support the medial lower eyelid. The anterior lamella of the medial lower eyelid requires vertical lengthening with a full-thickness skin graft or a transposition flap from the nasal bridge or glabella
(a–e) In this case of a lower eyelid and lateral canthal recurrent BCC in a 78-year-old woman, the defect after Mohs micrographic surgery was initially reconstructed with a partial direct closure, horizontal eyelid shortening and full-thickness skin graft from the upper eyelid. Due to vertical scar contracture, the ectropion recurred. This was successfully corrected with a cheek rotation flap
Shortening the posterior limb of the medial palpebral ligament is more difficult to achieve. The posterior limb of the medial palpebral ligament, which is the key structure holding the lower lid in apposition to the eye, is more diffuse than the lateral retinacular tissues and difficult to suture to the posterior lacrimal crest which has a very fragile, thin periosteal covering.
If there is a defect of the medial lower eyelid and palpebral ligament, the best approximation is to suture the cut medial eyelid tarsal plate to the medial remnants of the medial palpebral ligament’s anterior limb or to a medial periosteal flap. To recreate the normal lower lid contour, the medial eyelid should be pulled slightly superiorly.
Secondary correction of a cicatricial ectropion is achieved by addressing laxity of the inferior retractors of the lower eyelid, horizontally shortening the lower lid and replacing the shortened anterior lamella by a full-thickness skin graft [30] or transposition flap.
9.2 Recurrent Tumour at the Site of Previous Tumour Causing Lower Eyelid Cicatricial Ectropion (Fig. 45)
(a–g) A 79-year-old man with a medial cicatricial ectropion after previous excision of a lower eyelid BCC. An incisional biopsy at the site of the previous surgery revealed a recurrent infiltrating morphoeic BCC. After several stages of Mohs micrographic surgery, the procedure was abandoned as the patient was not able to tolerate further excision. In Fig. 45b, the circled areas had residual disease that was not able to be excised by the Mohs surgeon. The resulting defect was repaired with glabellar and island cheek flaps. Necrosis of the tip of the cheek flap resulted in a medial ectropion. The upper eyelid was tethered medially and laterally. Further cicatrisation occurred after adjuvant radiotherapy. The resulting ptosis interfered with the left eye’s vision. The medial end of the lid was released, and the medial conjunctival fornix reformed with a buccal mucous membrane flap. Further surgery including a Hughes tarsoconjunctival flap & a full thickness skin graft was planned to correct the lower eyelid cicatricial ectropion
9.3 Lagophthalmos (Fig. 46)
An 81-year-old woman who had a paramedian forehead flap to repair a left medial canthal defect. The patent’s upper eyelid was sutured to the skin of the flap, immobilising it. This resulted in lagophthalmos, chronic ocular irritation and reduced vision. Care must be taken when attaching the thin flexible eyelid tissues to flaps with thicker skin and subcutaneous tissue. To maintain satisfactory eyelid excursion, periosteal flaps are a more suitable option for reattaching disinserted upper eyelids
9.4 Severe Postoperative Lagophthalmos and Blindness (Fig. 47)
This is the most feared complication of eyelid surgery. At the conclusion of eyelid reconstruction, the surgeon must ensure that the eye can passively close. In addition, to prevent corneal abrasions, scarring and vision loss, any graft overlying the cornea must be lined with non-keratinising epithelium, e.g. conjunctiva, buccal mucosa, hard palate mucosa or homologous amniotic membrane. A temporary or permanent tarsorrhaphy may be required to protect the cornea from abrasions and dehydration. A temporary suture tarsorrhaphy will usually last up to 3 weeks. Permanent tarsorrhaphies are usually constructed so they can be reversed, when appropriate (Fig. 48).
9.5 Postoperative Diplopia (Fig. 49)
(a–d) Conjunctival symblepharon causing diplopia. In this 63-year-old man, Mohs micrographic surgery was used to excise an infiltrating right medial canthal BCC. Bulbar conjunctiva was infiltrated with tumour and excised. The eyelids were reconstructed with a medial periosteal flap, glabellar flap and full-thickness supraclavicular skin graft. Generally the conjunctiva will granulate satisfactorily. In this case, a conjunctival adhesion caused restriction of right eye abduction and diplopia. The scarred bulbar conjunctiva was excised and replaced with an amniotic membrane graft
10 Innovations
Immunotherapy drugs are indicated in extreme facial cancer cases if other therapeutic options have been exhausted or are contraindicated. These include vismodegib, pembrolizumab and cemiplimab.
Vismodegib is a selective inhibitor of abnormal signalling in the molecular driver of BCC – the ‘hedgehog’ pathway. It can be considered in adults with locally advanced disease who are not able to undergo surgery or radiation [31]. It can also be used in metastatic BCC and in basal cell naevus (Gorlin-Goltz) syndrome. Vismodegib has also been used as neoadjuvant treatment to shrink large locally advanced BCCs prior to surgery. While it can be very effective, resistant BCCs have been reported to grow despite vismodegib treatment [32]. Rebound BCC growth after cessation of treatment has also been reported [33].
Cemiplimab and pembrolizumab are drugs that target programmed cell death (PD-1) receptors. They can be used for patients with advanced local or metastatic cutaneous SCC that is not treatable by surgery or radiation [34, 35].
11 Conclusion/Summary
The management of periorbital cancers is a challenge, and preservation of visual function is a priority. In the most extreme cases, vision may have to be sacrificed to preserve the patient’s life. The periorbital region has a direct connection to the ocular system, key cranial nerves and the central nervous system. Gillies’ enduring principles 12 and 13 are important to remember in this anatomical region:
-
12. Never let routine methods become your master.
-
13. Consult other specialists.
As in many other fields of oncology, the periorbital region may require solutions only possible with the collaboration of a co-ordinated and efficient multidisciplinary team. For the future, plastic surgeons and ophthalmologists specialising in oculoplastic surgery can learn much from each team member’s approach.
References
Mustardé JC. Repair and reconstruction in the orbital region: a practical guide. 1st ed. Edinburgh: Churchill Livingstone; 1965.
McMinn RMH, Hutchings RT, Logan BM. A colour atlas of head and neck anatomy. London: Wolfe Medical Publications Ltd; 1981.
van der Meulen JC, Gruss JS. Colour atlas and text of ocular plastic surgery. Maryland Heights: Mosby-Wolfe; 1996.
Brown E, Klaassen MF. Perfection: the life and times of Sir William Manchester. Auckland: Mary Egan Publishers; 2021.
McConnell LK, Syed NA, Zimmerman MB, Carter KD, Nerad JA, Allen RC, Shriver EM. An analysis of conjunctival map biopsies in sebaceous carcinoma. Ophthal Plast Reconstr Surg. 2017;33(1):17–21.
Cheung JJC, Esmaeli B, Lam SC, Kwok T, Yuen HKL. The practice patterns in the management of sebaceous carcinoma of the eyelid in the Asia Pacific region. Eye (Lond). 2019 Sep;33(9):1433–42.
Edge S, Byrd DR, Compton CC, Fritz AG, Greene F, Trotti A (Eds.) AJCC cancer staging handbook. From the AJCC cancer staging manual. 8th ed. Springer Nature.
Wolf DJ, Zitelli JA. Surgical margins for basal cell carcinoma. Arch Dermatol. 1987;123(3):340–4.
Giordano Resti A, Sacconi R, Baccelli N, Bandello F. Outcome of 110 basal cell carcinomas of the eyelid treated with frozen section-controlled excision: mean follow-up over 5 years. Eur J Ophthalmol. 2014;24(4):476–82.
Chalfin J, Putterman AM. Frozen section control in the surgery of basal cell carcinoma of the eyelid. Am J Ophthalmol. 1979;87(6):802–9.
Mohs FE. Micrographic surgery for the microscopically controlled excision of eyelid cancers. Arch Ophthalmol. 1986;104(6):901–9.
Leibovitch I, Huilgol SC, Selva D, Richards S, Paver R. Basal cell carcinoma treated with Mohs surgery in Australia II. Outcome at 5-year follow-up. J Am Acad Dermatol. 2005;53(3):452–7.
Leibovitch I, Huilgol SC, Selva D, Hill D, Richards S, Paver R. Cutaneous squamous cell carcinoma treated with Mohs micrographic surgery in Australia I. experience over 10 years. J Am Acad Dermatol. 2005 Aug;53(2):253–60.
Tierney EP, Hanke CW. Cost effectiveness of Mohs micrographic surgery: review of the literature. J Drugs Dermatol. 2009;8(10):914–22.
Wong VA, Marshall JA, Whitehead KJ, Williamson RM, Sullivan TJ. Management of periocular basal cell carcinoma with modified en face frozen section controlled excision. Ophthalmic Plast Reconstr Surg. 2002;18(6):430–5.
Morris DS, Elzaridi E, Clarke L, Dickinson AJ, Lawrence CM. Periocular basal cell carcinoma: 5-year outcome following slow Mohs surgery with formalin-fixed paraffin-embedded sections and delayed closure. Br J Ophthalmol. 2009;93(4):474–6.
Behan FC, Findlay M, Lo CH. The keystone perforator island flap concept. Sydney: Churchill Livingstone; 2012.
Klaassen MF, Brown E. An examiner’s guide to professional plastic surgery exams. Springer Nature; 2018. isbn:978-981-13-0688-4.
Pfeiffer ML, Savar A, Esmaeli B. Sentinel lymph node biopsy for eyelid and conjunctival tumors: what have we learned in the past decade? Ophthalmic. Plast Reconstr Surg. 2013;29(1):57–62.
Ng SGJ, Inkster CF, Leatherbarrow B. The rhomboid flap in medial canthal reconstruction. Br J Ophthalmol. 2001;85(5):556–9.
Klaassen MF, Brown E, Behan FC. Simply local flaps. Springer Nature; 2018. isbn:978-3-319-59400-2.
Kersten RC, Kulwin DR. “One-stitch” canalicular repair. A simplified approach for repair of canalicular laceration. Ophthalmology. 1996;103(5):785–9. https://doi.org/10.1016/s0161-6420(96)30615-5. PMID: 8637688.
Manchester WM. A simple method for repair of full thickness defects of the lower eyelid with special reference to the treatment of neoplasms. Br J Plast Surg. 1951;3:252–63.
Maloof A, Ng SGJ, Leatherbarrow B. The maximal Hughes procedure. Ophthalmic Plast Reconstr Surg. 2001;17(2):96–102.
McKelvie J, Ferguson R, Ng SGJ. Eyelid reconstruction using the “Hughes” tarsoconjunctival advancement flap: long-term outcomes in 122 consecutive cases over a 13-year period. Orbit. 2017;36(4):228–33.
Leibovitch I, Selva D. Modified Hughes flap: division at 7 days. Ophthalmology. 2004;111(12):2164–7.
Botha VE, Chow KTK, Salmon PJM, El-Khayat RH, Sun MT, Selva D, Ng SGJ. Periorbital desmoplastic squamous cell carcinoma. Orbit. 2019;38(3):240–3.
Pine KR, Sloan BH, Jacobs RJ. Clinical ocular prosthetics. Springer Nature; 2015. isbn:978-3-319-19057-0.
Liu D. Lower eyelid tightening: a comparative study. Ophthalmic Plast Reconstr Surg. 1997;13(3):199–203.
McKelvie J, Papchenko T, Carroll S, Ng SGJ. Cicatricial ectropion surgery: a prospective study of long-term symptom control, patient satisfaction and anatomical success. Clin Exp Ophthalmol. 2018;46(9):1002–7.
Wong KY, Fife K, Lear JT, Price RD, Durrani AJ. Vismodegib for locally advanced periocular and orbital basal cell carcinoma: a review of 15 consecutive cases. Plast Reconstr Surg Glob Open. 2017;5(7):e1424.
Chang AL, Atwood SX, Tartar DM, Oro AE. Surgical excision after neoadjuvant therapy with vismodegib for a locally advanced basal cell carcinoma and resistant basal carcinomas in Gorlin syndrome. JAMA Dermatol. 2013;149(5):639–41.
Wolfe CM, Green WH, Cognetta AB Jr, Hatfield HK. Basal cell carcinoma rebound after cessation of vismodegib in a nevoid basal cell carcinoma syndrome patient. Dermatol Surg. 2012;38(11):1863–6.
Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G, Psyrri A Jr, Basté N, Neupane P, Bratland Å, Fuereder T, Hughes BGM, Mesía R, Ngamphaiboon N, Rordorf T, Wan Ishak WZ, Hong RL, González Mendoza R, Roy A, Zhang Y, Gumuscu B, Cheng JD, Jin F, Rischin D, KEYNOTE-048 Investigators. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394(10212):1915–28.
Migden MR, Rischin D, Schmults CD, Guminski A, Hauschild A, Lewis KD, Chung CH, Hernandez-Aya L, Lim AM, Chang ALS, Rabinowits G, Thai AA, Dunn LA, Hughes BGM, Khushalani NI, Modi B, Schadendorf D, Gao B, Seebach F, Li S, Li J, Mathias M, Booth J, Mohan K, Stankevich E, Babiker HM, Brana I, Gil-Martin M, Homsi J, Johnson ML, Moreno V, Niu J, Owonikoko TK, Papadopoulos KP, Yancopoulos GD, Lowy I, Fury MG. PD-1 blockade with Cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med. 2018;379(4):341–51.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ng, S.G.J., Klaassen, M.F., Brown, E. (2022). Extreme Cancer of the Periorbital Region. In: Burton, I., Klaassen, M.F. (eds) Atlas of Extreme Facial Cancer. Springer, Cham. https://doi.org/10.1007/978-3-030-88334-8_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-88334-8_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-88333-1
Online ISBN: 978-3-030-88334-8
eBook Packages: MedicineMedicine (R0)